Abstract
Background
This study retrospectively compared short-term clinical outcomes and complications of minimally invasive surgery transforaminal lumbar interbody fusion(MIS-TLIF)and endoscopic lumbar interbody fusion(Endo-LIF))for two-segmental lumbar degenerative disease, aiming to guide spine surgeons in selecting surgical approaches.
Methods
From January 2019 to December 2023, 30 patients were enrolled,15 in the MIS-TLIF group and 15 in the Endo-LIF group. All patients were followed up for more than 3 months after surgery and the following information was recorded: (1)surgery time, difference in hemoglobin between preoperative and postoperative, surgical costs, first time out of bed after operation, postoperative hospitalization time, postoperative complication; (2) ODI score (The Oswestry Disability Index), leg and back VAS score (Visual Analogue Scale), and lumbar vertebra JOA score (Japanese Orthopaedic Association Scores); (3) MacNab score at final follow-up to assess clinical outcome, CT to evaluate lumbar fusion.
Results
There were significant differences between the two groups regarding operation time and cost, with the MIS-TLIF group performing significantly better. Intraoperative bleeding was considerably less in the Endo-LIF group compared to the MIS-TLIF group. However, there were no significant differences in the time of the first postoperative ambulation, postoperative hospitalization time, and postoperative complications. There was no significant difference in preoperative VAS, ODI, and JOA between the two surgical groups There were no significant differences in VAS(leg), ODI, and JOA scores between the two groups before and at 1 day,7 days, 1 month, 3 months and final follow-up. However, at 1 day postoperatively, the VAS( back)score in the Endo-LIF group was lower than that in the MIS-TLIF group, and the difference was statistically significant. At the final follow-up, all patients achieved grade III and above according to the Bridwell criteria, and there was no significant difference between the two surgical groups compared to each other. According to the MacNab score at the final follow-up, the excellent rate was 80.00% in the Endo-LIF group and 73.33% in the MIS-TLIF group, with no significant difference between the two groups.
Conclusion
There was no significant difference in short-term efficacy and safety between Endo-LIF and MIS-TLIF for two-segment degenerative lumbar diseases. MIS-TLIF has a shorter operative time and lower costs, while Endo-LIF causes less tissue damage, blood loss, and early postoperative pain, aiding long-term recovery. Both MIS-TLIF and Endo-LIF are promising for treating two-segment lumbar degenerative disease. The choice of a surgical procedure depends on the patient’s financial situation, their ability to tolerate surgery, and the surgeon’s expertise.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Degenerative lumbar spine disease, a major cause of disability worldwide, includes lumbar spondylolisthesis, disc degeneration, and spinal stenosis, often causing lower extremity pain, fatigue, and low back and leg pain. Approximately 266 million people [1] suffer from lumbar degenerative disease every year, and it has also been demonstrated that lumbar degenerative disease is also associated with psychiatric disorders such as depression [2]. Surgical interventions for lumbar degenerative diseases with lower limb and low back pain yield better results than conservative treatments [3], benefiting both physical and mental health. Since Boucher [4] introduced the pedicle screw technique in 1959, transforaminal lumbar interbody fusion (TLIF) has become the standard [5] for spinal fractures, lumbar degenerative disease, infections, and deformities. Traditional TLIF surgery faces issues common to open surgery, such as large incisions and soft tissue trauma, which can cause liquefaction necrosis and postoperative low back pain.
With advancements in surgical techniques and minimally invasive concepts, Foley [6] proposed minimally invasive surgery transforaminal lumbar interbody fusion (MIS-TLIF). Compared to conventional TLIF, MIS-TLIF protects paraspinal structures, resulting in less trauma, bleeding, and quicker recovery [7]. However, MIS-TLIF has a limited workspace and field of view, and the dilatation cannula can cause tissue damage from muscle compression. Recently, with advances in spinal endoscopy, percutaneous endoscopic-assisted transforaminal lumbar interbody fusion (Endo-LIF) has emerged [8]. Besides its minimally invasive nature, Endo-LIF offers a clearer intraoperative view, avoiding vascular damage and facilitating safe decompression of the dural sac and nerve roots [9]. Clinical results of MIS-TLIF versus Endo-LIF for single-segment lumbar degenerative disease have been published [10]. Multi-segment interbody fusion is more complex and time-consuming than single-segment surgery, requiring higher operator skills. Clinical outcomes for two-segment lesions have not yet been reported. Therefore, this study aimed to compare the short-term efficacy of MIS-TLIF and Endo-LIF for two-segment lumbar degenerative disease.
