Abstract
Background
Benign prostatic hyperplasia (BPH) is a prevalent urological disease in elderly males. However, few studies have estimated the temporal and spatial distributions of the BPH burden in male adults aged 60 years and over at the global, national, and regional scales.
Methods
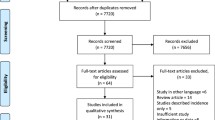
Leveraging the Global Burden of Disease, Injuries, and Risk Factors Study, we estimated the global epidemiological trends in the prevalence, incidence, and disability-adjusted life-years (DALYs) of BPH in 204 countries and 21 regions and 5 sociodemographic index (SDI) regions in males aged 60 years and over between 1990 and 2019. The average annual percentage changes (AAPCs) in age-specific rates were estimated to quantify overall trends. We estimated the contribution of population aging and epidemiological alterations in disease burden via composition analysis.
Results
Over the past three decades, the global prevalent cases, incident cases and DALYs of BPH have increased, ranging from 118.78 to 121.22%. The global number of prevalent BPH cases reached 79 million in people aged 60 years and older in 2019. The prevalence, incidence, and DALYs rates gradually increased, with AAPCs of 0.02, 0.02, and 0.01, respectively. Low-middle, middle, and low SDI regions experienced rapid increases in the number of prevalent cases of BPH. In 2019, China, India, and United States of America bore the largest burden of prevalent cases among people aged 60 years and over. The three regions with the highest prevalence rates of BPH were Eastern Europe, Central Latin America, and Andean Latin America. The increased prevalence was attributed to population growth (94.93%), epidemiological changes (3.45%), and aging (1.62%), globally.
Conclusions
BPH is a global health issue that imposes substantial economic burdens on most countries, particularly males aged 60 years and over. Effective health decisions are imperative for BPH prevention and treatment.
Similar content being viewed by others
Background
Benign prostatic hyperplasia (BPH) has become an emerging concern in male health with the aging population and changing lifestyle. BPH is characterized by an enlarged prostate that can cause symptoms linked to the bladder, urinary tract or kidney, such as partial or complete urethral blockage [1]. An enlarged prostate can hinder urinary output, leading to lower urinary tract symptoms (LUTS) [2,3,4]. In 2019, the age-standardized prevalence of BPH was 2480 (95% uncertainty interval [UI]: 1940–3090) per 100,000 people globally [5]. In the U.S., the direct expenditure attributed to treatment, excluding outpatient drugs, reached $1.1 billion in 2000 [6]. Given the profound social and medical implications of the BPH burden, further analysis of its long-term trend is imperative.
Aging is an important determinant of the development of BPH [7,8,9]. Globally, a meta-analysis including 30 epidemiological studies estimated an approximately 26% pooled prevalence of BPH in older men between 1990 and 2016 [10]. In China, a meta-analysis based on epidemiological surveys reported a pooled prevalence of 36.6% among men aged 40 years and older between 1989 and 2014 [11]. In addition to increasing the risk of acute urinary retention, BPH and LUTS significantly affect quality of life. A pilot study based on the International Prostatism Symptom Score (IPSS) revealed that older European men, coupled with LUTS and BPH, had an average score of 4.14 on items related to quality of life, indicating a worse condition [12]. This finding was supported by the American Urological Association Symptom Index [13]. Furthermore, BPH severity may lead to sleep disorders due to the occurrence of nocturia (frequently awakening to urinate at night). In a prior study, researchers reported that Nocturia-specific Quality of Life (N-QoL) scores were negatively associated with the frequency of nighttime voiding [14]. Older males also suffer from multiple chronic diseases, and these comorbidities increase the incidence risk and decrease the therapeutic effect of BPH. For example, among 547 patients who reported BPH, those who were diagnosed with depression had higher AUS-AI scores, and their odds of having moderate and even severe LUSTs were three times greater than those of those without depression in a longitudinal study [15]. Although a growing body of studies has elucidated the association between BPH and impaired quality of life, the current evidence remains heterogeneous due to contextual differences in various countries and regions. Therefore, a comprehensive analysis that compiles global metrics is warranted.
