Abstract
Background
With global climate change, the health threats of ambient high temperature have received widespread attention. However, latest spatio-temporal patterns of the non-communicable diseases (NCDs) burden attributable to high temperature have not been systematically reported. We aimed to analyze vulnerable areas and populations based on a detailed profile for the NCDs burden attributable to high temperature globally.
Methods
We obtained data from the Global Burden of Diseases (GBD) Study (2019) to describe the temporal and spatial patterns of NCDs burden attributable to high temperature globally from 1990–2019. Then we analyzed the differences by region, sex, and socio-demographic index (SDI). Finally, the age‑period‑cohort (APC) model was utilized to explore the age, period, and cohort effects of NCDs mortality caused by high temperature.
Results
In 2019, the number of deaths and Disability-adjusted life years (DALYs) from high-temperature-related NCDs was about 150,000 and 3.4 million globally, of which about 70% were in South Asia and North Africa and Middle East, and the burden was higher in men. Among 204 countries and territories, the highest age-standardized mortality rate (ASMR) and age-standardized DALY rate (ASDR) were observed in Oman and United Arab Emirates, respectively. The global burden showed an upward trend from 1990 to 2019, with an EAPC of 3.66 (95%CI: 3.14–4.18) for ASMR and 3.68 (95%CI: 3.16-4.21) for ASDR. Cardiovascular diseases were the main contributors to the global burden of high-temperature-related NCDs in 2019. The age and period effect in APC model showed an increasing trend globally. There was a significant negative correlation between SDI and both ASMR (r = -0.17) and ASDR (r = -0.20) from 1990 to 2019.
Conclusion
There was an increasing trend of the global burden of high-temperature-related NCDs. The burden was likely to be higher in males and the elderly, as well as in countries and regions with less economically and socially developed and in tropical climates. Surveillance and prevention measures should be implemented with a focus on these vulnerable areas and susceptible populations.
Similar content being viewed by others
Background
Non-communicable diseases (NCDs) are the leading cause of ill health and premature death globally, characterized by long duration of illness, high morbidity and high mortality. Globally in 2016, about 40.5 million people died from NCDs, accounting for about 70% of deaths worldwide, with more than 80% of NCDs occurring in low-and middle-income countries [1, 2]. NCDs burden has become an important global health problem, resulting in global health inequalities across the world. However, NCDs are largely preventable, and after the 2011 UN High-Level Meeting on non-communicable diseases, Member States of the WHO adopted “The reduction by a third of premature non-communicable disease mortality by 2030” as the target of Sustainable Development Goals (SDGs) [3]. Therefore, it is necessary to explore the risk factors for NCDs and develop targeted strategies to prevent NCDs and reduce the disease burden.
In recent decades, global climate change has intensified, and the fluctuation range of ambient temperature has increased significantly [4]. The World Meteorological Organization (WMO) reported in the State of the Global Climate 2023 that 2023 was the warmest year since the 174-year observational record. The global average near-surface temperature was 1.45 ± 0.12 °C above the pre-industrial average, with severe heatwaves occurring around the world [5]. Extreme weather and climate events pose a threat to the natural environment and social economy, and health problems caused by extreme heat are of increasing concern [6,7,8,9]. Substantial epidemiological evidence consistently indicated that high temperature was associated with an increased risk of many NCDs. Liu C et al. concluded that extreme heat exposure directly affects human cardiovascular health by altering thermoregulatory mechanisms [10]. A study from Augsburg, Germany, found an increasing relative risk of heat-related myocardial infarction in the population between 1987–2014 [11]. G. Brooke Anderson et al. found an average increase in chronic obstructive pulmonary disease (COPD) hospitalizations of 4.3% for every 10°F increase in average outdoor temperature in the U.S. [12]. A cross-case study in the UK reported that patients with diabetes were significantly more likely to consult their general practitioner during hot weather [13]. A study using data on specific causes of cardiovascular death in 27 countries from 1979 to 2019, estimated that 1.6 deaths per 1000 stroke deaths could be attributed to extreme heat [4]. Researchers in China noted that hot weather contributes to a greater burden of hypertensive disease [14]. In addition, the increased risk of NCDs such as chronic kidney disease (CKD) and ischemic heart disease has also been found to be associated with extreme heat [15, 16]. Moreover, the frequency of extreme heat events and heat waves will continue to increase [17], which will greatly affect human life and the risk of NCDs. However, studies on the burden of disease attributable to climate change are limited to a particular disease, such as COPD or CKD, some studies have been conducted only in selected countries and regions, especially lacking in low-income countries. Others have focused only on the impact of low temperature on the burden of NCDs and lack a systematic description of the burden of high-temperature-related NCDs in a global perspective.
The Global Burden of Disease (GBD) Study (2019) published data on the attributable burden of disease for 87 risk factors at global, regional, and 204 countries and territories levels for 1990–2019, including the data on disease burden attributable to high temperature [18]. In this study, we extracted data of the deaths and DALYs for high-temperature-related NCDs in GBD 2019, aiming to comprehensively analyze the burden of NCDs and cause-specific diseases attributable to high temperature globally in 2019 and the temporal and spatial patterns during 1990–2019. Age-period-cohort (APC) modeling was used to explore the age, period, and cohort effects on NCDs mortality caused by high temperature. In addition, we summarized the burden differences by sex and SDI. Our findings may help health policy makers and researchers to identify vulnerable populations and susceptible countries and regions of high-temperature-related NCDs and to better cope with the health problems caused by climate change.