Materials
Patient characteristics
We retrospectively analyzed 30 patients who underwent surgery for two-segment lumbar degenerative disease between January 2019 and December 2023. The type of surgery is determined through a mutual discussion between the doctor and the patient, with all procedures performed by the same doctor. Patients were divided into two groups based on the surgical approach: Endo-TLIF and MIS-TLIF.15 patients received MIS-TLIF and 15 patients received Endo-LIF. These included 22 females and 8 males, with a mean age of 59.67 years (43–76 years) and a mean postoperative hospitalization of 13.83 days (7–25 days). The surgical segments were L2-4 (2 patients), L3-5 (10 patients), and L4-S1 (20 patients). There was no significant difference between the MIS-TLIF group and the Endo-LIF group in terms of gender, age, and surgical segment (P > 0.05). Similarly, there was no significant difference in the preoperative diagnostic group between the MIS-TLIF and Endo-LIF groups (P > 0.05). The basic information of the patients is presented in Table 1.
Inclusion and exclusion criteria
The inclusion criteria were (1) persistent neurological symptoms after more than 3 months of conservative therapy; (2) Two-segment lumbar degenerative disease (lumbar disc herniation with instability; degree I or II spondylolisthesis based on radiography, CT(Computed tomography), or MRI (Magnetic Resonance Imaging); foraminal stenosis or central canal stenosis; cartilage endplate inflammation.
The exclusion criteria were (1) previous lumbar surgical treatment; (2) severe spinal deformity; (3) severe lumbar spinal stenosis(Schizas grade C and above) or severe lumbar instability with spondylolisthesis greater than degree II; (4) severe underlying disease that prevented surgical treatment; (5) tumor, infection, or severe osteoporosis;6. unwillingness or inability to participate in treatment and complete follow-up.
Surgical techniques
MIS-TLIF group
The surgical procedures were strictly performed as outlined in the text by Gu et al. [11]. ( Fig. 1, L4-S1)
56-year-old female with low back pain with right lower extremity pain for 6 months. (a): MRI of the lumbar spine showed deformed bulging and herniated discs at L4/5 and L5/S1, and lumbar spondylolisthesis at L4. (b, c): Transverse MRI showing L4/5 and L5/S1 disc herniation and L5/S1 spinal stenosis. (d): Intraoperative operation under Quadtrant channel. (e): Lateral X-ray after surgery. (f): CT review at the final follow-up showed an intact bone block and trabecular growth was seen between the implant block and the host bone
Endo-LIF group
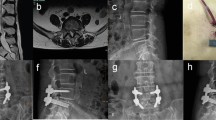
The surgical procedures were strictly performed as outlined in the text by He et al. [12]. (Fig. 2 L3- L5)
(a) 64-year-old woman with low back pain and bilateral lower extremity pain for 10 years. MRI of the lumbar spine shows L3 and L4 lumbar spondylolisthesis. (b, c): Transactional MRI showing bulging and herniated discs at L3-4 and L4-5 with spinal stenosis. (d, e, f, g): The cage was placed in L4/5 and L3/4, and the endoscopic view showed that the cage was placed in place and the nerve root decompression was complete. (h, i): Insertion of the nail bar system and proper repositioning. j: CT review at the final follow-up showed an intact bone block and trabecular growth was seen between the implant block and the host bone
Postoperative management
Patients in both groups were given the same postoperative treatment, and postoperative instructions were written by the surgeon. All patients were given symptomatic support treatment such as anti-inflammation and analgesia, nerve nutrition, and so on. Preoperative prevention measures included the prophylactic use of antibiotics within 24 h after surgery. Patients were also instructed to perform bed exercises and ankle pump exercises to prevent deep venous thrombosis. Patients were encouraged to wear a waist brace and get out of bed for daily activities starting on the second day after the operation. The dressing was changed every 3–5days after the operation, and incision sutures were removed 14 days after the operation. Patients were advised to gradually perform rehabilitation exercises, including strengthening the lumbar and dorsal muscles, as well as lower limb exercises.
Clinical and imaging evaluations.
Patients were clinically followed up at 1 day, 7 days, 1 month, 3 months, and at the end of the postoperative period through face-to-face interviews and telephone calls. To ensure consistency, all follow-ups were conducted and recorded by the same person. The perioperative parameters of the two groups of patients were compared, including the duration of the operation, the difference between preoperative and postoperative haemoglobin, the cost of the operation, first time out of bed after the operation, postoperative hospitalization time and the postoperative complications. Clinical outcomes were assessed by collecting leg and back VAS scores, lumbar vertebra JOA score, and ODI scores. A higher VAS score (maximum 10) indicates more severe pain, while a higher ODI score (maximum 50) indicates poorer quality of life, and the maximum total JOA score is 29, with lower scores indicating more significant dysfunction. The clinical efficiency was evaluated by the MacNab criteria. Fusion was evaluated based on CT findings and Bridwell grading at the final follow-up. The number of postoperative complications was counted to compare the difference in postoperative complications between the two surgical groups.
