Abstract
Background
We investigated whether double-bundle (DB) anterior cruciate ligament (ACL) reconstruction (ACLR) combined with anterolateral ligament reconstruction (ALLR) improved clinical and radiological outcomes in patients at high risk of ACL failure. The primary outcome was graft failure, and secondary outcomes included knee stability and patient-reported outcome measures (PROMs).
Patients and methods
Fifty-two patients who underwent DB ACLR combined with ALLR were included in this retrospective cohort study. Preoperative risk factors, including femorotibial angle (FTA), lateral tibial slope (LTS), medial tibial slope (MTS), and meniscal tears, were assessed using X-ray and magnetic resonance imaging (MRI). The grade of post-operative pivot shift, Lysholm score, and Tegner activity score were used to assess clinical outcomes. The minimum follow up duration was 2 years.
Results
The cohort (mean age, 26.1 ± 9.4 years; 51.9% male) had a mean follow-up duration of 28.9 ± 3.4 months. Preoperatively, 57.8% had lateral meniscus (LM) tears, and 61.0% had a grade 2–3 pivot shift. Postoperatively, no graft failures or revision cases occurred during follow-up. Approximately 90.4% of the patients exhibited a negative pivot shift (p < 0.001), with Lysholm and Tegner activity scores of 92.5 ± 6.1 and 5.1 ± 2.0. The medial meniscus (MM) tear group had a significantly smaller FTA than the intact group (p = 0.043). No significant differences in PROMs were found between the LM tear and intact LM groups or between the high and low MTS or LTS groups (p = n.s.).
Conclusion
DB ACLR combined with ALLR had satisfactory clinical outcomes in patients at high risk of ACL failure, with no graft failures observed during a mean follow-up duration of 2.4 years. The technique effectively reduced the postoperative pivot shift, regardless of preoperative risk factors.
Study design
Level IV, retrospective therapeutic case-series.
Trail registration
ethical approval number, 202300134B0; ethical committee, the Institutional Review Board of Chang Gung Medical Foundation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Anterior cruciate ligament (ACL) reconstruction (ACLR) is a common surgical procedure that provides satisfactory results in most patients [1, 2]. However, some patients may experience residual rotational instability, particularly those with steep medial or lateral tibial slopes, posterior third meniscal injuries, and anterolateral ligament (ALL) tears [3,4,5,6,7]. This residual instability can lead to secondary cartilage and meniscal injuries and an increased risk of graft failure [8,9,10].
To address these issues, various surgical techniques have been developed, such as double-bundle (DB) ACLR, different ALL reconstruction (ALLR) methods, and lateral extra-articular tenodesis (LET) [11,12,13,14].
The present study aims to determine the correlation between patient demographics and the risk factors for ACL failure and to investigate whether DB ACLR combined with ALLR can overcome unfavorable preoperative conditions and improve clinical outcomes in high-risk patients. The primary outcome was graft failure, and secondary outcomes included knee stability and patient-reported outcome measures (PROMs). We hypothesized that the clinical outcomes of this specific technique would be comparable between patients with and without a high ACLR failure risk.
Materials and methods
Patients
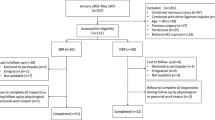
This retrospective study was approved by the Chang Gung Medical Foundation Institutional Review Board (IRB No. 202300134B0). A total of 67 patients who underwent DB ACLR at a single institution by a single surgeon between October 2018 and September 2020 were reviewed. The inclusion criteria were patients with complete radiographic records, including preoperative knee X-rays and magnetic resonance imaging (MRI) scans within 3 months before surgery, and a minimum follow-up of 2 years. The exclusion criteria were previous knee surgery, multi-ligamentous injuries, age over 50 years old, and a lack of follow-up. All patients underwent clinical evaluations before surgery and at the final follow-up. Patients with risk factors for residual pivot shift instabilities included those with a medial tibial slope (MTS) of > 5.6° or a lateral tibial slope (LTS) of > 3.8° [15] and lateral or medial meniscus (LM or MM) tears [3].
