Abstract
Background
A high proportion of medical school graduates pursue specialties different from those declared at matriculation. While these choices influence the career paths, satisfaction, and potential regret students will experience, they also impact the supply and demand ratio of the shorthanded physician workforce across many specialties. In this study, we investigate how the choice of medical specialty and the factors motivating those choices change between the beginning and end of medical school training.
Methods
A questionnaire was administered annually from 2017 to 2020 to a cohort of medical students at the University of Connecticut to determine longitudinal preferences regarding residency choice, motivational factors influencing residency choice, future career path, and demographic information.
Results
The questionnaire respondent totals were as follows: n = 76 (Year 1), n = 54 (Year 2), n = 31 (Year 3), and n = 65 (Year 4). Amongst newly matriculated students, 25.0% were interested in primary care, which increased ~ 1.4-fold to 35.4% in the final year of medical school. In contrast, 38.2% of matriculated students expressed interest in surgical specialties, which decreased ~ 2.5-fold to 15.4% in the final year. Specialty choices in the final year that exhibited the largest absolute change from matriculation were orthopedic surgery (− 9.9%), family medicine (+ 8.1%), radiology (+ 7.9%), general surgery (− 7.2%), and anesthesiology (+ 6.2%). Newly matriculated students interested in primary care demonstrated no differences in their ranking of motivational factors compared to students interested in surgery, but many of these factors significantly deviated between the two career paths in the final year. Specifically, students interested in surgical specialties were more motivated by the rewards of salary and prestige compared to primary care students, who more highly ranked match confidence and family/location factors.
Conclusions
We identified how residency choices change from the beginning to the end of medical school, how certain motivational factors change with time, how these results diverge between primary care and surgery specialty choice, and propose a new theory based on risk-reward balance regarding residency choice. Our study promotes awareness of student preferences and may help guide school curricula in developing more student-tailored training approaches. This could foster positive long-term changes regarding career satisfaction and the physician workforce.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
For medical students, deciding on a residency specialty that will guide careers and impact personal lives is a complicated and multifactorial process, made even more difficult by the complex and stressful nature of attempting to switch residency specialties post hoc [1]. These decisions have broad implications regarding healthcare and biomedical research across the globe, namely an imbalance between physician supply and demand in primary care [2,3,4], surgery [5,6,7], research [8,9,10], and clinical subspecialties [11,12,13], a disparity that dates back over a century and will continue to worsen for the foreseeable future [14,15,16]. These disparities can have a significant impact on healthcare outcomes. For example, a greater supply of primary care physicians per capita is associated with improved cardiovascular health, lower mortality, increased lifespan, and a reduction in low birth-weight rates [17,18,19]. While the physician workforce landscape is shaped by numerous variables that can differ in importance and oversight across municipalities, states/provinces, and countries, principal persistent factors that contribute are the personal desires and interests of the physician trainees themselves, which may or may not align with the needs of the healthcare system [20].
Investigating which specialties medical students prefer and why has been of long-standing interest to medical schools and healthcare administrations, as a better understanding of these preferences could provide insights that enable improvements to education curricula that better foster the wants and needs of future physicians and the healthcare system. Previous studies have demonstrated that the residency preferences of matriculating medical students change by the time a final residency choice is made at the end of medical school [21, 22]. Additionally, students have demonstrated a persistent tendency to categorically switch preference between primary care and surgical specialties [23,24,25,26]. Notably, a particularly worrisome finding is the degree of regret and dissatisfaction amongst residents and physicians with regard to their career choice [1, 27, 28]. While informative studies have observed specific predictive factors influencing residency choice, such as demographics, interest, lifestyle, finances, and prestige, the single time point nature of these studies limits our understanding of how these factors may change over time [23,24,25, 29,30,31,32], and results can be further confounded due to recall bias from methods that require retrospective assessment by respondents. Moreover, alterations to the medical curriculum itself have been shown to impact residency choice [33,34,35,36], making it imperative to obtain accurate and current data regarding student preferences that can be used to facilitate optimal curriculum changes.
In this longitudinal study, we track the residency specialty preferences and motivational factors for a cohort of U.S. medical students throughout their training at the University of Connecticut School of Medicine. The aim of this study is to identify if and how the residency preferences of newly matriculated medical students change compared to the residency specialties chosen in their last year of medical school. Concurrently, this study also aims to investigate the factors influencing residency choice, with a focus on how these factors may or may not change with time and between specialty categories, such as between primary care and surgical specialties. The results from this study will add to the growing understanding of medical student career preferences. This may help to inform decisions regarding medical education, such as more personalized training plans that foster career satisfaction and guidance towards in-demand specialties.