Methods
Study data
GBD 2019 is the world's most comprehensive and systematic epidemiologic database of risk factors and disease burden [19]. GBD 2019 added high temperature as a risk factor to the database for the first time and estimated the distribution of exposure and disease burden by location, sex, age and year [20]. In order to assess the burden of high-temperature-related NCDs globally in 2019 and its spatial and temporal patterns from 1990 to 2019, and to assess the differences in disease burden among populations and regions, we will use data on deaths and ASMRs, DALYs and ASDRs of NCDs attributable to high temperatures as well as SDI for secondary analyses. The GBD study divides the world into 21 regions based on geographic location and epidemiological characteristics [19, 21], and the 2019 data include all World Health Organization member states [18]. Meanwhile, the GBD team divided the 204 countries and territories into 5 SDI regions according to the SDI index, which represents the level of socioeconomic development: low SDI (< 0.46), Low-middle SDI (0.46–0.60), Middle SDI (0.61–0.69), High-middle SDI (0.70–0.81), and high SDI (> 0.81) [18, 21]. Socio-demographic index (SDI) is a composite indicator covering per capita income, years of schooling, and fertility of women under 25 years of age, which can be used to measure the position of health-related socio-demographic development in a region [18].
Definitions of high temperature exposure and NCDs
Estimates of high temperature exposure for each site in the GBD study were obtained and calculated from the European Centre for Medium-Range Weather Forecasts (ECMWF) [22]. According to GBD study, the minimum value of the average cause-specific exposure–response curves is the theoretical minimum risk exposure level (TMREL) [18]. Considering the differences in response to high temperature exposure across locations, diseases and years, the TMREL for high temperature in the GBD study was not globally consistent but was the temperature associated with the lowest risk of death for all diseases with the same etiology in the same year and location. High temperature were defined as ambient temperature above the TMREL [23]. Information of data sources on high temperature exposure is available at http://ghdx.healthata.org/gbd-2019/data-input-sources.
GBD study classified the risk factors and the causes of death or DALY into four levels [18], where NCD was at the first level, the causes of leve2 were sub-causes with level 1, containing three types of diseases: cardiovascular diseases, diabetes and kidney and chronic respiratory diseases, while the level 3 of etiology is a more detailed cause of the level 2, which contains ischemic heart disease, stroke, hypertensive heart disease, COPD, CKD and diabetes mellitus, and level 4 is the more detailed causes of level 3 [18, 22]. We mainly discussed the burden of level 1 to 3 in this study. A classification of NCDs can be found at: https://vizhub.healthdata.org/gbd-results/.
Statistical analysis
First, we used the number and age-standardized rate of deaths and DALYs to describe the burden of NCDs attributable to high temperature in 1990 and 2019, and applied the estimated Annual Percentage Change (EAPC) to assess the temporal trend from 1990 to 2019. Previous studies have used the EAPC to describe trends of age-standardized rate (ASR) in a specific time period [24, 25]. The natural logarithm of ASR can be fitted to a regression line using the model \(\mathit{ln}\left(ASR\right)=\alpha +\beta x+\varepsilon\), where \(x\) was the calendar year, \(EAPC=100*\left(\text{exp}\left(\beta \right)-1\right)\), and the 95% confidence interval (CI) for EAPC can be calculated from the regression model. The temporal trend was considered to be in an upward trend when the EAPC and its 95% CI lower bound were both > 0, conversely, it was considered to be in a downward trend when both the EAPC and the upper bound of its 95% CI were < 0. Otherwise, the ASR could be considered stable [26].
Second, based on the data of ASMR and ASDR in different countries and regions around the world in 2019, we demonstrated the burden of NCDs attributable to high temperature by using map construction. In addition, we showed differences in the burden of NCDs and cause-specific by sex, and verified the correlation of SDI with ASMR and ASDR using Pearson correlation coefficients.
Finally, in order to avoid errors caused by linear correlation (cohort = period-age), APC model was used to further explore the age, period and cohort effect trends of NCDs mortality caused by high temperature. APC model can capture the information of age, period and cohort contained in mortality trends, and it has been widely used in previous studies to estimate the impact of net age, period and cohort on disease morbidity and mortality [27]. Age effect can reflect changes in disease mortality with age. Period effect can reveal the influence of various events on the change of disease mortality over time, such as advances in disease diagnostic technology or the implementation of effective treatments. Cohort effect refers to the differences in disease mortality among generations due to the exposure levels of risk factors or changes in behavior and lifestyle [28]. APC model is a log-linear model based on the Poisson distribution as follows:
\(\lambda \left(a\cdot p\right)\) represents the age-specific ratio for age \(a\) and period \(p\); \(f\left(a\right)\), \(g\left(P\right)\), and \(h\left(c\right)\) refer to the age, period, and cohort effects of the observation unit respectively; \(\mu\) and \(\varepsilon\) refer to the intercept and random error [29]. This study analyzed the age, period and cohort effects of disease burden using the APC Web Tool developed by the US National Cancer Institute website (https://analysistools.cancer.gov/apc/). Considering the usage requirements of the APC Web Tool and the data characteristics of NCDs attributable to high temperature in GBD 2019, the age groups used to reflect the age effect in the APC model were 15 consecutive 5-year age groups ranging from 20–24 to 90–94 years, corresponding to birth cohorts ranging from 1900–1904 to 1995–1999, as well as 6 consecutive 5-year period groups from 1990–1994 to 2015–2019. All statistical analyses were performed using R software (version 4.2.3) except for the analysis of the APC model. p < 0.05 was considered statistically significant.