Surgical technique
All patients underwent DB ACLR combined with ALLR [12], and all operations were performed by the same surgeon. After marking the bony landmark, full-length semitendinosus and gracilis tendon autografts were harvested. The semitendinosus tendon was prepared in a quadruple-folded fashion to form the anteromedial bundle (AMB). The gracilis tendon was prepared as the posterolateral bundle (PLB) and ALL graft. A FiberTape (Arthrex, Naples, FL, USA), an internal brace for PLB and ALL, was shuttled together with the unfolded gracilis tendon (Fig. 1A). Under arthroscopic assistance, meniscus tears were repaired if possible, and a flexible reamer was used to create a femoral AM tunnel using the inside-out drilling technique (Smith & Nephew Endoscopy, Andover, MA, USA). (Fig. 1B, C) The femoral PL tunnel was created using the outside-in technique (Fig. 1D) to avoid undesirable tunnel connections. Tibial ACL and ALL tunnels were created based on their anatomical positions. One No. 5 Ethibond suture (Ethicon, NJ, USA) was passed from the femoral AM tunnel to the tibial ACL tunnel and another one from the femoral PL tunnel to the tibial ACL tunnel. The third no. 5 Ethibond suture was inserted from the lateral tibia ALL footprint to the medial side of the tibia. The single gracilis tendon with the FiberTape was shuttled intraarticularly through the tibial ACL tunnel and pulled out from the femoral PL tunnel. We ensured that the length outside the lateral femoral cortex was enough to create an extraarticular ALL. Subsequently, a hydroxyapatite interference screw (BioRCI-HA screws; Smith & Nephew Endoscopy) that was 1 mm bigger than the graft size in diameter was used to fix the PLB in an outside-in fashion (Fig. 1E).
Tunnel drilling, graft shuttling, and fixation of the right knee double-bundle ACL combined with ALL reconstruction (A) The semitendinosus is prepared in a quadruple-folded fashion and used as the anteromedial bundle. The gracilis tendon is prepared and used as the posterolateral bundle and ALL graft. The FiberTape serves as an internal brace for the PLB and ALL. (B, C) The femoral AM tunnel is created by the inside-out drilling technique using a flexible reamer. (D) The femoral PL tunnel is created using the outside-in technique. (E) A hydroxyapatite interference screw is used to fix the PLB in an outside-in fashion. (F) The AM bundle is tied with an EndoButton and shuttled intra-articularly. (G) The AM and PL bundles of the double-bundle ACL reconstruction (H, I) The single gracilis tendon and FiberTape are shuttled from the lateral end of the femoral PL tunnel to the lateral end of the tibial ALL tunnel as the ALLR. ACL, anterior cruciate ligament; ALL, anterolateral ligament; HT, hamstring tendon; G, gracilis tendon; AMB, anteromedial bundle; PLB, posterolateral bundle; IB, internal brace; AMT, anteromedial tunnel; PLT, posterolateral tunnel; asterisk, gracilis graft with the FiberTape; arrowhead, the quadruple hamstring graft
Thereafter, the AM bundle was tied using an EndoButton (Smith & Nephew Endoscopy) and shuttled until it was fixed on the femoral cortical surface (Fig. 1F). Another hydroxyapatite interference screw (BioRCI-HA screws; Smith & Nephew Endoscopy) was used to fix the tibial end of both the AMB and PLB grafts in the tibial ACL tunnel at 60 degrees of knee flexion (Fig. 1G). Finally, the single gracilis tendon and the FiberTape were shuttled from the lateral end of the femoral PL tunnel to the lateral end of the tibial ALL tunnel to complete the ALLR with an augmented Swivelock anchor (Arthrex) fixation (Fig. 1H and I).
Clinical and functional evaluation
The evaluation included a preoperative pivot-shift test, a pivot-shift test at the final follow-up, Tegner activity score measurement [16], and Lysholm score assessment [24]. The pivot-shift test was performed by a single examiner, and pain at the ALL attachment sites was recorded [25].
