Abstract
Background
Insurance claims data have been used to inform an understanding of Lyme disease epidemiology and cost of care, however few such studies have incorporated post-treatment symptoms following diagnosis. Using longitudinal data from a private, employer-based health plan in an endemic US state, we compared outpatient care utilization pre- and post-Lyme disease diagnosis. We hypothesized that utilization would be higher in the post-diagnosis period, and that temporal trends would differ by age and gender.
Methods
Members with Lyme disease were required to have both a corresponding ICD-9 code and a fill of an antibiotic indicated for treatment of the infection within 30 days of diagnosis. A 2-year ‘pre- diagnosis’ period and a 2-year ‘post-diagnosis period’ were centered around the diagnosis month. Lyme disease-relevant outpatient care visits were defined as specific primary care, specialty care, or urgent care visits. Descriptive statistics examined visits during these pre- and post-diagnosis periods, and the association between these periods and the number of visits was explored using generalized linear mixed effects models adjusting for age, season of the year, and gender.
Results
The rate of outpatient visits increased 26% from the pre to the post-Lyme disease diagnosis periods among our 317-member sample (rate ratio = 1.26 [1.18, 1.36], p < 0.001). Descriptively, care utilization increases appeared to persist across months in the post-diagnosis period. Women’s care utilization increased by 36% (1.36 [1.24, 1.50], p < 0.001), a significantly higher increase than the 14% increase found among men (1.14 [1.02, 1.27], p = 0.017). This gender difference was mainly driven by adult members. We found a borderline significant 17% increase in visits for children < 18 years, (1.17 [0.99, 1.38], p = 0.068), and a 31% increase for adults ≥ 18 years (1.31 [1.21, 1.42], p < 0.001).
Conclusions
Although modest at the population level, the statistically significant increases in post-Lyme diagnosis outpatient care we observed were persistent and unevenly distributed across demographic and place of service categories. As Lyme disease cases continue to grow, so will the cumulative prevalence of persistent symptoms after treatment. Therefore, it will be important to confirm these findings and understand their significance for care utilization and cost, particularly against the backdrop of other post-acute infectious syndromes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Lyme disease (LD) is a tick-borne infection caused by various genospecies of the bacteria Borrelia burgdorferi sensu lato complex [1]. The Centers for Disease Control and Prevention (CDC) has estimated that 476,000 patients are diagnosed and treated for LD in the US annually, with increasing cases in recent years due to geographic expansion of the tick vector and shifting land use patterns [2, 3]. LD incidence has historically been strongly geographically determined, with cases primarily concentrated in the northeastern, mid-Atlantic, upper Midwestern, and Pacific coast states [4]. Surveillance for LD is conducted through passive reporting in the US and is known to reflect significant underreporting of cases [5, 6]. The use of insurance claims data in LD has limitations of generalizability and specificity, however it has been shown to be useful in informing a broader understanding of LD prevalence and disease trends, particularly in states with high LD incidence [7].
Even in the context of appropriate and timely antibiotic treatment of early LD, a subset of patients develop persistent symptoms such as fatigue, musculoskeletal pain, and cognitive difficulties [8]. When patients subsequently meet criteria for a specific, research-based case definition, these symptoms can additionally be referred to as post-treatment Lyme disease (PTLD). There are no FDA-approved treatment options for these persistent symptoms, which can last for months to years with substantial impacts on health-related quality of life [9,10,11]. Similar to other post-acute infection syndromes, including long COVID, much remains unknown or disputed about illness prevalence, severity, risk factors, and pathophysiology [8, 12]. A recent modeling study estimated the cumulative prevalence of PTLD at 1–2 million people in the US alone [13].
