Abstract
Background
The prognostic value of the pretreatment prognostic nutritional index (PNI) for gynaecological malignancies remain unclear. This meta-analysis aimed to explore the predictive significance of the PNI for gynaecological tumours.
Methods
The PubMed, Embase, Web of Science, and Cochrane Library databases were searched up to January 30, 2024, to identify relevant studies. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated to assess the associations of the PNI with overall survival (OS), progression-free survival (PFS), and disease-free survival (DFS) in patients with gynaecological tumours. We examined the correlation of the PNI with clinicopathological parameters of patients with gynaecological carcinoma by utilizing pooled odds ratios (ORs) and 95% CIs.
Results
A total of 28 articles involving 9,428 patients were included in the meta-analysis. The results revealed that a low PNI significantly predicted worse OS (HR = 1.60, 95% CI: 1.39–1.84, P < 0.001), PFS (HR = 1.63, 95% CI: 1.20–2.23, P = 0.002), and DFS (HR = 1.73, 95% CI: 1.19–2.52, P = 0.004). In addition, the subgroup analysis confirmed that the PNI had a prognostic effect on OS for all cancer types, but a significant association with PFS was not observed in patients with cervical cancer. A low PNI was significantly associated with FIGO stages III‒IV (OR = 2.30, 95% CI: 1.89‒2.80, P < 0.001) and LN metastasis (OR = 2.76, 95% CI: 2. 05‒3.73, P < 0.001).
Conclusion
The PNI may be noninvasive and promising biomarker for predicting the prognosis of patients with gynaecological tumours.
Similar content being viewed by others
Introduction
Cervical, ovarian, and endometrial cancers are the three most common gynaecological malignancies. According to the most recent global cancer data, two of the top ten cancers with the highest mortality rates are gynaecological tumours, with ovarian cancer ranking high. Additionally, the incidence rate of cervical cancer among young people is increasing by 1–2% annually [1]. In contrast to the majority of solid tumours, the incidence and mortality rates of endometrial cancer have both significantly increased over the past decade [2]. Gynaecological malignancies pose a grave threat to women’s lives and health. Despite the rapid development of medical methods such as diagnosis, surgery, radiotherapy, and chemotherapy over the past few decades, which have increased survival rates, the prognosis for gynaecological cancer patients remains suboptimal [3, 4]. The prediction of the prognosis of patients with gynaecological cancers is crucial, and biomarkers can provide guidance for personalized optimized treatments. Therefore, there is an urgent need to detect and identify reliable and cost-effective biomarkers for gynaecological cancers.
Serum biological parameters, including the platelet-to-lymphocyte ratio [5], lymphocyte-to-monocyte ratio [6], neutrophil-to-lymphocyte ratio [7], and PNI [8], are important biomarkers for gynaecological cancers. The PNI, which is calculated based on lymphocytes and albumin in peripheral blood, can be used to evaluate nutritional status and the immune response. The PNI is calculated using the following formula: 10 × albumin (g/dl) + 0.05 × total lymphocyte count (/mm3). Buzby et al. first proposed that the PNI can be used to assess the risk of patients undergoing gastrointestinal surgery in 1980 [9]. This index was initially used to evaluate the prognosis of cancer patients [10]. Previous studies have shown that the PNI is associated with clinical pathological characteristics and survival prognosis in various cancers, such as lung cancer [11], colorectal cancer [12], and hepatocellular carcinoma [13]. Many studies have also explored the prognostic significance of the PNI in patients with gynaecological malignancies, but the results are inconsistent [14, 15]. Therefore, it is necessary to systematically and comprehensively study the value of the PNI in the prognosis of patients with gynaecological cancer.
In this study, we conducted a meta-analysis on the relationships between the PNI and clinical outcomes, such as OS, PFS, DFS and other clinical indicators, in gynaecological cancer patients. These findings will provide more evidence regarding the use of the PNI as a prognostic indicator for gynaecological cancer.
Materials and methods
All analyses in this report were based on previously published research, thus ethical approval and patient informed consent were not involved. Additionally, the review methods of this meta-analysis have been prospectively registered in PROSPERO (registration number: CRD42024507737).