Radiographic evaluation
Lower limb alignment was assessed using standing full-leg radiographs. The MTS and LTS were measured on lateral X-ray and sagittal MRI scans, respectively, using previously described methods [17, 18]. Meniscal injuries, collateral ligament integrity, and cartilage injuries were evaluated on MRI, and the two independent orthopedic surgeons who performed all the radiographic measurements (Table 1) were blinded to the clinical outcomes.
Statistical analysis
Statistical analyses were performed using SPSS (IBM SPSS Statistics 23.0, IBM Inc., Armonk, NY, USA) and Microsoft Office Excel 2016 (Microsoft, Redmond, WA, USA). Categorical data were analyzed using Fisher’s exact tests, whereas continuous data were compared using the Mann–Whitney U test or unpaired t-test, as appropriate. The results were considered statistically significant at p < 0.05. A post hoc power analysis was conducted, and Pearson correlation coefficients were calculated to assess the relationship between MTS or LTS and functional scores.
Results
Demographic, radiological, and functional patient data
Sixty-seven patients were originally enrolled in the study. Of these, 4 were excluded because of a previous surgery and 11 owing to a lack of preoperative images, resulting in a total of 52 patients (77.6%). The mean follow-up duration was 28.9 ± 3.4 months. Our study included 27 (51.9%) male patients; the average age was 26.1 ± 9.4 years; the mean BMI was 25.1 ± 4.0 kg/m2, and 29 (55.8%) patients injured their left knee.
Before the operation, there were 30 (57.7%) cases of LM tears and 32 (61.0%) cases of grade 2 pivot shift. The valgus femorotibial angle (FTA) was 3.6° ± 2.5°, and the MTS was 7.3° ± 2.8° on X-ray and 6.1° ± 2.4° on MRI. Forty-three (82.7%) of the 52 patients had meniscus injuries and underwent meniscus repair. The mean size of the AMB was 7.2 ± 0.7 mm. No patient experienced graft failure or required revision surgery during follow-up. The pivot shift was evaluated at the last follow up, and 47 (90.4%) patients had no residual pivot shift. The Lysholm (92.5 ± 6.1) and Tegner activity (5.1 ± 2.0) scores were also recorded. The demographic data are presented in Table 1.
The intact medial meniscus group versus the medial meniscus tear group
Upon comparing patients in the intact MM and MM tear groups, no significant differences were observed in any demographic characteristics, including sex, age, height, weight, BMI, and perioperative pivot shift (p = n.s.). A significantly smaller FTA was observed in the MM tear group than in the intact MM group (intact vs. tear, 4.0° ± 2.8° vs. 2.6° ± 1.0°; p = 0.043). A steeper MTS was not observed in the MM tear group on X-ray (intact vs. tear, 7.5° ± 2.9° vs. 6.8° ± 2.6°; p = 0.472) or MRI (intact vs. tear, 6.2° ± 2.5° vs. 5.8° ± 2.2°; p = 0.680), compared with the intact MM group (Table 2).
The intact lateral meniscus group versus the lateral meniscus tear group
Upon comparing patients in the intact LM and LM tear groups, no significant difference was observed in any demographic characteristic (p = n.s.). No difference was observed in the FTA between the two groups (intact vs. tear, 3.7° ± 3.2° vs. 3.6° ± 1.9°; p = 0.959). There was a non-significant trend of a steeper MTS on X-ray and MRI in the LM tear group compared to the intact LM group (X-ray: intact vs. tear, 6.5° ± 2.0° vs. 7.9° ± 2.9°, p = 0.088; MRI: intact vs. tear, 5.3° ± 1.6° vs. 6.7° ± 2.6°, p = 0.073) (Table 3). A pre-operative grade 3 pivot shift was significantly more common among patients with LM injuries than among those without LM injuries (97.0% vs. 0%, p < 0.001). No significant differences in clinical scores were observed between the groups (Lysholm score: intact vs. tear, 91.4 ± 4.8 vs. 93.8 ± 6.7, p = 0.320; Tegner activity score: intact vs. tear, 5.8 ± 1.7 vs. 5.0 ± 2.3, p = 0.324) (Table 3).
