Abstract
Background
Severe COVID-19 carries a high morbidity and mortality. Previous studies have shown an association between COVID-19 severity and SARS-CoV-2 viral load (VL). We sought to measure VL in multiple compartments (urine, plasma, lower respiratory tract) in patients admitted to the intensive care unit (ICU) with severe COVID-19 pneumonia and correlate with clinical outcomes.
Methods
Plasma, urine, and endotracheal aspirate (ETA) samples were obtained on days 1, 3, 7, 14, and 21 from subjects admitted to the ICU with severe COVID-19. VL was measured via reverse transcriptase polymerase chain reaction. Clinical data was collected from the electronic health record. Grouped comparisons were performed using Student’s t-test or 1-way ANOVA. Linear regression was used to correlate VL from different compartments collected at the same time. Logistic regression was performed to model ventilator-freedom at 28 days as a function of peak plasma VL.
Results
We enrolled 57 subjects with severe COVID-19 and measured VL in plasma (n = 57), urine (n = 25), and ETA (n = 34). Ventilator-associated pneumonia developed in 63% of subjects. 49% of subjects were viremic on study day 1. VL in plasma and ETA both significantly decreased by day 14 (P < 0.05), and the two were weakly correlated on study day 1 (P = 0.0037, r2 = 0.2343) and on all study days (P < 0.001, r2 = 0.2211). VL were not detected in urine. While no associations were observed with peak ETA VL, subjects with higher peak plasma VL experienced a greater number of respiratory complications, including ventilator-associated pneumonia and fewer ventilator-free and hospital-free days. There was no association between VL in either plasma or ETA and mortality. In viremic patients, plasma VL was significantly lower in subjects that were ICU-free and ventilator-free (P < 0.05), with trends noted for hospital-freedom, ventilator-associated pneumonia, and survival to discharge (P < 0.1). By logistic regression, plasma VL was inversely associated with ventilator-freedom at 28 days (odds ratio 0.14, 95% confidence interval 0.02–0.50).
Conclusions
Elevated SARS-CoV-2 VL in the plasma but not in the lower respiratory tract is a novel biomarker in severe COVID-19 for respiratory complications.
Similar content being viewed by others
Background
COVID-19 due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can cause acute respiratory distress syndrome (ARDS), characterized by significant inflammation in the lungs that often requires intensive care. Prior research indicates that the amount of virus in the body (i.e., viral load) is linked to the severity of the illness. For instance, higher viral load in the upper airways of non-hospitalized patients with COVID-19 is associated with higher symptom burden [1,2,3]. In hospitalized patients, higher viral load in the bloodstream is associated with higher severity of illness, need for mechanical ventilation, and death [4,5,6].
The majority of studies have measured VL in the upper airways, and few have studied VL in the lower airways [6, 7]. Our objective of this observational study was to measure VL in three compartments, the lower airways (endotracheal aspirate), urine, and plasma in patients admitted to the intensive care unit (ICU) with severe COVID-19 and correlate with respiratory complications such as ventilator-dependence and ventilator-associated pneumonia. We hypothesized that higher VL in both plasma and the lower respiratory tract would directly correlate with increased rates of respiratory complications.
Methods
Enrollment
The Duke University COVID-19 Intensive Care Unit Biorepository is an observational cohort study of critically ill subjects with severe COVID-19. Subjects were considered eligible for the study that were positive for SARS-CoV-2 by nasopharyngeal swab reverse transcriptase polymerase chain reaction (RT-PCR), ages 18 years or older, and admitted to the ICU. To minimize selection bias, Spanish language consent was provided for Spanish-only speaking subjects. Exclusion criteria included enrollment in blood conservation program or refusal of blood transfusion (to minimize the potential risk of anemia associated with blood collection for research purposes); non-English or non-Spanish speaking; and no ability to provide consent or no designated legally authorized representative to provide consent on the subject’s behalf.