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) synthesizes global, national, and regional epidemiological data via a validated estimation framework, standardized procedure, and advanced analysis methods to identify epidemiological trends and conduct comparisons during specific periods stratified by cause, sex, age group and geographical location [16,17,18]. In this study, we aimed to estimate the number, prevalence, incidence, and disability-adjusted life years (DALYs) of BPH among older people aged between 60 and 90 years at the global, regional, and national scales via a GBD study from 1990 to 2019. We also assessed the proportions attributable to aging, population and epidemiological factors through a decomposition analysis.
Methods
Study data
The study data were collected and downloaded from the GBD 2019, which was integrated and published by the Institute for Health Metrics and Evaluation at the University of Washington, USA. The GBD 2019 offers rough estimates and 95% UI on cause-specific prevalence, incidence, and disability for 369 diseases and injuries, alongside 87 risk factors, in 204 countries and territories between 1990 and 2019 [19]. The GBD 2019 has been widely studied for its epidemiological description of and trends in diseases, prediction of cases, estimation of health loss and economic burden, and assessment of health disparities [20,21,22]. All the data can be found on the Global Health Data Exchange (GHDx) website.
The definition of BPH was based on the clinical diagnosis using the codes of the International Classification of Diseases (ICD) [23]. The ICD-9 codes used were 600, 600.0, 600.1, 600.2, 600.3 and 600.9, and the ICD-10 codes used were N40, N40.0, N40.1, N40.2, N40.3 and N40.9. The complications associated with BPH were not considered in this analysis because these diseases were mapped to other forms of GBD definitions, such as kidney stones. According to the GBD 2019 design, BPH incidence was estimated only for nonfatal health loss because fatal complications were grouped into other types of conditions and mortality attributed to these complications should not be recalculated. Because the WHO defines older people as those aged 60 years and over, we included people aged between 60 and 90 years [24]. The age stratification was divided into 5-year intervals starting from 60 years.
Statistical analysis
We procured annual measures encompassing the numbers and rates of prevalence, incidence, and DALYs. Prevalence refers to the total number of cases of a disease in a population at a given time, whereas incidence refers to the number of new cases that develop in a specific period. DALYs measure the overall disease burden, expressed as the number of years lost due to ill health, disability, or early death. The detailed data processing and statistical modeling methods used were described previously [19]. In brief, DisMod-MR V2.5 software and meta-regression-Bayesian, regularized, trimmed (MR-BRT) software were used to estimate the metrics. The UI was ascertained for each metric via posterior distributions after 1000 posterior draws, ranging from the 25th and 975th order values. However, we used the aggregated data rather than the original data to estimate the burden of diseases, increasing potential bias.
The sociodemographic index (SDI), a composite indicator used to assess social and population development in a country or region, is derived from parameters such as the fertility rate, education level, and per capita income. With a range from 0 to 1, higher SDI values denote superior socioeconomic development. Furthermore, the SDI is correlated with epidemiological patterns of disease and mortality [25]. The countries and regions included in the GBD 2019 study were generally categorized into five grades (high, high-middle, middle, low-middle, and low). In this study, we further examined the associations of BPHs with various SDI regions over time.
We employed joinpoint regression modeling to investigate alterations in BPH epidemiology trends at global, regional, and national scales [26]. This method can identify significant points where the slopes of trends change, and then the periods can be divided into multiple time intervals on the basis of the locations of the observed points. We then calculated the epidemiological trends for each time interval, represented via average annual percentage changes (AAPCs) and their 95% CIs [27]. The total asymptotic significance was ascertained via the Bonferroni correction and Monte Carlo permutation method, which was applied to 4499 datasets of random permutations. The AAPCs represent the magnitude of annual changes. Negative AAPCs denote a downward epidemiological trend, whereas positive AAPCs denote an upward epidemiological trend. In detail, AAPC is determined by first estimating the joinpoint model that best fits the data. The AAPC for any fixed interval is then computed as a weighted average of the slope coefficients from the joinpoint regression model, with the interval. Finally, this weighted average of the slope coefficients is transformed into an annual percent change. If \(\:{b}_{i}\) represents the slope coefficient for the \(\:{i}_{th}\) segment and \(\:{w}_{i}\) denotes the length of each segment within the specified range of years, the following formula is applied:
Decomposition analysis was used to quantify the contributions of three determinants (aging, population growth and epidemiological changes) to epidemiological metrics over specific periods. Epidemiological changes were characterized as modifications in age-adjusted and population-adjusted mortality and prevalence rates. We first used the decomposition methodology of Das Gupta to decompose, prevalence, incidence, and DALYs by population age structure, population growth, and epidemiologic changes. For example, the number of DALYs at each location was obtained from \(\:\:\:DAL{Y_{ay,py,ey}} = \sum\nolimits_{i = 1}^{20} {\left( {{a_{i,y}}*{p_y}*{e_{i,y}}} \right)}\), where \(\:{DALY}_{ay,py,ey}\) represents DALYs based on the factors of age structure, population, and the DALYs rate for a specific year y; \(\:{a}_{i,y}\) represents the proportion of the population for the age category \(\:i\) of the different age categories in a given year \(\:y\); \(\:{p}_{y}\) represents the total population in a given year \(\:y\); and \(\:{e}_{i,y}\:\)represents the DALYs rate given age category \(\:i\) in year \(\:y\). The contribution of each factor to the change in DALYs from 1990 to 2019 was defined by the effect of factor changes while the other factors were held constant.
