Abstract
Background
Most people diagnosed with dementia live and die in community settings. This study aimed to: (i) describe the palliative care needs of patients with dementia at commencement of community palliative care; (ii) compare palliative care needs between patients with dementia and those with lung cancer and cardiovascular disease (CVD).
Methods
This is a population-based descriptive study that involved 8,727, 7,539 and 25,279 patients who accessed community palliative care across Australia principally because of dementia, CVD and lung cancer. Patients’ functional abilities, symptom burden and clinical condition were assessed at commencement of community alliative care using five validated instruments: Resource Utilisation Groups—Activities of Daily Living, Australia-modified Karnofsky Performance Status, Symptoms Assessment Scale, Palliative Care Problem Severity Score and Palliative Care Phase. We fitted ordinal logistic regression models to examine the differences in these assessments for dementia versus CVD and lung cancer, respectively.
Results
Overall, patients with dementia generally had low levels of distress from symptoms but poor functional problems. Compared to the other two diagnostic groups, palliative care for dementia was often initiated later and with shorter contacts. Also, patients with dementia presented with poorer functional performance (adjusted OR (aOR) = 4.02, Confidence Interval (CI): 3.68 – 4.38 for dementia vs CVD; aOR = 17.59, CI: 15.92 – 19.44 for dementia vs lung cancer) and dependency (aOR = 5.68, CI: 5.28 – 6.12 for dementia vs CVD; aOR = 24.97, CI: 22.77 – 27.39 for dementia vs lung cancer), but experienced lower levels of distress and problem severity for the majority of symptoms.
Conclusion
Community palliative care is often an ideal care option for many patients, particularly for those with dementia. We call for expansion of the palliative care workforce and options for home care support to optimize accessibility of community palliative care for dementia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Dementia is a progressive, irreversible and life-limiting neurodegenerative disorder [1]. Dementia is the second leading cause of death in Australia with 472,000 people living with the condition in 2021, and an expected increase to 1,076,000 by 2058 [2]. Late-stage dementia is usually associated with multiple physical and psychosocial complications, as well as being a substantial burden for caregivers and society [3, 4]. However, ensuring access to palliative care services for advanced dementia is a significant challenge because recognition of dementia as having “end-stage” or “terminal” stages is still uncommon amongst the public and healthcare professionals [4, 5]. Recently, there has been a greater focus on palliative care for people with dementia because of the escalating disease burden and unmet need in this population [5, 6].
In Australia, palliative care is defined as person and family-centred care that aims to optimize the quality of life for a person with an active, progressive, advanced disorder through management of physical symptoms and psychological, social and spiritual wellbeing. Palliative care is provided in both community and inpatient settings, with patients often starting with community care. Community-based palliative care is provided by a multidisciplinary team of healthcare professionals, each addressing physical, psychological, social, spiritual, and cultural needs, while also supporting family and carers [7,8,9,10]. Palliative care consultants, who are specialized medical doctors, manage complex cases in hospitals or residential aged care homes with dedicated palliative care units. Nurses handle ongoing care and treatment by assessing, planning, administering treatment, and managing symptoms. Allied health professionals, such as social workers, physiotherapists, and pastoral care workers, contribute by treating symptoms, managing daily tasks, offering emotional support, and providing rehabilitation services. Palliative care volunteers, recruited, trained, and managed by local services, offer free support to individuals with life-limiting illnesses and their families, providing practical help around the home, emotional support, and assistance with errands.
The majority of people with dementia live and die in community settings (home or a residential care home) [11,12,13]. However, it is not known whether palliative care provided in the community settings (i.e., private residence and residential aged care facility) sufficiently meets the needs of people with dementia. Many of these patients experience an illness trajectory that is distinct from other common diseases for which palliative care is often implemented, such as cancer and cardiovascular disease (CVD) [14,15,16]. A comprehensive comparison of the clinical characteristics and palliative care needs of individuals diagnosed with dementia versus those with other chronic conditions can help identify the unique palliative care requirements for patients with dementia. This, in turn, has the potential to inform the development of dementia-specific palliative care strategies, as well as guide policy development, resource allocation, and personnel training for dementia palliative care in community settings.