Information sources and search strategy
Two investigators independently conducted a systematic literature search of the Web of Science, PubMed, Embase, and Cochrane Library databases up to January 30, 2024, to identify relevant publications. The search was conducted using the following terms: (“prognostic nutritional index” OR “PNI”) AND (“gynecological” OR “ovarian” OR “cervical” OR “endometrial”) AND (“cancer” OR “tumor” OR “neoplasm” OR “carcinoma”). Furthermore, eligible original publications and other relevant studies were identified by manually searching the reference lists of the included studies.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) gynaecological cancer patients diagnosed by pathology; (2) patients who did not take anti-inflammatory drugs and had no inflammation, active infection, or complications before preoperative blood examination; (3) articles that reported the relationship between the PNI and survival outcomes, which were assessed by OS and/or PFS and/or DFS; (4) articles that provided cut-off values for distinguishing high /low PNI; (5) articles that reported HRs and 95% CIs or had sufficient raw data to calculate these parameters; and (6) articles that were published in English. The exclusion criteria were as follows: (1) conference abstracts, commentaries, case reports, and reviews; (2) duplicate research data; (3) animal studies; (4) insufficient survival data to calculate HRs and 95% CIs; and (5) an NOS score < 6 points.
Data extraction
Two investigators independently evaluated and extracted survival data and study characteristics from the included studies. Any disagreements were resolved by a third researcher and team discussion. The following data were extracted first author, publication year, region, cancer type, sample size, median age, study duration, FIGO stage, treatment method, follow-up period, PNI cut-off value, and type of survival analysis. Additionally, the extraction of multivariate analysis data of HRs and 95% CIs was prioritized for assessing the prognostic value of the PNI. If HRs and 95% CIs were not provided in the study, survival data were calculated from Kaplan‒Meier curves via Engauge Digitizer 10.8 software.
Quality assessment
The Newcastle‒Ottawa Scale (NOS) was used to evaluate the quality of each included publication. Two authors independently performed the quality assessment. Scores on the NOS range from 0 to 9, and studies with a score of ≥ 6 were considered as high-quality.
Statistical analysis
The data were analysed via Stata 12.0 software (Stata Corporation, College Station, TX), with the significance level set at P < 0.05. The data for OS, PFS, and DFS were pooled using HRs and 95% CIs, and the data for clinicopathological parameters were pooled using ORs and 95% CIs. Cochran’s Q test and the I2 statistic were applied to evaluate study heterogeneity. When the P < 0.10 or I2 > 50%, there is significant heterogeneity. In such cases, the random effects model was adopted to pool the estimated HR and 95% CI. Otherwise, a fixed effects model was employed. Subgroup analysis, sensitivity analysis, and meta-regression were conducted to explore the sources of heterogeneity. Subgroups were divided based on the median integer values, and subgroup analyses were performed based on cancer type, region, sample size, median age, FIGO stage, cut-off values, median follow-up, and HR source. Furthermore, publication bias was assessed via Begg’s funnel plot and Egger’s test, with P < 0.05 indicating significant publication bias. Trim-and-fill procedures were utilized to adjust for publication bias.
Results
Search results and study characteristics
A total of 551 published articles were identified through the database search. We conducted a full-text evaluation of 36 publications after deleting duplicate studies and screening the titles and abstracts. At this stage, 8 studies were excluded (5 studies lacked relevant data, 2 studies had duplicate data, and 1 study had an NOS score less than 6 points). Ultimately, 28 articles involving 9428 patients were included in this meta-analysis. The detailed process is shown in Fig. 1.
Among the 28 included studies, one involved training and validation cohorts, and one involved research on two different FIGO stages. Therefore, a total of 30 datasets were used for statistical analysis in this study (Table 1). The cut-off value of the PNI in the included studies ranged from 38 to 52.83, and the sample sizes ranged from 32 to 1051. Among them, 9 studies evaluated the relationship between the PNI and prognosis in ovarian cancer patients, 13 studies focused on cervical cancer patients, and 6 studies focused on endometrial cancer patients. Additionally, 26 studies assessed clinical indicators for OS, 11 studies for PFS, and 6 studies for DFS. All the included studies had an NOS score of ≥ 6, indicating overall high quality. Further details on the other characteristics of the cohort studies are shown in Table 1.