Results
NCDs burden attributable to high temperature from 1990 to 2019 globally
As shown in Table 1, there were 151312.45 (95% UI: 79214.61, 224816.6) deaths and 3400461.56 (95% UI: 1762998.32, 5033020.83) DALYs of NCDs attributable to high temperature globally in 2019. The global ASMR increased from 0.56 (95% UI: -2.72, 1.84) in 1990 to 1.9 (95% UI: 0.99, 2.83) in 2019, with an EAPC of 3.66 (95% CI: 3.14, 4.18), whereas the ASDR increased from 11.87 in 1990 (95% UI: -65.96, 40.1) to 41.45 (95% UI: 21.49, 61.36) in 2019 and the EAPC was 3.68 (95% CI: 3.16, 4.21) (Table 1). Both the EAPC for ASMR and ASDR and their lower bound of the 95% CI were > 0, indicating that the global ASMR and ASDR of NCDs caused by high temperature showed an increasing trend from 1990 to 2019.
In addition, the burden of high-temperature-related NCDs varied between sexes. Global ASMR and ASDR in 2019 were 1.61 (95% UI: 0.87–2.41) and 34.53 (95% UI: 18.50–50.79) for females, respectively, whereas males were higher than females at 2.25 (95% UI: 1.13–3.40) and 49.12 (95%UI: 22.20–74.57) (Table 1). Quantitatively, the number of deaths from NCDs attributable to high temperature increased more than sixfold over the 30 years from 1990 to 2019 globally, with a nearly sixfold increase in females, compared with a faster increase of nearly sevenfold in males. The number of DALYs increased nearly sixfold, with a more than fivefold increase in females and an approximately 6.5-fold increase in males. From 1990 and 2019, the EAPC for ASMR was higher in males (3.64, 95%CI: 3.09–4.19) than in females (3.58, 95%CI: 3.09–4.06), and similarly, the EAPC of ASDR in males (3.8, 95%CI: 3.24–4.37) was also higher than that of females (3.46, 95%CI: 2.97–3.94), indicating that both sexes showed an increasing trend in ASR and the increase was faster in males (Table 1).
The NCDs burden attributable to high temperature varied across countries and regions. Figure 1 illustrates the spatial distribution of ASMR and ASDR in 2019. Among the 21 GBD regions in 2019, the highest ASMR of high-temperature-related NCDs was found in South Asia (7.1, 95% UI: 3.27–11.21), followed by North Africa and Middle East (4.69, 95%UI: 2.13–7.37), while Western Europe had the lowest ASMR (0.04, 95%UI: 0.02–0.08) (Table 1). South Asia also had the highest ASDR (141.22,95% UI: 68.05–218.26) and Western Europe also had the lowest (0.58, 95% UI: 0.24–1.09) among 21 GBD regions in 2019 (Table 1). From 1990 to 2019, the ASMR and ASDR among 21 GBD regions around the world, except in Australasia and high-income North America, showed an increasing trend, especially in Eastern Sub-Saharan Africa, which has the fastest rise, with EAPC of 28.31 (95% CI: 18.14–39.36) for ASMR and 24.8 (95% CI: 14.59–35.91) for ASDR (Table 1). ASMR and ASDR declined slightly in Australia with an EAPC of -2.08 (95% CI:-2.51–1.65) for ASMR and -2.43 (95% CI:-2.88–1.98) for ASDR, as did ASMR in High-income North America (Table 1). In 2019, among the 204 countries and territories in the world, Oman had the highest ASMR of NCDs due to high temperature in 2019 (27.79, 95%UI: 11.02–40.77), followed by Qatar (26.78, 95%UI: 10.99- 43.43) and United Arab Emirates (26.32, 95%UI: 12.78–39.51) (Table S1; Fig. 1). The top of three countries with the highest ASDR were United Arab Emirates (483.64, 95%UI: 231.83–739.71), Oman (453.03, 95%UI: 190.67–668.63) and Mali (373.46, 95%UI: 202.09–551.94) (Table 1). Among the five SDI regions, Low-middle SDI regions had the highest ASMR (5.39, 95%UI: 2.19–8.4) and ASDR (107.73, 95%UI: 46.48–163.06), followed by Low SDI regions in 2019; ASMR and ASDR were lowest in High SDI regions with 0.33 (95% UI: 0.18–0.48) and 8.22 (95% UI: 4.55–12.11). The fastest growth in disease burden during the period 1990–2019 was in Low SDI regions, ASMR and ASDR were the fastest growing in the Low SDI regions over the period 1990–2019, with EAPC for ASMR and ASDR of 5.55 (95%CI: 4.68–6.43) and 6.49 (95%CI: 5.39–7.6), respectively (Table 1).
