Abstract
Background
Surgery is the cornerstone of the treatment for primary retroperitoneal sarcoma (RPS). The purpose of this study was to establish a nomogram predictive model for predicting postoperative morbidity in primary RPS.
Methods
Clinicopathological data of patients who underwent radical resection from 2009 to 2021 were retrospectively analyzed. Risk factor analysis was performed using a logistic regression model, and modeling variables were selected based on Akaike Information Criterion. The nomogram prediction model was built on the basis of a binary logistic regression model and internally validated by calibration curves and concordance index.
Results
A total of 319 patients were enrolled, including 162 males (50.8%). 22.9% (n = 73) were over 65 years of age, and 70.2% (n = 224) had tumors larger than 10 cm. The most common histologic subtypes were well-differentiated liposarcoma (38.2%), dedifferentiated liposarcoma (25.1%) and leiomyosarcoma (7.8%). According to the Clavien–Dindo Classification, 96 (31.1%) and 31 (11.6%) patients had grade I–II complications and grade III–V complications, respectively. Age, tumor burden, location, operative time, number of combined organ resections, weighted resected organ score, estimated blood loss and packed RBC transfusion was used to construct the nomogram, and the concordance index of which was 0.795 (95% CI 0.746–0.844). and the calibration curve indicated a high agreement between predicted and actual rates.
Conclusions
Nomogram, a visual predictive tool that integrates multiple clinicopathological factors, can help physicians screen RPS patients at high risk for postoperative complications and provide a basis for early intervention.
Similar content being viewed by others
Background
Soft tissue sarcoma is a rare tumor, accounting for only about 1% of all solid tumors. Of these, 15% were retroperitoneal sarcomas (RPS) [1]. Surgical resection remains the mainstay of treatment for primary RPS [2]. Since RPS is asymptomatic in its early stages, the tumor burden is often huge at the time of diagnosis. Meanwhile, as reported by Gronchi [3] and Bonvalot [4], aggressive surgical strategies may help reduce the local recurrence of the disease. Therefore, an increasing number of high-volume sarcoma centers now advocate multivisceral resection (MVR). So the median number of combined organ resections for RPS in many hospitals may be as high as 4–5 [5]. The larger the surgery and the longer the operative time, the more complications there will be. The incidence of complications within 30 days after surgery has been reported to be more than 20% [6]. And the incidence of serious postoperative complications is as high as about 15%, and the rate of unplanned reoperations exceeds 10% [7]. In contrast, the proportion of unplanned reoperations for routine general surgery was only 3.5% [8].
A number of studies focused on the perioperative safety of RPS, and age, tumor burden, number of combined organ resections, and packed RBC transfusion have been reported as risk factors for postoperative morbidity [6, 7, 9]. However, there is no predictive tool at present that integrates multiple clinicopathological factors to predict postoperative complications.
The nomogram prediction model, which converts complex regression equations into visual graphs for patient assessment, is gradually gaining more and more attention and application in medical research and clinical practice. There are many high-quality nomogram prediction models for primary RPS, but the primary endpoint of these studies is long-term prognosis [3, 10, 11], and there is currently no nomogram prediction model for postoperative complications alone.
Therefore, the purpose of this study was to establish a nomogram prediction model for postoperative complications in patients with primary RPS, thereby providing a more accurate tool that would help clinicians involved in patient care and clinical research.
Methods
Patients
All patients with RPS who underwent curative surgery in the Shanghai Public Health Clinical Center, Fudan University, Shanghai, China from August 2009 to December 2021 were included. The inclusion criteria were as follows: (1) primary disease, (2) histologically confirmed sarcoma, (3) tumors originating from retroperitoneum, and (4) complete clinical pathological information and follow-up information. Patients with Ewing sarcoma, rhabdomyosarcoma, desmoid sarcoma, gynecologic sarcoma, or gastrointestinal stromal tumor were excluded. This study was approved by the Ethics Committee of Shanghai Public Health Clinical Center and was conducted in accordance with the Declaration of Helsinki.
Surgical procedure
All surgeries were performed by the multidisciplinary team for soft tissue sarcoma at Zhongshan Hospital Affiliated to Fudan University. Well differentiated liposarcoma and low-grade dedifferentiated liposarcoma are mainly local recurrences, so we implement a more aggressive surgical strategy (even if the surrounding organs of the tumor are not violated by the naked eye, they will be resected together); for high-grade dedifferentiated liposarcoma, If it is evaluated that there is the invasion of surrounding organs, complete radical resection should be attempted, and combined organ resection should also be performed; leiomyosarcoma often presents as a tumor with clear borders, and if the surrounding organs invade the adjacent units of the tumor, it should be preserved; for pleomorphic undifferentiated sarcoma, malignant peripheral nerve sheath tumor, and solitary fibrous tumor, complete resection with negative margins is enough.