Prognostic significance of the PNI for OS in gynaecological cancer
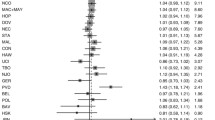
As shown in Figs. 2A and 27 datasets were used to examine the relationship between the PNI and OS in patients with gynaecologic cancers. Owing to significant heterogeneity among the studies, a random effects model was employed (I2 = 80.0%; P = 0.000). The results revealed that patients with a low PNI had a worse OS (HR = 1.60; 95% CI: 1.39–1.84; P < 0.001). To comprehensively assess the correlation between the PNI and OS, subgroup analyses were conducted based on cancer type, region, sample size, median age, FIGO stage, treatment, median follow-up, cut-off values, and survival. The results revealed that, with the exception of the II-IV stage subgroup (combined HR = 1.57; 95% CI: 0.73–3.41; P = 0.251), the other factors did not influence the prognostic effect of the PNI on OS (Supplementary Table S1). To explore the potential sources of heterogeneity, a meta-regression analysis was conducted, which revealed that factors such as cancer type (P = 0.923), region (P = 0.680), sample size (P = 0.986), median age (P = 0.667), FIGO stage (P = 0.965), treatment (P = 0.964), median follow-up (P = 0.919), cut-off value (P = 0.456), and survival analysis (P = 0.406) were not sources of heterogeneity.
Prognostic significance of the PNI for PFS in gynaecological cancer
A meta-analysis of thirteen datasets involving 2575 patients was conducted to analyse the prognostic value of the PNI for PFS. The pooled data indicated that, a low PNI serves as a poor predictor of PFS in patients with gynaecologic cancers (HR = 1.63; 95% CI: 1.20–2.23; P = 0.002) (Fig. 2B). Significant heterogeneity was observed (I2 = 78.8%; P = 0.000); thus, a random effects model was employed. Additionally, subgroup analyses were performed on relevant variables to study the prognostic significance of the PNI. Within subgroups such as the cervical cancer group, the median age < 54 years, I-II stage group, surgical treatment group, follow-up group, and univariate Cox survival analysis group, as well as the subgroup with a cut-off value > 48, the PNI did not have a statistically significant prognostic value for PFS, but their findings did not reverse this conclusion (Supplementary Table S2). A meta-regression analysis was subsequently conducted to explore the source of heterogeneity, revealing that cancer type (P = 0.309), region (P = 0.127), sample size (P = 0.293), age (P = 0.123), FIGO stage (P = 0.166), treatment (P = 0.503), follow-up duration (P = 0.283), cut-off value (P = 0.268), and survival analysis (P = 0.287) were unrelated to heterogeneity between studies.
Prognostic significance of the PNI for DFS in gynaecological cancer
Only six studies investigated the prognostic significance of the PNI for DFS in patients with gynaecological tumours. The meta-analysis results revealed that, compared with a high PNI, a low PNI was associated with worse DFS (HR = 1.73; 95% CI: 1.19–2.52; P = 0.004; Fig. 2C). Significant heterogeneity was observed in these studies. Hence, a random effects model was used to analyse the prognostic value of the PNI for DFS in gynaecologic cancer patients (I2 = 91.3%; P = 0.000).
Associations of the PNI with clinicopathological parameters in patients with gynaecological cancer
As listed in Table 2, a low PNI was significantly associated with a more advanced FIGO stage (OR = 2.30; 95% CI: 1.89–1.90; P < 0.001), the occurrence of LN metastasis (OR = 2.76; 95% CI: 2.05–3.73; P < 0.001), a lower BMI (OR = 1.46; 95% CI: 1.00–2.14; P = 0.049), the occurrence of ascites (OR = 3.60; 95% CI: 2.11–6.15; P < 0.001) and larger tumours (OR = 2.05; 95% CI: 1.39–3.03; P < 0.001) in gynaecological cancer patients. There was no obvious association of the PNI with age (P = 0.194), or histological grade (P = 0.175).
Sensitivity analysis
In studies evaluating OS, PFS, and DFS as endpoints for gynaecological cancer, significant heterogeneity existed among the studies. Therefore, we conducted a sensitivity analysis. The analysis results indicated that the combined HRs for OS, PFS, and DFS were not obviously affected after excluding any single study (Fig. 3), which suggested that our conclusions were relatively robust.
