Abstract
Background
This study aimed to investigate the association between central sensitivity to thyroid hormones and all-cause mortality in euthyroid patients with chronic kidney disease (CKD).
Methods
Data on thyroid function indicators and all-cause mortality for CKD patients were extracted from the NHANES database (2007–2012). Central sensitivities to thyroid hormones were mainly evaluated by Thyroid Feedback Quantile-based Index (TFQI). The Kaplan–Meier method, Cox proportional hazards regression model and subgroup analysis were performed to explore the potential associations between thyroid hormone sensitivity and all-cause mortality.
Results
A total of 1303 euthyroid CKD patients were enrolled in this study. After a median follow-up of 115 months, 503 participants died. The Kaplan-Meier analysis demonstrated significant variations in survival rates among different levels of TFQI (P = 0.0015). Cox regression analysis showed that increased levels of TFQI were independent risk factors for all-cause mortality after adjusting for multiple confounding factors (HR = 1.40, 95% CI 1.10–1.79, P = 0.007). Subgroup analysis did not reveal any significant variation in the association between TFQI and all-cause mortality between the subgroups assessed (P for interaction > 0.05).
Conclusion
Our study suggests that impaired thyroid hormone sensitivity might be linked to increased mortality in euthyroid CKD patients. Further research is needed to confirm and explore this association.
Similar content being viewed by others
Introduction
As one of the leading causes of death and suffering in the 21st century, chronic kidney disease (CKD) affects more than 10% of the general population worldwide, placing enormous economic and social pressure on the world [1]. Previous studies have shown that here is a bi-directional link between kidney and thyroid function [2, 3]. Thyroid hormones directly or indirectly affect renal development, structure, hemodynamics, glomerular filtration rate, and water and electrolyte homeostasis [4]. The high burden of thyroid dysfunction, whether subclinical or overt, is closely associated with survival prognosis and adverse outcomes in patients with CKD [3, 5, 6]. Studies have shown that TSH levels in the abnormal range are associated with a higher risk of death for non-dialysis and dialysis-dependent CKD patients [6, 7].
However, whether this risk extends to CKD patients with normal thyroid function remains controversial. One previous study suggested that a mild form of acquired thyroid hormone resistance may occur in the general population and accordingly proposed a new central thyroid hormone resistance index (Thyroid Feedback Quantile-based Index, TFQI) that focuses on deviations in the average pituitary inhibition to thyroid hormone in the population [8]. Thyroid hormone resistance can be systematically divided into central resistance which influences the feedback loop set point in the central nervous system and peripheral resistance which reduces hormone metabolism [9, 10]. Compared to the latter, the former is easier to evaluate and can be quantified by looking at thyroid hormone and TSH concentrations or indicators derived from them [8, 11, 12]. One retrospective study found that decreased thyroid hormone sensitivity is associated with decreased renal function in normal thyroid function population, and that the composite index composed of TSH and free thyroxine (FT4) correlates more strongly to renal function than TSH or FT4 alone [13].
At present, it is uncertain whether changes in thyroid hormone sensitivity affect survival outcomes in patients with CKD. Therefore, we analyzed data from the National Health and Nutrition Examination Survey (NHANES) database (2007–2012) to explore the association between central thyroid hormone resistance index and the risk of all-cause death in CKD patients.
Methods
Study population
Data were obtained from NHANES, which is a periodic program designed to assess the health and nutrition status of adults and children in the United States administered by the National Center for Health Statistics (NCHS) [14]. NHANES is a stratified, multi-stage survey with good national representation and participants are selected at random through a complex statistical process each year. Our analysis finally comprised of a total of 1303 eligible participants, obtained by merging data from the NHANES cycles: 2007–2008, 2009–2010, and 2011–2012 (30,442 participants) (Fig. 1). All included participants were CKD (Stage 1–4) patients aged 20 and above, with complete thyroid function indicators and death data, and no history of pregnancy. The laboratory normality reference ranges were 7.74 − 20.64 pmol/L for FT4 and 0.34 − 5.60 mIU/L for TSH [15]. Those with abnormal TSH and FT4 levels were also excluded. Additionally, participants undergoing thyroid hormone replacement therapy (levothyroxine, thyroxine, thyroid desiccated, or other) and those with a history of thyroid disease were also excluded from the study.