Statistical analysis
Continuous variables such as age, VAS score, ODI score, ODI, the duration of the operation, the difference between preoperative and postoperative haemoglobin, the cost of the operation, first time out of bed after the operation, postoperative hospitalization time were displayed as the mean ± standard deviation and were analyzed with the independent sample t-test for intergroup comparisons and the paired t-test for intragroup comparisons. Nominal data such as complications, MacNab criteria, and Bridwell grading were analyzed with the χ2 test or Fisher’s exact test. P value of < 0.05 was considered indicative of statistical significance. Statistical analysis was performed using IBM SPSS, version 25.0.
Results
Perioperative parameters
Preoperative and postoperative Hb differences, operative time, first time getting out of bed after operation, postoperative hospitalization time, operative cost, and postoperative complications in both groups are shown in detail in Tables 2 and 3. There was no significant difference between the two groups in terms of surgical segment, first postoperative time out of bed, length of hospitalization, and postoperative complications (P > 0.05). The duration of surgery in the Endo-LIF group was (437.87 ± 64.45) minutes, which was significantly longer than that in the MIS-TLIF group was (339.53 ± 71.85) minutes, with a significant difference (P < 0.05). The comparison of intraoperative bleeding, based on the difference between preoperative and postoperative hemoglobin levels, showed that the decrease in hemoglobin in the Endo-LIF group was significantly lower than in the MIS-TLIF group. This indicates that the Endo-LIF group experienced significantly less bleeding compared to the MIS-TLIF group, with a statistically significant difference. (P < 0.05).The hospitalization cost was (77,771.52 ± 10,431.07) yuan in the Endo-LIF group and (67,473.96 ± 11,358.68) yuan in the MIS-TLIF group, which was a significant difference (P < 0.05). Both groups had one case of postoperative wound infection, which healed after antibiotic treatment. In the Endo-LIF group, there was one case of epidural hematoma and infection with cage retropulsion. The patient underwent two separate surgeries and was successfully discharged.
Clinical follow-up parameters
Patients were followed up after surgery (Table 4). VAS(leg and back) scores and ODI were significantly lower in both surgical groups at all postoperative follow-up time points compared to preoperative (P < 0.05). Additionally, JOA scores significantly increased compared to preoperative levels (P < 0.05). There was no significant difference in preoperative VAS, ODI, and JOA between the two surgical groups (P > 0.05). There were no significant differences in VAS(leg), ODI, and JOA scores between the two groups before and at 1 day,7 days, 1 month, 3 months, and final follow-up. However, at 1 day postoperatively, the VAS (back) score in the Endo-LIF group was (4.07 ± 1.09) lower than that in the MIS-TLIF group (5.40 ± 1.60), and the difference was statistically significant (P = 0.02).Based on the Bridwell criteria, all patients achieved grade III and above, and there was no significant difference between the two surgical groups compared to each other (P > 0.05). Based on the MacNab score at the final follow-up, the excellent rate was 80.00% in the Endo-LIF group and 73.33% in the MIS-TLIF group, with no significant difference between the two groups(P > 0.05).
Discussion
Lumbar degenerative disease, common among the elderly, is the leading cause of low back pain. Low back pain is the most frequent pain and disability complaint among patients aged 65 years and older, and it is also highly prevalent in the second most common age group for low back pain [13]. An estimated $100 billion is spent annually worldwide on treating low back pain caused by degenerative lumbar spine conditions [14]. As the global population ages, it not only increases pain and disability for patients but also imposes a growing cost burden on healthcare systems and economies [15]. Lumbar fusion is an excellent solution for severe lumbar degenerative disease and is widely recognized by spine surgeons. Wong et al. [16] prospectively studied 198 patients and found a significantly lower complication rate with MIS-TLIF. It is attributed to less tissue trauma, lower blood loss, less drainage, and a smaller potential dead space. Several studies have also demonstrated that there is no statistically significant difference in the long-term clinical outcomes of MIS-TLIF compared with open TLIF [17], so MIS-TLIF is recognized by an increasing number of spine surgeons.
