Abstract
Objectives
To optimize cervical vertebral bone quality (C-VBQ) score and explore its effectiveness in predicting cage subsidence in Anterior Cervical Corpectomy and Fusion (ACCF) and identify a new method for evaluating subsidence without different equipment and image scale interference.
Methods
Collecting demographic, imaging, and surgical related information. Measuring Cage Subsidence with a new method. Multifactorial logistic regression was used to identify risk factors associated with subsidence. Pearson’s correlation was used to determine the relationship between C-VBQ and computed tomography (CT) Hounsfield units (HU). The receiver operating characteristic (ROC) curve was used to assess C-VBQ predictive ability. Correlations between demographics and C-VBQ scores were analyzed using linear regression models.
Results
92 patients were included in this study, 36 (39.1%) showed subsidence with a C-VBQ value of 2.05 ± 0.45, in the no-subsidence group C-VBQ Value was 3.25 ± 0.76. The multifactorial logistic regression showed that C-VBQ is an independent predictor of cage subsidence with a predictive accuracy of 93.4%. Pearson’s correlation analysis showed a negative correlation between C-VBQ and HU values. Linear regression analysis showed a positive correlation between C-VBQ and cage subsidence. Univariate analyses showed that only age was associated with C-VBQ.
Conclusions
The C-VBQ values obtained using the new measurements independently predicted postoperative cage subsidence after ACCF and showed a negative correlation with HU values. By adding the measurement of non-operated vertebral heights as a control standard, the results of cage subsidence measured by the ratio method are likely to be more robust, perhaps can exclude unavoidable errors caused by different equipment and proportional.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Anterior cervical corpectomy and fusion (ACCF) is a surgery used to treat cervical spinal diseases, tumors, and trauma [1, 2]. ACCF relieves compression in front of the spinal cord, including the removal of herniated discs, ossified posterior longitudinal ligaments, and osteophytes [3]. However, hardware-related complications can arise, such as screw and plate breakage and cage subsidence, which are the most common complications [4]. According to the previous studies, subsidence ranges from 9 to 79.7% [5,6,7,8,9].
Subsidence is inherent when achieving fusion between vertebrae, and it can have adverse clinical and biomechanical effects, such as cervical foraminal stenosis and cage displacement [10, 11]. The method of measuring subsidence can differ among researchers and may include the measurement of variations in disc gap height, fused segment height, or displacement from cage insertion. Subsidence is classified into 2 mm, 3 mm, 4 mm, or > 10% in different studies [12]. However, differences in equipment and image scales often lead to unavoidable errors in subsidence judgment.
Lower bone mineral density(BMD) is a crucial risk factor for cage subsidence according to numerous studies, and dual-energy X-ray absorptiometry (DEXA) is the most effective method for assessing BMD [13]. However, the use of DEXA in the cervical spine is extremely limited; therefore, measuring and obtaining cervical vertebra Hounsfield units (HU) values via cervical computed tomography (CT) is gradually becoming an effective method for determining the bone quality of cervical vertebrae [14, 15]. Soliman et al. [16]. developed a cervical vertebral bone quality (C-VBQ) score to predict cage subsidence following anterior cervical discectomy and fusion (ACDF). The C-VBQ score was derived from the VBQ score for the lumbar spine developed by Ehresman et al. [17] and has been validated [16]. The utilization of the C-VBQ score in ACCF has not been thoroughly studied, and it is possible that varying cage sizes and biomechanics may result in increased cage subsidence and impact the predictive accuracy of this score.
In this study, we aimed to optimize the C-VBQ score, explore its effectiveness in predicting cage subsidence in ACCF patients and identify a new assessment method that eliminates interference from variations in equipment and imaging scales.
Methods
Patient population
This study examined 92 patients who underwent single-level ACCF at a hospital between 2016 and 2021 and received Ethics Committee approval from West China Hospital of Sichuan University. Because this was a retrospective study, informed consent was waived with the approval of the Ethics Committee. Preoperatively, the patients underwent a T1-weighted cervical magnetic resonance imaging (MRI), CT, and a lateral cervical spine X-ray. At 3 days and at 1 year post-surgery, the patients were re-examined with a lateral cervical spine X-rays. The study included only patients with complete imaging data. The clinical information collected included age, sex, body mass index (BMI), smoking history, hypertension status, diabetes status, cage type, surgical levels, blood loss, and Charlson Comorbidity Index score. Patients were excluded if they had been given a diagnosis of trauma, malignancy or infection, or had a history of cervical surgery. Radiological calculations were performed by two authors independently; when the two initial scores differed by more than 10%, a third author (with a senior title) rechecked them and determined the final score. Imaging parameters were measured using a picture archiving and communication system (PACS) (Siemens, syngo MultiModality Workplace, Germany).
