Abstract
This review seeks to address major gaps and delays between our rapidly evolving body of knowledge on type 2 diabetes and its translation into real-world practice. Through updated and improved best practices informed by recent evidence and described herein, we stand to better attain A1c targets, help preserve beta cell integrity and moderate glycemic variability, minimize treatment-emergent hypoglycemia, circumvent prescribing to “treatment failure,” and prevent long-term complications. The first topic addressed in this review concerns updates in the 2023 and 2024 diabetes treatment guidelines for which further elaboration can help facilitate integration into routine care. The second concerns advances in diabetes research that have not yet found their way into guidelines, though they are endorsed by strong evidence and are ready for real-world use in appropriate patients. The final theme addresses lingering misconceptions about the underpinnings of type 2 diabetes—fundamental fallacies that continue to be asserted in the textbooks and continuing medical education upon which physicians build their approaches. A corrected and up-to-date understanding of the disease state is essential for practitioners to both conceptually and translationally manage initial onset through late-stage type 2 diabetes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Key takeaways
-
Recent new guideline recommendations ready to be routinely incorporated into routine practice include the following:
-
◦ Complication-centric prescribing should take center stage. Treatment plans should no longer ‘silo’ hyperglycemia as a single treatment target but rather manage it synchronously with the patient’s comorbidities and risk factors.
-
◦ In patients with cardiorenal risk factors, long-acting glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose cotransporter-2 inhibitors (SGLT-2is) have been shown to provide protection and are recommended as preferred treatments.
-
◦ A novel algorithm enables treatment decision-making for latent autoimmune diabetes in adults (LADA) based on glutamic acid decarboxylase (GADA) and C-peptide testing [1]
-
-
Several key advances in the management of type 2 diabetes are supported by strong evidence that make these ready for use in routine care, despite remaining in a ‘holding pattern’ before full integration into guidelines. These include:
-
◦ The pleiotropic benefits of several antidiabetic agents provide important new considerations to treatment decision-making; and, should be employed in treatment selection in the clinic.
-
◦ Disease remission should be elevated to a primary objective of case management of type 2 diabetes beyond the role it had in past routine care. The inherent resilience of beta cells can be harnessed to help remit hyperglycemia through the use of diet and lifestyle modifications and/or short-term intensive pharmacotherapy.
-
-
The underpinnings of type 2 diabetes etiology and progression have been corrected. In particular,
-
◦ Early type 2 diabetes is no longer considered an intractable (‘inexorable’) state. Beta cells, in fact, remain robust and resilient through much of the course of the disease, and with support, can resume partial or complete glucoregulation.
-
◦ Type 2 diabetes is not a single disease across all patients, nor does it arise from the same defects. Accordingly, tailored therapy is imperative.
-
◦ Precision medicine veers away from management to treatment failure with sequential add-on therapy. Instead, targeted therapy can address the individual drivers of hyperglycemia in each patient without agents that are ineffective in the given patient.
-
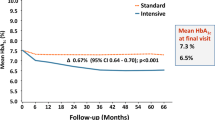
◦ Target attainment is distinctly possible with current treatments, without treatment-emergent hypoglycemia. Intensive glucose control is pivotal for preventing or offsetting diabetes-related long-term outcomes.
-
◦ With the expanding antidiabetes armamentarium, it is possible to reduce reliance on sulfonylureas and exogenous insulin, which present less desirable benefit: risk profiles (including weight gain, hypoglycemia, and ‘wear and tear’ on beta cells) than many other currently available options.
-
Background
Despite the recent expansion of antidiabetic agents such as GLP-1 receptor agonists and SGLT-2is, glycemic control remains suboptimal in many patients. Approximately half of all type 2 diabetic patients in the United States and worldwide fail to achieve the glycemic target of A1c ≥ 7.0% [2,3,4].