With advancements in endoscopic techniques and concepts, Osman et al. [18] first reported endoscopic transforaminal lumbar decompression, interbody fusion, and percutaneous pedicle screw internal fixation in 2012, leading to the development of Endo-LIF. He et al. [12] concluded that the Endo-LIF technique has the following advantages over the TLIF technique: (1) Endoscopic removal of the hyperplastic ligamentum flavum allows for more thorough decompression of the lateral recess and central areas. (2) Most spine surgeons are familiar with posterior lumbar surgery and can more easily overcome the learning curve of endoscopic techniques. (3) A shorter working channel makes it easier to control instruments, improving decompression efficiency and reducing operative time. (4) Endoscopic osteotomy is safer. (5) A nucleus pulposus that prolapses upward or downward can be removed by expanding the working area accordingly. Although postoperative follow-up data show that the Endo-LIF technique is as effective as the TLIF technique, Endo-LIF offers faster postoperative recovery, minimizes damage to the paraspinal muscles, and results in less intraoperative blood loss and shorter hospital stays compared to TLIF. Therefore, the authors concluded that Endo-LIF may be a reliable alternative to minimally invasive lumbar fusion. Endo-LIF significantly reduces blood loss and hospitalization time. It offers the advantages of less surgical injury, less blood loss, faster recovery, and early relief of postoperative back pain [19]. One article pointed out [10] that there is no significant difference in the short-term clinical efficacy and safety between Endo-LIF and MIS-TLIF for the treatment of single-segment degenerative lumbar spine disease, but no report has been seen about Endo-LIF and MIS-TLIF for the treatment of two-segment lumbar degenerative disease.We hope that our study will provide spine surgeons with valuable insights to aid in the selection of surgical methods for treating two-segment lumbar degenerative disease.
Numerous studies have shown that minimally invasive techniques in the treatment of lumbar degenerative diseases can effectively reduce postoperative pain and facilitate recovery [19, 21, 25, 27]. In our retrospective study, we compared the short-term clinical efficacy of Endo-LIF and MIS-TLIF in treating two-segment lumbar degenerative disease. There were no significant differences between the two groups regarding general surgical approach data, such as age, gender, preoperative diagnosis, and complications (P > 0.05). There was no significant difference in preoperative VAS, ODI, and JOA scores between the two surgical groups. There was no significant difference in VAS (leg), ODI, and JOA scores between the two groups on the first postoperative day (P > 0.05). This may be because patients in both groups were on bed rest on the first postoperative day. There were no significant differences in VAS, ODI, and JOA scores at 7 days, 1 month, 3 months after surgery, and the final follow-up (P > 0.05). At the final follow-up, all patients achieved varying degrees of fusion according to the Bridwell criteria, with no differences in fusion outcomes. Ito et al. [20]. concluded that intervertebral fusion typically occurs 2 years after surgery, with significant intervertebral bone growth occurring 3 to 5 years post-surgery. Due to regional and economic constraints, surgical patients in this study could not receive long-term follow-up beyond the final assessment. Therefore, the long-term fusion efficacy of the two techniques could not be further investigated, which is a limitation of the study. However, 1 day after surgery, the VAS(back) score in the Endo-LIF group was (4.07 ± 1.09) lower than that in the MIS-TLIF group (5.40 ± 1.60), with a statistically significant difference (P = 0.02). We conclude the MIS-TLIF procedure involves using an expanded cannula to expose the surgical field, which protects surrounding muscles but may put pressure on them. Muscles that have slipped out from beneath the cannula are often directly excised using an electrosurgical knife during the procedure. In the Endo-LIF procedure, the endoscope eliminates the need to address slipped muscles, and it theoretically causes less postoperative trauma than MIS-TLIF, which is more conducive to postoperative recovery and more in line with the concept of ERAS (Enhanced Recovery After Surgery) [21]. However, in studies comparing Endo-LIF and MIS-TLIF for the treatment of single-segment degenerative lumbar diseases, there was no significant difference in postoperative day 1 back pain VAS scores between the two groups. We believe this may be related to the increased number of surgical segments in these procedures. Over time, there were no significant differences in VAS, ODI, and JOA scores between the two groups, consistent with previous related studies. Song [10] et al. suggested that the lack of difference may be due to the identical screw placement in both surgeries, resulting in similar trauma from the screw insertion. Other studies have noted that gender differences in pain persist before and after surgical interventions for lumbar degenerative pathologies. The authors suggest that physiological, environmental, and economic factors may contribute to these differences, with females potentially being more sensitive to pain [22]. This paper did not consider the impact of gender on surgical outcomes, which is a limitation of the study.