Methods
Subjects and questionnaire
This study was reviewed by the Institutional Review Board (IRB) at UConn Health and qualified for exempt status (IRB number 18–062-3). A voluntary, self-administered questionnaire (Table 1) was developed to longitudinally assess medical students’ residency specialty preferences, as well as the factors motivating those preferences, throughout their medical school training towards conferral of their medical degree (M.D.). A survey was chosen as the data collection instrument in order to measure attitudes/beliefs, as these qualities are personal/internal and thus not directly observable. The questionnaire was administered annually from 2017 to 2020 to the same student cohort from the University of Connecticut School of Medicine (UConn SOM Class of 2021), a 4-year M.D.-granting medical school in the U.S., starting upon matriculation (Year 1; n = 102 matriculants) and concluding during submission of residency applications using the Electronic Residency Application Service (ERAS) (Year 4; n = 100 matches). The anonymous questionnaire consisted of respondents self-reporting their preferred (Years 1–3) or chosen (Year 4) residency specialty, their likely career path following residency (e.g. subspecialty training, research, etc.), and ranking the various motivational factors (e.g. specialty lifestyle, prestige, etc.) on these stated choices from least important to most important, in addition to demographics information (e.g. age, marital status, etc.). To meet recent guidelines for survey-based research, this questionnaire format (Table 1) is similar to what has been utilized in previous studies [22, 23, 37], was reviewed by two faculty members unaffiliated with the study, and a survey trial with interview-based feedback was performed using a small number of respondents outside the cohort of interest to ensure content, face, and response process validity as well as interrater reliability [38, 39].
Procedure
For Years 1–3, the questionnaire was administered in person at curriculum sessions in which a majority of students would be present, such as at the end of lecture (Years 1–2) or prior to an orientation session (Year 3) and students were given 20 min to complete the survey. The surveyors (F.A.L. and A.M.P.) announced the goals and voluntary/anonymous nature of the study to the students present, distributed paper copies of the questionnaire, and collected the completed questionnaires with respect to respondent anonymity. Due to the COVID-19 pandemic, the Year 4 questionnaire was distributed using the class email listserv and voluntary, anonymous responses were submitted electronically. No incentive was offered for completing the survey.
Data analysis
The data obtained in this study were electronically cataloged and analyzed. Data in this study excluded oral and maxillofacial surgery and preliminary surgery Match outcomes, as well as longitudinal results from students in dual degree programs (e.g. M.D./Ph.D., M.D./M.B.A, etc), as these represent atypical training timelines and/or career paths. For comparison and correlation to the Year 4 survey results, the specialty match results from the National Resident Matching Program (NRMP) for the UConn SOM Class of 2021 (n = 100 students) were also included in this study. For the “primary care” specialty categorization, this encompassed internal medicine, pediatrics, and family medicine, as defined by the American Academy of Family Physicians (AAFP). For the “surgery” specialty categorization, this encompassed general surgery, orthopedic surgery, neurological surgery, vascular surgery, plastic surgery, otolaryngology, and urology, as defined by the American College of Surgeons (ACS). Obstetrics and gynecology (OB/GYN) was excluded from either classification due to its hybrid nature and evolving landscape [40,41,42,43].
With the potential for small sample sizes due to specific residency choice, incomplete questionnaires, and/or survey distribution logistics (i.e. cohort availability), a 90% confidence level (α = 0.1) was chosen [44, 45]. For analysis, the percentages of students who chose each residency specialty were calculated relative to the total respondents for each year the questionnaire was completed. To assess correlation between Year 4 survey results and Match outcomes, a Pearson correlation coefficient (r) and its associated P-value were calculated using GraphPad Prism. The importance of the six factors motivating the chosen specialties, which were numerically recorded on an ordinal scale from least important (1) to most important (6), were compiled by both medical school year and specialty choice. The median scale values and interquartile ranges were calculated and plotted in GraphPad Prism. Statistical comparisons were performed using nonparametric Mann-Whitney U tests in GraphPad Prism, and the resulting P-values were considered statistically significant if P ≤ 0.1.