Ninety percent of diabetes cases are managed by primary care providers [5]. Guidelines are integral to updating best practices and are especially edifying for general practitioners who maintain a broad knowledge base across numerous medical conditions. Primary care providers are encouraged to apply the most effective treatment parameters in clinical practice rather than relying on specialists [5]. This review seeks to highlight key developments in the field to both provision and empower generalists as well as specialists in dispensing care in line with the latest knowledge in the disease state ready for use in routine care.
The field of type 2 diabetes research has detailed guidelines issued by the American Diabetes Association and the American Association of Clinical Endocrinology [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. Many advances, however, see extensive delays in anatomizing research discoveries into clinical approaches. This prudence helps prevent the need to elaborate extensively on areas pending additional research or to deadopt a faulty recommendation. On the other hand, it impedes the timeliness of advances reaching patients. It also sets a deceptively slow rate of change in best practices, contributing to “physician habituation,” one contributing aspect to clinical inertia [21, 22].
In this review, we shortlisted timely leaps in the management of type 2 diabetes—advances that we believe are ready for “prime time.” We provide context for selected updates that have already been incorporated into guidelines—context that we feel will edify the rationale for readers and speed adoption into real-world use. Second, we detail several important developments that are yet to be translated to the clinic while these remain either in vigorous debate or in limbo despite a strong body of evidence of the benefit and utility of these having benefit to patients.
Third, this review revisits outmoded dogmas about the basic science of type 2 diabetes—premises that continue to be widely reiterated in physician education but are, in fact, incorrect. Today’s type 2 diabetes is “not your mother’s type 2 diabetes,” that is, our modern understanding of dysglycemia is a departure from old tenets. A correct understanding of beta cell function and dysglycemia is needed for physicians to be in command and optimally control diabetes and its sequelae in their clinics.
Manage hyperglycemia synchronously, rather than in parallel, with patient comorbidities and risk factors
Type 2 diabetes, metabolic syndrome, and cardiorenal compromise have been classically viewed as separate diagnostic entities and are managed autonomously. These conditions are highly interrelated, however, and should be regarded as coincident conditions. Moreover, these conditions represent overlapping targets for therapy [18]. For example, renal dysfunction continues to be underdiagnosed in patients with diabetes [23]. Patients with type 2 diabetes and comorbid renal dysfunction are five times more likely to die from cardiovascular causes before reaching kidney failure, highlighting the interrelatedness of the cardiorenal axis with dysglycemia. One study reported a 16-year differential in longevity for individuals with type 2 diabetes with or without renal compromise [24], stressing the importance of screening and managing renal dysfunction alongside hyperglycemia.
In 2023, an international expert task force issued a dictate for physicians: apply early, intensive, and coordinated approaches across interrelated disease states [18]:
“…all too often, the risk factors for these disorders are not addressed promptly in clinical practice, leading to irreversible pathologic progression… Traditional approaches to treatment involving sequential therapy, in which agents are added only after one has failed, contribute to clinical inertia and often prevent goal attainment, leading to adverse outcomes…. in turn contributing to increased morbidity and mortality. In contrast, early diagnosis and prompt, intensive intervention, often with initial combination therapy, leads to faster goal attainment and improved outcomes for at-risk patients.” Handelsman et al. [18].
Early intervention and intensive management of patients with diabetes, cardiorenal, and metabolic diseases) [18].