Surgical treatment of multi-segment lumbar degenerative disease can be more complex and challenging compared to single segments [23]. In a retrospective study on the efficacy of Endo-LIF and MIS-TLIF for single-segment lumbar degenerative disease, Xu [24] et al. reported that the average durations of the procedures were 205.64 ± 56.2 min for Endo-LIF and 120.36 ± 30.56 min for MIS-TLIF. In our study, the operative times for Endo-LIF and MIS-TLIF were 437.87 ± 64.45 min and 339.53 ± 71.85 min, respectively, showing a significant difference (P < 0.01). The duration of the operation increased as the number of segments operated on increased.
We also believe the longer surgical time for Endo-LIF compared to MIS-TLIF may be due to the following reasons:1. Easier Access: MIS-TLIF allows relatively easy surgical access and the use of open tools, such as ultrasonic osteotomes, for managing the spinal canal and endplates. Endo-LIF, on the other hand, is less efficient due to the combination of drilling, fluoroscopy, and endoscopy.2. Fluoroscopy Time: MIS-TLIF offers the option of trans-channel nailing during the procedure, which reduces fluoroscopy time.3.Learning Curve: Endo-LIF, being a minimally invasive technique, has a steeper learning curve compared to MIS-TLIF, so it takes longer to achieve technical proficiency [25]. Minimally invasive multisegment lumbar fusion is more complex than single-segment lumbar fusion and is performed less frequently [26]. This explains the longer operation duration and the lower number of cases included in our study.
Although the Endo-LIF procedure had a longer duration compared to MIS-TLIF, there were significant differences (P < 0.05) in pre- and post-surgical Hb levels. Additionally, the time out of bed on the first postoperative day and the length of postoperative hospitalization was shorter for Endo-LIF compared to MIS-TLIF. Abuduwupuer et al. [27] found that, despite its shorter operative time, MIS-TLIF results in more intraoperative blood loss and longer postoperative hospitalization compared to Endo-LIF. Our results showed no statistically significant difference in time out of bed or length of hospitalization on the first postoperative day(P > 0.05). This may be due to the small sample size, which is a limitation of the study. Compared to MIS-TLIF, Endo-LIF resulted in significantly less intraoperative bleeding, with a statistically significant difference (P < 0.05). Due to limitations in surgical conditions, intraoperative hemorrhage during Endo-LIF is aspirated along with the flushing saline, making it difficult to accurately measure the exact amount of blood loss. Therefore, we used the difference between preoperative and postoperative Hb levels to estimate blood loss. This method may introduce some errors in accurately measuring blood loss, which is an area for improvement. Compared to MIS-TLIF, Endo-LIF minimizes excessive handling of tissue during the procedure and is performed under constant water pressure, which helps compress surrounding tissues and blood vessels to reduce bleeding. Additionally, endoscopic observation of tiny blood vessels allows for the use of a radiofrequency knife to preemptively stop bleeding, further reducing blood loss. The hospitalization cost for the Endo-LIF group was (77,771.52 ± 10,431.07) yuan, which was significantly higher than that of the MIS-TLIF group at (67,473.96 ± 11,358.68) yuan. The difference was statistically significant (P < 0.05). The hospitalization costs were calculated from the time of admission to discharge. All patients underwent identical preoperative laboratory and imaging tests. Postoperative orders were issued by the same doctor, and all patients received identical postoperative care. Therefore, we believe that the higher surgical costs in the Endo-LIF group may be attributed to the use of a radiofrequency knife, flushing saline, and specialized endoscopic instruments.