MTS and clinical outcomes
Following the method used by Li et al. (27), the patients were separated into a group with MTS > 5.6° (n = 19) and a group with MTS < 5.6° (n = 14). The number of female patients was slightly higher in the high MTS group, but this was not significantly different (p = 0.051) between the groups. Other demographic data, including age, BMI, and coronal alignment, were not significantly different between the groups (p = n.s.). The LTS and perioperative pivot shifts did not differ significantly between the two groups. The Lysholm score was significantly higher in the high MTS group than in the low MTS group (95.0 ± 5.8 vs. 89.9 ± 5.5, p = 0.046) (Table 4).
LTS and clinical outcomes
The patients were divided into a group with a LTS of > 3.8° (n = 20) and another with a LTS of < 3.8° (n = 13). No significant differences were found in the demographic characteristics (including sex, age, BMI, coronal alignment, LTS, and perioperative pivot shift) or clinical outcomes (Lysholm score or Tegner activity score) between the groups (p = n.s.) (Table 5).
Discussion
Patients with risk factors for ACL failure, including steep medial or lateral tibial slope, posterior third meniscal injury, or anterolateral ligament (ALL) tears owing to postoperative residual rotational instability, who underwent DB ACLR combined with ALLR achieved similar clinical outcomes to those of patients without these risk factors.
Based on a comparison between patients with multiple, one, and no ACL failures, Grassi et al. concluded that a higher posterior tibial slope on MRI is more common in patients who experienced multiple ACL failures [17]. However, the details of the clinical outcomes and surgical procedures were not provided in their study. Yoon et al. followed up on patients who underwent primary ACLR for at least 10 years and found that patients with increased MTS (> 5.6°) and LTS (> 3.8°) exhibited higher failure rates and lower survival rates [19]. In another study that investigated specific factors in patients with a preoperative high-grade pivot shift, Batty et al. found that ligamentous laxity, male sex, posterior third MM or LM injury, increased posterior tibial slope (> 5.6°), and chronicity were associated with a high-grade pivot shift, which causes ACL failures [3]. In our study, no patient experienced a graft failure during the 2-year follow-up, and the PROMs were comparable between the groups. Sundemo et al. [20] proposed that anteroposterior and rotatory knee laxities were related to inferior subjective outcomes. In our cohort, patients with or without MM or LM injuries had comparable Lyshom or Tegner activity scores. Neither high MTS nor high LTS were correlated with subjective outcomes. Although the results imply that DB ACLR combined with ALLR seems to eliminate the negative effects of meniscus injury and steep MTS and LTS, cadaveric and biomechanical studies are warranted to confirm this observation.
Different methods of performing ALLR have been reported [21,22,23,24,25]. According to Sonnery-Cottet et al., the subjective postoperative outcomes of using a patella-tendon bone autograft for ACLR and a hamstring autograft for ACLR and ALLR were identical between groups, as were side-to-side laxity differences [26]. However, patients who underwent ACLR and ALLR had lower graft failure rates and higher chances of returning to preinjury levels of sport than those that underwent only ACLR [26]. Analysis of the prognostic factors for graft failure indicated that younger age (< 25 years), > 7 mm side-to-side difference, and ACL combined with ALLR were associated with a lower graft failure rate. However, the study did not discuss meniscus tears or the degree of tibial slope. Na et al. conducted another systemic review of 20 studies, comparing patients who underwent ACLR with anterolateral extra-articular procedures (including ALLR and LET) with those who underwent ACLR without anterolateral extra-articular procedures. They found that patients who underwent the anterolateral procedures had improved pivot shift grades and lower graft failure rates, and among these patients, those who underwent ALLR had better subjective outcomes and lower knee stiffness than those that underwent LET [27, 28].
