Abstract
Background
Symptomatic Bochdalek hernias are found mainly in infants in respiratory distress and occur rarely in adults.
Case presentation
We report a rare case of Bochdalek hernia associated with developmental abnormalities in an adult who exhibited acute chest pain and dyspnea on exertion.
Conclusions
This case highlights the importance of the differential diagnosis of acute left-sided chest pain and antenatal examination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Bochdalek hernia (BH) is one of the most common diaphragmatic abnormalities in infants and is characterized by cyanosis, tachycardia, and asymmetric growth in the chest cavity. By contrast, symptomatic BH is rare in adults. Reduction of the herniated content back into the peritoneal cavity, repair of the hernia, and relief of the intestinal obstruction are important objectives of operative repair. We describe here a case involving a 19-year-old woman with BH who presented with acute paroxysmal left chest pain radiating to the epigastrium. She underwent a mesh-based patch repair and the herniated viscera were returned to the abdominal cavity.
Case presentation
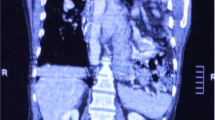
A 19-year-old woman presented with acute paroxysmal left chest pain radiating to the epigastrium of 4 days duration. She had a 10-year history of exertional dyspnea that was aggravated in the supine position, but no history of chest or abdominal trauma. She was misdiagnosed with a pulmonary abscess at another hospital, and the oral antibiotic treatment was ineffectual. Clinical examination on admission to our hospital revealed bowel sounds and decreased air entry in the left chest and that the abdomen appeared to be scaphoid. No obstructive gastrointestinal symptoms were observed. An X-ray revealed herniated loops of both the small and large intestines in the left hemithorax, which produced multiple lucent shadows and severely reduced lung space (Fig. 1, arrow). Computed tomography (CT) images showed that the bowel loops and fat passed through a defect in the posterolateral left hemidiaphragm (Fig. 2, arrow).
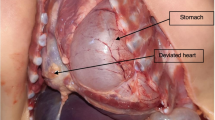
A left posterolateral thoracotomy was performed through the sixth intercostal space. The diaphragmatic defect was found along with herniation of the jejunum, ileum, ileocecal junction, appendix, and ascending and transverse colon. Pulmonary hypoplasia was also seen in the left lower lung lobe. We separated the adhesions around the foramen and within the pleural cavity. A laparotomy was subsequently performed through a median incision. During the operation, anomalies were found in intestinal rotation and fixation, and the total length of the jejunoileum was measured as 750 cm. The herniated viscera were returned to the abdominal cavity.
We performed a sublay patch repair of the left posterolateral diaphragmatic hernia using a Dacron patch (Balance Medical Technology Co., Ltd., Beijing, China). The procedure lasted for about 3 h. The patient had an uneventful postoperative period. An X-ray of the upper gastrointestinal tract with soluble iodine contrast at the 1-month follow-up showed that the repair was satisfactory (Fig. 3). A chest X-ray revealed that the left upper lung lobe was expanded completely (Fig. 4). After the surgery, the patient’s chest pain and dyspnea were relieved.
Discussion and conclusions
BH was first described by the Czech anatomist and pathologist, Vincent Alexander Bochdalek (1801–1883), in 1848 [1]. The condition is also known as a congenital posterolateral diaphragmatic hernia or pleuroperitoneal hernia. The abdominal viscera can herniate through into the thorax through the defect in the posterolateral part of the diaphragm. BH is one of the most common diaphragmatic abnormalities in infants and can cause respiratory distress in the newborn baby. The main clinical manifestations are cyanosis, tachycardia, and asymmetric growth in the chest cavity [2]. By contrast, BH is extremely rare in adults; its prevalence is 0.17–6% of all diaphragmatic hernias and it is almost always misdiagnosed.
Patients with BH can be asymptomatic or present with nonspecific gastrointestinal and respiratory signs and symptoms [3]. Other less common congenital hernias of the diaphragm in infants and children include hernias through the central tendon of the diaphragm, paraesophageal hernia, Morgagni hernia, and peritoneal pericardial hernia.
Radiological examination has great clinical value for the discovery of BH and exclusion of other differential diagnoses, especially when BH is an incidental finding or is asymptomatic and involves a small congenital diaphragmatic hernia [4]. Radiological findings can identify diaphragmatic defects, congenital pulmonary malformations, and lesions occupying the intrathoracic space. Surgery is recommended to avoid future strangulation in both symptomatic and asymptomatic adult patients [5]. The primary option is the transabdominal approach, which has lower morbidity compared with thoracotomy. However, a laparoscopic or open laparotomy may not be the best choice for chronically incarcerated giant BHs, in which extensive and severe adhesions are expected in the chest cavity. Therefore, the surgeon should choose an appropriate surgical method based on the situation of each patient.
We have described a rare case of a giant BH in an adult who presented with acute chest pain and dyspnea on exertion. The patient was initially misdiagnosed with a pulmonary abscess. After undergoing a mesh-based patch repair, the patient’s pain and dyspnea were relieved, and good therapeutic outcomes were achieved.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- BH:
-
Bochdalek hernia
- CT:
-
Computed tomography
References
Hu X, Liu B. Bochdalek hernia. Lancet (Lond, Engl). 2018;392(10141):60.
Sarac M, Bakal U, Tartar T, Canpolat S, Kara A, Kazez A. Bochdalek hernia and intrathoracic ectopic kidney: presentation of two case reports and review of the literature. Niger J Clin Pract. 2018;21(5):681–6.
Tan CQY, Chan DL, Chu F, Fisher OM. Rare presentation of a Bochdalek hernia in adulthood with incarcerated splenic flexure of the colon mimicking diverticulitis: a report and review. ANZ J Surg. 2018;89:1518–20.
Lee J, Nam SH, Kim SW, Hong JM, Kim D. Diaphragmatic hernia with isolated shoulder pain evoked by surfeit. Ann Transl Med. 2019;7(1):11.
Davakis S, Kordzadeh A, Charalabopoulos A. An extraordinary rare cause of acute dyspnea in an adult. Gastroenterology. 2019;156(6):e15–6.
Acknowledgements
We want to thank our patient for consenting to the publication of the article.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
GYM and LXY performed the literature review and formatted the manuscript. WWP participated in the diagnosis and treatment and supervised the writing of the article. CLQ performed the surgery and described the case. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Clearance was obtained from the Institutional Research and Ethics Review Committee of West China Hospital of Sichuan University for the publication of this case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gu, YM., Li, XY., Wang, WP. et al. A rare Bochdalek hernia in an adult: a case report. BMC Surg 21, 364 (2021). https://doi.org/10.1186/s12893-021-01357-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-021-01357-2