Prior studies have examined care utilization and costs associated with a LD diagnosis [14]. However, the burden of PTLD at the population level has been difficult to quantify, therefore few studies have examined these trends temporally or incorporated the potential additional impact of persistent symptoms in the months or years following diagnosis in their analyses. One such large-scale study of national insurance claims found 87% more outpatient visits and almost $3,000 higher health care costs among patients in the 12-month period following LD diagnosis compared to matched controls, amounting to upwards of $1 billion per year in direct medical costs [15].
In the current retrospective study, we drew upon longitudinal claims data from a large, employer-based health insurance plan in a Lyme-endemic US state to examine trends in outpatient care utilization after treatment of diagnosed LD. We used members’ own pre-LD diagnosis period as comparison. We hypothesized that the number of outpatient visits in members’ post-LD diagnosis period would be higher than their pre-LD diagnosis period, and that temporal trends in increased utilization would differ by members’ age and gender. Specifically, we hypothesized any increases in utilization would be more pronounced for women than for men, and for adults than for children, given previously observed trends in prevalence of persistent symptoms following LD [8, 16,17,18,19,20].
Methods
Study sample
Our initial sample included retrospective person-month level data from members of Johns Hopkins Employer Health Programs (EHP), a private, employer-based program. All residents of Maryland enrolled at any time over a 7-year period (July 2004-June 2011) with a diagnosis code of LD (as described below) were included. For each member, a 48-month (4-year) study window was created around the LD diagnosis month, with months − 24 to -1 representing the ‘pre-LD diagnosis’ period, month 0 representing the month of LD diagnosis, and months 1 to 23 representing the ‘post-LD diagnosis’ period. Members were not required to contribute continuous data at each of these months, therefore each member contributed a varying number of months to the final data set. While we assumed that any missing months would be randomly distributed relative to members’ LD diagnosis month, we also performed a sensitivity analysis only among those with 48 months of continuous membership to ensure that this attribute of the data did not substantively affect our results.
Lyme disease diagnoses
Diagnoses of LD were defined as detailed by the authors in a previous study [21]. Briefly, the first paid medical professional claim with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9), code 088.81 was identified [22]. This diagnosis code encompasses all stages of Lyme disease. Any members with a diagnosis 1 year prior to the study period (July 1, 2003 through June 30, 2004) were excluded from the sample to reduce spillover of previously incident cases. To increase diagnostic specificity in the current study, we also required a fill within 30 days of an antibiotic indicated for treatment of Lyme disease. Doxycycline, tetracycline, cefuroxime, amoxicillin, ampicillin, ceftriaxone, amoxicillin/clavulanate potassium, and azithromycin (if given at least a 14 days’ supply) were considered to be indicated antibiotics.
Variables of interest
LD-relevant outpatient health care visits were defined as any of the following; (a) primary care visits (a provider with one of the following specialties: general practice, family practice, family medicine, pediatrics, internal medicine without other specialties, and nurse practitioner); (b) specialty care visits (a provider with one of the following as their primary practice: infectious diseases, neurology, ophthalmology, otolaryngology, cardiology, rheumatology, orthopedics, physical therapy, or mental health); and (c) urgent care visits (an urgent care or emergency department resulting in either treat-and-release or hospitalization). As a measure of health-care utilization, a monthly sum of these three types of visits was generated as the outcome and used to calculate the rate of outpatient visits per person-month. Lyme disease diagnosis period (pre vs. post diagnosis month) was the primary predictor. Covariates of interest included gender, age, and season. Age was treated in the following ways, depending on the aims of the specific analysis: (a) as a continuous variable for descriptive purposes; (b) categorized into 10-year increments and centered for regression analyses; and (c) dichotomized by members’ age in the last available month for each member (< 18 years vs. ≥ 18 years) to examine differences in children compared to adults (i.e. “adult status”). Similarly, season was treated in the following ways, depending on the aims of the specific analysis: (a) “season of the year” (e.g. spring, summer, fall, winter), and (b) “LD incidence season” based on the monthly distribution of confirmed LD cases reported to the CDC [23]. We considered low Lyme disease season to be December – March, medium Lyme disease season to be April, May, September – November, and high Lyme disease season to be June – August.