Data collection
Between 2020 and 2021, biological samples collected included citrated whole blood, endotracheal aspirate obtained via inline suction trap, and urine on study days 1, 3, 7, 14, and 21. Citrated whole blood was separated by centrifugation into plasma. Samples were stored at -80 °C until analysis. SARS-CoV-2 VL were measured in plasma, endotracheal aspirate, and urine supernatant by RT-PCR. Clinical data was captured from the electronic medical record, including subject demographics, comorbidities, treatments, complications, and survival. Subjects were followed for 90 days or until death.
Ventilator-associated Pneumonia Definition
Ventilator-associated pneumonia (VAP) was defined based on the IDSA/ATS guidelines [8] as the presence of a new lung infiltrate occurring more than 48 h after intubation with signs of infection such as fever (temperature ≥ 38.0 C), purulent secretions, leukocytosis (white blood cell count > 9.8 × 109/L), or decline in oxygenation or ventilation (increase above baseline of respiratory rate, tidal volume, inspiratory pressure, positive-end expiratory pressure, or fraction of inspired oxygen).
Outcomes of interest
The primary outcomes of interest assessed in all enrolled subjects were viral RNA levels (copies/ml) in each compartment, correlation of plasma VL and endotracheal aspirate (ETA) VL, and association of plasma and ETA VL with ICU-related outcomes: ventilator-free days, ventilator-associated pneumonia, hospital-free days, and survival to hospital discharge. The secondary outcomes assessed in only those subjects with detectable VL were ICU-free days, ventilator-associated pneumonia, ventilator-free days, hospital-free days, survival to hospital discharge, and 90-day survival.
Statistical analysis
RNA data were log transformed prior to analysis. Grouped data are shown as count (percentage), mean with standard deviation, or median with interquartile range (Q1, Q3). All statistical analyses were performed using Graphpad Prism. Peak viral load (Log10 RNA copies/ml) was defined as the maximal viral load measured for a given patient at any time point and was used to correlate with clinical outcomes: Between-group comparisons were made using the Student’s t-test with Welch’s correction (for two groups) or 1-way ANOVA with Tukey’s post-hoc test (for three or more groups). Simple linear regression was performed using paired plasma and ETA samples collected on the same study days in the same patients. Logistic regression was performed to model ventilator-freedom at 28 days (a composite of death and ventilator-dependence) as a function of peak plasma VL in subjects with detectable viremia. P-values of < 0.05 were accepted as statistically significant and trends were noted for P < 0.1.
Results
Fifty-seven subjects were enrolled in this study. Median (Q1, Q3) age was 59 (51, 67) years, 65% of subjects were non-White, and 32% (n = 18) were female (Table 1 and Supplemental Table 1). The most common comorbidities were obesity (n = 34, 60%), diabetes mellitus (n = 25, 44%), and chronic lung disease (n = 15, 26%). Fifty-two subjects (91%) required mechanical ventilation. Median (Q1, Q3) length of hospital stay was 26 (13, 46) days. Ventilator-associated pneumonia occurred in 36 subjects (63%) (Supplemental Table 2). Twenty-two (38%) subjects died prior to hospital discharge.
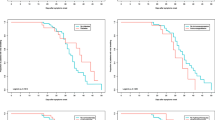
SARS-CoV-2 was not detectable in urine of any subject at any time point, whereas 49% of subjects (n = 27) were viremic on study day 1. Plasma and ETA viral loads (VL) are shown by study day (Fig. 1A-B) and by hospital day (Fig. 1C-D) and consistently decreased over time. Thirty-six subjects had paired plasma and ETA samples collected at the same time points. Using simple linear regression, plasma VL was weakly associated with ETA VL on study day 1 (p = 0.0037, r2 = 0.2343) (Fig. 1E) as well as on all study days (p < 0.0001, r2 = 0.2211) (Fig. 1F).