Publication bias
Egger’s and Begg’s funnel plots were used to analyse the publication bias of studies with OS, PFS, and DFS as endpoints. For OS, no significant publication bias was detected via in Begg’s test (P = 0.707), but Egger’s funnel plot revealed asymmetry, indicating significant publication bias (P < 0.001; Fig. 4A). No changes in the prognostic significance of the PNI for OS were found after the trim-and-fill method (HR = 1.42; 95% CI: 1.24–1.62; P < 0.001; Fig. 4B). In terms of PFS, the results indicated that no significant publication bias was detected in the included studies (Egger’s test: P = 0.10; Begg’s test: P = 0.36; Fig. 4C). Furthermore, only six studies reported the DFS endpoint, and thus, we did not analyse publication bias for this outcome.
Discussion
Our meta-analysis, which was based on data from 28 studies comprising a total of 9428 patients, investigated the precise role of the PNI in predicting gynaecological cancer outcomes. The results indicated that a lower PNI significantly predicted poor survival outcomes, such as shorter OS, PFS, and DFS. Subgroup analysis revealed that the PNI had significant prognostic value for the OS of patients with different types of gynaecological cancers regardless of the treatment strategy. Owing to its ease of accessibility and cost-effectiveness, the PNI can serve as an economical, effective, and reliable prognostic marker for gynaecological cancer patients. In addition, to the best of our knowledge, this meta-analysis is the first to investigate whether the PNI can be used as an independent prognostic marker for patients with these three major gynaecological malignancies.
According to the guidelines of the ESGO/ESTRO/ESP (European Society of Gynaecological Oncology, European Society for Radiotherapy and Oncology–European Society of Pathology), FIGO stage, tumour grade, histological type, and lymph node metastasis are the most common clinical prognostic indicators [16]. Higher FIGO stages generally correlate with poorer patient prognosis. Our results indicate that a decreased PNI is associated with advanced FIGO stage, lymph node metastasis, and larger tumours in gynaecologic cancer patients, suggesting that patients with a low PNI are more prone to tumour metastasis and more severe cancer. Our findings confirm that the PNI is highly consistent with prognostic indicators such as FIGO stage, further reinforcing its clinical prognostic value and establishing it as a more promising personalized prognostic indicator.
The PNI is calculated based on serum albumin levels and peripheral blood lymphocyte counts [17]. Albumin levels can reveal the nutritional status of cancer patients, whereas low albumin levels indicate malnutrition. Research has shown that malnutrition can lead to adverse clinical outcomes by altering organ function and cellular physiology, and is closely related to a decrease in survival and quality of life in gynaecological cancer patients [18]. Moreover, serum albumin, which is an acute-phase protein [19], is related to the inflammatory response, and can activate the cytokines IL–1 and TNF–α [20, 21]. The regulation of the tumour microenvironment by cytokines can stimulate cancer cell growth and affect the prognosis of patients [22]. Lymphocytes play an important role in cell-mediated immunity, and can inhibit the proliferation and invasion of tumour cells via cytokine-related cytotoxicity [23, 24]. A previous report demonstrated that both inflammation and immune cells could lead to a decrease in the lymphocyte count in ovarian cancer [25]. On the basis of the above mechanisms, a low PNI indirectly indicates insufficient nutritional and immune function in cancer patients, leading to increased tumour invasiveness. Therefore, this nutritional prognosis index is more likely to predict adverse pathological features and poorer survival rates in cancer patients.
Previous studies have explored the prognostic impact of the PNI in different types of tumours. In 2014, Sun et al. first investigated the correlation between a decreased PNI and poorer overall survival, suggesting that the PNI is a powerful indicator of poor prognosis [26]. In 2023, Hu et al. reported that in a meta-analysis including 2,322 patients, a lower PNI was closely associated with poorer OS in breast cancer patients [27]. A recent meta-analysis of 10 studies involving 3130 patients revealed that oral cancer patients with a lower PNI had poorer DFS and OS, suggesting that the PNI is an effective prognostic indicator for oral cancer patients [28]. In their meta-analysis, Xiong and colleagues reported that a low preoperative PNI in renal cell carcinoma patients was an adverse factor for OS, PFS, and DFS, potentially serving as an unfavourable prognostic marker associated with adverse clinicopathological features [29]. In another meta-analysis recruiting 2,627 gastrointestinal stromal tumours, a reduced PNI was indicative of poorer recurrence–free survival [30]. In the current meta-analysis, we identified a low PNI as an indicator of poorer survival prognosis in gynaecological cancer patients, which is consistent with findings in other cancers.