Impact of high temperature on cause‑specific NCDs by sex
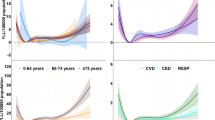
As shown in Fig. 2, among the level 2 cause-specific diseases attributable to high temperature globally in 2019, cardiovascular diseases had the highest ASMR (1.17,95% UI: 0.13–1.98) and ASDR (25.59, 95% UI: 2.07–44.17), and stroke had the highest ASMR (0.60, 95% UI: 0.07–1.30) and ASDR (13.31, 95% UI: 1.40–28.97) among the NCDs of level 3, which was one of the specific causes of cardiovascular diseases (Table 2). ASMR and ASDR of NCDs for both level 2 and level 3 cause-specific diseases show an upward trend from 1990 to 2019. In terms of mortality, the disease with the highest EAPC was hypertensive heart disease (30.17, 95% CI: 17.97–43.63), and comparatively, stroke had the lowest EAPC for ASMR (0.97, 95% CI: 0.63–1.31) (Table 2). Similarly, the fastest and slowest rise in DALY rates was also seen in hypertensive heart disease and stroke, with EAPCs of 32.26, (95% CI: 17.82–48.48) and 0.91 (95% CI: 0.59–1.24) for ASDR, respectively (Table 2). In terms of sex, among these 9 cause-specific NCDs, ASMR and ASDR were higher in males than females, except for hypertensive heart disease (Fig. 2; Table S2).
APC model analysis of the NCDs mortality rate attributable to high temperature from 1990 to 2019
We applied APC model to estimate the age, period, and cohort effects on mortality of NCDs attributable to high temperature globally and in 5 SDI regions (Fig. 3; Table S3-S5). Age effect of high-temperature-related NCDs globally showed a rising trend year by year from 1990 to 2019, indicating that the mortality rate increased with age (Fig. 3A). Notably, at age 30 and beyond, males had a higher mortality rate than females, with an increasing gap. Similarly, the trend of increasing mortality rate with age was observed in all SDI regions, with the slowest increase in the high SDI regions (Fig. 3D). Mortality rate of 70 and the later age groups in low SDI regions increased at the fastest rate of all SDI regions, from 74.35 (95% CI: 71.19–77.65) in the 75–79 age group to 468.22(95% CI: 433.24–506.03) in the 90–94 age group (Fig. 3D; Table S3).
From 1990 to 2019, the period effect of NCDs mortality attributable to high temperature showed a yearly increasing trend, with the period risk ratio (RR) rising from 0.56 (95% CI: 0.54–0.57) in 1990–1994 to 1.52 (95% CI: 1.50–1.55) in 2015–2019 (Fig. 3; Table S4). Using the period of 2000–2004 as the control group, the period effect of male mortality was slightly lower than that of females before that period, while the risk of death was higher in males after then. The mortality rate in all SDI regions showed a trend of increasing with year.
In terms of cohort effect, mortality of high-temperature-related NCDs showed an upward trend globally and in other SDI regions except for high SDI regions, which showed a decline in 1985–1990 (Fig. 3C; F). Globally, the death risk was lowest in the cohort of 1900–1904, with a RR of 0.21 (95%CI: 0.29–0.99) (Fig. 3; Table S5). The risk of death was highest in the cohort of 1995–1999, with a RR of 6.88 (95% CI: 4.43–5.33). The males and females born before 1955 had a similar risk of death, but the risk in males born in 1955 and later was higher than in females. The lowest risk of death was found among those born in 1905–1909 in the low SDI regions, however, after 1950, low SDI regions became the areas with the highest RR.
Influence of sociodemographic transitions on ASRs of NCDs attributable to high temperature
Figure 4 shows the trends of ASMR and ASDR of NCDs attributable to high temperature in 5 SDI regions from 1990 to 2019. Overall, the trends of the curves fitted to SDI and ASMR and the curves fitted to SDI and ASDR were essentially consistent, with nonlinear correlations. Significant correlations were found between the SDI and both ASMR (r = -0.17, P < 0.001) and ASDR (r = -0.20, P < 0.001) (Fig. 4). ASMR and ASDR showed an increasing trend until the SDI value was about 0.4, then ASMR and ASDR peak at the SDI value near 0.4, and leveled off after the SDI value was about 0.7. The maximum values of both ASMR and ASDR were in the low-middle SDI regions, while the minimum values were all found in the high SDI regions (Fig. 4). Among the different GBD regions, except for Australasia and High-income North America, ASMR showed an upward trend. ASDR also increased in all regions apart from Australasia. South Asia had the greatest changes in both ASMR and ASDR, while the changes of ASMR in High-income Asia Pacific and ASDR in High-income North America were the smallest.
Discussion
This study comprehensively analyzed the burden and temporal trends of NCDs caused by high temperature from 1990 to 2019 at the global, regions and countries levels, compared the differences in disease burden by sex, validated the relationship between SDI and ASMR, ASDR, and further analyzed the effects of age, period, and cohort on the mortality rate of high-temperature-related NCDs using APC model. We aimed to highlight the significant burden of NCDs attributable to high temperature globally, inform research priorities for environmental health researchers and provide a reference for public health policy makers in identifying vulnerable populations and areas in need of early prevention.
In recent years, the burden of NCDs caused by global high temperature has been considerable, with ASMR of 1.9% and ASDR of 41.45% in 2019. During the 30-year period 1990 to 2019, furthermore, the global number of deaths of NCDs attributable to high temperature increased by more than 6 times, and the increasing trend in DALY was also evident, which has been reported in previous studies [30,31,32]. Nevertheless, the burden of disease varied somewhat across regions and countries and in different age groups and sexes. In the context of global warming and the progressive increase in the burden of NCDs attributable to high temperature, understanding the spatiotemporal and population differences is important for developing extreme heat adaptation plan and proposing targeted strategies for the early surveillance, prevention and treatment of NCDs.