Recent reports indicate that the complication rate for endoscopic spinal fusion ranges from 0 to 28.6%, with most complications being minor and successfully treated [28]. In this study, although there was no statistically significant difference in the incidence of complications between the two surgical groups(P > 0.05), the Endo-LIF group still had a higher number of postoperative complications compared to the MIS-TLIF group. Specifically, the Endo-LIF group experienced one case of epidural hematoma, one case of cage retropulsion, and two cases of infection, whereas the MIS-TLIF group had only one case of postoperative infection. In the Endo-LIF group, one postoperative epidural hematoma occurred, requiring the patient to undergo additional spinal exploration and hematoma removal 6 days after surgery. It has been demonstrated that the probability of epidural hematoma after lumbar spine surgery is related to multi-segmental surgery and the duration of surgery [29]. The patient, a 45-year-old with normal preoperative coagulation, likely developed the postoperative epidural hematoma due to the multi-segmental surgery. The extensive duration and scope of the surgery may have caused significant damage to the venous plexus, leading to increased bleeding. Intraoperative water pressure aids in hemostasis, but its withdrawal post-surgery can cause some venous plexuses to reopen and bleed, increasing the incidence of postoperative epidural hematoma. Longer surgery duration, more surgical segments, and greater blood loss are also key factors in postoperative infections [23]. This could also explain the postoperative infections observed in both groups in our study. One patient in the Endo-LIF group developed a wound infection with fusion retropulsion and required an unplanned reoperation(URP) one week after the initial surgery. Surgical incision infection is the most common cause of URP in lumbar degenerative diseases [30]. It has been suggested [31] that prolonged surgical time and extended exposure of the surgical incision to cold temperatures can lead to surgical site infections and delayed wound healing. Endo-LIF requires continuous saline irrigation, which lowers body temperature and may increase the likelihood of postoperative wound infections. Therefore, in future Endo-LIF operations, we used thermostatic saline as the flushing fluid. Recent studies show that interleukin 6 is very useful for early diagnosis of postoperative wound infections, with levels of 26.0 pg/mL or higher indicating a surgical incision infection [32]. Early antibiotic treatment after diagnosis can greatly reduce the need for revisions and lower surgery costs for patients. Using intraoperative thermostatic saline irrigation and early postoperative interleukin 6 monitoring might have reduced the incidence of infection. We also believe that fusion loosening is related to intraoperative endplate damage and premature postoperative activity [33]. Endplate extrusion and collapse observed during URP may result from compression injury during the initial placement of the cage. Damage to the posterior edge of the endplate increases the height behind the fusion device, making retropulsion more likely. In lumbar fusion surgery, endplate injury ≥ 5 mm is a risk factor for cage retropulsion. Lumbar fusion takes about 3 months. Early removal of lumbar support and premature activity can affect lumbar stability and increase the risk of cage retropulsion. Peter et al. [26] found that the complication rate for single-segment and two-segment lumbar fusion surgery is relatively low. However, for three-segment fusion, the rate is comparable to open surgery. This study, limited by clinical data, does not discuss three-segment fusion outcomes. To obtain more accurate results for multi-segment fusion, further case collection is needed.
Therefore, based on our study’s conclusions, the Endo-LIF procedure offers several advantages over MIS-TLIF for treating two-segment lumbar degenerative disease: it theoretically causes less damage to muscles and soft tissues, results in reduced intraoperative bleeding, and and reduces early postoperative pain. These factors facilitate earlier postoperative rehabilitation exercises for patients and align more closely with the ERAS concept. However, the learning curve for Endo-LIF is steep, requiring a significant number of surgeries to achieve proficiency. Additionally, compared to MIS-TLIF, Endo-LIF has a relatively longer operation time and higher surgical costs. When considering this procedure, it’s important to fully assess the patient’s surgical tolerance and financial situation.
This study has some limitations. Although we followed strict inclusion and exclusion criteria for case selection, there may be a risk of selection bias. Interobserver bias in the measurement of the radiological parameters may have been present. The sample size was small and, thus, failed to show a difference in the complication rate. The follow-up time is short, so the safety and effectiveness of the operation cannot be fully evaluated. Although the safety and clinical efficacy of the two procedures and their respective advantages have been proven to some extent, but in the future, multicenter, large sample, and long-term follow-up studies are needed to further verify the clinical efficacy of endoscopic lumbar interbody fusion (Endo-LIF).
Conclusion
There was no significant difference in short-term safety and clinical efficacy between MIS-TLIF and Endo-LIF for treating two-segment lumbar degenerative disease. MIS-TLIF had shorter operative time and lower costs, while Endo-LIF caused less peripheral tissue damage, less intraoperative blood loss, and less early postoperative pain, which benefits long-term recovery. Therefore, we concluded that both MIS-TLIF and Endo-LIF are promising treatments for two-segment lumbar degenerative disease. The choice of a surgical procedure depends on the patient’s financial situation, their ability to tolerate surgery, and the surgeon’s expertise.
Data availability
All data generated or analysed during this study are included in this article.
References
Ravindra VM, Senglaub SS, Rattani A, et al. Degenerative lumbar spine disease: estimating Global Incidence and Worldwide volume. Global Spine J. 2018;8(8):784–94. https://doi.org/10.1177/2192568218770769.
Chen Z, Luo R, Yang Y, Xiang Z. The prevalence of depression in degenerative spine disease patients: a systematic review and meta-analysis. Eur Spine J. 2021;30(12):3417–27. https://doi.org/10.1007/s00586-021-06977-z.
Jacobs WC, Rubinstein SM, Koes B, van Tulder MW, Peul WC. Evidence for surgery in degenerative lumbar spine disorders. Best Pract Res Clin Rheumatol. 2013;27(5):673–84. https://doi.org/10.1016/j.berh.2013.09.009.