Assessment of CKD
Age, gender, race, and serum creatinine (SCr) were used to evaluate estimated glomerular filtration rate (eGFR, ml/min/1.73 m2) for each participant, according to the computational equations of the CKD Epidemiology Society (CKD-EPI) [16]. CKD was defined as eGFR < 60 mL/min/1.73 m2 and/or urinary albumin to urinary creatinine ratio (UACR) ≥ 30 mg/g. The corresponding CKD stages were defined as: Stage 1, eGFR ≥ 90 mL/min/1.73 m2, along with UACR ≥ 30 mg/g; Stage 2, eGFR 60–89 mL/min/1.73 m2, along with UACR ≥ 30 mg/g; Stage 3, eGFR 30–59 mL/min/ 1.73m2; Stage 4, eGFR 15–29 mL/min/ 1.73m2; and Stage 5, eGFR < 15 mL/min/ 1.73m2 [17]. We excluded these participants with CKD Stage 5 because it was not clear whether they were on dialysis.
Calculation of thyroid hormone sensitivity
The index reflecting thyroid central sensitivity were TSH T4 resistance index (TT4RI), TSH index (TSHI), and TFQI. TT4RI was calculated as FT4 (pmol/L) ⋅ TSH (mIU/L) [11]. TSHI = ln TSH (mIU/L) + 0.1345 ⋅ FT4 (pmol/L) [12]. The formula for calculating TFQI was cumulative distribution function (cdfFT4) – (1 – cdfTSH) [8]. FT4 and TSH concentrations were measured at the University of Washington using the two-step enzyme immunoassay and two-site immunoenzymatic (“sandwich”) assay, respectively.
Other variables
Data on other potential covariates employed in the statistical analyses included information on age, gender, race, smoking status, physical activity, annual household income, diabetes, hypertension, cardiovascular disease, body mass index (BMI, kg/m2), alanine transaminase (ALT, U/L), aspartate transaminase (AST, U/L), gamma-glutamyl transferase (GGT, U/L), and glycohemoglobin. BMI is categorized into three groups: <25 kg/m2 for normal weight, 25–29.9 kg/m2 for overweight, and ≥ 30 kg/m2 for obesity. Smokers are classified as current or former. Self-reported diabetes and hypertension are also defined, and the presence of cardiovascular disease is determined based on self-reported history of heart attack, stroke, congestive heart failure, coronary artery disease, or angina. Detailed measurement procedures for all variables in this study are publicly available in the NHANES database [15].
Mortality
We utilized the NHANES Public-Use Linked Mortality File up to 31 December 2019, which employs a probabilistic algorithm to match with National Death Index (NDI) data for ascertaining mortality status [18]. The duration of follow-up for each participant was determined as the difference between the baseline examination date and the last known date alive or censored from the mortality file. The outcome of this study was all-cause mortality, encompassing deaths from all diseases, accidental incidents, and various other factors.