Measurement of C-VBQ
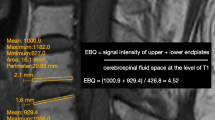
The C-VBQ scores were assessed on midsagittal sections of the patient’s preoperative cervical MRI T1-weighted, non-contrast-enhanced images. A region of interest (ROI) was delineated that included the C3, C4, C5, and C6 vertebrae, containing as much of the cancellous bone region as possible and excluding cortical bone, abnormal subchondral alterations, focal lesions (e.g., hemangiomas) and the posterior venous plexus. Two additional ROIs were delineated placed in the cerebrospinal fluid (CSF) anterior and posterior to the spinal cord in the C2 vertebral plane (Fig. 1). When obstruction exists in the CSF at the C2 level occurred, the ROIs were located in the CSF at the C1 vertebral plane. The median signal intensity (SI) of C3-6 was subsequently divided by the average of the pre and post spinal cord CSF SIs (Formula 1).
This score was proposed by Soliman et al. [16] based on the same principles identified by Ehresman et al. [18]. To avoid missing crucial areas, ROIs included as much of the cancellous bone region as possible due to uneven fat distribution in the vertebral body. Although the anterior spinal cord space is wider at the C2 vertebral level than at C3-6 [16], it is still more susceptible to posterior longitudinal ligaments or herniated discs; therefore, it is more accurate to include measurements of the posterior CSF area of the spinal cord and then take an average. The cardinal and C7 vertebrae were excluded because of typical anatomical differences compared to C3-6 [19].
Sagittal non-contrast-enhanced T1-weighted magnetic resonance imaging of the cervical spine with the signal intensity of the regions of interest (ROI) used to calculate the C-VBQ score. The ROIs include as much of the vertebral cancellous bone region as possible. The anterior CSF region of the spinal cord at the C2 vertebral plane is too narrow, and another ROI is placed in the posterior CSF region of the spinal cord at the C2 level. The C-VBQ score shown in this example is 1.88. C-VBQ: cervical vertebral bone quality
CT hounsfield value measurements
CT HU measurements were performed using the method previously reported by Schreiber et al. [20]. In this study, the HU values of C3-6 vertebrae were measured separately, and the average value was recorded as the global HU value.
Cage subsidence assessment standards
There is no consensus on the definition of subsidence, Some studies use a grading scale such as grade 0, 1, or 2, while others define subsidence as a loss of more than 3 mm in height in fused segments [21, 22]. In our study, we found that although the position of the cage did not change significantly from the postoperative period to the final follow-up in some of the patients, the height loss in the fused segments was much greater than 3 mm according to the methods used in previous studies, which led to the judgment of pseudosubsidence. One of the possible reasons for this difference is that two-dimensional imaging is usually uncalibrated, and the height of the fused segments depends on factors such as the radiation-emitting source and the angle and the distance between the patient and the detector. These factors are not considered in most of the studies related to cage subsidence. Thus, creating a method for subsidence measurement that can effectively address these differences is crucial. Therefore, we propose the proportional method for defining cage subsidence, which includes measurements of body height in vertebrae that have not undergone surgical manipulation (e.g., C3) in addition to the segmental height of the fusion (SH) postoperatively and at the time of the last follow-up (Fig. 2). The measurement formula is as follows (Formula 2):
(A), postoperative lateral cervical spine X-ray; (B), 1-year postoperative lateral cervical spine X-ray, the arrow shows a clear change in cage position with visible subsidence. The height loss of the fused segments measured individually was only 0.2 cm (< 0.3 cm), which does not comply with the traditional definition of subsidence. Using a new subsidence measurement method, the relative loss of height of the fused segments was 0.43 cm (> 0.3 cm)
Statistical analyses
Statistical analyses were performed using SPSS 22 (SPSS, Inc., Chicago, IL). Continuous variables are reported as the mean ± SD and were statistically analyzed using the Student’s t-test. The categorical variables are reported as frequencies and percentages and were assessed using the χ2 test. All clinical variables were included in a multifactorial logistic regression analysis used to identify risk factors associated with subsidence. Pearson’s correlation was used to evaluate the correlation between C-VBQ score and HU. The area under the ROC curve was used to assess the predictive power of the model. The Youden index of the ROC curve was used to determine the optimal cutoff values for the variables. Finally, univariate analyses of all baseline patient demographics were performed using linear regression models to determine potential correlations between these data and C-VBQ scores. A P value < 0.05 was considered statistically significant.