Different surgical techniques that combine DB ACLR with ALLR have been developed for treating ACL injuries in recent years. The main differences are in the femoral tunnel location, which is most commonly placed posterior and proximal to the lateral epicondyle. Few surgeons chose an anterior or distal tunnel location. There is minimal variation in the tibial tunnel location, and the most frequently used ALLR graft is a single-stranded gracilis tendon [27, 28]. However, few studies have reported the clinical results of these techniques. Mao et al. reviewed 15 patients who underwent ACL revision with DB ACLR combined with ALLR [29]. After the operation, the international knee documentation committee (IKDC), Lysholm, and Tegner activity scores significantly improved. Long-term clinical results showed that patients who underwent DB ACLR had lower graft failure rates and less residual anterior translation than those who underwent SB ACLR [1, 2, 7, 30,31,32,33,34,35,36,37]. In our study, we used a quadruple-folded semitendinosus tendon as the AMB and a non-folded gracilis tendon as the PLB. This raised concerns about whether the PLB is strong enough for this application. Therefore, we also passed an internal brace along with the gracilis tendon to augment its strength and improve its stability. Zhao et al. proposed another technique of folding the gracilis tendon into three and thereby increasing the PLB thickness [38]. However, similar to our technique, their technique used only a double-folded semitendinosus tendon as the AMB, thus creating a four-folded intra-articular tendon graft. Further biomechanical studies are required to evaluate these different techniques and their effect on knee stability.
This study has several limitations that should be considered when interpreting its findings. First, the retrospective design and the absence of a control group limit our ability to draw definitive conclusions about the effectiveness of the combined DB ACLR and ALLR technique.
Second, the study was conducted at a single institution, which may limit the generalizability of the results to other settings or populations. Further prospective, randomized controlled trials and multi-center studies with larger and more diverse patient cohorts are required for stronger evidence and generalizability.
Third, the assessment of the long-term outcomes and potential complications of the combined technique was hindered by the relatively short follow-up duration (mean 28.9 ± 3.4 months). Longer follow-up periods would be necessary to evaluate the durability of the results and the risk of late graft failure or osteoarthritis development.
Fourth, our ability to quantify postoperative stability in patients with different risk factors was limited by the lack of objective arthrometer data on residual anterior tibial translation. Future studies should include these objective measurements to better characterize the impact of the combined technique on knee laxity. However, some authors have proposed that graft failure and knee laxity could be related to PROM values [8].
Finally, the study’s final sample size (n = 52) may have been insufficient to detect clinically meaningful differences in outcomes between subgroups. A post hoc power analysis of the Lysholm score, assuming an alpha level of 0.05, an MCID of 10 points, and an SD of 15 points, revealed an estimated power of 0.62 with the current sample size, indicating that the study may have been underpowered to detect a difference. Larger studies with adequate power are needed to confirm our findings and explore the potential effects of risk factors on postoperative outcomes.
In summary, our study observed that some patients with risk factors such as a steep tibial slope, meniscal injury, or ALL tear experienced successful outcomes following standard ACL reconstruction without additional procedures like slope-reducing osteotomy. However, further research comparing the outcomes of surgeries with and without such additional procedures is needed to draw definitive conclusions about their necessity in managing the risk of residual instability.
Although this study offers insights into the potential benefits of DB ACLR combined with ALLR in high-risk patients, its findings should be interpreted with caution owing to the limitations of its design, sample size, and follow-up duration. Further high-quality research is needed to confirm our results and guide clinical decision-making in this patient population.