Statistical analysis
All statistical analyses were performed in accordance with Centers for Disease Control and Prevention (CDC) guidelines. A complex multistage cluster survey design was fully considered, and the corresponding weight values were applied. Continuous variables were presented as mean ± standard error and categorical variables were presented as proportions (standard error). Weighted Student’s t-test and chi-squared test were used to compare continuous and categorical variables in multiple groups, respectably. The Kaplan–Meier method was employed to estimate the survival among different TFQI levels, and the differences were evaluated with a stratified log-rank test. Cox regression model was employed to analyze the independent effects of various thyroid resistance indices (FT3/FT4, TT4RI, TSHI, and TFQI) on all-cause mortality in patients with CKD, using both unadjusted and fully adjusted models. The fully adjusted model accounted for multiple covariates, including age, gender, race, annual income, moderate physical activity, smokers, hypertension, diabetes, cardiovascular diseases, CKD stages, BMI, ALT, AST, GGT, and glycohemoglobin. Based on adjusted model, a restrictive cubic spline analysis was conducted to assess the relationship between the TFQI index and all-cause mortality risk in CKD patients, using the median values of the TFQI as the reference (HR = 1). Time-dependent Receiver Operating Characteristic (ROC) analyses using an unadjusted model were employed to evaluate clinical applicability. Subgroup analyses were performed on a priori basis, stratified by age, gender, race, BMI, hypertension, diabetes, cardiovascular diseases, and CKD stages. The Empower software (http://www.empowerstats.com) and R version 4.1.2 (http://www.R-project.org) were employed for all analyses. A P value ≤ 0.05 was considered statistically significant.
Results
Characteristics of study population
The median follow-up period was 115 months. By December 31, 2019, 503 participants had died (Table 1). The deceased group was generally older, more often male, had lower annual income, were smokers, engaged in less moderate physical activity, and had higher levels of SCr, eGFR, UACR, FT4, TSH, and higher CKD stages (P < 0.05). They also had a higher prevalence of hypertension, diabetes, and cardiovascular diseases (P < 0.001). There were also significant differences in the distribution of race between the groups (P = 0.001). The deceased group exhibited significantly lower FT3 levels (P < 0.001). No significant differences in BMI, ALT, AST, and GGT were observed between the deceased and surviving groups (P > 0.05). Importantly, the deceased group had higher TT4RI, TSHI, and TFQI levels compared to the surviving group (P < 0.001).
Clinical features of the participants according to the tertiles of TFQI index
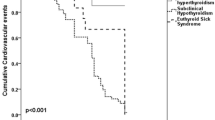
The weighted baseline characteristics based on the TFQI tertiles were also presented in Table 2. Participants with higher TFQI levels exhibited significantly higher age, prevalence of obesity, diabetes, hypertension, cardiovascular disease, SCr, eGFR, CKD stages, FT4, TSH, TT4RI, and TSHI (P < 0.05). FT3 levels were significantly lower (P < 0.001). Notably, all-cause mortality was significantly higher with elevated TFQI tertiles, increasing from 26.61% in Tertile 1 to 40.89% in Tertile 3 (P = 0.001). It was observed that TFQI values were associated with CKD stage, with more advanced stages of CKD associated with higher TFQI (P < 0.001) (Fig. 2).
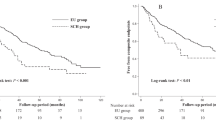
Survival analysis results based on TFQI tertiles
As shown in Fig. 3, the Kaplan-Meier analysis revealed statistically significant differences in survival probability across the three TFQI levels. The analysis indicated the lowest survival in participants with high level of TFQI (P = 0.0015).
The association between central thyroid hormone resistance index and all-cause death
Cox proportional hazards regression analysis confirmed that thyroid hormone indices were positively related with all-cause mortality among CKD patients (Table 3). In both fully adjusted and non-adjusted models, we found that TT4RI, TSHI and TFQI were positively associated with the risk of all-cause mortality. In fully adjusted models, the results indicated a 40% increased risk of death per unit increase in TFQI index (HR = 1.40, 95% CI 1.10–1.79, P = 0.007). Consistent with previous studies, we also discovered in CKD patients that peripheral thyroid hormone sensitivity (FT3/FT4) is associated with all-cause mortality (HR = 0.69, 95% CI 0.57–0.84, P < 0.001) [19]. Additionally, classification of TFQI into tertiles showed that higher TFQI teritles levels were associated with a higher prevalence of death (P for trend = 0.050). Results of restrictive cubic strip analysis showed a positive relationship between TFQI and all-cause mortality among participants with CKD, with no significant threshold effect observed (Fig. 4). In the ROC analyses, TFQI in patients of 150 months follow-up duration showed a higher AUC (0.61) for predicting all-cause mortality compared to 120 months (0.58) and 60 months (0.58) (Fig. 5). Additionally, compared to TSHI and TT4RI, TFQI performed better at predicting mortality (Attachment 1).