All the statistical analyses were completed via R version 4.2.1 and the joinpoint regression program (4.9.1.0).
Results
Global prevalence of BPH
In 2019, the global prevalent cases of BPH in patients aged ≥ 60 years was estimated to be 79,309,174 (95% UI: 61,181,380 to 100,520,944), which represented an increase of 119.01% since 1990. The number of prevalent cases across the SDI regions was 13,632,697 (95% UI: 10,998,556 to 16,806,334) in the high SDI region, 21,905,268 (95% UI: 16,972,535 to 27,614,632) in the high-middle SDI region, 25,432,808 (95% UI: 19,361,477 to 32,726,746) in the middle SDI region, 14,598,225 (95% UI: 10,963,470 to 19,018,350) in the low-middle region, and 3,698,996 (95% UI: 2,724,222 to 4876579) in the low region, with the highest increase observed in the low-middle region at 162.37% from 1990. The three GBD regions with the highest numbers of prevalent cases of BPH in patients aged 60 years and older were East Asia, South Asia, and Western Europe; Andean Latin America, South Asia, and Central Latin America presented the greatest increases in new cases since 1990 (Table 1). At the national and territorial levels, the patterns of prevalent cases were diverse among patients aged 60 years and older. The three countries or territories with the highest prevalent numbers were China, India, and United States of American (Fig. 1A and Table S1).
In 2019, the global prevalence rate of BPH in patients aged 60 years and older was 16,781 (95% UI: 12,946 to 21,269) per 100,000 population. The regions with low-middle SDIs had the highest prevalence of BPH (19,094.72 95% UI: 14,340.40 to 24876.32). In addition, the three GBD regions with the highest prevalence rates of BPH in patients aged ≥ 60 years were Andean Latin America, Central Latin America, and Eastern Europe (Table 1). During the period from 1990 to 2019, the AAPCs in people aged 60 years and older were 0.02 (95% CI: 0.00 to 0.72), indicating that the overall change in prevalence showed an increasing trend globally (Table 1; Fig. 2A).
In the decomposition analysis, the increasing prevalent number of BPH was attributed primarily to population growth (94.93%), aging (1.62%), and epidemiological changes (3.45%). Among the SDI regions, the high-middle SDI region reported the highest contribution from population growth (117.88%), whereas the low-middle SDI region had the lowest contribution (79.31%). Aging contributed the most to the middle SDI region (4.45%) and the least to the low SDI region (1.92%). The proportion of prevalent number attributed to epidemiological changes was highest in the low SDI region (18.78%), and the lowest proportion was detected in the high-middle SDI region (-23.85%) (Fig. 3A).
In the sensitivity analysis for prevalence in different aga groups, the 75–79 years age group had the highest prevalent rate, with 24324.8 per 100,000 population (Fig. 4A).