Results
Patient demographic characteristics
A total of 92 patients were ultimately enrolled in this study; 36(39.1%) patients exhibited subsidence, with C-VBQ values of 2.05 ± 0.45 in the non-subsidence group and 3.25 ± 0.76 in the subsidence group(P < 0.001). Moreover, the HU values were 405.76 ± 61.27 in the non-subsidence group and 307.01 ± 60.75 in the subsidence group (P < 0.001). The characteristics of all included patients collected are summarized in Table 1.
Predictors of cage subsidence
Multifactorial logistic regression was performed including all potential risk factors for cage subsidence after ACCF. The results showed that the C-VBQ score (odd ratio = 5.700, 95% CI= [3.435–8.193], P = 0.006) was an independent predictor of cage subsidence. The results of the analyses are detailed in Table 2. Linear regression analysis of the relationship between C-VBQ score and cage subsidence revealed a positive correlation (r = 0.817, P < 0.001; Fig. 3).
Assessment of predictive value
The ROC curve for predicting cage subsidence by the VBQ score was established, and the diagnostic accuracy was 93.4% (95% CI = 88.5-98.2%; Fig. 4). The ideal cutoff value for the C-VBQ score was 2.71 (sensitivity: 80.60%, specificity: 91.07%) according to the Youden index. Age was significantly correlation with C-VBQ score according to a univariate linear regression analysis (r = 0.069, P = 0.012; Table 3).
VBQ score and CT-HU correlation
We discovered a noteworthy adverse correlation between HU and C-VBQ score via Pearson’s correlation test (r=-0.458, P<0.001; Fig. 5).
Discussion
ACCF is one of the most effective treatment modalities for degenerative cervical spine disease [23]. Using cages is a primary technique for maintaining the height of the fused sector, preventing neuroforaminal narrowing, and accelerating osseous integration. However, cage subsidence is one of the most common hardware-related complications in the postoperative period; it can cause a decrease in height in fused segments and lead to serious complications such as nonunion, kyphosis, and screw breakage [6]. Cage subsidence is defined differently by various researchers; It can range from a loss of 1–4 mm or > 10% in postoperative fused segment height [9]. ACCF results in greater cage subsidence than ACDF due to the larger cage sizes and surgical resection areas. Studies show that subsidence ranges from 9 to 80% [5, 6, 8, 9]. Bone mineral density (BMD) is considered to be an essential factor affecting postoperative cage subsidence; therefore, tests, including dual-energy X-ray (DEXA), quantitative CT (QCT), and Hounsfield units (HU), are often used to assess vertebral bone quality preoperatively. The C-VBQ score, proposed by Soliman et al. [16] based on cervical MRI, has the advantages of being easy to obtain and not requiring radiation, confirming the validity of its application in ACDF. However, the C-VBQ measurement method can still be optimized and adapted appropriately, and its application range still needs to be proven by additional research. To the best of our knowledge, the C-VBQ score has not yet been applied in ACCF surgery, where subsidence is more significant.
In this study, we optimized the C-VBQ score and confirmed that it can independently predict cage subsidence in ACCF surgery; moreover, we propose a new method for measuring cage subsidence, which avoids errors caused by differences in imaging image scales and equipment. This method has a wide range of applications.
Previous research on ACCF cage subsidence
Based on the findings of previous studies, several factors, such as age, cage material, and surgical segment, can affect cage subsidence after ACCF [24]. Osteoporosis is well recognized as one of the factors affecting cage subsidence [25,26,27]. In our study, only age was significantly different between the two groups, except for C-VBQ and HU; however, consistent with the findings of Wang et al. [24], age was not an independent risk factor for predicting subsidence. The reason for this difference may be that older people often have a lower bone density, and it is not surprising that such discrepancies arise. No significant differences were observed in cage material or surgical segments between the two groups in our study, despite previous research suggesting their importance in subsidence [28]. This non-significant difference may have stemmed from adjustments in the measurement methods.