Our previous population-based study indicated that, at the time of first entry to inpatient palliative care, patients with dementia experienced lower levels of symptom distress but higher levels of dependency compared to those with lung cancer and CVD [17]. However, it has been reported that variations in clinical characteristics, symptom burden, as well as end-of-life experiences can arise amongst people with dementia receiving care in different settings [18, 19]. The current analysis therefore shifts the focus to clinical characteristics and palliative care needs of patients with dementia at commencement of community-based palliative care, which are likely to differ from the inpatient context we previously evaluated.
This study has two principal aims. The first aim was to describe the characteristics, functional status and symptom distress of patients with dementia on their first entry into community palliative care services. The second aim was to conduct comparisons on function and symptom burden for patients with dementia relative to those with lung cancer and CVD, both of which are frequently managed conditions within traditional palliative care frameworks.
Material and methods
Study design and data sources
This is an observational study using data derived from the Australian Palliative Care Outcomes Collaboration (PCOC). PCOC is an Australian government-funded national program that aims to systematically improve palliative care outcomes through routinely collecting point-of-care clinical assessments and providing feedback against established benchmarks for participating services (including community and inpatient settings) [20]. The participating services assess clinical outcomes of their patients using validated and standardized tools (described below). Community services perform assessments on admission, during each subsequent patient contact and at discharge. The point-of-care outcomes upon admission, at phase changes (defined below) and at discharge are submitted to PCOC bi-annually. Data quality assurances procedures are completed by PCOC staff before being analyzed. Six-monthly reports at national, state and service level allow comparisons on performance and outcomes against industry agreed benchmarks and against similar services.
Study setting and cohort selection
This study included patients who received community episode of palliative care which refer to the care provided in a community setting (i.e., either in a private residence or residential aged care facility). The episode of community palliative care start from the date when the first in-person comprehensive palliative care assessment is undertaken and documented using the five PCOC clinical assessment tools. The episode end on the date when: i) patient is separated from the current setting of care (e.g. from community to inpatient), or ii) patient dies, or iii) principal clinical intent of the care changes and the patient is no longer receiving palliative care.
Patients enrolled in this study were those who: (i) accessed palliative care from a service registered in PCOC between January 1st 2013 and June 29th 2022; (ii) accessed palliative care principally because of a formal diagnosis of dementia (including Alzheimer’s disease and other dementias), CVD, or lung cancer.
Variables and tools
The PCOC program uses five standardized and validated tools to collect data on patients’ clinical outcomes. The use of research instruments was obtained permission from authors. Patients (preferably) or proxies report levels of distress associated with seven common physical symptoms (insomnia, appetite, nausea, bowel symptoms, breathing problems, fatigue and pain) using the 11-point (0 – absent; 10 – worst possible distress) PCOC Symptoms Assessment Scale (SAS) [21]. Clinicians globally rate the severity of palliative care problems relating to pain, other symptoms, psychological/spiritual and family concerns based on the four-point (0—absent; 3—severe) Palliative Care Problem Severity Score (PCPSS) [22].
Resource Utilisation Groups—Activities of Daily Living (RUG-ADL) is used to evaluate patients’ dependency regarding basic living tasks of bed mobility, toileting, transfer and eating [23]. The activity of eating is assessed based on a three-point item (1—independent/supervision; 2—limited assistance; 3—total dependence/tube fed), but four-point items (1—independent/supervision; 3—limited assistance; 4—one person plus functional aid; 5—two or more persons assist) are used for other activities. (1) The total RUG-ADL scores range from 4 to 18. The Australia-modified Karnofsky Performance Status (AKPS) Scale evaluates a patient's performance in terms of activity, work, and self-care. Clinicians assign a single score ranging from 10 to 100, based on their observations of the patient's ability to perform typical tasks related to these dimensions. A score of 100 represents normal physical abilities with no signs of disease, while lower scores indicate diminished performance. A score of 0 signifies that the patient has died; however, this score is not used in the PCOC because no further assessments are conducted after a patient's death [24].
The non-sequential PCOC palliative care phases which describe four distinct, clinically meaningful phases of palliative care (i.e., stable, unstable, deteriorating and terminal) were determined by clinicians based on comprehensive clinical assessments of the patient and their family [25]. The palliative care phase identifies a clinically meaningful period in a patient’s condition and served as the foundation for developing palliative care casemix classification. Detailed definitions of each phase can be found in the study by M. Masso et al. [25] All the clinical outcomes reported in this study related to the assessments of the patient’s first episode of community palliative care.