At the regional level, we found that South Asia and North Africa and Middle East were the regions with the highest burden of high-temperature-related NCDs in 2019, and ASMR and ASDR were rising fastest in Eastern Sub-Saharan Africa. Conversely, Western Europe had the lowest disease burden among the 21 GBD regions. The drivers of geographic variation in the burden of high-temperature-related disease are complex and may be directly attributable to different climatic zones. The climate of South Asia and North Africa and Middle East are predominantly tropical, with high temperatures throughout the year. Countries in South Asia, such as India and Pakistan, are suffering from extreme high temperature and heat wave disasters in recent years [33, 34], and extreme high temperature approaching 50 °C have been observed in North Africa on several occasions [35]. Many studies have consistently shown that extreme high temperature affects the increased risk of morbidity, exacerbation and mortality in NCDs, such as COPD [36], diabetes mellitus [17], CKD [37], ischemic heart disease [10], hypertensive heart disease [14] and stroke [38]. In addition, the burden of diseases caused by high temperature may be related to factors such as the level of socio-economic development [39], the proportion of the elderly [40] and the rate of population growth [35] in regions and countries. Therefore, the rapid increase in the burden of NCDs attributable to high temperature in Eastern Sub-Saharan Africa may be related to its continuous population growth [41]. Oman and Qatar, which are located in the west of Asia, have the highest ASMR among the 204 countries and territories, and the highest ASDR was in United Arab Emirates, followed by Oman. These 3 countries were in the regions with the highest disease burden as mentioned above. However, there are few records on the diseases burden attributable to high temperature in these vulnerable countries and regions [42], let alone studies on high-temperature-related NCDs. We expect more studies will to be reported in these areas, so that we can learn about their climate and demographic dynamics, provide early warning and take effective heat adaptation measures in advance. For example, building shading facilities as needed, and adding emergency access in hospitals for heat-related illnesses when heat waves persist.
The results showed a negative correlation between SDI and the burden of NCDs attributable to high temperature, suggesting that areas with a high SDI had a lower burden of disease. Some studies indicated that people living in high-temperature environments have a higher heat stress tolerance compared to people living in suitable temperature for long periods of time [43]. However, our findings revealed that regions and countries located in areas with perennially high temperatures instead have the highest disease burden, such as South Asia and North Africa and Middle East, whose SDI values were not high. Therefore, we speculate that thermal adaptation had a limited role in reducing the burden of high-temperature-related NCDs, and factors such as economic and social development of the regions can greatly affect the NCDs burden caused by high temperature, which has been reported in previous studies [39, 44, 45]. Countries and territories with high levels of economic development have better healthcare and prevention systems for NCDs, which can largely reduce the incidence and mortality of high-temperature-related illnesses. In addition, government employees, the proportion of manual laborers, and the number of low-income elderly people were also socio-economic reasons affecting the NCDs burden attributable to high temperature [46]. With regard to cooling strategies, the use of air conditioning is undoubtedly the most widely used method in the world. However, the use of air-conditioning not only weakens people's thermal perception and adaptation functions, but also has the disadvantage of environmental unsustainability. For vulnerable people in economically underdeveloped areas, it is unaffordable to purchase air conditioners and pay for their electricity [47]. More attention and efforts are therefore urgent to reduce the NCDs burden attributable to high temperature in countries that are in hot climatic zones and less developed economically. We believe that economic and health technical assistance to these regions can be used to achieve short-term reduction of the rapidly increasing disease burden, and that long-term heat adaptation programs may need to be primarily based on sustainable individual cooling strategies and governmental early warning and public health interventions.
Further analyzing the burden of cause-specific NCDs attributable to high temperature and their differences by sex, we found that the burden of disease for each of the six level 3 of NCDs showed an upward trend from 1990 to 2019, and cardiovascular disease (including ischemic heart disease, stroke, and hypertensive heart disease) were the leading cause of high-temperature-related NCDs globally, with the greatest burden from stroke. Notably, ASMR and ASDR were rising fastest in hypertensive heart disease, suggesting that timely measures should be taken to reduce the risk of death from it. Current studies have confirmed that extreme high temperature would seriously damage cardiovascular health [10, 48], and heat-mediated dehydration and heat stress were direct causes of cardiovascular damage [10, 49], while ambient temperature can indirectly influence cardiovascular disease mortality by affecting physical activity [50]. Moreover, health damage was found to be greater in male, which was consistent with the results of previous studies [32, 51]. In the 30 years from 1990 to 2019, the number of deaths and DALYs, as well as ASMR and ASDR, increased more rapidly in males than in females. In 2019, except for hypertensive heart disease, males had higher NCDs burden caused by high temperature than females in the all level 3 diseases. The reason may be that a higher proportion of male workers were engaged in jobs such as construction, open pit mining and outdoor farm work in hot weather [52,53,54]. Therefore, public health interventions should be implemented with attention to the relationship between the pattern and extent of heat exposure and the incidence of non-communicable diseases among men. Additionally, in order to reduce the damage to health caused by hot work, it is necessary to provide hot-workers with cooling guidance and allowances.