The current gold standard for evaluating bone density is DEXA, which most often measures the lumbar spine and hip joints and does not directly reflect cervical spine bone density. Moreover, DEXA is often affected by abdominal aortic calcification, bone degeneration, fracture or osteophyte formation [29]. Therefore, the use of DEXA in the cervical spine is limited.
Quantitative computed tomography (QCT) is an alternative technique for assessing bone mineral density. Unlike DEXA T-scores, QCT results are considered more dependable due to their ability to mitigate superimposition effects that can impede DEXA measurements [30, 31]. However, the exorbitant expense and excessive radiation dosage have hindered the broad application of QCT in clinical settings [32].
In contrast, measurements of vertebral HU values based on conventional CT images are now more widely used. Lee et al. [15] discovered that the vertebral HU value provides a reliable means of assessing bone density in the cervical spine with good accuracy. Similarly, Wang et al. [33] reported that cage subsidence in single-level ACDF is associated with lower preoperative HU values in the vertebra. Additionally, another study revealed a significant correlation between cervical HU values and lumbar BMD values [34].
Vertebral bone quality score
In 2020, Ehresman et al. [17] introduced the VBQ score based on T1-weighted MRI. This study confirmed the correlation of VBQ score with the DEXA T-score and its clinical value in predicting lumbar osteoporosis patients. Unlike the M-score proposed by Bandirali et al. [35], which depends on the signal-to-noise ratio, the VBQ score includes CSF signal intensity to adjust for baseline signal differences between devices, giving it a wider range of applicability. Based on these result, additional authors have further investigated the clinical application of the VBQ score [16, 33, 34]. Subsequently, Salzmann et al. [36]. demonstrated a substantial correlation between the VBQ score and quantified CT measurements. The diagnostic accuracy for osteoporosis was 70.8%. The application of the VBQ score is not limited to the lumbar spine. Soliman et al. [16]. proposed the C-VBQ score and demonstrated its good application in ACDF surgery. However, this new measurement method can still be further optimized, and its validity for application in ACCF surgery, which has a higher cage subsidence rate, has yet to be demonstrated. The VBQ score assumes that osteoporosis causes fat infiltration and adipocyte replacement, resulting in increased T1-signal intensity in trabecular bone; however, fat infiltration and partitioning in vertebral trabeculae are not always homogeneous, and smaller circular regions of interest may exclude important information leading to errors [37]. Therefore, the delineation of the ROIs on the vertebral body should, as much as possible, include areas of trabecular bone and exclude cortical bone, abnormal subchondral alterations, focal lesions (e.g., hemangiomas) and the posterior venous plexus. In addition, the C-VBQ score includes a region of interest is placed in the anterior region of the spinal cord at the C2 vertebral level. However, in many patients, we find that this region is often too narrow and is affected by the posterior longitudinal ligament and the emanating nerve roots. Therefore, we suggest the addition of an ROI in the CSF posterior to the spinal cord at the C2 vertebral level, which is more spacious and less susceptible to interference by ligaments and nerve roots. We used the optimized C-VBQ score in ACCF surgery and demonstrated that it can independently predict cage subsidence after ACCF surgery. Although the C-VBQ score may still be affected by pathological changes in the cervical vertebral bodies such as tumours, infections, and so on, which may limit its use in patients with tumours, infections, or trauma, Since cervical MRI is routinely required prior to performing ACCF surgery and the limited use of DEXA T-scores in the cervical spine, the C-VBQ score is still a promising measure of cervical bone quality that is also free of radiation. The C-VBQ score is an effective complementary or alternative method for assessing cervical bone quality. The simple and convenient measurement method can help surgeons quickly determine the patient bone quality.