Results
The total number of cohort respondents by year were n = 76 for Year 1, n = 54 for Year 2, n = 31 for Year 3, and n = 64 for Year 4, as summarized in Table 2. Due to the lower response rate in Years 2 and 3, we directed our focus and analyses on Years 1 and 4. The age range for Year 1 respondents was 21–33 years-old and 25–34 years-old for Year 4 respondents. This was accompanied by an increase in the percentage of married respondents (6.6% in Year 1 and 15.6% in Year 4) and respondents with children (0.0% in Year 1 and 3.1% in Year 4).
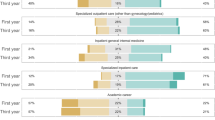
With regard to residency specialty choices (Table 3), the top six choices for the entering students in Year 1 were internal medicine (14.5%), emergency medicine (14.5%), orthopedic surgery (14.5%), general surgery (11.8%), pediatrics (7.9%), and OB/GYN (7.9%). For Year 4, the top six residency specialty choices were internal medicine (15.4%), emergency medicine (12.3%), family medicine (10.8%), pediatrics (9.2%), OB/GYN (9.2%), and radiology (9.2%). Of note, the specialty choices that exhibited the greatest absolute change from Year 1 to Year 4 were orthopedic surgery (− 9.9%), family medicine (+ 8.1%), radiology (+ 7.9%), general surgery (− 7.2%), and anesthesiology (+ 6.2%). This correlated well with the final NRMP Match outcomes for this cohort of UConn SOM students (r = 0.91, P < 0.001), as the greatest absolute changes from Year 1 to the Match were orthopedic surgery (− 12.5%), anesthesiology (+ 8.0%), general surgery (− 7.8%), radiology (+ 6.7%), and family medicine (+ 5.4%; tied with psychiatry). Of note, the least popular specialties—those that garnered no interest in Year 1 and no Match outcomes—were child neurology, combined internal medicine and pediatrics (med-peds), pathology, and physical medicine and rehabilitation. Finally, the majority of students reported a desire to pursue fellowship/subspecialty training after residency in both Year 1 (51.3%) and Year 4 (66.2%), whereas 0% of Year 1 students were interested in research compared to 13.8% of students in Year 4 (Table 4). Industry was the least likely post-residency path for respondents, with only 2.6% of Year 1 students and 4.6% of Year 4 students expressing interest.
To determine which factors may motivate a student’s preferred/chosen residency specialty, we asked respondents to rank six factors—family/location, field interest, prestige, lifestyle, financial incentive, and match confidence—from least important to most important in motivating their reported residency specialty choice. Using a linear scale (1 = least important to 6 = most important) to numerically compare these responses, we identified no significant leading motivational factor in Year 1, as the median ranking was relatively similar across the six assessed factors (Fig. 1). However, when compared to Year 4, significant changes were observed. Interest in the field itself (e.g. underlying science, day-to-day duties, target patient population, subsequent training opportunities, etc.) and field lifestyle (e.g. hours) significantly increased in importance in Year 4, whereas field prestige, financial incentive (e.g. salary), and match confidence significantly decreased in importance. The importance of family and/or location requirements did not significantly change from Year 1 to Year 4.
Factors motivating residency choice. Median and interquartile range for the six motivational factors influencing choice of residency specialties from least important (1) to most important (6), comparing the student cohort in Year 1 (white circle) versus Year 4 (black square). P-values were calculated using Mann-Whitney U tests
As we observed disparities and changes between specialty choices within and between Years 1 and 4, we next set out to compare interest amongst broad specialty categorizations, specifically primary care versus surgery, as change between these specialty categories during medical school has been shown to occur across studies from multiple decades [23,24,25, 35, 36]. In Year 1, 25.0% of students were interested in primary care specialties (internal medicine, pediatrics, or family medicine), which increased ~ 1.4-fold to 35.4% in Year 4 and ~ 1.3-fold to 32.0% in the final Match outcome (Fig. 2A). In contrast, 38.2% of Year 1 students expressed interest in surgical specialties (orthopedic surgery, general surgery, neurological surgery, vascular surgery, plastic surgery, otolaryngology, and urology), which decreased ~ 2.5-fold to 15.4% in Year 4 and ~ 2.7-fold to 14.0% in the final Match outcome (Fig. 2B).
With the knowledge that considerable changes occurred between the proportion of students interested in primary care versus surgery in Year 1 compared to Year 4 and the Match, we next wanted to assess if and how our panel of motivational factors may have changed within primary care and surgery from Year 1 to Year 4. For primary care, interest in the field itself significantly increased as a factor motivating students’ choice of a career in a primary care specialty from Year 1 to Year 4, whereas prestige and financial incentives associated with primary care specialties decreased (Fig. 3A). Specialty lifestyle, match confidence, and family/location factors did not significantly change. For surgery, interest in the field itself significantly increased from Year 1 to Year 4, while the influence of prestige decreased (Fig. 3B). Factors pertaining to specialty lifestyle, financial incentive, match confidence, and family/location did not significantly change amongst those interested in surgery between Years 1 and 4.