Subgroup stratification analyses
The subgroup analyses in Fig. 6 demonstrated that the association of TFQI level and all-cause mortality is consistent after being stratified by age, gender, race, BMI, hypertension, diabetes, cardiovascular diseases, and CKD (P for interaction > 0.05).
Discussion
We noted a strong association between TFQI and all-cause mortality among patients with stage 1–4 CKD in a representative sample of US adults on the NHANES 2007–2010 data. In this cohort study, we discovered a linear relationship between TFQI levels and all-cause mortality in CKD patients. After fully adjusting for confounding factors, increased levels of TFQI were independent risk factors for all-cause mortality (HR = 1.40, 95% CI 1.10–1.79, P = 0.007).
Previous studies have also revealed an association between FT4 levels within the normal range and the risk of all-cause mortality [19, 20]. However, some studies have indicated that both the high-normal and low-normal TSH groups have a significantly higher risk of all-cause mortality compared to the mid-normal TSH group [21, 22]. Based on negative feedback regulation, it seems difficult to fully explain this phenomenon, especially for the high-normal TSH. Hence, we attempted to elucidate this association from the perspective of central thyroid resistance. In individuals with normal thyroid function, the correlation between the assessment index based on thyroid hormone sensitivity and the risk of death is stronger than the assessment of individual indices alone [23]. This finding might partly explain the inconsistencies observed in previous studies, such as the nonlinear relationship between TSH levels and the risk of death and helps establish the link between thyroid function and all-cause mortality risk in CKD patients with normal thyroid function. Among the three indices for evaluating thyroid hormone central sensitivity, we found that TFQI has a stronger correlation with the risk of death. Previous studies have also indicated that in assessing abnormal response ranges of the thyroid to TSH, TFQI is more closely related to diabetes risk compared to TT4RI and TSHI [8]. We observed that in the time-dependent ROC analysis, the AUC for TFQI alone ranges from 0.58 to 0.61. Evaluating the predictive ability of TFQI in isolation may underestimate its true effect. A more comprehensive assessment of TFQI’s contribution can be achieved through multivariable analysis, which considers the incremental value of combining TFQI with other variables. Furthermore, the specific impact of TFQI should be evaluated within different clinical contexts and subjected to repeated validation across diverse populations to assess its value more objectively in predicting mortality.
The association between thyroid resistance index and mortality also has some reasonable biological mechanisms. Higher levels of FT4 within the reference range are associated with many adverse cardiac events, including heart failure, atrial fibrillation, and cardiac sudden death [24,25,26]. Elevated FT4 levels in the general population are also associated with an increased risk of solid tumors, including breast, prostate, lung, and ovarian cancers [23, 27]. Despite the results of interaction tests not identifying specific populations, patients without hypertension, diabetes, or cardiovascular diseases appear to have a greater risk. Previous findings also indicated that reduced sensitivity to thyroid hormones serves as a risk factor for hypertension, diabetes, and cardiovascular diseases [8, 28, 29]. Therefore, we speculate that these diseases might partially mediate the link between thyroid hormone sensitivity and the risk of all-cause mortality. Additionally, the relatively small sample sizes in subgroups might also contribute to potential biases in the results. We also found that the impaired central sensitivity of the thyroid is related to the CKD stage, indicating that the impaired central sensitivity of the thyroid may itself be involved in the exacerbation of CKD. Thyroid hormones can directly participate in vascular and endothelial dysfunction and contribute to the formation of albuminuria [30, 31]. Thyroid resistance may also induce changes in the immune microenvironment of kidney disease, thereby enhancing immune inflammatory responses, ultimately leading to kidney damage [32].