Improved subsidence measurement methods
Previous studies have not standardized the measurement methods or the subsidence cut-off values [12]. It is possible that differences in imaging instrumentation and potentially unavoidable image scale errors may have contributed to this discrepancy. Two-dimensional radiography is usually uncalibrated, so the height of the fused segments depends on the angles and distances among the radiation-emitting source, the patient and the detector. Although modern image assessment tools can be used to circumvent this error to some extent, more accurate measurements are not possible without the simultaneous presence of a reference line. For accuracy, it is recommended to divide the height of the fused segment by the height of the nonoperated vertebral body because its height remains relatively unchanged. (Formula 2; Fig. 2). Theoretically, we can circumvent the errors associated with the image calibration problem by using a proportionality relationship to evaluate cage subsidence. Wang et al. [24] concluded that defining the cut-off value for subsidence as 2 mm produces the largest error; therefore, we defined the presence of subsidence as a relative subsidence height ≥ 3 obtained through Formula 2. This new method was applied in this study with good results. We believe that this measurement method provides more stable results and has a wider range of applicability.
Limitations
Although our results showed that the C-VBQ score was an independent predictor of postoperative cage subsidence after ACCF according to multifactorial logistic regression and was strongly correlated with CT-HU values, the limited sample size remains a nonnegligible problem in our study. Second, the retrospective nature of this study based on a single center limits the representativeness of our findings. Third, CT-HU is not the gold standard for evaluating bone quality, and DEXA is still needed to evaluate the effectiveness of the C-VBQ score. Therefore, studies with larger sample sizes are needed to validate the use of the C-VBQ score in other cervical spine surgeries and the correlation between C-VBQ and DEXA T scores. Finally, as a new subsidence measurement method, additional research is needed to verify the stability of this method and to establish a uniform standard for evaluating subsidence. Furthermore, additional research is needed to evaluate the potential advantages of optimized C-VBQ score measurements and the extent to which pathological changes associated with the vertebral bodies affect C-VBQ scores.
Conclusion
After optimization, the C-VBQ score was significantly correlated with cage subsidence following ACCF surgery. Additionally, it demonstrated a negative correlation with HU values. The C-VBQ score is a promising tool. In addition, a C-VBQ score > 2.71 suggested that the vertebral body was of poor quality. By adding the measurement of non-operated segmental vertebral heights as a control standard, the assessment of cage subsidence can exclude the differences caused by different equipment and image scales, which can help establish a uniform standard for judging subsidence.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- C-VBQ:
-
Cervical vertebral bone quality
- ACCF:
-
Anterior Cervical Corpectomy and Fusion
- ROC:
-
Receiver operating characteristic
- BMD:
-
Bone mineral density
- DEXA:
-
Dual-energy X-ray absorptiometry
- HU:
-
Hounsfield unit
- CT:
-
Computed tomography
- ACDF:
-
Anterior cervical discectomy and fusion
- MRI:
-
Magnetic Resonance Imaging
- BMI:
-
Body Mass Index
- SI:
-
Signal intensity
- CSF:
-
Cerebrospinal fluid
- SH:
-
Segmental height of the fusion
- QCT:
-
Quantitative computed tomography
References
Chuang HC, Cho DY, Chang CS, Lee WY, Jung-Chung C, Lee HC, Chen CC. Efficacy and safety of the use of titanium mesh cages and anterior cervical plates for interbody fusion after anterior cervical corpectomy. Surg Neurol. 2006;65(5):464–71. discussion 471.
Badhiwala JH, Ahuja CS, Akbar MA, Witiw CD, Nassiri F, Furlan JC, Curt A, Wilson JR, Fehlings MG. Degenerative cervical myelopathy - update and future directions. Nat Rev Neurol. 2020;16(2):108–24.
Fessler RG, Steck JC, Giovanini MA. Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery. 1998;43(2):257–65. discussion 265 – 257.
Dhar UK, Menzer EL, Lin M, Hagerty V, O’Connor T, Tsai CT, Vrionis FD. Factors influencing cage subsidence in anterior cervical corpectomy and discectomy: a systematic review. Eur Spine J. 2023;32(3):957–68.
Chen Y, Chen D, Guo Y, Wang X, Lu X, He Z, Yuan W. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech. 2008;21(7):489–92.
Hu BW, Wang LN, Song YM, Hu YJ, Lyu QN, Liu LM, Zhu C, Zhou CG, Yang X. A comparison of long-term outcomes of nanohydroxyapatite/polyamide-66 cage and titanium mesh cage in anterior cervical corpectomy and fusion: a clinical follow-up study of least 8 years. Clin Neurol Neurosurg. 2019;176:25–9.