Factors influencing residency choice by year within primary care and surgery. Median and interquartile range for the six motivational factors influencing choice of residency specialties from least important (1) to most important (6), comparing A) the student cohort in Year 1 (white circle) versus Year 4 (black square) amongst those who chose primary care specialties, and B) the student cohort in Year 1 (white circle) versus Year 4 (black square) amongst those who chose surgical specialties. P-values were calculated using Mann-Whitney U tests
Additional analyses were performed to assess if and how these motivational factors differ between primary care and surgery within Year 1 and Year 4. For Year 1, none of the surveyed factors demonstrated a significant difference between students who were interested in primary care versus surgery (Fig. 4A); however, significant changes were observed in Year 4 (Fig. 4B). The influence of family and/or location factors was significantly lower in students who had chosen a surgical specialty in Year 4 compared to primary care, as was the importance of confidently matching into the specialty of choice. Furthermore, specialty prestige and financial incentive were more influential amongst students who were pursuing a surgical specialty. Field interest and lifestyle were not significantly different between the two groups in Year 4.
Factors influencing residency choice between primary care and surgery in Years 1 and 4. Median and interquartile range for the six motivational factors influencing choice of residency specialties from least important (1) to most important (6), comparing A) Year 1 medical students who chose primary care (white square) versus surgical (black triangle) specialties, and B) Year 4 medical students who chose primary care (white square) versus surgical (black triangle) specialties. P-values were calculated using Mann-Whitney U tests
Discussion
The principal finding of this study is that the factors motivating medical student residency preference change over the course of medical school and differ between primary care and surgical specialties. Importantly, these motivational factors did not differ between specialty preference at matriculation. We show that specific factors motivate the final choice between primary care and surgical specialties, providing evidence that may help guide medical schools in promoting more student-tailored curricula that help foster long-term career satisfaction, which is particularly important in this era of increasing physician burnout and worsening mismatch between physician supply and demand.
In the cohort surveyed in this study, a considerable decrease was observed regarding the proportion of students choosing surgical specialties in their final year compared to matriculation. The top residency choices at matriculation were internal medicine (14.5%), emergency medicine (14.5%), orthopedic surgery (14.5%), general surgery (11.8%), pediatrics (7.9%), and OB/GYN (7.9%). In contrast, the top choices for this cohort in their final year were internal medicine (15.4%), emergency medicine (12.3%), family medicine (10.8%), pediatrics (9.2%), OB/GYN (9.2%), and radiology (9.2%). Notably, 25.0% of students at matriculation were interested in primary care, while 38.2% were interested in surgical specialties. In the final year, these results shifted to 35.4 and 15.4%, respectively. The specialty choices that exhibited the greatest absolute change were orthopedic surgery (− 9.9%), family medicine (+ 8.1%), radiology (+ 7.9%), general surgery (− 7.2%), and anesthesiology (+ 6.2%). The final year survey results were similar to the final NRMP Match results for this cohort.
These results are in accord with previous studies, which have demonstrated that ~ 30% of medical graduates now pursue primary care, a globally applicable percentage that has been in decline across multiple countries [22, 30, 46, 47]. Similarly, a decline in graduating medical students choosing surgical specialties has been observed over the years, such that ~ 15% of medical graduates now pursue surgery [6, 7, 48, 49], in line with the percentage observed in our study. The other ~ 55% of graduates mostly pursue emergency medicine, OB/GYN, radiology, anesthesiology, and psychiatry, in varying proportions. Moreover, the declining entry rates of students into primary care and surgery are generally inconsistent with student preferences upon matriculation, as it has been previously reported that students choose residencies different than the ones they claim to be interested in upon matriculation [21,22,23,24,25, 50]. Within this context, our study further supports this by providing the most current investigation of these multi-decade patterns that continue to afflict physician supply.