The prevalence, incidence, and DALYs of BPH across different age groups in 2019. The prevalence (A), incidence (B), and DALYs (C) in older adults with 60–64 years, 60–89 years, 65–69 years, 70–74 years, 75–79 years, 80–84 years and 85–89 years in 2019 were described, respectively. BPH: benign prostatic hyperplasia
Global incidence of BPH
At the global level, the number of incident cases of BPH in patients aged 60 years and older was estimated to be 8,357,953 (95% UI: 6,126,619 to 11,303,565), representing an increase of 121.22% from 1990 (Table 2). The highest number of incident cases was 2,862,907 (95% UI: 2,089,644 to 3,866,897) in the region with middle SDI, whereas the lowest number was 1,268,882 (95% UI: 948,649 to 1,685,017) in the region with high SDI. The high-middle region exhibited the most pronounced growth, increasing by 158.37%. The top three GBD regions for incident cases were East Asia (2.5 million cases), South Asia (1.8 million cases) and Southeast Asia (767 thousand cases). A rapid increase of 217.48% was reported in South Asia (Table 2). At the national or territorial scale, China, India, and United States of American ranked as the top three countries for incident cases of BPH in patients aged 60 years and older in 2019 (Fig. 1B and Table S2).
Globally, the incidence rate of BPH was 1768.50 (95% UI: 1296.36 to 2391.78) per 100,000 population, with a large epidemiological change of 121.22% in people aged 60 years and older. An increasing overall trend was observed since AAPCs exceeded 0 (0.02, 95% CI: 0.00 to 0.03) among older people in 2019 globally. The highest incidence of BPH was 1988.75 (95% UI: 1456.56 to 2680.07) in the high-middle region, with a decreasing trend between 1990 and 2019 (AAPCs: -0.37, 95% CI: -0.42 to -0.33) (Table 2; Fig. 2B). The top three GBD regions for the incidence of BPH in 2019 were Eastern Europe, Central Latin America and Oceania for patients aged 60 years and older (Table 2).
From 1990 to 2019, 98.14% of incident cases of BPH globally was attributable to population growth, -1.29% attributable to age, and 3.14% attributable to epidemiological changes. Like the pattern of prevalence, the incidence of BPH attributed to population growth among people aged 60 and over has increased to 113.68% in the high-middle SDI region at most, as opposed to the low-middle SDI region, with the lowest proportion of 83.9%. Aging contributor was linked to decreased BPH incidence during the study period, with the greatest decrease in the high-SDI region (-3.72%). The largest proportion of epidemiological changes increased to 21.61% in the low-SDI region and decreased to -12.33% in the high-middle-SDI region (Fig. 3B).
In the sensitivity analysis for incidence in different age groups, the age group of 65–69 years had the highest prevalent rate, with 2289.45 per 100,000 population (Fig. 4B).
Global DALYs of BPH
Globally, BPH resulted in approximately 1,561,886 DALYs among people aged 60 years and over in 2019, representing an increase of 118.78%. The middle SDI region had the highest numbers of DALYs of BPH at 502,355 (95% UI: 295,820 to 761,702), whereas the low SDI region reported the lowest at 72,338 (95% UI: 41,955 to 111,020). A significant surge of 161.73% was observed in the low-middle SDI region. The middle SDI region accounted for the highest number of DALYs, whereas the low SDI region reported the lowest number of DALYs among individuals aged 60 and above. A similar rapid increase of 161.73% was noted in the proportion within the low-middle SDI region. The regions of East Asia, South Asia, and Western Europe had the greatest number of DALYs in 2019, with a dramatic increase of 221.70% detected in Andean Latin America (Table 3). Across countries and territories, China, India, and United States of American ranked among the top three total number of DALYs of BPH among older people aged 60 year and older in 2019 (Fig. 1C and Table S3).
Globally, the DALYs rate increased by approximately 329.64 to 330.49 per 100,000 population from 1990 to 2019 among patients aged 60 years and older. The overall trend over time increased, with an AAPC value of 0.01 (95% CI: 0.00 to 0.03). In 2019, the low-middle SDI region reported the highest number of DALYs, at approximately 373.05 per 100,000 population, whereas the high SDI region presented the lowest rate of DAYLs, at approximately 247.39 per 100,000 population (Fig. 2C). In 2019, Andean Latin America, Central Latin America, and Eastern Europe were the regions with the highest DALYs rate of BPH among individuals aged 60 years and over (Table 2).
During 1990 and 2019, the number of DALYs of BPH globally included epidemiological changes of -3.35%, an age of 3.76%, and population growth of 99.59%. Among the five SDI regions, the largest proportion of aging, population, and epidemiology contributors was 5.59% in the high-middle SDI region, 103.21% in the high SDI region, and 18.91% in the low SDI region, respectively (Fig. 3C).
In the sensitivity analysis for DALYs rate in different age groups, the 75–79 years age group had the highest prevalent rate, with 471.04 per 100,000 population (Fig. 4C).