Other characteristics of patients involved in the study included sex, age, indigenous status, country of birth, preferred language, year of admission, Socio-Economic Indexes for Areas (SEIFA, a standardized summary measure of social and economic conditions for an area developed by the Australian Bureau of Statistics) [26], accommodation type at episode start, referral agencies for the specific episode of care, length of the care episode and reason for ending of the episode of care (i.e., death, other).
Statistical methods
Descriptive statistics were used to assess categorical and numerical variables in relation to sociodemographic characteristics and other clinical characteristics. We tested for differences in characteristics of patients and episodes of care between dementia versus CVD and lung cancer using Pearson's chi-squared tests and Mann Whitney U Test (for length of stay only). We reported means (± standard deviation (SD) and medians (with interquartile range, IQR) for standard clinical measures (AKPS, RUG-ADL, PCPSS and PCOC SAS) based on their original scores.
For the analyses we assigned clinical assessments as ordinal variables to reflect the distributional patterns of the scores (refer to Supplementary Figs. 1–4). For PCOC SAS and PCPSS: 0 = absent (corresponding to PCOC SAS = 0, PCPSS = 0), 1 = mild (PCOC SAS = 1—3, PCPSS = 1), and 2 = moderate to severe (PCOC SAS = 4—10, PCPSS = 2—3); for RUG-ADL: 0 = independence or supervision only (corresponding to total RUG-ADL = 4—5), 1 = limited physical assistance (RUG-ADL = 6—13), 2 = one assistant plus equipment (RUG-ADL = 14—17), 3 = two assistants for full care (RUG-ADL = 18); for AKPS, 0 = from normal activity to in bed less than 50% of the time (corresponding to AKPS = 50—100), 1 = in bed more than 50% of the time (AKPS = 20—40), 2 = completely bedfast or comatose (AKPS = 10—20). For the purposes of analyses, AKPS scores were reversed through statistical transformation.
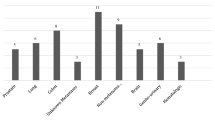
Ordinal logistic regression models were used to estimate unadjusted and adjusted odds ratios (ORs) with CVD and lung cancer as the reference conditions for comparison with dementia. The adjusted ORs were shown in Figs. 1 and 2. The covariates we adjusted for included sex, age, Socio-Economic Indexes for Areas (SEIFA, a standardized summary measure of social and economic conditions for an area developed by the Australian Bureau of Statistics) [2], country of birth, preferred language, year of admission, palliative care phase and referral sources. We used Stata 15.1 (StataCorp, College Station, TX) to perform all analyses. The level of significance was defined as α = 0.05.
Adjusted odds ratios of scores on Resource Utilization Groups-Activities of Daily Living (RUG-ADL) and Australia modified Karnofsky Performance Score (AKPS) by pairwise comparison. CVD, cardiovascular disease. Note: Covariates such as sex, age, SEIFA, country of birth, preferred language, year of admission, palliative care phase, and referral sources were adjusted for in this figure
Adjusted odds ratios of Scores on Palliative Care Problem Severity Score (PCPSS) and Symptoms Assessment Scale (PCOC SAS) by pairwise comparison. CVD, cardiovascular disease. Note: Covariates such as sex, age, SEIFA, country of birth, preferred language, year of admission, palliative care phase, and referral sources were adjusted for in this figure
Results
Table 1 summarizes the characteristics of patients and care episodes. The study population consisted of 8 727, 7 539 and 25 279 people who received palliative care primarily because of dementia, CVD and lung cancer, respectively. Compared to patients with CVD and lung cancer, those with dementia were more likely to be female (P < 0.001 for both comparisons), to exceed 85 years of age (P < 0.001 for both comparisons), and to reside in areas with higher Socio-Economic Indexes (P < 0.001 for both comparisons). Patients with dementia were less likely than those with CVD and lung cancer to be born in Australia (P = 0.003 for CVD versus dementia, P < 0.001 for lung cancer versus dementia) and report that English was their preferred language (P = 0.033 for CVD versus dementia, P < 0.001 for lung cancer versus dementia).