Importantly, our study additionally aimed to examine the underlying motivational factors that influence residency choice, with particular focus on how these factors change with time and specialty choice. Compared to matriculation, influence of specialty interest and lifestyle were significantly more important when students made their final residency choice, whereas field prestige, financial incentive, and match confidence were significantly less important. Similar temporal trends existed when results were stratified by residency choice amongst primary care and surgical specialties. As the influence of certain factors differed with time and coincided with an increase and decrease in the proportion of students choosing primary care and surgery, respectively, we wanted to test if factor differences existed between these specialty categories over time, as a frequently proposed theory regarding primary care being a less attractive career choice is due to the salary inequality compared to other specialities [51, 52], as well as the lower perceived prestige [22, 53]. At matriculation in our cohort, no significant differences were detected amongst the factor rankings between students interested in primary care versus surgery; however, in the final year, students choosing surgery ranked prestige and financial incentive significantly higher than primary care. In contrast, final year students interested in primary care rated match confidence and family/location factors higher than students in surgery. These results support another previously proposed theory that lifestyle, hours, and training commitment are a common reason that students may shy away from surgical specialties [53,54,55,56]. Finally, both groups expressed a similarly high importance of interest in their chosen field as well.
Interestingly, we believe that these results provide preliminary evidence that students may exhibit different risk-reward profiles based on the type of residency specialty they choose to pursue. Specifically, students interested in surgery may risk successfully matching into these more competitive residencies for the reward of the salary and perceived prestige that accompany many surgical specialties, whereas students pursuing primary care place greater emphasis on family/location requirements that may also relate to match confidence. Vice versa, students interested in surgery may have more competitive application characteristics, giving them greater confidence and having less concern about matching. While these implications would need to be more closely examined amongst larger student cohorts in order to establish more definitive correlation, the associations observed in our study are not without precedent. It has previously been reported, albeit in separate studies, that students pursuing primary care are more motivated by medical lifestyle/work-life balance [23, 29, 32], ease of residency entry [23], and family status [24]. In contrast, students pursuing surgery or other non-primary care fields were more motivated by economics [23, 24, 30, 31], prestige [22, 24], and having more competitive application characteristics [23, 57]. Our study adds to these previous findings by comprehensively assessing the relative influence of many of these factors, not only on the basis of specialty choice, but also, uniquely, in association with different training stages.
However, while students state having high interest in the fields they pursue and contemplate additional key factors supporting that pursuit, many residents and physicians regret or are unsatisfied with their career choice [1, 27, 28], undermining the health of a long-depleted workforce [14,15,16]. One reason, amongst many, that may explain this is that students may not fully understand the specialties they choose and how they align with their personal/career values. Additionally, the formal, informal, and hidden curricula students are exposed to through their interpersonal, organizational, and cultural interactions in medical school can have significant impact on students’ career perceptions [58, 59]. As our study shows, newly matriculated students interested in primary care versus surgery exhibit no differences in their ranking of motivational factors, but many of these factors significantly deviate between the two career paths in the final year, as we have described. This demonstrates, in part, the impact of the medical curriculum. While exposure to the informal and hidden curricula will vary from student-to-student and school-to-school, making it difficult to exactly measure and control, interventions regarding the formal curriculum have been well-established. Particularly, outside of the typical required clinical clerkships, longitudinal and auxiliary experiences have been shown to foster student interest and impact residency choice [24, 29, 30, 33,34,35]. The long-term effects regarding career choice regret and satisfaction have yet to be explored, but these experiential curricular additions offer an opportunity for medical schools to provide more personalized scholastic exposures that cultivate student interests, which could be performed in conjunction with consideration of student values upon matriculation and throughout major training stages.
Study limitations
This study has important limitations to consider. First, analysis was performed on a single U.S. medical student cohort from the University of Connecticut, a public research university with longitudinal curriculum experiences that provide significant exposure to primary care, making external extrapolation challenging, though multi-institutional studies have shown consistent residency choice outcomes between schools [22, 32]. Second, cohort sizes at this institution are roughly ~ 100 students per year, and when considering factors that can dampen response rate for a voluntary survey (student availability, willingness, survey completion, etc.), our sample size was limited, and particularly low for Years 2 and 3, hindering our ability to confidently assess these stages, which may have allowed us to more specifically identify crucial points in the medical curriculum and propose potential interventions that better accommodate student preferences. This small class size also failed to demonstrate interest (at matriculation or in the Match) in child neurology, combined internal medicine and pediatrics, pathology, and physical medicine and rehabilitation, likely owing to the roughly ≤1% national Match outcomes for these specialties [60]. While the Year 4 survey results correlated well with our cohort’s Match outcomes, our limited response rate also failed to identify the high proportion of students who matched into psychiatry, illustrating potential confounding from non-response bias. Finally, while inspired by previous studies, our questionnaire format and delivery method can be improved upon. The anonymous nature of our survey prevented us from tracking the same students throughout the study, limiting more refined longitudinal analysis and potentially introducing selection bias based on the specific respondents at each timepoint. Methods for anonymity through electronic questionnaire distribution could address this and also expand the cohort scope and sample size in future studies. Additionally, the ordinal scale of our ranking system limits weighted analysis of the motivational factors examined in this study. Allowing respondents to attribute influence weight to these ranked factors, as well as expanding the specificity and range of factors surveyed in the questionnaire, such as assessing students’ perceptions of specialty-specific physician burnout and reasons behind factors such as match confidence, could provide more accurate and nuanced results. Overall, addressing these limitations and expanding this research to include a larger cohort from multiple institutions would help to enhance the internal and external validity of future studies.