Discussion
In the spatial and temporal GBD analysis among people aged 60 years and over, we found significant increasing trends in the number of incident and prevalent cases, as well as DALYs of BPH between 1990 and 2019, which is consistent with studies showing that the histological situation of BPH continues to rise with age [6, 28, 29]. Overall, the number of prevalent cases increased by 119.01% from 1990 to 2019. We also observed increasing prevalence rates in high-middle, middle, and low-middle regions among older people aged 60 years and over. Specifically, the highest metrics, including prevalence, incidence, and DALYs, were found in China, India, and United States of America, in that order. The two largest regions contributing to the rates of prevalence, incidence, and DALYs were East Asia and South Asia. These findings inform the ongoing debate on health decisions regarding BPH among older people.
Our findings suggested that the burden of BPH was highest in older people, especially those aged 60 and over, which was consistent with the findings of previous surveys. A meta-analysis including 25 countries reported that the lifetime prevalence of BPH was 26.2%, and the age-specific prevalence increased with age [10]. Global epidemiological estimates further substantiated this evidence, indicating that adult males aged 65–74 years bore the maximum absolute burden of BPH. Additionally, the highest age-specific prevalence was observed among individuals aged between 75 and 79 years [5]. In addition, these global estimates were supported by community studies from different countries, such as Britain and the U.S. [30, 31], indicating that older male people were associated with a high risk of BPH and that this condition can even be aggravated as LUTS. Our analysis revealed that incident rates, prevalence rates and DALYs rates were highest in China. Several epidemiological studies based on the Chinese population have addressed this issue. Xiong et al. reported that 12.01% of middle-aged and older Chinese people were considered to have BPH according to national longitudinal data from 2015 [32]. Furthermore, using a complex sampling design, Wang et al. reported that the weighted total prevalence of BPH in males aged 45 years and older was 13.1% [33]. However, the aforementioned studies also pinpointed that older people with comorbidities were inclined to have a higher prevalence [32, 33]. In summary, because older people are linked to multiple chronic diseases, the number of BPH patients is increasing, especially in emerging aging countries, such as China.
The prevalence of BPH has been altered due to lifestyle changes, population growth, aging, and medical activities [34,35,36,37]. In our analysis, we observed that population growth contributed to the largest share of the prevalence of BPH, followed by population aging. Therefore, we should maintain our concerns about populous countries and regions. For example, we observed that China, India, and United States of America ranked in the top three countries in prevalent cases. Moreover, East Asia, South Asia, and Western Europe contributed to the greatest number of prevalent cases. These results may be related to the allocation of healthcare resources, exposure to risk factors, and public health awareness. Over the past few decades, most Asian countries have focused their disease prevention and control efforts on fatal diseases, resulting in insufficient healthcare resources allocated to nonfatal diseases such as BPH [38]. Consequently, the burden of BPH has continued to increase. Furthermore, existing studies have shown that obesity, hypertension, metabolic syndrome, dietary habits, smoking and alcohol consumption, and lack of physical activity are associated with the progression of BPH [39,40,41]. These risk factors remain inadequately controlled in countries such as China and India [42,43,44]. Additionally, with economic development and improved education levels, public health awareness has increased [45], leading to more patients being diagnosed and treated at early stages of the disease. This has indirectly contributed to the increase in prevalence, incidence, and DALYs. Moreover, treatment modalities also influence the trends in the BPH burden. Currently, there is no standardized treatment method for BPH patients [46]. Common treatments include medication and surgery, with medication being the preferred choice for most patients in countries like China and India [47, 48]. However, contrary to our study, other studies have shown that the prostate volumes of men in Japan, China, and India are significantly smaller than those of men in Australia or the United States [49] and that the incidence of BPH in Asian men is lower than that in Caucasian men [50]. This discrepancy may be due to variations in the methodologies and populations studied in different studies, leading to different outcomes.