BOUCHER HH. A method of spinal fusion. J Bone Joint Surg Br. 1959;41–B(2):248–59. https://doi.org/10.1302/0301-620X.41B2.248.
Zhai WJ, Wang ZK, Liu HL, Qin SL, Han PF, Xu YF. Comparison between minimally invasive and open transforaminal lumbar interbody fusion for the treatment of multi–segmental lumbar degenerative disease: a systematic evaluation and meta–analysis. Exp Ther Med. 2024;27(4):162. https://doi.org/10.3892/etm.2024.12450. Published 2024 Feb 23.
Kambin P, Re: Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003; 28: S26-35. Spine (Phila Pa 1976). 2004 ; 29(5) 598–599. https://doi.org/10.1097/01.brs.0000112066.78935.74
Chen H, Zheng G, Bian Z et al. Comparison of minimally invasive transforaminal lumbar interbody fusion and endoscopic lumbar interbody fusion for lumbar degenerative diseases: a retrospective observational study. J Orthop Surg Res. 2023;18(1):389. Published 2023 May 27. https://doi.org/10.1186/s13018-023-03875-6
Hoogland T, van den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976). 2008;33(9):973–8. https://doi.org/10.1097/BRS.0b013e31816c8ade.
Ahn Y, Youn MS, Heo DH. Endoscopic transforaminal lumbar interbody fusion: a comprehensive review. Expert Rev Med Devices. 2019;16(5):373–80. https://doi.org/10.1080/17434440.2019.1610388.
Song Z, Zhu W, Zheng J, et al. Comparison of short-term efficacy of MIS-TLIF and Endo-LIF in the treatment of single-segment degenerative lumbar diseases. Front Surg. 2022;9:922930. https://doi.org/10.3389/fsurg.2022.922930. Published 2022 Sep 23.
Gu G, Zhang H, Fan G, et al. Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop. 2014;38(4):817–24. https://doi.org/10.1007/s00264-013-2169-x.
He LM, Chen KT, Chen CM, et al. Comparison of percutaneous endoscopic and open posterior lumbar interbody fusion for the treatment of single-segmental lumbar degenerative diseases[J]. BMC Musculoskelet Disord. 2022;23(1):329.
Bydon M, Alvi MA, Goyal A. Degenerative lumbar spondylolisthesis: definition, natural history, Conservative Management, and Surgical Treatment. Neurosurg Clin N Am. 2019;30(3):299–304. https://doi.org/10.1016/j.nec.2019.02.003.
Choi YS. Pathophysiology of degenerative disc disease. Asian Spine J. 2009;3(1):39–44. https://doi.org/10.4184/asj.2009.3.1.39.
Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine. 2019;31(1):1–14. https://doi.org/10.3171/2019.4.SPINE18915.
Wong AP, Smith ZA, Stadler JA 3rd, et al. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am. 2014;25(2):279–304. https://doi.org/10.1016/j.nec.2013.12.007.
Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. 2019;14(1):229. https://doi.org/10.1186/s13018-019-1266-y. Published 2019 Jul 22.
Osman SG. Endoscopic transforaminal decompression, interbody fusion, and percutaneous pedicle screw implantation of the lumbar spine: a case series report. Int J Spine Surg. 2012;6:157–66. https://doi.org/10.1016/j.ijsp.2012.04.001. Published 2012 Dec 1.
Zhu L, Cai T, Shan Y, Zhang W, Zhang L, Feng X. Comparison of clinical outcomes and complications between percutaneous endoscopic and minimally invasive transforaminal lumbar Interbody Fusion for degenerative lumbar disease: a systematic review and Meta-analysis. Pain Physician. 2021;24(6):441–52.
Ito Z, Imagama S, Kanemura T, et al. Volumetric change in interbody bone graft after posterior lumbar interbody fusion (PLIF): a prospective study. Eur Spine J. 2014;23(10):2144–9. https://doi.org/10.1007/s00586-014-3410-z.
Guo T, Ding F, Fu B, et al. Efficacy and safety of enhanced recovery after surgery (ERAS) protocols for patients undergoing minimally invasive transforaminal lumbar Interbody Fusion surgery: a systematic review and Meta-analysis. World Neurosurg. 2024;188:199–e2101. https://doi.org/10.1016/j.wneu.2024.05.133.
MacLean MA, Touchette CJ, Han JH, Christie SD, Pickett GE. Gender differences in the surgical management of lumbar degenerative disease: a scoping review. J Neurosurg Spine. 2020;32(6):799–816. https://doi.org/10.3171/2019.11.SPINE19896. Published 2020 Jan 31.