Our study has several limitations. First, the relatively small sample size and limited number of events available for analysis restrict the precision of the estimates and have prevented us from exploring specific analyses by causes of mortality that should be assessed in larger studies. Second, thyroid function was measured only at baseline, with no data on the changes in thyroid function over time. Thyroid-related antibodies, metabolic syndrome, and nonalcoholic fatty liver disease, as possible confounding factors, were not included in the study. Third, the mortality data we used was sourced from Public-use-files. Synthetic data were substituted for follow-up time or underlying cause of death, which to some extent hindered more in-depth analysis. Additionally, our study also did not consider the history of medication use that might affect thyroid function, such as beta blockers, steroids, and amiodarone. Finally, as our research used samples from people in the United States, the universal applicability of our results requires further validation.
Conclusion
Our study demonstrates that impaired sensitivity to thyroid hormone might be associated with all-cause mortality in CKD patients with normal thyroid function, independent of other traditional risk factors and comorbidities. The nature of this association is currently unclear and requires further research to confirm and explore.
Data availability
Data was collected from the NHANES database (https://www.cdc.gov/nchs/nhanes/). Summary data supporting the study’s findings are available upon request from the corresponding author.
References
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022;12(1):7–11. https://doi.org/10.1016/j.kisu.2021.11.003.
Rhee CM. The interaction between thyroid and kidney disease: an overview of the evidence. Curr Opin Endocrinol Diabetes Obes. 2016;23(5):407–15. https://doi.org/10.1097/med.0000000000000275.
Narasaki Y, Sohn P, Rhee CM. The interplay between thyroid dysfunction and kidney disease. Semin Nephrol. 2021;41(2):133–43. https://doi.org/10.1016/j.semnephrol.2021.03.008.
Mariani LH, Berns JS. The renal manifestations of thyroid disease. J Am Soc Nephrol. 2012;23(1):22–6. https://doi.org/10.1681/asn.2010070766.
Kang EW, Nam JY, Yoo TH, Shin SK, Kang SW, Han DS, Han SH. Clinical implications of subclinical hypothyroidism in continuous ambulatory peritoneal dialysis patients. Am J Nephrol. 2008;28(6):908–13. https://doi.org/10.1159/000141933.
Rhee CM, Ravel VA, Streja E, Mehrotra R, Kim S, Wang J, Nguyen DV, Kovesdy CP, Brent GA, Kalantar-Zadeh K. Thyroid functional disease and mortality in a National Peritoneal Dialysis Cohort. J Clin Endocrinol Metab. 2016;101(11):4054–61. https://doi.org/10.1210/jc.2016-1691.
Rhee CM, Kalantar-Zadeh K, Ravel V, Streja E, You AS, Brunelli SM, Nguyen DV, Brent GA, Kovesdy CP. Thyroid status and death risk in US Veterans with chronic kidney disease. Mayo Clin Proc. 2018;93(5):573–85. https://doi.org/10.1016/j.mayocp.2018.01.024.
Laclaustra M, Moreno-Franco B, Lou-Bonafonte JM, Mateo-Gallego R, Casasnovas JA, Guallar-Castillon P, Cenarro A, Civeira F. Impaired sensitivity to thyroid hormones is Associated with Diabetes and metabolic syndrome. Diabetes Care. 2019;42(2):303–10. https://doi.org/10.2337/dc18-1410.
Refetoff S, Weiss RE, Usala SJ. (1993) The syndromes of resistance to thyroid hormone. Endocr Rev 14(3): 348 – 99. https://doi.org/10.1210/edrv-14-3-348
Corica D, Licenziati MR, Calcaterra V, Currò M, Di Mento C, Curatola S, Zuccotti G, Alibrandi A, Ientile R, Aversa T, Wasniewska M. Central and peripheral sensitivity to thyroid hormones and glucose metabolism in prepubertal children with obesity: pilot multicenter evaluation. Endocrine. 2023;80(2):308–11. https://doi.org/10.1007/s12020-022-03276-5.