Patients with dementia usually had shorter lengths of care episode, with a median of 11 days as compared to 18 days for those with CVD (P < 0.001) and 30 days for lung cancer patients (P < 0.001). The percentage of admissions for dementia increased faster than those for CVD and lung cancer (P < 0.001 for both comparisons). Relative to those with CVD and lung cancer, patients diagnosed with dementia more frequently lived in a residential aged care facility at the episode start (P < 0.001 for both comparisons), and were also more likely to be referred from this care setting (P < 0.001 for both comparisons). Episodes for patients with dementia more frequently started with “deteriorating” and “terminal” palliative care phases (P < 0.001 for both comparisons), and ended with death (P < 0.001 for both comparisons).
Performance status and dependency
Table 2 shows the outcomes of standard clinical measures for different groups of patients and unadjusted ORs for group comparisons. Large differences in AKPS and RUG-ADL scores were observed between dementia and the other two conditions. The mean AKPS score for patients with dementia was 29.09 versus 41.05 for CVD and 55.49 for lung cancer. Patients with dementia had higher mean total RUG-ADL (16.03) than patients with CVD (11.15) and lung cancer (6.38).
Adjusted ORs (aOR) are presented in Fig. 1. People diagnosed with dementia had higher odds of poor performance (AKPS assessments) when compared to those with CVD (aOR 4.02, 95%CI: 3.68 – 4.38) and lung cancer (aOR 17.59, 95%CI: 15.92 – 19.44). For RUG-ADL scores, the value of aORs (all statistically significant with p < 0.001) were between 4.60 and 6.82 for dementia versus CVD, and between 19.28 and 24.97 for lung cancer versus dementia, respectively. Compared to lung cancer patients, Fig. 1 clearly shows that the performance status of CVD patients more closely resembles that of dementia patients.
Symptom burden
Table 2 indicated that the majority of patients in all three groups experienced absent or relatively mild symptom burdens. Compared to CVD group, patients with dementia had significantly lower aORs (ranged from 0.49 to 0.89, P ≤ 0.02 for all) in all the four PCPSS domains. (Fig. 1) In comparisons to lung cancer, aORs (ranged from 0.36 to 0.61, P < 0.001 for all) were significantly lower for dementia in three of the four PCPSS domains, with the domain of “family concerns” as an exception. (Fig. 2).
For PCOC SAS assessments, mean levels of distress for each symptom are all less than four out of a possible maximum score of ten. Pain, fatigue and appetite, however, were associated with comparatively high levels of distress for all patients. Breathing problems also caused relatively high levels of distress for patients with lung cancer and CVD (Table 2). Compared with other two groups, people with dementia had significantly lower aORs (ranged from 0.13 to 0.86, p < 0.001 for all) for all symptoms (as shown in Fig. 2).
Discussion
The study described the clinical characteristics, functional status and symptom distress of dementia patients in community palliative care and conducted comparisons with those of patients with lung cancer and cardiovascular disease. At commencement of community palliative care, patients with dementia reported substantially lower functional performance and higher levels of dependence compared to CVD and lung cancer. Slightly lower levels of symptoms distress were reported by people with dementia, although overall high levels of symptom severity and distress were not common amongst patients in any of the three groups.
The patterns of differences in palliative care needs between dementia and other diagnostic groups are consistent with our previous studies focusing on palliative care inpatients with dementia, lung cancer and CVD [9]. These differences should be considered when developing tailored palliative care models. For lung cancer and cardiovascular disease, more expertise from palliative care physicians is needed for symptom management, particularly in addressing fatigue and breathing problems, which are more prevalent in these groups. In contrast, the palliative care model for dementia should focus more on family support from nurses and social workers, as these patients typically experience poorer functional status and performance impairment.
There is also increasing evidence to suggest that community-based palliative care for patients with advanced dementia would significantly reduce the rates of emergency department visits, hospital-acquired infections, and inappropriate active treatment [27, 28]. Community-based palliative care services are usually more cost-effective, and maintain links to patients’ regular care providers, particularly general practitioners [29,30,31]. The close collaboration between community palliative care team, general practitioners, specialists, and families have the potential to reduce the often-recurring cycle of transfers between home and hospital during end-of-life care for patients with dementia. Provision of palliative care in community settings has the potential to reduce the often recurring cycle of transfers to and from home to hospital during end-of-life care for patients with dementia [28], which is accompanied by the risk of distress, confusion, and injury from transport between settings. However, it must be emphasized that other types of palliative care, including inpatient options, should be available whenever patients require such management.