Statistical analyses
We first removed any members with an outlying total number of outpatient visits in a given month, as determined by both (a) the maximum, and (b) the magnitude of the difference between the maximum and the second maximum values for each member across all months. This represents members with an unusually high number of visits in only one month, skewing the overall data for that month. Next, descriptive statistics were calculated to summarize members’ characteristics during the month of their LD diagnosis, and to display outpatient visits during the pre and post-LD diagnosis periods.
We then explored the association between the number of all LD-relevant outpatient visits and LD diagnosis period (e.g. pre vs. post) through multivariate analyses adjusting for age, season of the year, and gender, as we hypothesized that these factors may independently affect care utilization. We used generalized linear mixed effects models with a log-link and a negative binomial variance for the monthly visit count. A negative binomial distribution was selected over a Poisson distribution to account for over-dispersion. To account for the correlation of monthly visits contributed by the same member over time, member was included as a random intercept. Based on existing literature, we also hypothesized that there would be gender and adult status effects on the relationship between number of outpatient visits and LD diagnosis period. Therefore, we also studied models that included an interaction term between gender and LD diagnosis period. Due to collinearity between the age and adult status variables, adult status effects could not be studied with interaction models. As a result, this association was explored in models fit on children and adults separately.
All reported p-values are 2-sided. All statistical analyses and graphs were generated using R, version 4.2.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Our initial sample included 113,462 EHP members, 564 of whom had a LD diagnosis, for an average of 80.57 LD diagnoses annually. After accounting for outliers (0.4%) and those without an indicated antibiotic fill (43.4%), a final sample of 317 members were included in the analysis representing 11,704 person-months (Fig. 1).
Members contributed an average of 36.92 (standard deviation 10.69, range 6–48) months of follow-up within the 48-month study time frame. Members contributed an average of 18.18 months (standard deviation 7.10, range 1–23) in the post-LD diagnosis period, and 18.66 months (standard deviation: 7.57, range 1–24) in the pre-LD diagnosis period. The demographic characteristics of this sample, as well as the LD incidence level in the month of their diagnosis, and the place of service of their diagnosis, are shown in Table 1.
In our sample, 59.3% were diagnosed during typical summer months. Although our overall sample had a slightly higher proportion of women (53.3%), a higher proportion of children < 18 years of age (50/75, 66.7%) were boys, consistent with surveillance data in which LD has a higher incidence among young boys compared to girls.
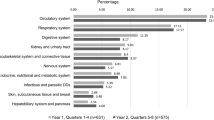
Figure 2 depicts the unadjusted rate of LD-relevant outpatient visits with all months combined within the pre and post-diagnosis periods.
Increases in care utilization during the post-diagnosis period were observed in the sample as a whole (change from pre to post: +0.12 visits per person-month), and among women (+ 0.22), adults (+ 0.14), and those diagnosed during high LD season months (+ 0.20). Increases were also more marked in specialty care (+ 0.09) compared to primary or urgent care. Outpatient care utilization was high in both the pre- and post-diagnosis periods for those diagnosed during low LD season months. When the unadjusted rate of outpatient visits is instead depicted longitudinally at each month rather than collapsed into periods, increases in the number of outpatient visits appear more frequently in the months immediately before and after the LD diagnosis (Fig. 3).
Unadjusted rate of Lyme disease-relevant outpatient visits in the 24 months before LD diagnosis (-24 to -1), the month of Lyme disease diagnosis (0), and the 23 months after Lyme disease diagnosis (1 to 23). Note that for monthly data, rate of outpatient visits per person-month is equivalent to the average number of visits per person per month
However, particularly among women, increases in outpatient visits appear sustained in the post-diagnosis period out to a year and beyond. Figure 4 shows a right-skewed distribution of the difference between the pre-and post-LD diagnosis period, where the median increase in member-level average monthly visits was 0.06 (interquartile range [IQR]: -0.15, 0.31; range: -3.08, 9.70), significantly different from 0 (p = 0.001).