In addition, in 2019, Wang et al. performed a meta-analysis including only nine retrospective articles and concluded that the PNI was independently associated with OS in patients with gynaecologic cancers. However, they did not include studies on endometrial cancer [31]. Due to significant differences in the clinical characteristics and prognoses of patients with ovarian, cervical, and endometrial cancer, it is crucial to include all relevant studies on these three types of cancer to ensure a more accurate conclusion. Therefore, this study searched relevant published literature and ultimately included 28 studies involving 9,428 patients from various countries. Although the results of the meta-analysis are similar to those of previous studies, our analysis included more research on the three gynaecological cancers. Notably, our study newly incorporated six reports related to endometrial cancer, such as those by Kiuchi et al. [32], Mirili et al. [33], Gen et al. [34], Njoku et al. [35], Zhang et al. [36] and Yuan et al. [37]. Additionally, our study included research from the UK, South Korea, Japan, Turkey and other countries. In particular, studies conducted by Karakaş et al. [38], Kiuchi et al. [32], and Zhang et al. [39]. over the past five years have indicated that the PNI is not an independent prognostic factor. Furthermore, this study systematically evaluated various factors that affect prognosis, such as stage, age, follow-up, and treatment. Updating the evidence on this issue is crucial for appropriate clinical applications, and our findings may still have some clinical practicality and significance.
Study limitations
The current meta-analysis has several limitations. First, the majority of studies included in our meta-analysis were retrospective, inevitably leading to potential flaws and biases in the original data. Second, most of the included studies were from Asia, which inevitably introduces regional differences, necessitating the inclusion of research from different countries. Third, the critical value of the PNI has not been standardized due to variations in cut-off threshold selection. Fourth, the cancer treatment strategies included were not entirely consistent, which could affect patient survival and introduce heterogeneity.
Recommendations for further research
To conduct a more accurate assessment of publication bias, the number of studies included in the meta-analysis from diverse regions and published in different languages should be increased. Incorporating more studies helps stabilize the funnel plot and yields more reliable analysis outcomes. Additionally, future research should prioritize the exploration of potential sources of heterogeneity, which may encompass the study design, patient treatment approaches, a specific PNI cut-off value, and demographic characteristics of the subjects. Furthermore, to further explore the prognostic value of the PNI in gynaecologic cancers, larger-scale studies with more high-quality prospective trials are necessary.
Conclusion
This meta-analysis demonstrated that a low PNI was significantly associated with poor prognosis in gynaecological cancer patients in terms of OS, PFS, and DFS. Therefore, the PNI can be used as an effective prognostic indicator, not only to help clinicians better assess the prognosis of patients but also to formulate more precise treatment strategies for patients.
Data availability
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):12–49.
Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229–63.
Armstrong DK, Alvarez RD, Backes FJ, Bakkum-Gamez JN, Barroilhet L, Behbakht K, Berchuck A, Chen LM, Chitiyo VC, Cristea M, et al. NCCN Guidelines® insights: ovarian Cancer, Version 3.2022. J Natl Compr Cancer Network: JNCCN. 2022;20(9):972–80.
Mayadev JS, Ke G, Mahantshetty U, Pereira MD, Tarnawski R, Toita T. Global challenges of radiotherapy for the treatment of locally advanced cervical cancer. Int J Gynecol cancer: Official J Int Gynecol Cancer Soc. 2022;32(3):436–45.
Yu J, Huang L, Dong T, Cao L. Prediction of outcomes after chemoradiotherapy for cervical cancer by neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. J Obstet Gynaecology: J Inst Obstet Gynecol. 2024;44(1):2361858.
Bilir F, Arioz DT, Vatansever N, Filiz T, Elaziz B. Hematologic parameters as a predictor of myometrial and cervical invasion in endometrial cancer. Minerva Obstet Gynecol. 2021;73(6):770–5.
Pergialiotis V, Papalios T, Haidopoulos D, Papapanagiotou A, Vlachos A, Rodolakis A, Thomakos N. Pre-operative neutrophil-to-lymphocyte ratio as a predictor of post-operative infectious morbidity in Gynecologic Oncology patients. Surg Infect. 2023;24(4):390–6.