First, the age effect in the APC model showed that the global mortality rate of NCDs attributable to high temperature increased with age, especially after the age group of 65–69 years. The incidence and mortality of NCDs in the elderly were much higher than that in young people because of organ aging and physiological function decline [55]; And the elderly were more sensitive to high temperature [56]; In addition, a study found that patients suffering from NCDs such as ischemic heart disease, diabetes mellitus, stroke, and hypertension were susceptible to extreme temperature [57], coupled with the increasing proportion of aging population in the world, the elderly were at higher risk of NCDs death due to high temperature. We found that mortality increased most slowly with age in high SDI regions, while those in low SDI regions had the fastest rate in the age group after 70–74 years. In addition to the special characteristics of the elderly in terms of physiological functioning, they are also disadvantaged in terms of access to economic and social resources related to heat adaptation [58]. Unhealthy lifestyle and inadequate health resources may be important contributors to the higher burden among older adults in low SDI regions [59]. Consequently, it is necessary to develop health management plans for older adults in hot weather at the community level, such as comprehensive monitoring of potential health risk factors, assessment of the ability to adapt to high temperatures, health education and NCDs intervention, and the establishment of public cooling places for the elderly [56]. Second, the results indicated that the period effect of NCDs mortality attributable to high temperature showed an increasing trend year by year globally. The technology of diagnosis and etiological determination of NCDs had become more mature, and the registration and reporting of vital health data had become timely over time, which may also explain the upward trend in period effect. Third, during the period of 1990 to 2019, the upward trend in cohort effect suggested that the global death risk of high-temperature-related NCDs increased the further back in the birth year one went.
There are several limitations in this study. Data bias was inevitable even though GBD 2019 had explicitly corrected the data by using methods such as standardization and improved modelling. First, GBD 2019 did not estimate high-temperature exposure using a method that takes potential synergies between relative risk factors into account. In addition, the patterns of data availability for high temperature exposure measurements were inconsistent across locations and time [18]. Second, the determination of the cause of death is complex, so bias in the attribution of death may occur. Regions with poor medical diagnosis technology are more likely to have data errors. Third, the limited number of specific diseases of NCDs included in GBD 2019 and data from areas with low healthcare accessibility may have led to an underestimation of NCDs detection rates [60]. These potential data sources and biases may affect the accuracy of the study results. Fourth, there are a lot of factors affecting NCDs, however, we only examined the effect of high temperature due to the limitations of the GBD 2019 data. Therefore, in the future, consideration should be given to using more comprehensive and detailed data to include factors such as air pollution, ethnicity, and behavioral lifestyle as control variables in the study. Moreover, in GBD 2019, people aged 95 years or older were combined into one age group, which did not meet the requirements of the framework in APC Web Tool, and the death number of some cause-specific NCD in people younger than 20 years was small. Therefore, the age group we selected was 20–24 to 90–94 years old, 15 consecutive age groups of 5 years old. In addition, the types of NCDs included in our study may not be comprehensive enough due to the limited number of specific diseases of NCDs included in GBD 2019.
Conclusions
Overall, the burden of NCDs attributable to high temperature had been increasing from 1990 to 2019. The disease burden was higher in males and the elderly and varies markedly across regions and countries. We found that the driving factors of regional differences may be climatic zones in which they are located, socio-economic development level and demographic structure after analyzing. Therefore, it is significant to focus on the prevention and treatment of NCDs caused by high temperature in males and the elderly, as well as to increase reporting and research in tropical and less developed regions. In addition, a range of climate change adaptation strategies, monitoring and early warning of extreme heat events, and policies targeting vulnerable populations and areas are needed to reduce the burden of NCDs attributable to high temperature.
Availability of data and materials
The database used during the current study is available in http://ghdx.healthdata.org/gbd-results-tool.
Abbreviations
- NCDs:
-
Non-communicable diseases
- GBD:
-
The Global Burden of Diseases
- EAPC:
-
Estimated annual percentage change
- SDI:
-
Socio-demographic index
- APC:
-
Age-period-cohort
- ASMR:
-
Age-standardized mortality rate
- DALY:
-
Disability-adjusted life year
- ASDR:
-
Age-standardized DALY rate
- COPD:
-
Chronic obstructive pulmonary disease
- CKD:
-
Chronic kidney diseases
- TMREL:
-
Theoretical minimum risk exposure level
- ASR:
-
Age-standardized rate
- CI:
-
Confident interval
- UI:
-
Uncertainty interval
- RR:
-
Risk ratio
References
Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, Riley LM, Dain K, Kengne AP, Chalkidou KJ. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392(10152):1072–88.
Niessen LW, Mohan D, Akuoku JK. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda (vol 391, pg 2036, 2018). Lancet. 2019;393(10175):986–986.
Martinez R, Lloyd-Sherlock P, Soliz P, Ebrahim S, Vega E, Ordunez P, McKee M. Trends in premature avertable mortality from non-communicable diseases for 195 countries and territories, 1990–2017: a population-based study. Lancet Global Health. 2020;8(4):E511–23.
Alahmad B, Khraishah H, Roye D, Vicedo-Cabrera AM, Guo Y, Papatheodorou SI, Achilleos S, Acquaotta F, Armstrong B, Bell ML, et al. Associations between extreme temperatures and cardiovascular cause-specific mortality: results from 27 countries. Circulation. 2023;147(1):35–46.
WMO. State of the Global Climate 2023 [19 March 2024]. [https://wmo.int/publication-series/state-of-global-climate-2023].
Gronlund CJ, Sullivan KP, Kefelegn Y, Cameron L, O’Neill MS. Climate change and temperature extremes: a review of heat- and cold- related morbidity and mortality concerns of municipalities. Maturitas. 2018;114:54–9.
Amegah AK, Rezza G, Jaakkola JJK. Temperature-related morbidity and mortality in Sub-Saharan Africa: a systematic review of the empirical evidence. Environ Int. 2016;91:133–49.
Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305(5686):994–7.
McMichael AJ, Woodruff RE, Hales SJTL. Climate change and human health: present and future risks. Lancet. 2006;367(9513):859–69.