Sevki K, Mehmet T, Ufuk T, Azmi H, Mercan S, Erkal B. Results of surgical treatment for degenerative cervical myelopathy: anterior cervical corpectomy and stabilization. Spine (Phila Pa 1976). 2004;29(22):2493–500.
Lau D, Song Y, Guan Z, La Marca F, Park P. Radiological outcomes of static vs expandable titanium cages after corpectomy: a retrospective cohort analysis of subsidence. Neurosurgery. 2013;72(4):529–39. discussion 528–529.
van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW. Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine J. 2005;5(6):645–9. discussion 649.
Ji C, Yu S, Yan N, Wang J, Hou F, Hou T, Cai W. Risk factors for subsidence of titanium mesh cage following single-level anterior cervical corpectomy and fusion. BMC Musculoskelet Disord. 2020;21(1):32.
Daubs MD. Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine (Phila Pa 1976). 2005;30(12):1402–6.
Karikari IO, Jain D, Owens TR, Gottfried O, Hodges TR, Nimjee SM, Bagley CA. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech. 2014;27(1):1–10.
Guzman JZ, Feldman ZM, McAnany S, Hecht AC, Qureshi SA, Cho SK. Osteoporosis in cervical spine surgery. Spine (Phila Pa 1976). 2016;41(8):662–8.
Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR. Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J. 2009;9(7):537–44.
Lee HJ, You ST, Kim JH, Kim IS, Sung JH, Hong JT. Significance of cervical spine computed Tomography Hounsfield Units to Predict Bone Mineral density and the Subsidence after Anterior Cervical Discectomy and Fusion. Clin Spine Surg. 2021;34(8):E450–7.
Soliman MAR, Aguirre AO, Kuo CC, Ruggiero N, Khan A, Ghannam MM, Rho K, Jowdy PK, Mullin JP, Pollina J. A novel cervical vertebral bone quality score independently predicts Cage Subsidence after Anterior Cervical Diskectomy and Fusion. Neurosurgery. 2023;92(4):779–86.
Ehresman J, Schilling A, Pennington Z, Gui C, Chen X, Lubelski D, Ahmed AK, Cottrill E, Khan M, Redmond KJ et al. A novel MRI-based score assessing trabecular bone quality to predict vertebral compression fractures in patients with spinal metastasis. J Neurosurg Spine 2019:1–8.
Ehresman J, Pennington Z, Schilling A, Lubelski D, Ahmed AK, Cottrill E, Khan M, Sciubba DM. Novel MRI-based score for assessment of bone density in operative spine patients. Spine J. 2020;20(4):556–62.
Kaiser JT, Reddy V, Lugo-Pico JG. Anatomy, Head and Neck: Cervical Vertebrae. In: StatPearls. edn. Treasure Island (FL) ineligible companies. Disclosure: Vamsi Reddy declares no relevant financial relationships with ineligible companies. Disclosure: Julian Lugo-Pico declares no relevant financial relationships with ineligible companies.: StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.; 2023.
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93(11):1057–63.
Song KJ, Choi BW, Ham DH, Kim HJ. Prognosis of hardware-related problems in Anterior Cervical Discectomy and Fusion with cage and plate constructs. World Neurosurg. 2020;134:e249–55.
Kast E, Derakhshani S, Bothmann M, Oberle J. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev. 2009;32(2):207–14. discussion 214.
Perez-Cruet MJ, Samartzis D, Fessler RG. Anterior cervical discectomy and corpectomy. Neurosurgery. 2006;58(4 Suppl 2):ONS. discussion ONS-359.
Wang Z, Mei J, Feng X, Deng C, Tian X, Lv J, Sun L. Low cervical vertebral CT value increased early subsidence of titanium mesh cage after anterior cervical corpectomy and fusion. J Orthop Surg Res. 2022;17(1):355.
Igarashi H, Hoshino M, Omori K, Matsuzaki H, Nemoto Y, Tsuruta T, Yamasaki K. Factors influencing Interbody Cage Subsidence following anterior cervical discectomy and Fusion. Clin Spine Surg. 2019;32(7):297–302.
Kao TH, Wu CH, Chou YC, Chen HT, Chen WH, Tsou HK. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg. 2014;134(10):1343–51.