Li P, Lai Y, Tian L, Zhou Q. The prognostic value of prognostic nutritional index in advanced cancer receiving PD-1/L1 inhibitors: a meta-analysis. Cancer Med. 2022;11(16):3048–56.
Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139(1):160–7.
Onodera T, Goseki N, Kosaki G. [Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients]. Nihon Geka Gakkai Zasshi. 1984;85(9):1001–5.
Hayasaka K, Notsuda H, Onodera K, Watanabe T, Watanabe Y, Suzuki T, Hirama T, Oishi H, Niikawa H, Okada Y. Prognostic value of perioperative changes in the prognostic nutritional index in patients with surgically resected non-small cell lung cancer. Surg Today 2024.
Liu LX, Wang H, Gao B, Xu TT, Yuan QG, Zhou SZ, Ding C, Miao J, Guan WX. Preoperative controlling nutritional status as an optimal prognostic nutritional index to predict the outcome for colorectal cancer. World J Gastrointest Oncol. 2024;16(2):343–53.
Ho CT, Chia-Hui Tan E, Lee PC, Chu CJ, Huang YH, Huo TI, Hou MC, Wu JC, Su CW. Prognostic Nutritional Index as a prognostic factor for very early-stage Hepatocellular Carcinoma. Clin Translational Gastroenterol. 2024;15(4):e00678.
Tan F, Xia R, Zeng L, Xie H, Long X, Peng C. Value of preoperative controlling nutritional status score in prognosis of patients with high-risk factors for early-stage cervical cancer. Pakistan J Med Sci. 2024;40(1Part–I):120–7.
Zhang W, Liu K, Ye B, Liang W, Ren Y. Pretreatment C-reactive protein/albumin ratio is associated with poor survival in patients with stage IB-IIA cervical cancer. Cancer Med. 2018;7(1):105–13.
Cibula D, Raspollini MR, Planchamp F, Centeno C, Chargari C, Felix A, Fischerová D, Jahnn-Kuch D, Joly F, Kohler C, et al. ESGO/ESTRO/ESP guidelines for the management of patients with cervical cancer - update 2023. Virchows Archiv: Int J Pathol. 2023;482(6):935–66.
Kang SH, Cho KH, Park JW, Yoon KW, Do JY. Onodera’s prognostic nutritional index as a risk factor for mortality in peritoneal dialysis patients. J Korean Med Sci. 2012;27(11):1354–8.
Yan X, Zhang S, Jia J, Yang J, Song Y, Duan H. Total parenteral Nutrition Treatment improves the Nutrition Status of Gynecological Cancer patients by improving serum albumin level. Front Med. 2021;8:759387.
Erstad BL. Serum albumin levels: who needs them? Annals Pharmacotherapy. 2021;55(6):798–804.
Buck M, Zhang L, Halasz NA, Hunter T, Chojkier M. Nuclear export of phosphorylated C/EBPbeta mediates the inhibition of albumin expression by TNF-alpha. EMBO J. 2001;20(23):6712–23.
Sohda M, Sakai M, Yamaguchi A, Watanabe T, Nakazawa N, Ubukata Y, Kuriyam K, Sano A, Yokobori T, Ogawa H, et al. Pre-treatment CRP and albumin determines prognosis for Unresectable Advanced Oesophageal Cancer. In vivo (Athens Greece). 2022;36(4):1930–6.
Yu X, Zhang X. Prognostic role of C-reactive protein in patients with endometrial cancer: a meta-analysis. Biomark Med. 2024;18(6):279–89.
Fan Z, Zhang Q. Molecular mechanisms of lymphocyte-mediated cytotoxicity. Cell Mol Immunol. 2005;2(4):259–64.
Wu ES, Oduyebo T, Cobb LP, Cholakian D, Kong X, Fader AN, Levinson KL, Tanner EJ 3rd, Stone RL, Piotrowski A, et al. Lymphopenia and its association with survival in patients with locally advanced cervical cancer. Gynecol Oncol. 2016;140(1):76–82.
Winkler I, Woś J, Bojarska-Junak A, Semczuk A, Rechberger T, Baranowski W, Markut-Miotła E, Tabarkiewicz J, Wolińska E, Skrzypczak M. An association of iNKT+/CD3+/CD161 + lymphocytes in ovarian cancer tissue with CA125 serum concentration. Immunobiology. 2020;225(6):152010.