However, when considering home care options, the relatively low levels of physical symptom distress for patients with dementia need to be weighed up against their poor functional performance and self-care capacity as well as the increased need for support for the family. Palliative care is designed to be patient-centered care and, where relevant, considers the family as part of the unit of care [32]. Families of patients with dementia face multiple challenges in coping with home care, including the requirement for long-term high-demand management, insufficient support, and difficulties in communication because of the patient’s cognitive impairment.
Adequate home care (e.g., personal, nursing and social care) that ensures safety, independence of basic living activities and social connection are required to support people to live in their own homes if that is their preference. In the Australian context, the government is increasing its investment in home care support to allow more older Australians to live longer at home. This policy is partly in response to a recent report by the Australian Royal Commission into Aged Care Quality and Safety, which indicated that more than 10,000 older Australians were waiting for a home care package at their approved level and often received less care than they need after prolonged waiting periods [33].
Our study revealed marked disparities in patterns of access to palliative care. In comparison to patients with lung cancer and CVD groups, those with a diagnosis of dementia more frequently entered palliative care services at the terminal phase, and these contacts were usually shorter in duration and more often ended with death. Similar findings were reported in our previous study focusing on palliative care inpatients [17]. These findings suggest that access to palliative care occurred later and with shorter contact with palliative care for people with dementia compared to CVD and lung cancer. Disparities in access for people with dementia relative to other conditions have also been reported in previous studies [34]. A 2015 study in Western Australia reported that only 6% of people dying with or of dementia in the state received community-based palliative care at their end of life, compared to 26% for the other disease groups [28].
One of the major reasons for late and inadequate access to palliative care could be the shortages in the palliative care workforce, which is a major issue both globally and in Australia [35]. In 2021, there were only 289 employed medical specialists and 3,080 FTE (full-time equivalent) employed nurses working as specialist palliative care professionals in Australia [7]. This is equivalent to every 100,000 Australians having 1.1 FTE palliative medicine physician and 12.0 FTE nurses [7]. This workforce of palliative medicine physicians is only half of the benchmark of 2.0 full-FTE specialist palliative care physicians per 100,000 population recommended by Palliative Care Australia in 2018 [10]. Moreover, there is relatively greater shortage of palliative care services in community settings. In 2021, 73% of all employed palliative medicine physicians and half (52%) of all employed palliative care nurses worked in a hospital setting in Australia [7]. Another major reason for the observed service gaps is that many people with dementia at end of life are in residential care facilities, where comprehensive palliative care is only now starting to become routinely established.
To our knowledge, this is the first large-scale study to compare the characteristics, symptoms and care needs among people with dementia, CVD and lung cancer at the commencement of community palliative care. However, some limitations of the study should be noted. First, there may be potential biases in the estimates of symptom distress used in our study. These biases might arise from two factors: challenges in symptom assessment amongst patients with dementia, and variations in data-reporting between patients with dementia and other two conditions. Assessing subjective symptoms for patients with dementia is always challenging in practice [36, 37]. Inconsistencies in comparisons of symptom burden between patients with and without dementia have been noted in previous studies [38, 39]. Compared to the CVD and cancer groups, proxy rating of symptom distress likely occurred more frequently amongst for people with dementia, who more commonly have diminished communication capacity and impaired cognitive function. Another potential bias in this study may have arisen from coding of diagnostic groups, which were assigned according to their primary reason for accessing palliative care but did not account for comorbidities. For example, patients in the dementia group may also suffered from other chronic diseases such as CVD. It should be noted that the three diagnostic groups included in the study were likely to represent patients at different stages of life given the large variations in AKPS assessments between them. Future studies can conduct more reasonable comparisons between them with consideration of their clinical trajectories and survival patterns.
Conclusion
On admission to community palliative care, patients with dementia exhibited significantly lower functional performance and higher dependence than those with cardiovascular disease (CVD) or lung cancer, reported slightly lower symptom distress. The unique pattern of palliative care needs for people diagnosed with dementia suggest that community palliative care is often an optimal care option for the majority. However, sufficient support for families to manage the increasing functional and cognitive impairment in the home-care setting is a prerequisite for such care options. Expansion of the palliative care workforce and greater options for home care support are required to optimize timely access to community-based palliative care for dementia.
Availability of data and materials
The data that were used for this study are available upon reasonable request from the Palliative Care Outcomes Collaboration. Requests can be made through the application form which can be found at: https://www.uow.edu.au/ahsri/pcoc/.