Notably, rapidly increasing cases have been reported in Andean Latin America, South Asia, and Central Latin America. A previous study revealed that the disease burden of LUTS will be greatest in Asia, South America and Africa in the coming decades [31]. Nevertheless, our findings provide a warning against the increasing prevalence of BPH in burgeoning countries. The economic burden attributed to BPH has been highlighted in the 21st century. In 2000, the U.S. recorded approximately 8 million clinic visits for benign prostatic hyperplasia, incurring a direct treatment expenditure of US$1.1 billion, excluding outpatient medication costs [31, 51]. In the global male population aged > 65 years, the estimated economic burden of BPH is $73.8 billion annually [52, 53]. According to our analysis, the prevalence in Western European peaked in 2019, with 42171.49 per 100,000, along with increased medical expenditures. Hence, our findings are highly relevant for the enhancement of health service infrastructure, capacity development of human resources, and prediction of economic burdens. Furthermore, our study results indicate that the burden of BPH has increased most significantly in high-middle SDI regions, which is consistent with previous findings [54, 55]. This is primarily due to changes in dietary patterns and lifestyles as SDI levels rise, increasing men’s exposure to BPH risk factors, along with the extended life expectancy of men.
Some limitations of this work should be acknowledged. First, the estimation and description of the GBD database should be meticulous because the results depend on the quality of the data source and the robustness of the methodology. Second, the temporal analysis of BPH in the GBD was divided into distinct age, sex, year, and geographic location groups; however, the differences in race and ethnicity merit further study. For example, we found heterogeneous rates across Eastern countries and Western countries that represented diverse populations. Third, this study relies on the GBD 2019 database; however, the estimates for different countries and regions worldwide may lack accuracy due to variations in healthcare infrastructure, data collection methods, and reporting practices. The quality of GBD data can differ significantly across countries, with lower-income countries often having less comprehensive health data systems. This can lead to underreporting or misclassification of BPH cases, particularly in countries such as China, India, and the Russian Federation, where large-scale epidemiological surveys are lacking. These factors can affect the reliability of our estimates. Fourth, according to the designed GBD framework, each death was assigned to a unique underlying cause of death. The mortality associated with BPH was attributed to diverse complications and was excluded from the BPH estimates. Finally, owing to data limitations, this study did not explore the impact of socioeconomic factors and healthcare accessibility on the economic burden of BPH across different countries and regions. Variations in socioeconomic status and access to healthcare can significantly influence the diagnosis, treatment, and management of BPH, affecting reported prevalence and incidence rates. Future research should examine how these factors contribute to differences in the burden of BPH across various settings to provide a more comprehensive understanding of its impact on healthcare resources.
Conclusions
Preventing BPH threatens global male health, especially in people aged 60 years and older, leading to significant disease burdens and economic expenditures. Our findings show that the increasing prevalent cases of BPH impacts individuals aged 60 years and over and that population growth is an underlying determinant. In the future, several populous countries, such as China, India, and United States of America, will experience a greater disease burden of BPH among older people aged 60 years and over. Effective health decisions are imperative for the prevention and treatment of BPH. For example, enhancing the allocation of relevant healthcare resources, strengthening health education campaigns, promoting knowledge about the prevention of urinary system diseases, and advocating for healthy diets and lifestyles can help rapidly reduce the global burden of BPH.
Data availability
To download the source data and analytic code used in these analyses, please visit the Global Health Data Exchange GBD 2019 website.
Abbreviations
- AAPCs:
-
Average annual percentage changes
- BPH:
-
Benign prostatic hyperplasia
- DALYs:
-
Disability-adjusted life-years
- GBD:
-
Global Burden of Diseases
- GHDx:
-
Global Health Data Exchange
- ICD:
-
International Classification of Diseases
- IPSS:
-
International Prostatism Symptom Score
- LUTS:
-
Lower urinary tract symptoms
- MR-BRT:
-
Meta-regression-Bayesian, regularized, trimmed
- N-QoL:
-
Nocturia-specific Quality of Life
- SDI:
-
Sociodemographic index
- UI:
-
Uncertainty interval
References
Cornu JN, Oelke M, Parsons KF. Benign prostatic hyperplasia and lower urinary tract symptoms. N Engl J Med. 2012;367(17):1668. author reply 1668-9.
Bushman W. Etiology, epidemiology, and natural history of benign prostatic hyperplasia. Urol Clin North Am. 2009;36(4):403–15.
Fusco F, Creta M, De Nunzio C, et al. Progressive bladder remodeling due to bladder outlet obstruction: a systematic review of morphological and molecular evidences in humans. BMC Urol. 2018;18(1):15.
McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185(5):1793–803.