Liu C, Yavar Z, Sun Q. Cardiovascular response to thermoregulatory challenges. Am J Physiol Heart Circ Physiol. 2015;309(11):H1793–812.
Chen K, Breitner S, Wolf K, Hampel R, Meisinger C, Heier M, von Scheidt W, Kuch B, Peters A, Schneider A, et al. Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987–2014. Eur Heart J. 2019;40(20):1600–8.
Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD. Heat-related emergency hospitalizations for respiratory diseases in the Medicare population. Am J Respir Crit Care Med. 2013;187(10):1098–103.
Hajat S, Haines A, Sarran C, Sharma A, Bates C, Fleming LE. The effect of ambient temperature on type-2-diabetes: case-crossover analysis of 4+million GP consultations across England. Environ Health. 2017;16:73.
Pan R, Zheng H, Ding Z, Xu Z, Ho HC, Hossain MZ, Huang C, Yi W, Song J, Cheng J, et al. Attributing hypertensive life expectancy loss to ambient heat exposure: a multicenter study in eastern China. Environ Res. 2022;208:112726.
Barraclough KA, Blashki GA, Holt SG, Agar JWM. Climate change and kidney disease-threats and opportunities. Kidney Int. 2017;92(3):526–30.
Lin Y-K, Zafirah Y, Ke M-T, Andhikaputra G, Wang Y-C. The effects of extreme temperatures on emergency room visits-a population-based analysis by age, sex, and comorbidity. Int J Biometeorol. 2021;65(12):2087–98.
Vallianou NG, Geladari EV, Kounatidis D, Geladari CV, Stratigou T, Dourakis SP, Andreadis EA, Dalamaga M. Diabetes mellitus in the era of climate change. Diabetes Metab. 2021;47(4):101205.
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49.
Murray CJL, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, Naghavi M, Salomon JA, Shibuya K, Vos T, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380(9859):2063–6.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58.
Vos T. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 (vol 396, pg 1204, 2020). Lancet. 2020;396(10262):1562–1562.
Song J, Qin W, Pan R, Yi W, Song S, Cheng J, Su H. A global comprehensive analysis of ambient low temperature and non-communicable diseases burden during 1990–2019. Environ Sci Pollut Res. 2022;29(44):66136–47.
Cui Y, Yang W, Shuai J, Ma Y, Yan Y. High, low, and non-optimum temperatures exposure on road injuries in a changing climate: a secondary analysis based on the Global Burden of Disease Study 2019. Environ Sci Pollut Res. 2023;30(4):11012–24.
Zhang T, Yin X, Chen H, Li Y, Chen J, Yang X. Global magnitude and temporal trends of idiopathic developmental intellectual disability attributable to lead exposure from 1990 to 2019: results from Global Burden of Disease Study. Sci Total Environ. 2022;834:155366.
Yang X, Zhang T, Zhang X, Chu C, Sang S. Global burden of lung cancer attributable to ambient fine particulate matter pollution in 204 countries and territories, 1990–2019. Environ Res. 2022;204:112023.
Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, Jin L, Zhang T, Chen X. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–83.
Wang Z, Hu S, Sang S, Luo L, Yu C. Age-period-cohort analysis of stroke mortality in China: data from the Global Burden of Disease Study 2013. Stroke. 2017;48(2):271–5.
Wu X, Zhu B, Xu S, Bi Y, Liu Y, Shi J. A cross country comparison for the burden of cardiovascular disease attributable to tobacco exposure in China, Japan, USA and world. BMC Public Health. 2020;20(1):888.
Bai J, Cui J, Yu C. Burden of chronic obstructive pulmonary disease attributable to non-optimal temperature from 1990 to 2019: a systematic analysis from the Global Burden of Disease Study 2019. Environ Sci Pollut Res Int. 2023;30(26):68836–47.
Faurie C, Varghese BM, Liu J, Bi P. Association between high temperature and heatwaves with heat-related illnesses: a systematic review and meta-analysis. Sci Total Environ. 2022;852:158332.
Aboubakri O, Khanjani N, Jahani Y, Bakhtiari B, Mesgari E. Projection of mortality attributed to heat and cold; the impact of climate change in a dry region of Iran, Kerman. Sci Total Environ. 2020;728:138700.
Ban J, Xu D, He MZ, Sun Q, Chen C, Wang W, Zhu P, Li T. The effect of high temperature on cause-specific mortality: a multi-county analysis in China. Environ Int. 2017;106:19–26.
Jain Y, Jain R. India and Pakistan emerge as early victims of extreme heat conditions due to climate injustice. Bmj-Br Med J. 2022;377:o1207.
Shepherd A. Record breaking heat hits India and Pakistan. Bmj-Br Med J. 2022;377:o1293.
Iyakaremye V, Zeng G, Yang X, Zhang G, Ullah I, Gahigi A, Vuguziga F, Asfaw TG, Ayugi B. Increased high-temperature extremes and associated population exposure in Africa by the mid-21st century. Sci Total Environ. 2021;790:148162.
Zhao Q, Li S, Zanotti Stagliorio Coelho MdS, Nascimento Saldiva PH, Xu R, Huxley RR, Abramson MJ, Guo Y. Ambient heat and hospitalisation for COPD in Brazil: a nationwide case-crossover study. Thorax. 2019;74(11):1031–6.
Glaser J, Lemery J, Rajagopalan B, Diaz HF, Garcia-Trabanino R, Taduri G, Madero M, Amarasinghe M, Abraham G, Anutrakulchai S, et al. Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. 2016;11(8):1472–83.