Conclusion
In conclusion, DB ACLR combined with ALLR shows promise in addressing the challenges of high-risk patients undergoing ACL reconstruction, providing satisfactory clinical outcomes, and reducing postoperative pivot-shift. Although these findings are encouraging, additional research is necessary to confirm the benefits of this approach and guide its integration into clinical practice. As our understanding of the factors that influence ACL reconstruction outcomes improves, refining surgical techniques to better serve high-risk patients will remain an important goal in sports medicine.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Tashman S, Zandiyeh P, Irrgang JJ, Musahl V, West RV, Shah N, Fu FH. Anatomic single- and double-bundle ACL reconstruction both restore dynamic knee function: a randomized clinical trial-part II: knee kinematics. Knee Surg Sports Traumatol Arthrosc. 2021;29(8):2676–83.
Chen H, Chen B, Tie K, Fu Z, Chen L. Single-bundle versus double-bundle autologous anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials at 5-year minimum follow-up. J Orthop Surg Res. 2018;13(1):50.
Batty LM, Firth A, Moatshe G, Bryant DM, Heard M, McCormack RG, Rezansoff A, Peterson DC, Bardana D, MacDonald PB, et al. Association of Ligamentous Laxity, male sex, chronicity, Meniscal Injury, and posterior tibial slope with a high-Grade Preoperative Pivot Shift: a Post Hoc Analysis of the STABILITY study. Orthop J Sports Med. 2021;9(4):23259671211000038.
Hoshino Y, Hiroshima Y, Miyaji N, Nagai K, Araki D, Kanzaki N, Kakutani K, Matsushita T, Kuroda R. Unrepaired lateral meniscus tears lead to remaining pivot-shift in ACL-reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3504–10.
Hoshino Y, Miyaji N, Nishida K, Nishizawa Y, Araki D, Kanzaki N, Kakutani K, Matsushita T, Kuroda R. The concomitant lateral meniscus injury increased the pivot shift in the anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):646–51.
Oh JY, Kim KT, Park YJ, Won HC, Yoo JI, Moon DK, Cho SH, Hwang SC. Biomechanical comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction: a meta-analysis. Knee Surg Relat Res. 2020;32(1):14.
Musahl V, Bedi A, Citak M, O’Loughlin P, Choi D, Pearle AD. Effect of single-bundle and double-bundle anterior cruciate ligament reconstructions on pivot-shift kinematics in anterior cruciate ligament- and meniscus-deficient knees. Am J Sports Med. 2011;39(2):289–95.
Lindanger L, Strand T, Mølster AO, Solheim E, Inderhaug E. Effect of early residual laxity after Anterior Cruciate Ligament Reconstruction on Long-term laxity, Graft Failure, return to sports, and subjective outcome at 25 years. Am J Sports Med. 2021;49(5):1227–35.
Ventura A, Legnani C, Boisio F, Borgo E, Peretti GM. The association of extra-articular tenodesis restores rotational stability more effectively compared to contralateral hamstring tendon autografts ACL reconstruction alone in patients undergoing ACL revision surgery. Orthop Traumatol Surg Res. 2021;107(2):102739.
Kawanishi Y, Kobayashi M, Yasuma S, Fukushima H, Kato J, Murase A, Takenaga T, Yoshida M, Kuroyanagi G, Kawaguchi Y, et al. Factors Associated with residual pivot Shift after ACL Reconstruction: a quantitative evaluation of the pivot-shift test Preoperatively and at Minimum 12-Month follow-up. Orthop J Sports Med. 2024;12(2):23259671241230967.
Sonnery-Cottet B, Saithna A, Blakeney WG, Ouanezar H, Borade A, Daggett M, Thaunat M, Fayard JM, Delaloye JR. Anterolateral Ligament Reconstruction protects the repaired medial Meniscus: a comparative study of 383 anterior cruciate ligament reconstructions from the SANTI Study Group with a Minimum follow-up of 2 years. Am J Sports Med. 2018;46(8):1819–26.
Chiu C-H, Chi J-E, Huang P-H, Chang S-S, Hsu K-Y, Chen AC-Y, Chan Y-S. Anatomic double-bundle ACL Reconstruction with Extra-articular Anterolateral Ligament Reconstruction and Internal Brace. Arthrosc Techniques. 2021;10(3):e789–96.