Li T, Shi L, Luo Y, Chen D, Chen Y. One-level or Multilevel Interbody Fusion for Multilevel lumbar degenerative diseases: a prospective Randomized Control Study with a 4-Year Follow-Up. World Neurosurg. 2018;110:e815–22. https://doi.org/10.1016/j.wneu.2017.11.109.
Xu H, Yu L, Xiao B, et al. Comparison of outcomes between endoscopic transforaminal lumbar Interbody Fusion and minimally invasive transforaminal lumbar Interbody Fusion in patients with single-level lumbar degenerative disease: a retrospective study. World Neurosurg. 2024;183:e98–108. https://doi.org/10.1016/j.wneu.2023.11.092.
Son S, Yoo BR, Lee SG, Kim WK, Jung JM. Full-Endoscopic versus Minimally Invasive Lumbar Interbody Fusion for Lumbar Degenerative Diseases: A Systematic Review and Meta-Analysis [published correction appears in J Korean Neurosurg Soc. 2022;65(6):875. https://doi.org/10.3340/jkns.2021.0168.e1]. J Korean Neurosurg Soc. 2022;65(4):539–548. doi:10.3340/jkns.2021.0168.
Passias PG, Bortz C, Horn SR, et al. Diminishing clinical returns of Multilevel minimally invasive lumbar Interbody Fusion. Spine (Phila Pa 1976). 2019;44(20):E1181–7. https://doi.org/10.1097/BRS.0000000000003110.
Haibier A, Yusufu A, Hang L, Abudurexiti T. Comparison of clinical outcomes and complications between endoscopic and minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative diseases: a systematic review and meta-analysis. J Orthop Surg Res. 2024;19(1):92. Published 2024 Jan 27. https://doi.org/10.1186/s13018-024-04549-7
Compagnone D, Mandelli F, Ponzo M, et al. Complications in endoscopic spine surgery: a systematic review. Eur Spine J. 2024;33(2):401–8. https://doi.org/10.1007/s00586-023-07891-2.
Wang ZP, Zhao XY, Li YZ, Guo CL, Zhang HW, Qin DP, et al. A meta-analysis of risk factors for symptomatic epidural hematoma after lumbar spine surgery. Chin J Spine Spinal Cord. 2022;32(10):919–29. https://doi.org/10.3969/j.issn.1004-406X.2022.10.08.
Du R, Li Z. Reasons analysis on unplanned reoperation of degenerative lumbar spine diseases. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(12):1637–41. https://doi.org/10.7507/1002-1892.202107040.
Aleem IS, Tan LA, Nassr A, Riew KD. Surgical Site infection Prevention following spine surgery. Global Spine J. 2020;10(1 Suppl):S92–8. https://doi.org/10.1177/2192568219844228.
Roch PJ, Ecker C, Jäckle K, et al. Interleukin-6 as a critical inflammatory marker for early diagnosis of surgical site infection after spine surgery [published correction appears in infection. 2024 Jun 13. Doi: 10.1007/s15010-024-02319-5]. Infect Published Online May. 2024;6. https://doi.org/10.1007/s15010-024-02271-4.
Xi J, Lu Q, Wang Y, Wang Y, Wang X, Lv P, Chen L, et al. Risk factors for cage retropulsion following transforaminal lumbar interbody fusion. Chin J Tissue Eng Res. 2024;28(9):1394. https://doi.org/10.12307/2023.785.
Acknowledgements
Can Zhuo and Yang Liu are the first co-authors and equally contributed to this study.
Haidan Chen and Huili Cai are the correspondences and equally contributed to this study.
Funding
Joint Fund for Innovation and Development of Natural Science Foundation of Hubei Province (2024AFD130).
Author information
Authors and Affiliations
Contributions
HC, HC and YL conceived the concept of the study. CZ and ZY contributed to the design of the research. All authors were involved in data collection. HT, LW, DY, SC and RZ analyzed the data. HC coordinated funding for the project. All authors edited and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Review Board of The First College of Clinical Medical Science of Three Gorges University. (Approval Number:2023-187-01). For all participating sites and was conducted following the Declaration of Helsinki. We obtained all necessary informed consent from all patients involved in the study, including consent to participate in the study where appropriate.
Consent for publication
Written informed consent for publication of their clinical details and/or clinical images was obtained from all study patients. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhuo, C., Liu, Y., Zhang, Y. et al. Comparison of the short-term efficacy of MIS-TLIF and Endo-LIF for the treatment of two-segment lumbar degenerative disease. BMC Musculoskelet Disord 25, 708 (2024). https://doi.org/10.1186/s12891-024-07815-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07815-1