Viral loads. SARS-CoV-2 viral loads (RNA copies/ml plasma) are plotted on a logarithmic scale by study day for (A) plasma and (B) endotracheal aspirate (ETA) and by hospital day for (C) plasma and (D) ETA. Plasma viral loads are plotted against endotracheal viral loads (n = 36 subjects) on study day 1 (E), and for all available study days (F), demonstrating a weakly positive correlation. Number (N) of subjects at each study day is shown below the x-axis for (A) and (B). Bars are mean and standard deviation. Abbreviations: ND, not detected
Of the 52 subjects on mechanical ventilation, 37 had sufficient respiratory secretions to collect via endotracheal suction at any study day. Of the 37 subjects with ETA, 33 had detectable VLs. There was no significant correlation between peak ETA VL and ventilator-free days, hospital-free days, incidence of VAP, or in-hospital mortality (Fig. 2A-D).
Endotracheal viral loads and clinical outcomes. Endotracheal aspirate (ETA) was obtained and measured for viral load. Thirty-seven subjects had sufficient secretions for sampling. There was no statistically significant relationship between peak ETA viral load and A) ventilator-free days, B) incidence of ventilator-associated pneumonia, C) hospital-free days, and D) in-hospital mortality. Plots show mean and standard deviations. Abbreviations: ND, not detected
In contrast, peak plasma VL was significantly higher in subjects who were not ventilator-free by day 14, not hospital-free by day 30, and who developed VAP (Fig. 3A-C). However, there was no association between plasma VL and in-hospital mortality (Fig. 3D). In secondary analyses, we investigated outcomes in the subset of subjects (n = 33) with detectable plasma VL only (Supplemental Figure). Peak plasma VL was significantly associated with ICU-freedom at 30 days and ventilator-freedom at 28 days (both P < 0.005). Trends were noted for associations with ventilator-associated pneumonia (P = 0.0585), hospital freedom at 60 days (P = 0.0642), and survival to hospital discharge (P = 0.0852). Using logistic regression, plasma VL was negatively associated with ventilator-freedom at day 28 (odds ratio 0.14, 95% CI 0.02–0.50).
Plasma viral loads and clinical outcomes. The relationship between peak plasma viral load and (A) ventilator-free days, (B) incidence of ventilator-associated pneumonia, (C) hospital-free days, and (D) in-hospital mortality. Plots show mean and standard deviations. Abbreviations: ND, not detected. *p < 0.05
Discussion
Herein we report the measurements of SARS-CoV-2 VL in three compartments, ETA, plasma, and urine, in hospitalized patients with severe COVID-19 and ARDS. While we did not detect VL in urine, we found plasma VL, but not ETA VL, is associated with more respiratory complications, including fewer ventilator-free days and higher incidence of VAP. In viremic subjects specifically, we found plasma VL was significantly associated ICU-freedom and ventilator-freedom. Our study provides further data that VL measured in plasma may be a better biomarker for risk of respiratory complications than ETA VL for COVID-19 severity in critically ill patients.
Previous studies have demonstrated an association between severity of illness in hospitalized patients and high SARS-CoV-2 plasma RNA [4, 9] or nucleocapsid antigen levels [10,11,12]. Our study is one of the few to compare plasma and the lower respiratory tract VL directly and reports the novel finding that this relationship extends to ventilator complications as well. Specifically, we found higher peak plasma VL was significantly associated with less ventilator- and hospital-freedom, and higher rates of ventilator-associated pneumonia. Ventilator-associated pneumonia following COVID-19 ARDS is more common than in non-COVID-19 ARDS [13] and is associated with an increased mortality [14,15,16]. Previously identified risk factors for VAP in COVID-19 ARDS patients specifically include prolonged ventilator-dependence, acute kidney injury, male sex, and hypertension [14], and risk factors in general include chronic lung disease, older age, and immunosuppression. Furthermore, peripheral blood SARS-CoV-2 infection of circulating immune cells [17, 18] suppresses innate and adaptive immune responses [19], which may predispose to secondary bacterial infections such as VAP. However, the association of SARS-CoV-2 viremia and VAP may be confounded by more prolonged ventilator dependence and should be confirmed in future larger studies.