Torkaman A, Hosseinzadeh M, Mohammadyahya E, Torkaman P, Bahaeddini MR, Aminian A, Tayyebi H. All-inside anterior cruciate ligament reconstruction with and without anterolateral ligament reconstruction: a prospective study. BMC Musculoskelet Disord. 2024;25(1):16.
Legnani C, Borgo E, Macchi V, Ventura A. Restoring rotational stability following anterior cruciate ligament surgery: single-bundle reconstruction combined with lateral extra-articular tenodesis versus double-bundle reconstruction. J Comp Eff Res. 2022;11(10):729–36.
Li Y, Hong L, Feng H, Wang Q, Zhang J, Song G, Chen X, Zhuo H. Posterior tibial slope influences static anterior tibial translation in anterior cruciate ligament reconstruction: a minimum 2-year follow-up study. Am J Sports Med. 2014;42(4):927–33.
Tegner Y, Lysholm J, Lysholm M, Gillquist J. A performance test to monitor rehabilitation and evaluate anterior cruciate ligament injuries. Am J Sports Med. 1986;14(2):156–9.
Grassi A, Macchiarola L, Urrizola Barrientos F, Zicaro JP, Costa Paz M, Adravanti P, Dini F, Zaffagnini S. Steep posterior tibial slope, anterior tibial subluxation, deep posterior lateral femoral condyle, and Meniscal Deficiency are common findings in multiple anterior cruciate ligament failures: an MRI case-control study. Am J Sports Med. 2019;47(2):285–95.
Grassi A, Signorelli C, Urrizola F, Macchiarola L, Raggi F, Mosca M, Samuelsson K, Zaffagnini S. Patients with failed Anterior Cruciate Ligament Reconstruction have an increased posterior lateral tibial Plateau slope: a case-controlled study. Arthroscopy. 2019;35(4):1172–82.
Yoon KH, Park SY, Park JY, Kim EJ, Kim SJ, Kwon YB, Kim SG. Influence of posterior tibial slope on clinical outcomes and Survivorship after Anterior Cruciate Ligament Reconstruction using hamstring autografts: a Minimum of 10-Year Follow-Up. Arthroscopy. 2020;36(10):2718–27.
Sundemo D, Sernert N, Kartus J, Hamrin Senorski E, Svantesson E, Karlsson J, Samuelsson K. Increased postoperative manual knee laxity at 2 years results in Inferior Long-Term Subjective Outcome after Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2018;46(11):2632–45.
DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, LaPrade RF. Anterolateral Ligament Reconstruction Techniques, biomechanics, and clinical outcomes: a systematic review. Arthroscopy. 2017;33(8):1575–83.
Rosenstiel N, Praz C, Ouanezar H, Saithna A, Fournier Y, Hager JP, Thaunat M, Sonnery-Cottet B. Combined anterior cruciate and Anterolateral Ligament Reconstruction in the Professional Athlete: clinical outcomes from the Scientific Anterior Cruciate Ligament Network International Study Group in a series of 70 patients with a Minimum Follow-Up of 2 years. Arthroscopy. 2019;35(3):885–92.
Hamido F, Habiba AA, Marwan Y, Soliman ASI, Elkhadrawe TA, Morsi MG, Shoaeb W, Nagi A. Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1173–80.
Kunze KN, Manzi J, Richardson M, White AE, Coladonato C, DePhillipo NN, LaPrade RF, Chahla J. Combined Anterolateral and Anterior Cruciate Ligament Reconstruction improves Pivot Shift compared with isolated Anterior Cruciate Ligament Reconstruction: a systematic review and Meta-analysis of Randomized controlled trials. Arthroscopy. 2021;37(8):2677–703.
Moon HS, Choi CH, Seo YJ, Lee Y, Jung M, Park JH, Kim SH. The orientation of the ALL femoral tunnel to minimize collision with the ACL tunnel depends on the need or not of far-cortex drilling. Knee Surg Sports Traumatol Arthrosc 2022.