Yagi H, Pohlenz J, Hayashi Y, Sakurai A, Refetoff S. Resistance to thyroid hormone caused by two mutant thyroid hormone receptors beta, R243Q and R243W, with marked impairment of function that cannot be explained by altered in vitro 3,5,3’-triiodothyroinine binding affinity. J Clin Endocrinol Metab. 1997;82(5):1608–14. https://doi.org/10.1210/jcem.82.5.3945.
Jostel A, Ryder WD, Shalet SM. The use of thyroid function tests in the diagnosis of hypopituitarism: definition and evaluation of the TSH Index. Clin Endocrinol (Oxf). 2009;71(4):529–34. https://doi.org/10.1111/j.1365-2265.2009.03534.x.
Yang S, Lai S, Wang Z, Liu A, Wang W, Guan H. Thyroid feedback quantile-based Index correlates strongly to renal function in euthyroid individuals. Ann Med. 2021;53(1):1945–55. https://doi.org/10.1080/07853890.2021.1993324.
Fain JA. NHANES Diabetes Educ. 2017;43(2):151. https://doi.org/10.1177/0145721717698651.
The National Health and Nutrition Examination. Survey (NHANES) database. https://www.cdc.gov/nchs/nhanes/. Accessed 10 Jan 2024.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Whaley-Connell AT, Sowers JR, Stevens LA, McFarlane SI, Shlipak MG, Norris KC, Chen SC, Qiu Y, Wang C, Li S, Vassalotti JA, Collins AJ. CKD in the United States: kidney early evaluation program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 Suppl 2):S13–20. https://doi.org/10.1053/j.ajkd.2007.12.016.
The NHANES Public-Use Linked Mortality Database. https://www.cdc.gov/nchs/data-linkage/mortality-public.htm. Accessed 10 Jan 2024.
Lang X, Li Y, Zhang D, Zhang Y, Wu N, Zhang Y. FT3/FT4 ratio is correlated with all-cause mortality, cardiovascular mortality, and cardiovascular disease risk: NHANES 2007–2012. Front Endocrinol (Lausanne). 2022;13964822. https://doi.org/10.3389/fendo.2022.964822.
Yuan D, Jia S, Zhu P, Zhang C, Liu Y, Liu R, Xu J, Tang X, Zhao X, Gao R, Yang Y, Xu B, Gao Z, Yuan J. Usefulness of FT3 to FT4 ratio to Predict Mortality in Euthyroid patients with Prior Cardiovascular events undergoing PCI: five-year findings from a large single-Center Cohort Study. Front Endocrinol (Lausanne). 2021;12700349. https://doi.org/10.3389/fendo.2021.700349.
Zhu P, Lao G, Chen C, Luo L, Gu J, Ran J. TSH levels within the normal range and risk of cardiovascular and all-cause mortality among individuals with diabetes. Cardiovasc Diabetol. 2022;21(1):254. https://doi.org/10.1186/s12933-022-01698-z.
Inoue K, Tsujimoto T, Saito J, Sugiyama T. Association between serum thyrotropin levels and mortality among euthyroid adults in the United States. Thyroid. 2016;26(10):1457–65. https://doi.org/10.1089/thy.2016.0156.
Alonso SP, Valdés S, Maldonado-Araque C, Lago A, Ocon P, Calle A, Castaño L, Delgado E, Menéndez E, Franch-Nadal J, Gaztambide S, Girbés J, Chaves F, Garcia-Serrano S, Garcia-Escobar E, Fernandez-García JC, Olveira G, Colomo N, Rojo-Martínez G. Thyroid hormone resistance index and mortality in euthyroid subjects: Di@bet.es study. Eur J Endocrinol. 2021;186(1):95–103. https://doi.org/10.1530/eje-21-0640.