Clinicopathologic evaluation
We collected the baseline characteristics that might affect the patient's prognosis such as gender, age, tumor burden, and histologic subtypes. Surgery-related indicators such as operative time, intraoperative blood loss, and the number of combined organ resections were also collected. Among them, the physical status of patients before anesthesia was assessed according to the American Society of Anesthesiologists Physical Status (ASA score) [12]. Tumor burden was the sum of the maximum diameters of all tumors in the patient. According to the 2020 World Health Organization pathological classification, the pathological types were classified as follows: (1) well-differentiated liposarcoma; (2) dedifferentiated liposarcoma; (3) leiomyosarcoma; (4) solitary fibroma; and (5) Others [13]. Meanwhile, according to the French Federation of Centers for the Fight against Cancer (FNCLCC) criteria, tumors were graded into I, II, and III [13]. Complete resection was defined as grossly negative margins, including both R0 and R1 resections. In 2017, realizing that the removal of specific organs may mean more complications, the Transatlantic RPS Working Group scored the different organs removed, as follows: Adrenal gland, aortocaval lymph nodes, appendix, gallbladder, inguinal ligament, omentum, psoas fascia, and skin are 0 points; Adnexa and/or uterus, bladder, bone, diaphragm,
distal pancreas, duodenum or duodenojejunal flexure, femoral/sciatic/obturator nerve or lumbar/sacral nerve root, iliac artery and/or aorta, iliac vein and/or IVC, kidney, left colon and/or rectum, liver, lung, parietal muscles, pericardium, posterior vaginal wall, prostate (with or without seminal vesicle), psoas muscle, right colon, small bowl, spleen, stomach, testis and/ or spermatic cord and/or vas deferens, and ureter (complete or partial resection not associated with nephrectomy) is 1 point; pancreaticoduodenectomy is 2 points [7]. According to the above scoring criteria, we scored each patient's organ resection.
Postoperative complications within 30 days were the primary endpoint of this study, and were classified according to the Clavien–Dindo Classification [14] as follows: I, abnormal conditions not requiring medical therapy or surgery, endoscopy, and radiation therapy; II, complications requiring medical therapy other than Level I complications; III, complications requiring surgery, endoscopy, or radiation therapy Complications; IV, life-threatening complications; V, postoperative death. Among them, grade III or above was defined as serious postoperative complications.
Statistical analyses
Overall survival was defined as the time from surgery to death or loss to follow-up, and we used the Kaplan–Meier method to calculate the overall survival rate. Categorical variables were described as numbers and percentages and compared using Fisher's exact test or Pearson Chi-square. Continuous variables were described by means and standard deviations and compared using an independent sample t-test. Univariate analysis were performed using binary logistic regression, and variables with p < 0.05 were further included in multivariate analysis. Binary logistic regression was also used for Multivariate analyses.
For variable selection, all clinicopathological variables were included and a backward procedure based on the Akaike Information Criteria (AIC) was applied [15]. A nomogram based on a multivariate logistic model was then built. Discrimination was assessed using Harrell C's Concordance Index (c-index). Means and 95% confidence intervals were calculated and plotted for each subgroup. Decision curve analysis (DCA) was used to assess the clinical potential application value of the nomogram.
All tests were two-tailed and P < 0.05 was considered statistically significant. All data were analyzed using SPSS 22.0 (SPSS Inc., Chicago, IL, USA) and R 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org/).
Results
Baseline characteristics
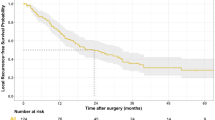
A total of 319 patients were enrolled, and the mean follow-up time for all patients was 45 (range, 1–140) months. 5-year overall survival rate was 63.0 (95%CI, 56.3–69.7) % (Fig. 1). Baseline characteristics of patients and tumors are listed in Table 1. The proportions of men and women were similar (50.8% vs. 49.2%), as were the proportions of symptomatic and asymptomatic patients (43.3% vs. 56.7%). 22.9% of patients were older than 65 years, and 95 patients (29.8%) had a tumor burden greater than 10 cm. Among the histologic subtypes, well-differentiated liposarcoma, dedifferentiated liposarcoma, leiomyosarcoma, and solitary fibroma accounted for 38.2%, 25.1%, 16.3%, and 7.8%, respectively. 31 patients (9.7%) had multifocal disease. 7.8% (n = 25) of patients had received radiotherapy, and 11.0% (n = 35) had received chemotherapy.