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral Ligament Reconstruction is Associated with significantly reduced ACL graft rupture rates at a Minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med. 2017;45(7):1547–57.
Zein AMN, Elshafie M, Elsaid ANS, Elrefai MAE. Combined anatomic anterior cruciate ligament and double bundle Anterolateral Ligament Reconstruction. Arthrosc Tech. 2017;6(4):e1229–38.
Mediavilla I, Aramberri M, Tiso G, Murillo-González JA. Combined double bundle Anterior Cruciate Ligament Reconstruction and Anterolateral Ligament Reconstruction. Arthrosc Tech. 2018;7(8):e881–6.
Mao Y, Sun W, Fu W, Li J. [Effectiveness of double-bundle anterior cruciate ligament reconstruction combined with anterolateral ligament reconstruction for revision]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(3):330–6.
Bedi A, Musahl V, O’Loughlin P, Maak T, Citak M, Dixon P, Pearle AD. A comparison of the effect of central anatomical single-bundle anterior cruciate ligament reconstruction and double-bundle anterior cruciate ligament reconstruction on pivot-shift kinematics. Am J Sports Med. 2010;38(9):1788–94.
Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(9):1000–6.
Chen K, Zhu W, Zheng Y, Zhang F, Ouyang K, Peng L, Liu H, Feng W, Huang Y, Zhang G, et al. A retrospective study to compare the clinical effects of individualized anatomic single- and double-bundle anterior cruciate ligament reconstruction surgery. Sci Rep. 2020;10(1):14712.
Eliya Y, Qureshi AR, Kay J, Nagai K, Hoshino Y, de Sa D. Anatomical double-bundle anterior cruciate ligament reconstruction moderately improved tegner scores over the long-term: a systematic review and meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 2022.
Järvelä S, Kiekara T, Suomalainen P, Järvelä T. Double-bundle Versus single-bundle Anterior Cruciate Ligament Reconstruction: a prospective Randomized Study with 10-Year results. Am J Sports Med. 2017;45(11):2578–85.
Seppänen A, Suomalainen P, Huhtala H, Mäenpää H, Kiekara T, Järvelä T. Double bundle ACL reconstruction leads to better restoration of knee laxity and subjective outcomes than single bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1795–808.
Svantesson E, Sundemo D, Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu FH, Desai N, Stålman A, Samuelsson K. Double-bundle anterior cruciate ligament reconstruction is superior to single-bundle reconstruction in terms of revision frequency: a study of 22,460 patients from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3884–91.
Zhang Y, Xu C, Dong S, Shen P, Su W, Zhao J. Systemic review of anatomic single- Versus double-bundle Anterior Cruciate Ligament Reconstruction: does femoral tunnel drilling technique matter? Arthroscopy. 2016;32(9):1887–904.
Zhao J, Qiu J, Chen J, Xu J. Combined double-bundle Anterior Cruciate Ligament Reconstruction and Anterior Cruciate ligament-mimicking Anterolateral structure Reconstruction. Arthrosc Tech. 2020;9(8):e1141–6.
Acknowledgements
The authors thank Linkou Chang Gung Memorial Hospital for their support of this study.
Funding
This study was supported by Chang Gung Medical Foundation (CORPG3N0511). Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, CMRPG5K0092, CMRPG3M2032.
Author information
Authors and Affiliations
Contributions
CY and MC wrote the manuscript. MC measured the radiological result. CW performed the statistics. AC, KH, and YC provided professional opinion regarding DBACL combined ALL reconstruction. CC provided all study cases and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval number, 202300134B0; ethical committee, the Institutional Review Board of Chang Gung Medical Foundation; the Institutional Review Board of Chang Gung Medical Foundation approved the study and waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, CP., Chen, MZ., Wang, CL. et al. Double-bundle ACL combined with ALL reconstruction for patients at high risk of ACL failure: clinical and radiological results. BMC Musculoskelet Disord 25, 594 (2024). https://doi.org/10.1186/s12891-024-07703-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07703-8