After controlling for gender, age, and season of the year, the rate of LD-relevant outpatient visits increased 26% from the pre to the post-LD diagnosis periods (Table 2, Model 1: rate ratio [RR] = 1.26 [1.18, 1.36], p < 0.001).
Although not statistically significant, there was a trend for women to have a higher rate of visits in the pre-LD diagnosis period compared to men (Model 4: RR = 1.22 [0.95, 1.56], p = 0.118). Furthermore, the rate of visits for women increased significantly more than that of men in the post-LD diagnosis period (Model 4 interaction: ratio of RRs: 1.20 [1.04, 1.38], p = 0.013). Specifically, care utilization by men increased by 14% (Model 4: RR = 1.14 [1.02, 1.27], p = 0.017), whereas care utilization by women increased by 36% (RR = 1.36 [1.24, 1.50], p < 0.001, calculated using Model 4 but with women as the reference group).
This difference by gender was mainly driven by adult members. Among children, boys had higher increases in the number of visits from the pre- to post-LD diagnosis periods than girls, though this difference between boys and girls was not statistically significant (Model 5: boys: 1.27 [1.03, 1.55], p = 0.023; girls: RR = 1.01 [0.77, 1.32], p = 0.937; interaction: ratio of RRs: 0.80 [0.58, 1.10], p = 0.169). By comparison, among adults, this gender difference was significant (Model 6: adult men: 1.13 [0.99, 1.28], p = 0.068; adult women: RR = 1.43 [1.29, 1.58], p < 0.001; interaction: ratio of RRs: 1.27 [1.08, 1.49], p = 0.004). Overall, we found a 17% increase in visits for children, although this was of borderline statistical significance (Model 2: RR = 1.17 [0.99, 1.38], p = 0.068), and a 31% increase for adults (Model 3: RR = 1.31 [1.21, 1.42], p < 0.001) from the pre to the post-LD diagnosis period. However, the difference in the increases between children and adults was not statistically significant (p = 0.234, manually calculated).
We performed a sensitivity analysis including only members who contributed continuous data at every month over the 48-month interval (n = 95) and the results were consistent with the primary analysis (regression results in Supplemental Table 1).
Discussion
We conducted a retrospective, longitudinal pre-post study of claims data from members of a private health insurance plan largely residing in urban or peri-urban regions in Maryland. In the overall sample of 317 members with a LD diagnosis, we found a 26% increase in outpatient health care visits in the 2 years following the month of LD diagnosis compared to the 2 years before, after controlling for gender, age, and season of the year. Among adult members, this increase was significantly higher among women compared to men. Although we did not examine temporal trends in care utilization within the post-LD period statistically, these increases appear to arise in the months immediately prior to diagnosis and persist across months over 2 years beyond the immediate convalescent period. These results are similar to a prior study of national-level insurance claims which found an increase in outpatient visits in the 12 months following treatment for LD compared to matched controls [15]. The reason for the increases we observed in the months immediately prior to diagnosis are unknown, but they may reflect diagnostic uncertainty or misdiagnosis of the initial presentation.
Ultimately, we cannot be certain that the statistically significant outpatient claim increases we observed in the post-LD diagnosis period are due to persistent symptoms and not alternative factors. Nevertheless, we posit this as a reasonable explanation based on several aspects of our analysis. First, our findings remained significant in multivariate analyses controlling for gender, age, and season of the year, factors hypothesized to generally affect care utilization patterns. Second, the extended duration of individual, monthly data points on either side of the LD diagnosis helped to account for expected month-to-month variability and allowed us to generate a pre-morbid baseline of outpatient care patterns for comparison to the post-LD diagnosis period. Despite the fact that members were allowed to contribute a varying number of data points, sensitivity analyses among those with complete, continuous data also found similar trends. Lastly, our study period (2004–2011) occurred well before SARS-COV-2. While other historical events may have temporarily driven an increase in care visits, given our wide study window, the inclusion of members across multiple years, and the anchoring of diagnosis month seasonally throughout the year, we would hypothesize that these would be randomly distributed before and after LD diagnosis in our sample and would not affect comparisons between the pre and post-LD periods in a systematic way.