Collaborators GBDBPH. The global, regional, and national burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Healthy Longev. 2022;3(11):e754–76.
Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173(4):1256–61.
Lim KB. Epidemiology of clinical benign prostatic hyperplasia. Asian J Urol. 2017;4(3):148–51.
Lin YH, Wu CT, Juang HH. Exploring the complex interplay: BPH, nocturia, and aging male health. World J Urol. 2024;42(1):105.
Khan S, Wolin KY, Pakpahan R, et al. Body size throughout the life-course and incident benign prostatic hyperplasia-related outcomes and nocturia. BMC Urol. 2021;21(1):47.
Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep. 2017;7(1):7984.
Wang W, Guo Y, Zhang D, et al. The prevalence of benign prostatic hyperplasia in mainland China: evidence from epidemiological surveys. Sci Rep. 2015;5:13546.
Fourcade RO, Theret N, Taieb C, et al. Profile and management of patients treated for the first time for lower urinary tract symptoms/benign prostatic hyperplasia in four European countries. BJU Int. 2008;101(9):1111–8.
Welch G, Weinger K, Barry MJ. Quality-of-life impact of lower urinary tract symptom severity: results from the Health professionals follow-up study. Urology. 2002;59(2):245–50.
Abraham L, Hareendran A, Mills IW, et al. Development and validation of a quality-of-life measure for men with nocturia. Urology. 2004;63(3):481–6.
Johnson TV, Abbasi A, Ehrlich SS, et al. Major depression drives severity of American Urological Association Symptom Index. Urology. 2010;76(6):1317–20.
Collaborators GBDCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88.
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858.
Collaborators GBDCoD. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210.
Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Wafa HA, Marshall I, Wolfe CDA, et al. Burden of intracerebral haemorrhage in Europe: forecasting incidence and mortality between 2019 and 2050. Lancet Reg Health Eur. 2024;38:100842.
Collaborators GBDNP. Global, regional, and national burden of neck pain, 1990–2020, and projections to 2050: a systematic analysis of the global burden of Disease Study 2021. Lancet Rheumatol. 2024;6(3):e142–55.
Collaborators GUHD. Burden of liver cancer mortality by county, race, and ethnicity in the USA, 2000-19: a systematic analysis of health disparities. Lancet Public Health. 2024;9(3):e186–98.
WHO. International Statistical Classification of Diseases and Related Health Problems (ICD). 2022. https://www.who.int/classifications/classification-of-diseases, accessed on February 15, 2024.
WHO. Ageing and health 2022. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health, accessed on February 15, 2024.
Collaborators GBDA. Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the global burden of Disease 2019 study. BMJ. 2022;376:e068208.
Cao F, Liu YC, Ni QY, et al. Temporal trends in the prevalence of autoimmune diseases from 1990 to 2019. Autoimmun Rev. 2023;22(8):103359.
Clegg LX, Hankey BF, Tiwari R, et al. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–82.
Sarma AV, Parsons JK, McVary K, et al. Diabetes and benign prostatic hyperplasia/lower urinary tract symptoms–what do we know? J Urol. 2009;182(6 Suppl):S32–7.
Rhodes T, Girman CJ, Jacobsen SJ, et al. Longitudinal prostate growth rates during 5 years in randomly selected community men 40 to 79 years old. J Urol. 1999;161(4):1174–9.
Bauer SR, Le T, Ensrud KE, et al. Lower urinary tract symptom severity, urinary bother, and incident life-space mobility restriction among older men. J Am Geriatr Soc. 2023;71(4):1093–104.
Griebling TL. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence, and bladder outlet obstruction. BJU Int. 2011;108(7):1138–9.
Xiong Y, Zhang Y, Zhang F, et al. Reduced sleep duration increases the risk of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in middle-aged and elderly males: a national cross-sectional study. Aging Male. 2022;25(1):159–66.
Zhang W, Cao G, Sun Y, et al. Depressive symptoms in individuals diagnosed with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH) in middle-aged and older Chinese individuals: results from the China Health and Retirement Longitudinal Study. J Affect Disord. 2022;296:660–6.
Zhang S, Wang Q, Zhao D, et al. Association of Sensory Impairment with Institutional Care willingness among older adults in Urban and Rural China: an observational study. Innov Aging. 2023;7(3):igad013.