References
Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and management of dementia. JAMA. 2019;322(16):1589–99.
Dementia Australia. Dementia Prevalence Data Estimates and Projections. Available at: https://www.dementia.org.au/information/statistics/prevalence-data. Accessed July 2, 2023.
Abreu W, Tolson D, Jackson GA, Costa N. A cross-sectional study of family caregiver burden and psychological distress linked to frailty and functional dependency of a relative with advanced dementia. Dementia. 2020;19(2):301–18.
Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–38.
van der Steen JT, Radbruch L, Hertogh CM, et al. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med. Mar2014;28(3):197–209.
Eisenmann Y, Golla H, Schmidt H, Voltz R, Perrar KM. Palliative care in advanced dementia. Front Psych. 2020;11:699.
Australian Institue of Health and Welfare. Palliative care services in Australia. Available at: https://www.aihw.gov.au/reports/palliative-care-services/palliative-care-services-in-australia/contents/summary. Accessed July 2, 2023.
van Gaans D, Erny-Albrecht K, Tieman J. Palliative Care Within the Primary Health Care Setting in Australia: A Scoping Review. Public Health Rev. 2022;43:1604856.
Department of Health and Aged Care. The National Palliative Care Strategy 2018 2019.
Palliative Care Australia. Palliative Care Service Development Guidelines 2018.
BROWN L, HANSNATA E, LA HA. Economic cost of dementia in Australia 2016–2056: report prepared for Alzheimer’s Australia. 2017.
Goodman C, Evans C, Wilcock J, et al. End of life care for community dwelling older people with dementia: an integrated review. International Journal of Geriatric Psychiatry: A journal of the psychiatry of late life and allied sciences. 2010;25(4):329–37.
Houttekier D, Cohen J, Bilsen J, Addington‐Hall J, Onwuteaka‐Philipsen BD, Deliens L. Place of death of older persons with dementia. A study in five European countries. Journal of the American Geriatrics Society. 2010;58(4):751–756.
Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med. 2010;362(13):1173–80.
Morgan DD, Tieman JJ, Allingham SF, Ekström MP, Connolly A, Currow DC. The trajectory of functional decline over the last 4 months of life in a palliative care population: a prospective, consecutive cohort study. Palliat Med. 2019;33(6):693–703.
Stolz E, Gill TM, Mayerl H, Rásky É, Freidl W. Trajectories of late-life disability vary by the condition leading to death. The Journals of Gerontology: Series A. 2021;76(7):1260–4.
Ding J, Johnson CE, Lee YC, Gazey A, Cook A. Characteristics of people with dementia vs other conditions on admission to inpatient palliative care. J Am Geriatr Soc. 2020;68(8):1825–33.
Ding J, Cook A, Qin X, Ho SC, Johnson CE. Palliative care needs and utilization of specialist services for people imminently dying with dementia: A national population-based study. Int J Nurs Stud. 2020;109: 103655.
Harrison KL, Ritchie CS, Patel K, et al. Care settings and clinical characteristics of older adults with moderately severe dementia. J Am Geriatr Soc. 2019;67(9):1907–12.
Currow DC, Eagar K, Aoun S, Fildes D, Yates P, Kristjanson LJ. Is it feasible and desirable to collect voluntarily quality and outcome data nationally in palliative oncology care? J Clin Oncol. 2008;26(23):3853–9.
Daveson BA, Allingham SF, Clapham S, et al. The PCOC Symptom Assessment Scale (SAS): A valid measure for daily use at point of care and in palliative care programs. PLoS ONE. 2021;16(3): e0247250.
Masso M, Allingham SF, Johnson CE, et al. Palliative care problem severity score: reliability and acceptability in a national study. Palliat Med. 2016;30(5):479–85.
Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III). Medical care. 1994:668–685.
Abernethy AP, Shelby-James T, Fazekas BS, Woods D, Currow DC. The Australia-modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice [ISRCTN81117481]. BMC Palliat Care. 2005;4(1):1–12.
Masso M, Allingham SF, Banfield M, et al. Palliative care phase: inter-rater reliability and acceptability in a national study. Palliat Med. 2015;29(1):22–30.
Statistics ABO. Socio-economic indexes for areas (SEIFA). Canberra: Australian Bureau of Statistics. 2011.