Accordingly, the first key take-away of this review is to incorporate change from the creation of the treatment plan for the patient: looking beyond hyperglycemia. Large-scale studies in type 2 diabetes patients have proven to be a treasure-trove for insights into the nature and management of the disease. Decades of data have elucidated the full range of hyperglycemia-related conditions and long-term complications. The continuum of related conditions spans obvious conditions, including obesity and metabolic syndrome, prediabetes, type 2 diabetes, hypertension, and dyslipidemia, and includes nonalcoholic fatty liver disease, atherosclerotic cardiovascular disease, atrial fibrillation, chronic kidney disease, heart failure, and cognitive dysfunction [18]. This represents some seemingly disparate conditions under which case management has traditionally siloed or overlooked. In addition to being an outcome of dysglycemia, the presence of one disease state may be a harbinger for, or exacerbate, another. This insight elevates the constellation of comorbid conditions of hyperglycemia from a theoretical construct to a bona fide, practical management tool and objective [18]. This broadened view of dysmetabolism affords valuable opportunities in the clinic for early diagnosis—and therefore prevention—of comorbid conditions. This recommendation made our list because it readily translatable into practice and sanctioned in the guidelines yet relies on practitioners to make a wholesale revision of their approach to care, if not already adopting this approach. The benefit to their patients is improved short- and long-term outcomes.
Cardiorenal benefits of antidiabetic agents: pleiotropic benefits
In addition to the classic long-term outcomes (cardiovascular disease, peripheral artery disease, nephropathy, retinopathy, and neuropathy), incontrovertible evidence connects hyperglycemia to stroke, cognitive decline, gastrointestinal problems, immunocompromise, cancer, and even dental disease. This awareness expands our appreciation for the broad physiologic consequences of dysglycemia.
Another dividend of large studies in patients with type 2 diabetes has been that many of our current glucose-lowering agents possess valuable pleiotropic actions. For example, the PROactive Study showed that pioglitazone improves triglycerides, albuminuria, markers of inflammation, and fatty liver and reduces the risk of stroke and myocardial infarction—each through mechanisms that appear to be distinct from its direct insulin-sensitizing action [25,26,27,28]. Icosapent ethyl similarly conferred cardiovascular benefits independent of its direct lipid-lowering effects [29, 30]. Finerenone was shown to pleiotropically influence tissue remodeling through alternative mechanisms to those of the mineralocorticoid receptor [31,32,33].
GLP-1 receptor agonists and SGLT-2is were found to exert striking benefits on the heart, liver, kidney, and even the brain [34,35,36,37,38,39,40]. Emerging research indicates that these benefits are conferred by pleiotropic mechanisms, that is, pathways distinct from those involved in glucose balance. For example, GLP-1 receptor agonists were found to improve myocardial blood flow in a manner independent of myocardial glucose uptake [41]. Interestingly, receptors for GLP-1 have been found in numerous tissues beyond the endocrine pancreas and gastrointestinal tract, including the brain, immune system, heart, and peripheral cardiovascular vasculature.
GLP-1 receptor agonists confer protection to the kidney. To characterize the mechanisms through which GLP-1 receptor agonists protect against diabetic kidney disease, the phase 3B FLOW Trial will assess the effects of semaglutide treatment on kidney outcomes in participants with type 2 diabetes and chronic kidney disease (NCT03819153), and this trial is expected to be completed at the end of 2024. Planned meta-analyses [42] and other studies are also underway. Studies investigating the protective effects of GLP-1 receptor agonists on cognitive dysfunction [43, 44], nonalcoholic fatty liver disease (NAFLD)/nonalcoholic steatohepatitis (NASH), and metabolic dysfunction-associated fatty liver disease (MAFLD) are ongoing [45].
As an antidiabetic agent, SGLT-2 inhibitors improve plasma glucose levels by increasing renal glucose and sodium excretion and lowering intraglomerular pressure [46,47,48]. SGLT-2 inhibitors exert a wide range of pleiotropic actions, some of which may prove as important future targets of therapy. SGLT-2 inhibitors reduce glycolysis, rebalance the coupling between glycolysis and oxidative phosphorylation, and attenuate adverse cardiac remodeling and the progression of heart failure. SGLT-2 inhibitors have been found to impact cardiomyocyte function through the adenosine monophosphate-activated protein kinase mammalian target of rapamycin complex 1 pathway [49].