In the convalescent period following appropriate treatment for LD, approximately 10–20% of patients with early LD will meet criteria for a research case definition for PTLD which incorporates both symptoms and functional impact [25, 26]). Therefore, persistent symptoms will likely have an outsized effect on individual patients compared to what can be identified in the larger population diagnosed and treated for LD. Consequently, while the utilization increases we observed in the overall sample are statistically relevant, we would not expect them to be exceedingly large (approximately 0.12 increase in visits per month overall; 0.22 among women). The distribution of the magnitude of these utilization increases depicted in Fig. 4 shows a right-skewed tail that may be highlighting a subset of members with persistent symptoms.
Although the magnitude of the outpatient care increases we observed are relatively modest, they are likely clinically meaningful, particularly at the larger population level. They appeared most marked within specialty care, which may lead to new diagnostic testing and/or prescriptions thereby incurring greater costs. Furthermore, they appear to persist for longer than the immediate convalescent period, continuing to generate additional costs and reflect morbidity among those who remain ill for years to even decades [9, 27]. With the exception of the study by Adrion et al., [15] estimates of LD cost don’t typically consider the added impact of persistent symptoms. By comparing members to their own pre-LD diagnosis period, our findings further support a significant, population-level increase in utilization post-LD diagnosis which is likely distinct from expected levels of outpatient care utilization in the general population and should be considered in such analyses.
It is generally reported that utilization of health care services varies by sex/gender, [28]. We did note a trend for women to have a higher rate of visits in the baseline pre-LD diagnosis period than men, although it was not statistically significant. Regardless, in our data among adults, women had a significantly higher increase in outpatient visits in the post-LD diagnosis period compared to men. This is consistent with the observation that the risk of developing post-treatment symptoms may be increased among women, particularly in the broader clinical setting where specific research definitions for PTLD are not always applied [17]. Interestingly, we did not find a similar gender interaction among children as we did among adults. This could be due to a range of factors and is also left for future studies to address.
Overall, interpretation of our findings among patients under 18 years of age is less straightforward, but our data suggest a modest increase in outpatient visits among children in the post-LD diagnosis period. The 17% increase in visits we observed among children was of borderline statistical significance, however it was also statistically no different than the increase in visits seen among adults, which was of greater magnitude. Given that our sample size among children was much smaller than adults, it is possible that we lacked statistical power to detect this trend and a larger sample would be needed to properly evaluate differences in children compared to adults. While several previous studies have reported that the rate of persistent symptoms among children is low in appropriately and promptly treated patients, [18,19,20] direct comparison of this rate among adults and children is difficult and to our knowledge has not been reported.
There are several additional limitations to our study. There is inherently lower diagnostic specificity when relying on ICD codes, although we attempted to address this by requiring a relevant antibiotic fill within 30 days of a LD diagnosis. Notably, this criterion excluded over 40% of our initial sample. The relevance of this large subset of patients without a fill within 30 days is unknown. However, it may represent patients with a tentative LD diagnosis which was later ruled out, those given LD codes in error or at a date divorced from their actual diagnosis date, as well as those who experienced treatment delays. We did find that the overall seasonal distribution of excluded cases differed significantly from those included in our final sample (p < 0.001). Those without a relevant antibiotic fill within 30 days had a higher proportion of cases diagnosed in the ‘medium’ and ‘low’ months compared to those in our final sample with a fill, who had more cases diagnosed in the traditional ‘high’ incidence, summer months. This proportion (59%) is similar to reported CDC surveillance data in which 54% of LD cases were diagnosed in these months, lending confidence that our sample with a relevant antibiotic fill within 30 days was more reflective of the overall population of newly incident LD cases [23].