Conclusion
In summary, this study examined the longitudinal residency choices and motivational factors for a cohort of U.S. medical students, with the aim of generating insight that could aid the training of the next generation of physicians. We identified how residency choices change between the beginning and end of medical school, how the influence of certain factors change over this period, and stratify our results by specialty choice between primary care and surgery. Our study promotes awareness of student preferences, provides a blueprint for future studies to examine these factors on a larger scale, proposes a new theory based on risk-reward balance regarding residency choice, and may help guide medical school curricula in developing more student-tailored approaches to education and training. Eventually, we hope this work can help play a part in addressing the supply and dissatisfaction issues plaguing the physician workforce, which will ultimately improve healthcare outcomes for patients.
Availability of data and materials
The acquired dataset used and analyzed during the current study are not publicly available due to participant anonymity but are available from the corresponding author on reasonable request.
Abbreviations
- IRB:
-
Institutional Review Board
- UConn SOM:
-
University of Connecticut School of Medicine
- ERAS:
-
Electronic Residency Application Service
- NRMP:
-
National Resident Matching Program
- AAFP:
-
American Academy of Family Physicians
- ACS:
-
American College of Surgeons
- OB/GYN:
-
Obstetrics and gynecology
References
Dyrbye LN, Burke SE, Hardeman RR, Herrin J, Wittlin NM, Yeazel M, et al. Association of Clinical Specialty with Symptoms of burnout and career choice regret among US resident physicians. JAMA. 2018;320(11):1114.
Bodenheimer T. Primary care--will it survive? N Engl J Med. 2006;355(9):861–4.
Chen C, Petterson S, Phillips RL, Mullan F, Bazemore A, O’Donnell SD. Toward graduate medical education (GME) accountability: measuring the outcomes of GME institutions. Acad Med. 2013;88(9):1267–80.
Bucur PA, Bhatnagar V, Diaz SR. A “U-shaped” curve: appreciating how primary care residency intention relates to the cost of board preparation and examination. Cureus. 2019;11(9):e5613.
Grigg M, Arora M, Diwan AD. Australian medical students and their choice of surgery as a career: a review. ANZ J Surg. 2014;84(9):653–5.
Scott IM, Matejcek AN, Gowans MC, Wright BJ, Brenneis FR. Choosing a career in surgery: factors that influence Canadian medical students’ interest in pursuing a surgical career. Can J Surg. 2008;51(5):371–7.
Ellison EC, Pawlik TM, Way DP, Satiani B, Williams TE. Ten-year reassessment of the shortage of general surgeons: increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018;164(4):726–32.
Archer SL. The making of a physician-scientist--the process has a pattern: lessons from the lives of Nobel laureates in medicine and physiology. Eur Heart J. 2007;28(4):510–4.
Salata RA, Geraci MW, Rockey DC, Blanchard M, Brown NJ, Cardinal LJ, et al. U.S. Physician-scientist workforce in the 21st century: recommendations to attract and sustain the pipeline. Acad Med. 2018;93(4):565–73.
Ishikawa M. Distribution and retention trends of physician-scientists in Japan: a longitudinal study. BMC Med Educ. 2019;19(1):394.
Rallis KS, Wozniak AM, Hui S, Nicolaides M, Shah N, Subba B, et al. Inspiring the future generation of oncologists: a UK-wide study of medical students’ views towards oncology. BMC Med Educ. 2021;21(1):82.
Narang A, Sinha SS, Rajagopalan B, Ijioma NN, Jayaram N, Kithcart AP, et al. The supply and demand of the cardiovascular workforce. J Am Coll Cardiol. 2016;68(15):1680–9.