The relationship between SARS-CoV-2 VL in the respiratory tract and COVID-19 severity has been inconsistent [20]: In the upper respiratory tract, some studies measuring VL from nasopharyngeal swabs found correlations with illness severity [1,2,3], or death [4,5,6], whereas others studies have found no such association [17, 21, 22]. Lower respiratory tract sampling for SARS-CoV-2 may be more reliable than the upper respiratory tract [7], but has also been inconsistent, with one study finding no increased risk of pneumonia after adjusting for multiple confounders [23] whereas other studies found an increased risk of death [4, 24]. We also found no association between lower respiratory tract viral load and clinical outcomes such as ventilator-free days, ventilator-associated pneumonia incidence, and hospital-free days. The use of cycle threshold rather than quantitative PCR to measure VL [20] and univariable analysis without adjustment for confounders [23] appear to be areas observed in other studies that can introduce error. Additionally, time to first VL measurement may also be important. For instance, Jacobs, et al. found a strong correlation between plasma VL and ETA VLs on study day 1 that weakened over time and was no longer significant by study day 10 [9]. We found a weaker correlation between plasma and ETA VLs, perhaps because of longer time to enrollment in our study (median of 1 day later than Jacobs, et al.), although we did not observe further weakening over time in our study. It is also possible that viral shedding in the respiratory tract does not correlate with infectivity, as it is unknown whether the RNA measured by PCR represents viral remnants or a live infectious pathogen, especially in critically ill patients where viral shedding in the lower respiratory tract can be protracted [6, 7]. In contrast, plasma VL do not suffer from dilution and plasma VL shedding is not as protracted, suggesting it may be a more reliable method to measure SARS-CoV-2 VL than from the respiratory tract.
Urine has been studied infrequently as a source to measure SARS-CoV-2 VL. Previous studies have found detectable VL in urine in a minority of critically ill subjects with severe COVID-19 [4, 7]. Travieso, et al. also reported detectable SARS-CoV-2 virus in a subset of critically ill subjects although extracted RNA from uroepithelial cells rather than urine supernatant [25]. In contrast, our study found no detectable SARS-CoV-2 virus in the urine supernatant of critically ill subjects. This may be because the viral loads in the urine are too low for consistent detection, or perhaps because the virus resides intracellularly within the uroepithelial cells rather than excreted in the urine. While it appears VL may be infrequently detected in the urine, urine VL do not appear to be a consistently reliable marker of COVID-19 severity.
Our study has a number of limitations. First, it is a single-center cohort study which may have limited external generalizability. However, the cohort studied was racially and ethnically diverse which strengthens its applicability. Second, ETA collection may vary between subjects because it is dependent on the amount of secretions available; a bronchoalveolar lavage might be more sensitive for lower respiratory tract viral load, although could also suffer from inconsistent collection method and dilution. Third, our sample size is small and therefore subject to bias. Our findings should be confirmed in a larger multicenter study. Fourth, there may be inherent variability between subjects in the time from symptom onset to enrollment in the study, which could affect viral load levels. Finally, all of the samples analyzed in our study were collected prior to the Omicron waves and may not be reflective of the current Covid-19 landscape.
Conclusions
In critically ill patients admitted to the ICU with COVID-19 respiratory failure, elevated plasma viral load but not ETA viral load was associated with increased days on mechanical ventilation, incidence of ventilator-associated pneumonia, and increased hospital length of stay. Plasma VL may be a more reliable and consistent method than respiratory VL to gauge risk of respiratory complications in severe COVID-19 pneumonia.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Duke University.
Abbreviations
- ANOVA:
-
Analysis of variance
- ARDS:
-
Acute respiratory distress syndrome
- COVID-19:
-
Coronavirus disease 2019
- ETA:
-
Endotracheal aspirate
- ICU:
-
Intensive care unit
- ml:
-
milliliter
- Q1:
-
Quartile 1
- Q3:
-
Quartile 3
- RNA:
-
Ribonucleic acid
- RT-PCR:
-
Reverse transcriptase-polymerase chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- VAP:
-
Ventilator-associated pneumonia
- VL:
-
Viral load
References
Puchinger K, Castelletti N, Rubio-Acero R, Geldmacher C, Eser TM, Deak F, et al. The interplay of viral loads, clinical presentation, and serological responses in SARS-CoV-2 - results from a prospective cohort of outpatient COVID-19 cases. Virology. 2022;569:37–43.