While this may suggest that many of those we excluded were not new diagnoses, it is also possible that some were but their antibiotic treatment was filled elsewhere not captured in our claims data. Similarly, we may have underestimated cases or outpatient care visits resulting from utilization that doesn’t generate ICD data, such as phone calls or complementary/alternative care not covered by insurance. In general, while we attempted to include all types of outpatient visits that, based on our clinical experience, typically encompass evaluation of persistent symptoms following treatment for LD, our definition of ‘LD-relevant’ care was subjectively determined and may have ultimately been over or under-specific, affecting the magnitude of our findings. It would be informative to determine which specific types of specialty care are driving these increases in future studies that are better able to parse out and identify PTLD.
Conclusions
We examined the impact of LD diagnosis on outpatient care utilization in a sample of patients from a Lyme-endemic state and found modest, statistically significant increases at the population level in the post-LD diagnosis period. These increases were most marked among adult women and in specialty care visits. As the number of LD cases, and subsequently the cumulative prevalence of persistent symptoms after treatment continues to increase, it will be crucial to understand both the individual and population-level impact of this condition on quality of life, care utilization, and cost. We hope that future studies will confirm these findings as well as seek to examine and understand their significance in the context of other post-acute infectious syndromes.
Availability of data and materials
The data that support the findings of this study are available from Johns Hopkins HealthCare, LLC but restrictions apply to the availability of these data, which were used under permission for the current study and so are not publicly available. Data are available from the authors upon reasonable request and with permission of Johns Hopkins HealthCare, LLC.
Abbreviations
- LD:
-
Lyme Disease
- CDC:
-
Centers for Disease Control and Prevention
- PTLD:
-
Post-Treatment Lyme Disease
- EHP:
-
Employer Health Programs
- ICD:
-
International Classification of Diseases
- RR:
-
Rate ratio
- IQR:
-
Interquartile range
References
Steere AC, Strle F, Wormser GP, Hu LT, Branda JA, Hovius JW, et al. Lyme borreliosis. Nat Rev Dis Primers. 2016;2:16090. https://doi.org/10.1038/nrdp.2016.90.
Kugeler KJ, Schwartz AM, Delorey MJ, Mead PS, Hinckley AF. Estimating the frequency of lyme disease diagnoses, United States, 2010–2018. Emerg Infect Dis. 2021;27(2):616.
Stone BL, Tourand Y, Brissette CA. Brave new worlds: the expanding universe of Lyme disease. Vector-Borne and Zoonotic Diseases. Mary Ann Liebert Inc. 2017;17(9):619–29.
Centers for Disease Control and Prevention. Lyme Disease Data and Surveillance. Available from: https://www.cdc.gov/lyme/datasurveillance/index.html. [Cited 2022 Sep 26].
Meek JI, Roberts CL, Smith EV Jr, Cartter ML. Underreporting of Lyme disease by Connecticut physicians, 1992. J Public Health Manag Pract. 1996;2(4):61–5.
Coyle BS, Strickland GT, Liang YY, Peña C, McCarter R, Israel E. The public health impact of Lyme disease in Maryland. J Infect Dis. 1996;173(5):1260–2. https://doi.org/10.1093/infdis/173.5.1260.
Schwartz AM, Kugeler KJ, Nelson CA, Marx GE, Hinckley AF. Use of commercial claims data for evaluating trends in Lyme disease diagnoses, United States, 2010–2018. Emerg Infect Dis. 2021;27(2):499–507. https://doi.org/10.3201/eid2702.202728.
Rebman AW, Aucott JN. Post-treatment Lyme disease as a model for persistent symptoms in Lyme disease. Front Med (Lausanne). 2020;7:57.