Martinsson L, Lundström S, Sundelöf J. Better quality of end-of-life care for persons with advanced dementia in nursing homes compared to hospitals: a Swedish national register study. BMC Palliat Care. 2020;19:1–9.
Rosenwax L, Spilsbury K, Arendts G, McNamara B, Semmens J. Community-based palliative care is associated with reduced emergency department use by people with dementia in their last year of life: a retrospective cohort study. Palliat Med. 2015;29(8):727–36.
Wiencek C, Coyne P. Palliative care delivery models. Paper presented at: Seminars in oncology nursing, 2014.
Paz-Ruiz S, Gomez-Batiste X, Espinosa J, Porta-Sales J, Esperalba J. The costs and savings of a regional public palliative care program: the Catalan experience at 18 years. J Pain Symptom Manage. 2009;38(1):87–96.
Kamal AH, Currow DC, Ritchie CS, Bull J, Abernethy AP. Community-based palliative care: the natural evolution for palliative care delivery in the US. J Pain Symptom Manage. 2013;46(2):254–64.
Radbruch L, De Lima L, Knaul F, et al. Redefining palliative care—a new consensus-based definition. J Pain Symptom Manage. 2020;60(4):754–64.
Department of Health. Australian Government Response to the Final Report of the Royal Commission into Aged Care Quality and Safety 2021.
Faes K, Cohen J, Annemans L. Resource use during the last 6 months of life of individuals dying with and of Alzheimer’s disease. J Am Geriatr Soc. 2018;66(5):879–85.
Spetz J, Dudley N, Trupin L, Rogers M, Meier DE, Dumanovsky T. Few hospital palliative care programs meet national staffing recommendations. Health Aff. 2016;35(9):1690–7.
Corbett A, Husebo B, Malcangio M, et al. Assessment and treatment of pain in people with dementia. Nat Rev Neurol. 2012;8(5):264–74.
Hadjistavropoulos T, Herr K, Prkachin KM, et al. Pain assessment in elderly adults with dementia. Lancet Neurol. Dec2014;13(12):1216–27.
Puente-Fernández D, Campos-Calderón CP, Burgos AAE, Hueso-Montoro C, Roldán-López CB, Montoya-Juárez R. Palliative Care Symptoms, Outcomes, and Interventions for Chronic Advanced Patients in Spanish Nursing Homes with and without Dementia. Int J Environ Res Public Health. Feb 25 2020;17(5).
van de Rijt LJ, Feast AR, Vickerstaff V, Lobbezoo F, Sampson EL. Prevalence and associations of orofacial pain and oral health factors in nursing home residents with and without dementia. Age Ageing. 2020;49(3):418–24.
Acknowledgements
The authors would like to thank the PCOC team, particularly Dr. Barbara Daveson for providing data and comments on wording and data interpretation for the study. PCOC is a national palliative care project funded by the Australian Government Department of Health and Aged Care.
Authors consent
All authors had approved the final article.
Funding
This study is supported by Hunan Provincial Natural Science Foundation of China (#2023JJ40791). The funder had no role in the conduct of the study.
Author information
Authors and Affiliations
Contributions
Study concept and design: Guiyun Wang, Jinfeng Ding, Angus Cook, Claire Johnson and Maya Ebrahimi Zanjani. Acquisition of data: Jinfeng Ding, Angus Cook and Claire Johnson. Analysis and interpretation of data: Jinfeng Ding, Guiyun Wang. Drafting of the manuscript: Jinfeng Ding, Maya Ebrahimi Zanjani, Yunyun Dai. Critical revision of the manuscript for important intellectual content: Guiyun Wang, Jinfeng Ding, Maya Ebrahimi Zanjani, Angus Cook, Yunyun Dai, Minghui Tan, Qiwen (Simon) Qin, and Claire Johnson
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The PCOC program has been approved by Human Research Ethics Committee (HREC) of the University of Wollongong (HE06/045) and this study was granted wavier of consent by The University of Western Australia HREC (RA/4/1/8365). All participants gave informed consent, and their anonymity was preserved.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, G., Zanjani, M.E., Cook, A. et al. Characteristics of people diagnosed with dementia vs lung cancer and cardiovascular disease at commencement of community palliative care: a population–based study. BMC Palliat Care 23, 219 (2024). https://doi.org/10.1186/s12904-024-01545-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-024-01545-w