Jin ZY, Teng Y, Wang HZ, Yang HL, Lu YJ, Gan MF. Comparative analysis of cage subsidence in Anterior Cervical Decompression and Fusion: Zero Profile Anchored Spacer (ROI-C) vs. conventional cage and plate construct. Front Surg. 2021;8:736680.
Wang T, Zhao Y, Cai Z, Wang W, Xia Y, Zheng G, Liang Y, Wang Y. Effect of osteoporosis on internal fixation after spinal osteotomy: a finite element analysis. Clin Biomech (Bristol Avon). 2019;69:178–83.
Zou D, Sun Z, Zhou S, Zhong W, Li W. Hounsfield units value is a better predictor of pedicle screw loosening than the T-score of DXA in patients with lumbar degenerative diseases. Eur Spine J. 2020;29(5):1105–11.
Zaman M, Shah A, Singal R, Kirmani A, Bhat AR, Singal RP. Role of Dual Energy X-ray Absorptiometry (DEXA) scan in the diagnosis of Chronic Low Back Pain - a prospective randomized controlled study in osteoporotic patients hospitalized in a Tertiary Care Institute. Maedica (Bucur). 2018;13(2):120–4.
Mao SS, Li D, Syed YS, Gao Y, Luo Y, Flores F, Child J, Cervantes M, Kalantar-Zadeh K, Budoff MJ. Thoracic quantitative computed tomography (QCT) can sensitively monitor bone Mineral metabolism: comparison of thoracic QCT vs lumbar QCT and dual-energy X-ray absorptiometry in detection of age-relative change in bone Mineral Density. Acad Radiol. 2017;24(12):1582–7.
Pennington Z, Ehresman J, Lubelski D, Cottrill E, Schilling A, Ahmed AK, Feghali J, Witham TF, Sciubba DM. Assessing underlying bone quality in spine surgery patients: a narrative review of dual-energy X-ray absorptiometry (DXA) and alternatives. Spine J. 2021;21(2):321–31.
Wang M, Mummaneni PV, Xi Z, Chang CC, Rivera J, Guinn J, Mayer R, Chou D. Lower Hounsfield units on CT are associated with cage subsidence after anterior cervical discectomy and fusion. J Neurosurg Spine 2020:1–8.
Lee JS, Son DW, Lee SH, Ki SS, Lee SW, Song GS, Woo JB, Kim YH. The Effect of Hounsfield Unit Value with Conventional computed tomography and intraoperative distraction on postoperative intervertebral height reduction in patients following stand-alone Anterior Cervical Discectomy and Fusion. J Korean Neurosurg Soc. 2022;65(1):96–106.
Bandirali M, Di Leo G, Papini GD, Messina C, Sconfienza LM, Ulivieri FM, Sardanelli F. A new diagnostic score to detect osteoporosis in patients undergoing lumbar spine MRI. Eur Radiol. 2015;25(10):2951–9.
Salzmann SN, Okano I, Jones C, Zhu J, Lu S, Onyekwere I, Balaji V, Reisener MJ, Chiapparelli E, Shue J, et al. Preoperative MRI-based vertebral bone quality (VBQ) score assessment in patients undergoing lumbar spinal fusion. Spine J. 2022;22(8):1301–8.
Haffer H, Muellner M, Chiapparelli E, Moser M, Dodo Y, Zhu J, Shue J, Sama AA, Cammisa FP, Girardi FP, et al. Bone quality in patients with osteoporosis undergoing lumbar fusion surgery: analysis of the MRI-based vertebral bone quality score and the bone microstructure derived from microcomputed tomography. Spine J. 2022;22(10):1642–50.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JL, LW, ZD, SZ, LW and YS contributed to the study conception and design. Material preparation, data collection and analysis were performed by JL, LW and SZ. The first draft of the manuscript was written by JL and LW, ZD, SZ, YS commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethics committee of West China Hospital, Sichuan University approved this study. Because this is a retrospective study, it was approved by the Ethics Committee of West China Hospital, Sichuan University to waive informed consent.
Consent for publication
Not applicable, our manuscripts do not contain any identifiable individual images or information.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, J., Wang, L., Deng, Z. et al. A novel cervical vertebral bone quality score can independently predict cage subsidence after anterior cervical corpectomy and fusion. BMC Musculoskelet Disord 25, 667 (2024). https://doi.org/10.1186/s12891-024-07791-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07791-6