Nakagawa T, Cho J, Yeung DY. Successful aging in East Asia: comparison among China, Korea, and Japan. J Gerontol B Psychol Sci Soc Sci. 2021;76(Suppl 1):S17–26.
Lee HW, Kim SA, Nam JW, et al. The study about physical activity for subjects with prevention of benign prostate hyperplasia. Int Neurourol J. 2014;18(3):155–62.
Sun J, Li Y, Xiao LF et al. Flattening the curve after the initial outbreak of Coronavirus Disease 2019: A Data-Driven modeling analysis for the Omicron pandemic in China. Vaccines (Basel). 2023;11(5).
World Health O. Men, ageing and health: achieving health across the life span. World Health Organization; 2001.
Corona G, Vignozzi L, Rastrelli G, et al. Benign prostatic hyperplasia: a new metabolic disease of the aging male and its correlation with sexual dysfunctions. Int J Endocrinol. 2014;2014:329456.
Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016;13(2):108–19.
De Nunzio C, Aronson W, Freedland SJ, et al. The correlation between metabolic syndrome and prostatic diseases. Eur Urol. 2012;61(3):560–70.
Shrivastava U, Misra A, Mohan V, et al. Obesity, Diabetes and Cardiovascular diseases in India: Public Health challenges. Curr Diabetes Rev. 2017;13(1):65–80.
Teo KK, Rafiq T. Cardiovascular Risk factors and Prevention: a perspective from developing countries. Can J Cardiol. 2021;37(5):733–43.
Low WY, Lee YK, Samy AL. Non-communicable diseases in the Asia-Pacific region: prevalence, risk factors and community-based prevention. Int J Occup Med Environ Health. 2015;28(1):20–6.
Hahn RA, Truman BI. Education Improves Public Health and Promotes Health Equity. Int J Health Serv. 2015;45(4):657–78.
Shrivastava A, Gupta VB. Various treatment options for benign prostatic hyperplasia: a current update. J Midlife Health. 2012;3(1):10–9.
Xia SJ, Cui D, Jiang Q. An overview of prostate diseases and their characteristics specific to Asian men. Asian J Androl. 2012;14(3):458–64.
Sabnis RB, Mulawkar P, Joshi R. Urological Society of India: Indian Guidelines on Management of BPH/BPO.
Liang GQ, Zhang SJ, Wang B, et al. [Lower urinary tract symptoms and prostatic growth pattern among old and middle-aged males in Shanghai community]. Zhonghua Nan Ke Xue. 2012;18(10):886–90.
Masumori N, Tsukamoto T, Kumamoto Y, et al. Japanese men have smaller prostate volumes but comparable urinary flow rates relative to American men: results of community based studies in 2 countries. J Urol. 1996;155(4):1324–7.
Zheng P, Barber R, Sorensen RJ, et al. Trimmed constrained mixed effects models: formulations and algorithms. J Comput Graphical Stat. 2021;30(3):544–56.
Vuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol. 2015;22(Suppl 1):1–6.
US National Institute of Diabetes and Digestive Kidney Diseases: Urologic disease in America. 2022. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/urologic-diseases-in-america, accessed on August 03, 2024.
Zhu C, Wang DQ, Zi H, et al. Epidemiological trends of urinary tract infections, urolithiasis and benign prostatic hyperplasia in 203 countries and territories from 1990 to 2019. Mil Med Res. 2021;8(1):64.
Launer BM, McVary KT, Ricke WA, et al. The rising worldwide impact of benign prostatic hyperplasia. BJU Int. 2021;127(6):722–8.
Acknowledgements
We are grateful to all participants who contributed to this research and all members who participated in the 2019 GBD study.
Funding
This study was not funded by any funding.
Author information
Authors and Affiliations
Contributions
ZY. Y and ZZ. C designed the study. ZY. Y and ZZ. C organized the data, JH. W, YF. X, JY. L and LJ. X finished the statistical analyses. ZY. Y and ZZ. C drafted the initial manuscript. All authors have read and approved the final version of the manuscript, and agreed with the order of presentation of the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ye, Z., Wang, J., Xiao, Y. et al. Global burden of benign prostatic hyperplasia in males aged 60–90 years from 1990 to 2019: results from the global burden of disease study 2019. BMC Urol 24, 193 (2024). https://doi.org/10.1186/s12894-024-01582-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-024-01582-w