Ross H, Higginson L, Ferguson A, O’Neill B, Kells C, Cox J, et al. Too many patients, too few cardiologists to care? Can J Cardiol. 2006;22(11):901–2.
Brewer JW. Shortage of Physicians. Boston Med Surg J. 1920;182(22):563–8.
Zhang X, Lin D, Pforsich H, Lin VW. Physician workforce in the United States of America: forecasting nationwide shortages. Hum Resour Health. 2020;18(1):8.
AAMC. The complexities of physician supply and demand: projections from 2018 to 2033. Washington, DC: Association of American Medical Colleges; 2020. p. 92. Available from: https://www.aamc.org/media/45976/download.
Shi L. The relationship between primary care and life chances. J Health Care Poor Underserved. 1992;3(2):321–35.
Shi L. Primary care, specialty care, and life chances. Int J Health Serv. 1994;24(3):431–58.
Pilkerton CS, Singh SS, Bias TK, Frisbee SJ. Healthcare resource availability and cardiovascular health in the USA. BMJ Open. 2017;7(12):e016758.
Blake A, Carroll BT. Game theory and strategy in medical training. Med Educ. 2016;50(11):1094–106.
Kaur B, Carberry A, Hogan N, Roberton D, Beilby J. The medical schools outcomes database project: Australian medical student characteristics. BMC Med Educ. 2014;14:180.
Compton MT, Frank E, Elon L, Carrera J. Changes in U.S. medical students’ specialty interests over the course of medical school. J Gen Intern Med. 2008;23(7):1095–100.
Scott I, Gowans MC, Wright B, Brenneis F. Why medical students switch careers. Can Fam Physician. 2007;53(1):94–5.
Bland CJ, Meurer LN, Maldonado G. Determinants of primary care specialty choice: a non-statistical meta-analysis of the literature. Acad Med. 1995;70(7):620–41.
Markert RJ. Why medical students change to and from primary care as career choice. Fam Med. 1991;23(5):347–50.
Fischer JP, Clinite K, Sullivan E, Jenkins TM, Bourne CL, Chou C, et al. Specialty and lifestyle preference changes during medical school. Med Sci Educ. 2019;29(4):995–1001.
Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–71.
Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–13.
Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O’Sullivan PS, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154–64.
Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997-2006. Acad Med. 2010;85(6):947–58.
Clinite KL, Reddy ST, Kazantsev SM, Kogan JR, Durning SJ, Blevins T, et al. Primary care, the ROAD less traveled: what first-year medical students want in a specialty. Acad Med. 2013;88(10):1522–8.
Cleland J, Johnston PW, French FH, Needham G. Associations between medical school and career preferences in year 1 medical students in Scotland. Med Educ. 2012;46(5):473–84.
Ford CD, Patel PG, Sierpina VS, Wolffarth MW, Rowen JL. Longitudinal continuity learning experiences and primary care career interest: outcomes from an innovative medical school curriculum. J Gen Intern Med. 2018;33(10):1817–21.
Stark E, Christensen JD, Schmalz NA, Uijtdehaage S. Evaluation of a curricular addition to assist medical students in specialty selection. J Med Educ Curric Dev. 2018;5:2382120518788867.
Sheu L, Goglin S, Collins S, Cornett P, Clemons S, O’Sullivan PS. How do clinical electives during the clerkship year influence career exploration? A Qualitative Study. Teach Learn Med. 2021:1–11.
Campwala I, Aranda-Michel E, Watson GA, Hamad GG, Losee JE, Kilic A, et al. Impact of a surgical subspecialty roundtable on career perception for Preclerkship medical students. J Surg Res. 2021;259:493–9.
Matthew Hughes JD, Azzi E, Rose GW, Ramnanan CJ, Khamisa K. A survey of senior medical students’ attitudes and awareness toward teaching and participation in a formal clinical teaching elective: a Canadian perspective. Med Educ Online. 2017;22(1):1270022.
Artino AR, Durning SJ, Sklar DP. Guidelines for reporting survey-based research submitted to academic medicine. Acad Med. 2018;93(3):337–40.
Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22(4):195–201.
Coleman VH, Laube DW, Hale RW, Williams SB, Power ML, Schulkin J. Obstetrician-gynecologists and primary care: training during obstetrics-gynecology residency and current practice patterns. Acad Med. 2007;82(6):602–7.