Rebman A, Bechtold K, Yang T, Mihm E, Soloski M, Novak C et al. The clinical, symptom, and quality-of-life characterization of a well-defined group of patients with posttreatment Lyme disease syndrome. Front Med (Lausanne). 2018/01/10. 2017;4:224.https://doi.org/10.3389/fmed.2017.00224.
Klempner MS, Hu LT, Evans J, Schmid CH, Johnson GM, Trevino RP, Klempner MS, Hu LT, Evans J, Schmid CH, Johnson GM, Trevino RP, Norton DeLona, Levy L, Wall D, McCall J, Kosinski M, Weinstein A. Two controlled trials of antibiotic treatment in patients with persistent symptoms and a history of Lyme disease. N Engl J Med. 2001;345(2):85–92. https://doi.org/10.1056/NEJM200107123450202.
Chandra AM, Keilp JG, Fallon BA. Correlates of perceived health-related quality of life in post-treatment Lyme encephalopathy. Psychosomatics. 2013;54(6):552–9. https://doi.org/10.1016/j.psym.2013.04.003.
Choutka J, Jansari V, Hornig M, Iwasaki A. Unexplained post-acute infection syndromes. Nat Med. 2022;28(5):911–23 (Available from: https://www.nature.com/articles/s41591-022-01810-6 [Cited 2022 Jun 13]).
DeLong A, Hsu M, Kotsoris H. Estimation of cumulative number of post-treatment Lyme disease cases in the US, 2016 and 2020. BMC Public Health. 2019;19(1):352. https://doi.org/10.1186/s12889-019-6681-9.
Mac S, da Silva SR, Sander B. The economic burden of Lyme disease and the cost-effectiveness of Lyme disease interventions: a scoping review. PLoS One. 2019;14(1):e0210280 (Favato G, editor).
Adrion ER, Aucott J, Lemke KW, Weiner JP. Health care costs, utilization and patterns of care following Lyme disease. PLoS ONE. 2015;10(2): e0116767. https://doi.org/10.1371/journal.pone.0116767.
Weitzner E, Visintainer P, Wormser GP. Comparison of males versus females with culture-confirmed early Lyme disease at presentation and at 11–20 years after diagnosis. Diagn Microbiol Infect Dis. 2016;85(4):493–5. https://doi.org/10.1016/j.diagmicrobio.2016.04.012.
Wormser GP, Shapiro ED. Implications of gender in chronic Lyme disease. J Womens Health (Larchmt). 2009;18(6):831–4. https://doi.org/10.1089/jwh.2008.1193.
Gerber MA, Shapiro ED, Burke GS, Parcells VJ, Bell GL. Lyme disease in children in southeastern Connecticut. N Engl J Med. 1996;335(17):1270–4. https://doi.org/10.1056/NEJM199610243351703.
Wang TJ, Sangha O, Phillips CB, Wright EA, Lew RA, Fossel AH, et al. Outcomes of children treated for Lyme disease. J Rheumatol. 1998;25(11):2249–53.
Gerber MA, Zemel LS, Shapiro ED. Lyme arthritis in children: clinical epidemiology and long-term outcomes. Pediatrics. 1998;102(4 I):905–8.
Rebman AW, Wang L, Yang T, Marsteller JA, Murphy SME, Uriyo M, Rebman AW, Wang L, Yang T, Marsteller JA, Murphy SME, Uriyo M, Mihm EA, Weinstein ER, Fagan P, Aucott JN. Incidence of Lyme Disease diagnosis in a maryland medicaid population, 2004–2011. Am J Epidemiol. 2018;187(10):2202–9. https://doi.org/10.1093/aje/kwy133.
Medicode (Firm), editor. Medicode. ICD-9-CM: International classification of diseases, 9th revision, clinical modification. 5th ed. Salt Lake City; 1997. https://www.worldcat.org/title/icd-9-cm-international-classification-of-diseases-9th-revision-clinicalmodification/oclc/33167902.