Cappola AR, Arnold AM, Wulczyn K, Carlson M, Robbins J, Psaty BM. Thyroid function in the euthyroid range and adverse outcomes in older adults. J Clin Endocrinol Metab. 2015;100(3):1088–96. https://doi.org/10.1210/jc.2014-3586.
Chaker L, Heeringa J, Dehghan A, Medici M, Visser WE, Baumgartner C, Hofman A, Rodondi N, Peeters RP, Franco OH. Normal thyroid function and the risk of Atrial Fibrillation: the Rotterdam Study. J Clin Endocrinol Metab. 2015;100(10):3718–24. https://doi.org/10.1210/jc.2015-2480.
Chaker L, van den Berg ME, Niemeijer MN, Franco OH, Dehghan A, Hofman A, Rijnbeek PR, Deckers JW, Eijgelsheim M, Stricker BH, Peeters RP. Thyroid function and sudden Cardiac death: a prospective Population-based Cohort Study. Circulation. 2016;134(10):713–22. https://doi.org/10.1161/circulationaha.115.020789.
Krashin E, Piekiełko-Witkowska A, Ellis M, Ashur-Fabian O. Thyroid hormones and Cancer: a Comprehensive Review of Preclinical and Clinical studies. Front Endocrinol (Lausanne). 2019;1059. https://doi.org/10.3389/fendo.2019.00059.
Mehran L, Delbari N, Amouzegar A, Hasheminia M, Tohidi M, Azizi F. Reduced sensitivity to thyroid hormone is Associated with Diabetes and Hypertension. J Clin Endocrinol Metab. 2022;107(1):167–76. https://doi.org/10.1210/clinem/dgab646.
Sun Y, Teng D, Zhao L, Shi X, Li Y, Shan Z, Teng W. Impaired sensitivity to thyroid hormones is Associated with Hyperuricemia, obesity, and Cardiovascular Disease risk in subjects with subclinical hypothyroidism. Thyroid. 2022;32(4):376–84. https://doi.org/10.1089/thy.2021.0500.
Yang Z, Duan P, Li W, Nie R, Lou X, Wang L, Wu K, Liu J, Tu P, Lai X. The correlation between thyroid hormone levels and the kidney disease progression risk in patients with type 2 diabetes. Diabetes Metab Syndr Obes. 2022;1559–67. https://doi.org/10.2147/dmso.S347862.
Liu X, Li Y, Chai Y, Zhang Y, Zhang L, Zhang H. Thyroid function and thyroid homeostasis parameters are associated with increased urinary albumin excretion in euthyroid individuals over 60 years old from NHANES. Front Endocrinol (Lausanne). 2023;141285249. https://doi.org/10.3389/fendo.2023.1285249.
Han Z, Chen L, Peng H, Zheng H, Lin Y, Peng F, Fan Y, Xie X, Yang S, Wang Z, Yuan L, Wei X, Chen H. The role of thyroid hormone in the renal immune microenvironment. Int Immunopharmacol. 2023;119110172. https://doi.org/10.1016/j.intimp.2023.110172.
Acknowledgements
We want to acknowledge all participants of this study and the support provided by the Jiangsu University.
Funding
This study was funded by the Science and Technology Project of Changzhou Health Commission (WZ202226) and the Young Talent Development Plan of Changzhou Health Commission (CZQM2022029).
Author information
Authors and Affiliations
Contributions
Q.Y. R.D. and Z.W. wrote the main manuscript text, H.Y. and R. X. prepared figures and tables. Y.X. and Y.Y. analyzed the data. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies involving humans were approved by the Ethics Review Board of the National Center for Health Statistics. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, Q., Dong, R., Yan, H. et al. Impaired sensitivity to thyroid hormone correlates to all-cause mortality in euthyroid individuals with chronic kidney disease. BMC Public Health 24, 2134 (2024). https://doi.org/10.1186/s12889-024-19660-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19660-x