Sun K, Chen S, Xu J, Li G, He Y. The prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2014;140(9):1537–49.
Hu G, Ding Q, Zhong K, Wang S, Wang S, Huang L. Low pretreatment prognostic nutritional index predicts poor survival in breast cancer patients: a meta-analysis. PLoS ONE. 2023;18(1):e0280669.
Dai M, Sun Q. Prognostic and clinicopathological significance of prognostic nutritional index (PNI) in patients with oral cancer: a meta-analysis. Aging. 2023;15(5):1615–27.
Xiong SC, Hu X, Lia T, Wang YH, Li X. Prognostic significance of Prognostic Nutritional Index in patients with renal cell carcinoma: a Meta-analysis. Nutr Cancer. 2022;74(3):860–8.
Li Z, Zhang D, Mo C, Zhu P, Fan X, Tang T. The prognostic significance of prognostic nutritional index in gastrointestinal stromal tumors: a systematic review and meta-analysis. Medicine. 2022;101(47):e32067.
Wang X, Wang Y. The prognostic nutritional index is prognostic factor of gynecological cancer: a systematic review and meta-analysis. Int J Surg (London England). 2019;67:79–86.
Kiuchi K, Hasegawa K, Ochiai S, Motegi E, Kuno T, Kosaka N, Fukasawa I. Prognostic significance of inflammatory parameters and nutritional index in clinical stage IVB endometrial carcinomas. J Obstet Gynaecology: J Inst Obstet Gynecol. 2019;39(2):237–41.
Mirili C, Bilici M. Inflammatory prognostic markers in endometrial carcinoma: systemic immune-inflammation index and prognostic nutritional index. Med Sci Discovery. 2020;7:351–9.
Gen Y, Yun J, Ahn J, Yoon JH, Park DC, Kim SI. Nutritional index in relation to prognosis of endometrial cancer. Int J Med Sci. 2024;21(1):169–74.
Njoku K, Barr CE, Ramchander NC, Crosbie EJ. Impact of pre-treatment prognostic nutritional index and the haemoglobin, albumin, lymphocyte and platelet (HALP) score on endometrial cancer survival: a prospective database analysis. PLoS ONE. 2022;17(8):e0272232.
Zhang N, Liu H, Yang J, Zhong F. Development and validation of a nomogram based on multiple preoperative immunoinflammatory indexes for survival prediction in patients with stage IA-IB endometrial cancer. Am J Translational Res. 2023;15(10):6286–98.
Yuan J, Wang Q, Cheng J, Wang J, Zhang Y. Using preoperative control nutritional status scores as prognostic factors for endometrial cancer. Front Oncol. 2023;13:1126576.
Karakaş S, Demirayak G, Önder AB, Özdemir İA, Comba C, Süzen Çaypınar S, Yıldız Ş, Avşar S, Bağhaki S, Yıldız G, et al. The Association between the Preoperative Prognostic Nutritional Index and the Controlling Nutritional Status score on Tumor Stage, Chemotherapeutic Response and overall survival in Ovarian Cancer. Nutr Cancer. 2022;74(5):1770–9.
Zhang G, Zhang Y, He F, Wu H, Wang C, Fu C. Preoperative controlling nutritional status (CONUT) score is a prognostic factor for early-stage cervical cancer patients with high-risk factors. Gynecol Oncol. 2021;162(3):763–9.
Acknowledgements
Not applicable.
Funding
This study was supported by Dalian Municipal Health Commission (grant number 23Z11001).
Author information
Authors and Affiliations
Contributions
Conceptualization: CL, JQL, QZ; Data curation: CL, QZ, YLY; Formal analysis: JQL, CL, ZY; Methodology: CL, QZ, YLY, ZY, JQL; Software: CL, QZ, YLY; Validation: JQL, CL, ZY, Writing-original draft: JQL, CL, QZ, YLY, ZY; Writing-review & editing: JQL, CL, QZ, YLY, ZY, WW. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, C., Yin, Y., Yang, Z. et al. Prognostic effect of the pretreatment prognostic nutritional index in cervical, ovarian, and endometrial cancer: a meta-analysis. BMC Women's Health 24, 464 (2024). https://doi.org/10.1186/s12905-024-03310-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-024-03310-w