Table 2 presents information related to the surgical procedure. The vast majority of patients underwent open surgery (98.1%) and achieved complete tumor resection (96.9%). 51.1% (n = 163) of patients received more than one combined organ resection, with the most frequently resected organs being the colon (47.3%), kidney (43.6%) and adrenal gland (18.2%). As for the weighted resected organ score, 28.2% (n = 90) of the patients had a score of 0, 25.3% (n = 81) of the patients had a score of 1, and about half of the patients (46.5%) had a score of greater than 1. 90 patients (n = 28.2%) had an operative time more than 4 h, and about half (48.6%) had intraoperative blood loss estimated to be more than 400 ml. 31.3% (n = 100) of patients received packed RBC transfusion. The median postoperative hospital stay for all patients was 18.4 days. The overall complication rate was 42.3%, with 31.1% of grade I–II complications. The serious complication rate was 11.6%, and the most common adverse events were bowel anastomotic leak/fistula (n = 6), sepsis(n = 5), and bleeding/hematoma(n = 4) (Table 3). Six postoperative death, three of them died of bowel anastomotic leak/fistula, one died of sepsis, one died of severe intra-abdominal infection, and one died of myocardial infarction. The 30-, 60-, and 90-day mortality rates were 0.9 (95%CI, 0.3–1.5) %, 2.2 (95%CI, 0.6–3.8)%, and 2.8 (95%CI, 1.0–4.6)%, respectively.
Feature selection
To select the best variables for the predictive model, we first performed a risk factor analysis (Table 4). Univariate analysis indicated age > 65 years (p = 0.015), tumor burden > 10 cm (p < 0.001), pathological type (p = 0.046), number of combined organ resections > 1 (p < 0.001), weighted resected organ score (continuous, p < 0.001), operation time > 4 h (p < 0.001), estimated blood loss > 400 ml (p < 0.001) and packed RBC transfusion (p < 0.001) were risk factors for complications. We further included the above risk factors in multivariate analysis. Through multivariate analysis, we found that number of combined organ resections > 1 (HR = 2.864, p = 0.012), weighted resected organ score (HR = 2.041, p < 0.001) and operation time > 4 h (HR = 2.074, p = 0.032) were independent risk factors for complications.
A backward stepwise selection was then performed with all clinicopathological factors using a likelihood ratio test with AIC as the stopping rule. Age, tumor burden, location, operative time, number of combined organ resections, weighted resected organ score, estimated blood loss and packed RBC transfusion was selected. In addition to location, all other variables have statistical differences in univariate analysis.
Nomogram development and validation
We developed a nomogram prediction model based on binomial logistic regression with the selected variables above (Fig. 2). In this nomogram prediction model, each clinicopathological risk factor corresponded to a score. The total score could be obtained by summing the scores of the above seven indicators, and the probability of postoperative complications for patients could be inferred from the total score.
The calibration curve in Fig. 3 shows that the predicted postoperative complication probability is highly consistent with the actual probability. And the Harrell C-index for the nomogram was 0.795 (95% CI 0.746–0.844).
As illustrated in Fig. 4, the model demonstrated a significant positive net benefit from the risk of postoperative complication, indicating its great clinical practical value in predicting postoperative complications.
Discussion
Surgery remains the most fundamental treatment for primary RPS [2], which often requires combined multiple organ resection. However, the occurrence of postoperative complications not only prolongs the postoperative hospital stay but also increases the healthcare burden [16]. Therefore, it is particularly important to be able to identify patients at high risk of complications and to intervene early. Consistent with previous studies, we found that age, tumor burden, and operation time were risk factors for postoperative complications in RPS patients. Further, we developed the first nomogram prediction model with selected clinicopathological factors to accurately predict the probability of postoperative complications in patients with primary RPS.