McAlister RP, Andriole DA, Brotherton SE, Jeffe DB. Are entering obstetrics/gynecology residents more similar to the entering primary care or surgery resident workforce? Am J Obstet Gynecol. 2007;197(5):536.e1–6.
Ogburn T, Espey E, Autry A, Leeman L, Bachofer S. Why obstetrics/gynecology, and what if it were not an option? A survey of resident applicants. Am J Obstet Gynecol. 2007;197(5):538.e1–4.
Morgan MA, Anderson BL, Lawrence H, Schulkin J. Well-woman care among obstetrician-gynecologists: opportunity for preconception care. J Matern Fetal Neonatal Med. 2012;25(6):595–9.
Miller J, Ulrich R. The quest for an optimal alpha. PLoS One. 2019;14(1):e0208631 Li Y, editor.
Kim JH, Choi I. Choosing the level of significance: a decision-theoretic approach. Abacus. 2021;57(1):27–71.
Pfarrwaller E, Sommer J, Chung C, Maisonneuve H, Nendaz M, Junod Perron N, et al. Impact of interventions to increase the proportion of medical students choosing a primary care career: a systematic review. J Gen Intern Med. 2015;30(9):1349–58.
Svirko E, Goldacre MJ, Lambert T. Career choices of the United Kingdom medical graduates of 2005, 2008 and 2009: questionnaire surveys. Med Teach. 2013;35(5):365–75.
Peel JK, Schlachta CM, Alkhamesi NA. A systematic review of the factors affecting choice of surgery as a career. Can J Surg. 2018;61(1):58–67.
Brundage SI, Lucci A, Miller CC, Azizzadeh A, Spain DA, Kozar RA. Potential targets to encourage a surgical career. J Am Coll Surg. 2005;200(6):946–53.
Kassebaum DG, Szenas PL. Medical students’ career indecision and specialty rejection: roads not taken. Acad Med. 1995;70(10):937–43.
Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff. 2010;29(5):799–805.
McDonald C, Henderson A, Barlow P, Keith J. Assessing factors for choosing a primary care specialty in medical students; a longitudinal study. Med Educ Online. 2021;26(1):1890901.
Yang Y, Li J, Wu X, Wang J, Li W, Zhu Y, et al. Factors influencing subspecialty choice among medical students: a systematic review and meta-analysis. BMJ Open. 2019;9(3):e022097.
Newton DA, Grayson MS, Thompson LF. The variable influence of lifestyle and income on medical students’ career specialty choices: data from two U.S. medical schools, 1998-2004. Acad Med. 2005;80(9):809–14.
Richardson JD. Workforce and lifestyle issues in general surgery training and practice. Arch Surg. 2002;137(5):515–20.
Pulcrano M, Evans SRT, Sosin M. Quality of life and burnout rates across surgical specialties: a systematic review. JAMA Surg. 2016;151(10):970–8.
Jones MD, Yamashita T, Ross RG, Gong J. Positive predictive value of medical student specialty choices. BMC Med Educ. 2018;18(1):33.
Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med. 1998;73(4):403–7.
Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med. 2013;88(12):1919–26.
National Resident Matching Program. Results and data: 2020 Main residency match. Washington, DC: National Resident Matching Program; 2020. (Charting Outcomes in the Match). Available from: https://www.nrmp.org/main-residency-match-data/ [cited 2021 Apr 8]
Acknowledgements
We would like to thank the UConn School of Medicine students who volunteered to participate in this study, professors Raymond J. Foley, D.O. (UConn) and Jason W. Ryan, M.D., M.P.H. (UConn) for helping the authors coordinate appropriate times to distribute the questionnaires used in this study, and professor James J. Grady, Dr.P.H. (UConn) for consultation regarding statistical analyses. The authors were supported, in part, by fellowship training grants from the American Heart Association (PRE35110005 to F.A.L. and PRE34381021 to A.M.P.) and institutional funds from the UConn Office of Physician-Scientist Career Development.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
F.A.L. and A.M.P.: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, and Writing – review & editing. A.E.P.: Conceptualization, Methodology, Project administration, Supervision, and Writing – review & editing. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Human Subjects Institutional Review Board (IRB) at UConn Health (IRB number 18–062-3) and all participants were consented for the study. All methods were carried out in accordance with the institutional guidelines and regulations. All the participants provided informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ladha, F.A., Pettinato, A.M. & Perrin, A.E. Medical student residency preferences and motivational factors: a longitudinal, single-institution perspective. BMC Med Educ 22, 187 (2022). https://doi.org/10.1186/s12909-022-03244-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03244-7