Knudtzen FC, Jensen TG, Lindvig SO, Rasmussen LD, Madsen LW, Hoegh SV, et al. SARS-CoV-2 viral load as a predictor for disease severity in outpatients and hospitalised patients with COVID-19: a prospective cohort study. PLoS ONE. 2021;16(10):e0258421.
Stankiewicz Karita HC, Dong TQ, Johnston C, Neuzil KM, Paasche-Orlow MK, Kissinger PJ, et al. Trajectory of viral RNA load among persons with Incident SARS-CoV-2 G614 infection (Wuhan Strain) in Association with COVID-19 Symptom Onset and Severity. JAMA Netw Open. 2022;5(1):e2142796.
Fajnzylber J, Regan J, Coxen K, Corry H, Wong C, Rosenthal A, et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nat Commun. 2020;11(1):5493.
El Zein S, Chehab O, Kanj A, Akrawe S, Alkassis S, Mishra T, et al. SARS-CoV-2 infection: initial viral load (iVL) predicts severity of illness/outcome, and declining trend of iVL in hospitalized patients corresponds with slowing of the pandemic. PLoS ONE. 2021;16(9):e0255981.
Pujadas E, Chaudhry F, McBride R, Richter F, Zhao S, Wajnberg A, et al. SARS-CoV-2 viral load predicts COVID-19 mortality. Lancet Respir Med. 2020;8(9):e70.
Huang Y, Chen S, Yang Z, Guan W, Liu D, Lin Z, et al. SARS-CoV-2 viral load in clinical samples from critically ill patients. Am J Respir Crit Care Med. 2020;201(11):1435–8.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated Pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–111.
Jacobs JL, Naqvi A, Shah FA, Boltz VF, Kearney MF, McVerry BJ, et al. Plasma SARS-CoV-2 RNA levels as a Biomarker of Lower Respiratory Tract SARS-CoV-2 infection in critically ill patients with COVID-19. J Infect Dis. 2022;226(12):2089–94.
Olea B, Albert E, Torres I, Gozalbo-Rovira R, Carbonell N, Ferreres J, et al. SARS-CoV-2 N-antigenemia in critically ill adult COVID-19 patients: frequency and association with inflammatory and tissue-damage biomarkers. J Med Virol. 2022;94(1):222–8.
Wick KD, Leligdowicz A, Willmore A, Carrillo SA, Ghale R, Jauregui A, et al. Plasma SARS-CoV-2 nucleocapsid antigen levels are associated with progression to severe disease in hospitalized COVID-19. Crit Care. 2022;26(1):278.
Group A-TS, Rogers AJ, Wentworth D, Phillips A, Shaw-Saliba K, Dewar RL, et al. The Association of Baseline Plasma SARS-CoV-2 Nucleocapsid Antigen Level and outcomes in patients hospitalized with COVID-19. Ann Intern Med. 2022;175(10):1401–10.
Lepape A, Machut A, Bretonniere C, Friggeri A, Vacheron CH, Savey A. network R-R. Effect of SARS-CoV-2 infection and pandemic period on healthcare-associated infections acquired in intensive care units. Clin Microbiol Infect. 2023;29(4):530-6.
Reyes LF, Rodriguez A, Fuentes YV, Duque S, Garcia-Gallo E, Bastidas A, et al. Risk factors for developing ventilator-associated lower respiratory tract infection in patients with severe COVID-19: a multinational, multicentre study, prospective, observational study. Sci Rep. 2023;13(1):6553.