Age has long been a risk factor for postoperative complications. A study by the Transatlantic RPS Working Group on the perioperative safety of 1007 patients with primary RPS also found that age was an independent risk factor for serious postoperative complications [5]. Sourrouille et al. also noted that individuals over 70 years of age undergoing RPS had a mortality rate of 8% and a serious postoperative complication rate of 32%. However, it is noteworthy that the 5-year recurrence-free survival rate of elderly patients can also reach 52% [17]. Therefore, age is not a contraindication to RPS surgery. Some insights may be drawn from the nomogram prediction model in this study. If a patient older than 65 years with a tumor burden less than 10 cm, when the operative time is greater than 4 h, estimated blood loss > 400 ml, and packed RBC transfusion, the patient’s total score was 252 points, meaning the likelihood of postoperative complications was greater than 70%. On the contrary, if this patient shortened the operation time, effectively reduced bleeding, and did not have blood transfusions, the incidence of postoperative complications would be only about 25%. The advantage of MVR lies in the complete resection of the chamber, which not only improves the local control but also reduces the prolonged operation time and increased blood loss in some patients due to the precise dissection of organs (such as renal vessels) [18]. Thus, contrary to previous understanding, an aggressive surgical strategy may also lead to better short-term prognostic outcomes in selected elderly patients.
Although estimated blood loss and packed RBC transfusion were not independent risk factors for postoperative complications in multivariate analysis, they were also included in this model. Intraoperative blood loss can lead to physiologic fluid shifts, coagulopathy, antibiotic dilution, and the need for transfusions [19]. Also, the detection and management of bleeding points will increase the operative time. Therefore, in addition to adequate preoperative preparations, a visit to an experienced high-volume sarcoma center is especially crucial as a relatively rare disease. As for packed RBC transfusion, our previous reports on the safety of surgery for retroperitoneal solitary fibroids also identified risk factors for postoperative complications [20]. We suggest that postoperative immune disturbances induced by blood transfusion may be a mechanism leading to poor prognosis [21].
The present study has the following shortcomings. First, as a retrospective study, selection bias is inevitable. Second, the nomogram prediction model developed in this study, although internally validated well, needs further external verification to confirm its practicability. Third, many recent studies have reported that preoperative nutritional indicators are also influential factors of complications after RPS, such as preoperative albumin, lymphocytes and CRP, but nutritional indicators were not included in this study due to the lack of data.
Conclusions
In conclusion, this study is the first to establish a predictive model of nomogram using high flow centers to predict postoperative complications in patients with primary RPS, providing a reference for preoperative counseling, selection of patients at high risk for complications, and early intervention.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- RPS:
-
Retroperitoneal sarcoma
- MVR:
-
Multivisceral resection
- ASA:
-
The American Society of Anesthesiologists Physical Status
- FNCLCC:
-
The Federal National Cancer Center
- AIC:
-
Akaike Information Criteria
- c-index:
-
Harrell C's Concordance Index
- DCA:
-
Decision curve analysis
References
Chia CS, Tan WJ, Wong JF, Tan GH, Lim C, Wang W, Sin EI, Tham CK, Soo KC, Teo MC. Quality of life in patients with peritoneal surface malignancies after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Eur J Surg Oncol. 2014;40:909–16.
Swallow CJ, Strauss DC, Bonvalot S, Rutkowski P, Desai A, Gladdy RA, Gonzalez R, Gyorki DE, Fairweather M, van Houdt WJ, et al. Management of Primary Retroperitoneal Sarcoma (RPS) in the adult: an updated consensus approach from the Transatlantic Australasian RPS Working Group. Ann Surg Oncol. 2021;28:7873–88.
Gronchi A, Miceli R, Shurell E, Eilber FC, Eilber FR, Anaya DA, Kattan MW, Honoré C, Lev DC, Colombo C, et al. Outcome prediction in primary resected retroperitoneal soft tissue sarcoma: histology-specific overall survival and disease-free survival nomograms built on major sarcoma center data sets. J Clin Oncol. 2013;31:1649–55.
Bonvalot S, Rivoire M, Castaing M, Stoeckle E, Le Cesne A, Blay JY, Laplanche A. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol. 2009;27:31–7.
Gronchi A, Strauss DC, Miceli R, Bonvalot S, Swallow CJ, Hohenberger P, Van Coevorden F, Rutkowski P, Callegaro D, Hayes AJ, et al. Variability in patterns of recurrence after resection of primary retroperitoneal sarcoma (RPS): a report on 1007 patients from the multi-institutional collaborative RPS Working Group. Ann Surg. 2016;263:1002–9.
Judge SJ, Lata-Arias K, Yanagisawa M, Darrow MA, Monjazeb AM, Kirane AR, Bold RJ, Canter RJ, Canter DJ. Morbidity, mortality and temporal trends in the surgical management of retroperitoneal sarcoma: an ACS-NSQIP follow up analysis. J Surg Oncol. 2019;120:753–60.