Zhang H, Sun M, Yao X, Xie Z, Zhang M. Increasing probability of record-population exposure to high temperature and related health-risks in China. Environ Res. 2023;231:116176.
Liu S, Chan EYY, Goggins WB, Huang Z. The mortality risk and socioeconomic vulnerability associated with high and low temperature in Hong Kong. Int J Environ Res Public Health. 2020;17(19):7326.
Chen K, Vicedo-Cabrera AM, Dubrow R. Projections of ambient temperature- and air pollution-related mortality burden under combined climate change and population aging scenarios: a review. Curr Environ Health Reports. 2020;7(3):243–55.
Harrington LJ, Otto FEL. Changing population dynamics and uneven temperature emergence combine to exacerbate regional exposure to heat extremes under 1.5 degrees C and 2 degrees C of warming. Environ Res Lett. 2018;13(3):034011.
Green H, Bailey J, Schwarz L, Vanos J, Ebi K, Benmarhnia T. Impact of heat on mortality and morbidity in low and middle income countries: a review of the epidemiological evidence and considerations for future research. Environ Res. 2019;171:80–91.
Hajat S, Kosatky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health. 2010;64(9):753–60.
Hong L, Yan MM, Zhang YQ, Wang K, Wang YQ, Luo SQ, Wang F. Global burden of cardiovascular disease attributable to high temperature in 204 countries and territories from 1990 to 2019. Biomed Environ Sci. 2023;36(3):222–30.
Lim Y-H, Bell ML, Kan H, Honda Y, Guo Y-LL, Kim H. Economic status and temperature-related mortality in Asia. Int J Biometeorol. 2015;59(10):1405–12.
Lin Y-K, Maharani AT, Chang F-T, Wang Y-C. Mortality and morbidity associated with ambient temperatures in Taiwan. Sci Total Environ. 2019;651:210–7.
Jay O, Capon A, Berry P, Broderick C, de Dear R, Havenith G, Honda Y, Kovats RS, Ma W, Malik A. Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet. 2021;398(10301):709–24.
Liu C, Luo B, Wang B, He L, Wu H, Hou L, Zhang K. Global spatiotemporal trends of cardiovascular diseases due to temperature in different climates and socio-demographic index regions from 1990 to 2019. Environ Sci Pollut Res. 2023;30(2):3282–92.
Cheng X, Su H. Effects of climatic temperature stress on cardiovascular diseases. Eur J Intern Med. 2010;21(3):164–7.
Mazidi M, Speakman JR. Predicted impact of increasing average ambient temperature over the coming century on mortality from cardiovascular disease and stroke in the USA. Atherosclerosis. 2020;313:1–7.
Zhai L, Ma X, Wang J, Luan G, Zhang H. Effects of ambient temperature on cardiovascular disease: a time-series analysis of 229288 deaths during 2009–2017 in Qingdao, China. Int J Environ Health Res. 2022;32(1):181–90.
Jackson LL, Rosenberg HR. Preventing heat-related illness among agricultural workers. J Agromedicine. 2010;15(3):200–15.
Li Y, Li C, Luo S, He J, Cheng Y, Jin Y. Impacts of extremely high temperature and heatwave on heatstroke in Chongqing, China. Environ Sci Pollut Res. 2017;24(9):8534–40.
Petitti DB, Harlan SL, Chowell-Puente G, Ruddell D. Occupation and environmental heat-associated deaths in Maricopa County, Arizona: a case-control study. Plos One. 2013;8(5):e62596.
Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, Zhu X, Preedy V, Lu H, Bohr VA, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24:197–205.
Zeng W, Yu M, Mai W, Zhou M, Zhou C, Xiao Y, Hou Z, Xu Y, Liu T, Hu J, et al. Age-specific disparity in life loss per death attributable to ambient temperature: a nationwide time-series study in China. Environ Res. 2022;203:111834.
Basu R, Pearson D, Malig B, Broadwin R, Green R. The effect of high ambient temperature on emergency room visits. Epidemiology. 2012;23(6):813–20.
Kohon JN, Tanaka K, Himes D, Toda E, Carder PC, Carlson B. Extreme heat vulnerability among older adults: a multilevel risk index for Portland, Oregon. Gerontologist. 2024;64(3):gnad074.
Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, Wickramasinghe K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Global Health. 2017;5(3):E277–89.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Acknowledgements
We would like to express our sincerest gratitude to all those who contributed in any way to the work of the Global Burden of Disease Study (2019).
Funding
This work was supported by the General Project of Philosophy and Social Science Planning of Guangdong Province in 2023 (grant numbers: GD23CGL09); and the National Project Cultivation Program of the School of Health Management, Southern Medical University (2022RFT005).
Author information
Authors and Affiliations
Contributions
BL and JDZ conceptualized the paper. JDZ performed the statistical analyses and drafted the manuscript. XFC, SHM and RQG performed software and method validation. RNW and YTH did data management and provided advice. YLZ and BL reviewed and edited the writing. All authors made significant intellectual contributions to multiple revisions of the draft. All authors have read and approved the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The ethical approval is not warranted for our work as the GBD data are de-identified and publicly available. A link to the raw data can be found in the data description section. All methods in this study were carried out in accordance with relevant guidelines and regulations.
Consent of publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, JD., Cheng, XF., Min, SH. et al. Burden of non-communicable diseases attributable to high temperature in a changing climate from 1990 to 2019: a global analysis. BMC Public Health 24, 2475 (2024). https://doi.org/10.1186/s12889-024-19947-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19947-z