Vacheron CH, Lepape A, Savey A, Machut A, Timsit JF, Comparot S, et al. Attributable mortality of ventilator-associated Pneumonia among patients with COVID-19. Am J Respir Crit Care Med. 2022;206(2):161–9.
Vacheron CH, Lepape A, Savey A, Machut A, Timsit JF, Vanhems P, et al. Increased incidence of Ventilator-Acquired Pneumonia in Coronavirus Disease 2019 patients: a Multicentric Cohort Study. Crit Care Med. 2022;50(3):449–59.
Abdullaev A, Odilov A, Ershler M, Volkov A, Lipina T, Gasanova T et al. Viral Load and Patterns of SARS-CoV-2 Dissemination to the Lungs, Mediastinal Lymph Nodes, and Spleen of Patients with COVID-19 Associated Lymphopenia. Viruses. 2021;13(7).
Borsa M, Mazet JM. Attacking the defence: SARS-CoV-2 can infect immune cells. Nat Rev Immunol. 2020;20(10):592.
Remy KE, Mazer M, Striker DA, Ellebedy AH, Walton AH, Unsinger J et al. Severe immunosuppression and not a cytokine storm characterizes COVID-19 infections. JCI Insight. 2020;5(17).
Silva S. Comparing studies of SARS-CoV-2 viral loads requires caution. J Med Virol. 2022;94(5):1811–2.
Rodriguez C, de Prost N, Fourati S, Lamoureux C, Gricourt G, N’Debi M, et al. Viral genomic, metagenomic and human transcriptomic characterization and prediction of the clinical forms of COVID-19. PLoS Pathog. 2021;17(3):e1009416.
Yilmaz A, Marklund E, Andersson M, Nilsson S, Andersson LM, Lindh M, Gisslen M. Upper respiratory tract levels of severe Acute Respiratory Syndrome Coronavirus 2 RNA and duration of viral RNA shedding do not differ between patients with mild and Severe/Critical coronavirus Disease 2019. J Infect Dis. 2021;223(1):15–8.
Kim C, Kim JY, Lee EJ, Kang YM, Song KH, Kim ES, et al. Clinical findings, viral load, and outcomes of COVID-19: comparison of patients with negative and positive initial chest computed tomography. PLoS ONE. 2022;17(3):e0264711.
Buetti N, Wicky PH, Le Hingrat Q, Ruckly S, Mazzuchelli T, Loiodice A, et al. SARS-CoV-2 detection in the lower respiratory tract of invasively ventilated ARDS patients. Crit Care. 2020;24(1):610.
Travieso TM, Hughes S, Chen K, Olson L, Gao LB, Kraft F, Wyatt BD, Klotman C, Blasi M. Unique SARS-CoV-2 furin-cleavage site variants in urine of severe COVID-19 patients. Top Antiviral Med. 2022;30(72):194.
Acknowledgements
Not applicable.
Funding
National Heart, Lung, and Blood Institute (K08 HL130557) and Duke University Division of Pulmonary, Allergy, and Critical Care Medicine, Durham, North Carolina.
Author information
Authors and Affiliations
Contributions
All authors contributed to study design. L.C., L.B.O., I.A.N., B.A.S., T.N.D., and B.D.K. performed data collection. L.C., T.N.D., and B.D.K. performed data analysis. L.C. and B.D.K. performed the literature search and prepared the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
B.D.K. is a consultant for Bluejay Diagnostics and received royalties from Cryo-Cell International. All other authors declare that they have no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Duke University Institutional Review Board (Protocol # Pro00101196) prior to all study activities and conducted in accordance with the Declaration of Helsinki. Written informed consent was provided by subjects or their legally authorized representatives prior to study participation. Subjects that were enrolled under a legally authorized representative that later regained decision-making capacity while hospitalized were re-consented to remain in the study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, L., Olson, L.B., Naqvi, I.A. et al. SARS-CoV-2 viremia but not respiratory viral load is associated with respiratory complications in patients with severe COVID-19. BMC Pulm Med 24, 366 (2024). https://doi.org/10.1186/s12890-024-03183-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03183-7