MacNeill AJ, Gronchi A, Miceli R, Bonvalot S, Swallow CJ, Hohenberger P, Van Coevorden F, Rutkowski P, Callegaro D, Hayes AJ, et al. Postoperative morbidity after radical resection of primary retroperitoneal sarcoma: a report from the transatlantic RPS working group. Ann Surg. 2018;267:959–64.
Birkmeyer JD, Hamby LS, Birkmeyer CM, Decker MV, Karon NM, Dow RW. Is unplanned return to the operating room a useful quality indicator in general surgery? Arch Surg. 2001;136:405–11.
Bonvalot S, Miceli R, Berselli M, Causeret S, Colombo C, Mariani L, Bouzaiene H, Le Péchoux C, Casali PG, Le Cesne A, et al. Aggressive surgery in retroperitoneal soft tissue sarcoma carried out at high-volume centers is safe and is associated with improved local control. Ann Surg Oncol. 2010;17:1507–14.
Ardoino I, Miceli R, Berselli M, Mariani L, Biganzoli E, Fiore M, Collini P, Stacchiotti S, Casali PG, Gronchi A. Histology-specific nomogram for primary retroperitoneal soft tissue sarcoma. Cancer-Am Cancer Soc. 2010;116:2429–36.
Anaya DA, Lahat G, Wang X, Xiao L, Pisters PW, Cormier JN, Hunt KK, Feig BW, Lev DC, Pollock RE. Postoperative nomogram for survival of patients with retroperitoneal sarcoma treated with curative intent. Ann Oncol. 2010;21:397–402.
Horvath B, Kloesel B, Todd MM, Cole DJ, Prielipp RC. The evolution, current value, and future of the American Society of Anesthesiologists Physical Status Classification System. Anesthesiology. 2021;135:904–19.
Sbaraglia M, Bellan E, Dei TA. The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives. Pathologica. 2021;113:70–84.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Akaike, H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974; 19(6): 716-723.
Tirotta F, Parente A, Hodson J, Desai A, Almond LM, Ford SJ. Cumulative burden of postoperative complications in patients undergoing surgery for primary retroperitoneal sarcoma. Ann Surg Oncol. 2021;28:7939–49.
Sourrouille I, Macovei R, Faron M, Le Péchoux C, Mir O, Adam J, Dumont S, Terrier P, Le Cesne A, Honoré C. Long-term outcome after surgery for a localized retroperitoneal soft tissue sarcoma in elderly patients: results from a retrospective, single-center study. Ann Surg Oncol. 2018;25:2201–8.
Bonvalot S, Raut CP, Pollock RE, Rutkowski P, Strauss DC, Hayes AJ, Van Coevorden F, Fiore M, Stoeckle E, Hohenberger P, Gronchi A. Technical considerations in surgery for retroperitoneal sarcomas: position paper from E-Surge, a master class in sarcoma surgery, and EORTC-STBSG. Ann Surg Oncol. 2012;19:2981–91.
Swoboda SM, Merz C, Kostuik J, Trentler B, Lipsett PA. Does intraoperative blood loss affect antibiotic serum and tissue concentrations? Arch Surg. 1996;131(1165–1171):1171–2.
Zhuang A, Fang Y, Ma L, Lu W, Tong H, Zhang Y. Postoperative morbidity after radical resection of retroperitoneal solitary fibrous tumor. Front Surg. 2022;9: 833296.
Goldfarb Y, Sorski L, Benish M, Levi B, Melamed R, Ben-Eliyahu S. Improving postoperative immune status and resistance to cancer metastasis: a combined perioperative approach of immunostimulation and prevention of excessive surgical stress responses. Ann Surg. 2011;253:798–810.
Acknowledgements
We would like to thank our patients, without whom this study would not be possible.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
ABZ, YJC and LJM developed the concept of the article. ABZ and YF developed the design and methodology. HY, YJC and WQL contributed to the manuscript revision. ABZ and YHZ contributed to the collection and analysis of clinical data. ABZ, YZ and HXT contributed to the drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shanghai Public Health Clinical Center, the authorization number is 2022-S058-05, and was carried out following the Declaration of Helsinki. All enrolled patients signed an informed consent form for data collection during their hospitalization.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhuang, A., Chen, Y., Ma, L. et al. Development and validation of a nomogram for predicting morbidity in surgically resected primary retroperitoneal sarcoma. BMC Surg 23, 42 (2023). https://doi.org/10.1186/s12893-023-01941-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-01941-8