Centers for Disease Control and Prevention. Lyme disease graphs: confirmed Lyme disease cases by month of disease onset-United States, 2001–2010. Available from: http://www.cdc.gov/lyme/stats/chartstables/casesbymonth.html.
United States Census Bureau. Delineation Files. Available from: https://www.census.gov/programs-surveys/metro-micro/about/delineation-files.html. [Cited 2022 Mar 3].
Wormser GP, McKenna D, Karmen CL, Shaffer KD, Silverman JH, Nowakowski J, Wormser GP, McKenna D, Karmen CL, Shaffer KD, Silverman JH, Nowakowski J, Scavarda C, Shapiro ED, Visintainer P. Prospective evaluation of the frequency and severity of symptoms in Lyme disease patients with erythema migrans compared with matched controls at baseline, 6 months, and 12 months. Clin Infect Dis. 2020;71(12):3118–24. https://doi.org/10.1093/cid/ciz1215.
Aucott JN, Yang T, Yoon I, Powell D, Geller SA, Rebman AW. Risk of post-treatment Lyme disease in patients with ideally-treated early Lyme disease: a prospective cohort study. Int J Infect Dis. 2022;116:230–7. https://doi.org/10.1016/j.ijid.2022.01.033.
Kalish RA, Kaplan RF, Taylor E, Jones-Woodward L, Workman K, Steere AC. Evaluation of study patients with Lyme disease, 10-20-year follow-up. J Infect Dis. 2001;183(3):453–60.
Bertakis K. Gender differences in the utilization of health care services. J Fam Pract. 2000;49(2):147–52.
Acknowledgements
We thank Dr. Sarah Kachur for her provision of medication codes and consultation on medication utilization, and Gitu Mirchadani for her provision of provider-specific codes and consultation on provider specialty classification. We also thank Eric Weinstein and Erica Kozero for their contributions to earlier versions of this analysis.
Dedication
This article is dedicated to the memory and collaborative scholarship of Dr. Peter Fagan.
Funding
This work was supported by a grant from the Steven and Alexandra Cohen Foundation. The funders had no role in the design of the study, the collection, analysis, and interpretation of the data, or the writing and publication of this manuscript.
Author information
Authors and Affiliations
Contributions
AWR, LW, JAM, SMEM, MU, and JNA contributed to the conception of the study design. LW, SMEM, and MU contributed to the acquisition of the data. LW performed initial data process and preliminary analyses. TY performed the primary statistical data analyses. AWR, TY, LW, JAM, SMEM, and JNA contributed to interpretation of the data and data analyses. AWR, TY, LW, JM, SMEM, and JNA drafted and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Johns Hopkins Medicine Institutional Review Board and the Johns Hopkins HealthCare Data Sharing Committee. The need for informed consent was waived by the Johns Hopkins Medicine Institutional Review Board as a retrospective analysis of existing, de-identified data that does not involve direct interaction with human subjects. All research was performed in accordance with relevant guidelines and regulations, including the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
JNA received consulting fees from the Pfizer North America Lyme Disease Vaccine Ad Board, has provided expert testimony in malpractice cases, and has been issued the following patent: Elevated CCL19 after completion of therapy for acute Lyme disease identifies patients at risk for development of post-treatment Lyme disease who will benefit from further antibiotic therapy. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Sensitivity analysis only including members who contributed continuous data at each month over the 48-month study interval. Generalized linear mixed effects regression models with number of all Lyme disease-relevant outpatient visits as the outcome. Models were run among the overall sample [1], as well as among adult [2] and children [3] strata only. Additional models [4, 5, and 6] were run with a gender and Lyme disease diagnosis period (pre vs post) interaction term included.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rebman, A.W., Yang, T., Wang, L. et al. Outpatient visits before and after Lyme disease diagnosis in a Maryland employer-based health plan. BMC Health Serv Res 23, 919 (2023). https://doi.org/10.1186/s12913-023-09909-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09909-3