SGLT-2 inhibitors also exert interesting effects on mitochondrial and cell viability. These agents directly modulate evolutionary responses to nutrient deprivation through adaptive cellular reprogramming and cell survival (reviewed by Packer, 2023) [49]. Starvation mimicry has been used to show that SGLT-2 inhibitor modulation of mitochondrial function and viability involves processes of autophagy, the clearing of reactive oxygen species, and the reduction of inflammation and fibrosis, each of which is a pathway distinct from the renal clearance of glucose [49].
GLP-1 receptor agonists and SGLT-2 inhibitors have been shown in clinical trials to benefit the cardiorenal axis [35, 36, 38,39,40,41,42]. This finding raises the following question: how much earlier in the disease course of dysglycemia and dysmetabolism might these drugs confer protection for the cardiorenal axis? Should these agents be used as first-line treatment in potentially all patients with type 2 diabetes? The observation that the protective effects are accomplished independent of glucose-lowering potential opens new possibilities: might these agents have utility in cardiorenal protection in normoglycemic patients? Tantalizing prospects await future research.
For the meantime, findings from long-term outcome studies have reshaped treatment sequencing in the guidelines. The 2023 directive authored by Handelsman et al. [18] mandates factoring a patient’s comorbidities and risk factors, including those of the cardiorenal axis, along with their hyperglycemia in treatment decision-making. As recommended in the guidelines, these authors reemphasize use of long-acting GLP-1 receptor agonists and SGLT-2 inhibitors in patients with type 2 diabetes and existing (or at risk for) comorbid cardiovascular or renal compromise. Based on the available evidence, there should be no delay in incorporating these recommendations into clinical practice for eligible patients.
Amend the canonical teaching of the “inexorable progression of type 2 diabetes”
Medical textbooks have always taught—and clinical practice correspondingly operates on the supposition—that type 2 diabetes can only “inexorably progress.” The belief is that once a patient with diabetes requires pharmacointervention, the disease is intractable. This long-entrenched dogma is omnipresent across medical school textbooks and continuing medical education and shapes practitioner expectations. However, it has been flatly refuted by decades of research.
Let us consider this supposition from a historical context. This arose in the early era of diabetes care, when diagnosis typically occurred late in the course of the disease. Indeed, at this point, beta cells had already largely “petered out” in their capacity to sense fluctuations in plasma glucose and correspondingly adjust plasma insulin levels. That is, type 2 diabetes was observed and tested in its advanced stages. Indeed, before annual screening, beta cells retain as little as 10% of their capacity at the time of diagnosis. The first-generation therapeutic options of that era were “oafish” drugs such as sulfonylureas, which rapidly reached treatment failure [50], arguably by further taxing overextended beta cells.
In today’s standards of care, however, hyperglycemia is detected sooner—as early as the prediabetic state. In current standards of care, beta cells often remain robust at the time of diagnosis. The inherent resilience of the beta cells and of the glucoregulatory apparatus, at large, are still available to be re-enlisted to resume normoglycemia.
It is worthwhile at this point to review defects that contribute to type 2 diabetes. These defects include beta cell dysfunction [51, 52], insulin resistance [53], and, less regarded but equally important, hyperinsulinemia [54,55,56]. In addition, genetic and epigenetic variables [57, 58] and environmental factors [59,60,61] each play a causative role. Hyperglycemia typically arises not from one but from multiple insults across these interrelated factors. Correcting any of these three variables typically has a domino effect on the others [62]. Peripheral insulin resistance is tethered to elevated insulin secretion [63, 64], with each impacting glucose tolerance [65]. The state of beta cell function is intricately linked to the magnitude and implacability of the resulting systemic insulin resistance.
Chronic nutrient excess has accompanied modern affluence. This overnutrition is out of sync with the evolutionary schema of metabolism. Overnutrition induces a maladaptive state of sustained hyperinsulinemia in some individuals. This taxes the beta cells and instigates insulin resistance—perpetuating all three imbalances. Beta cell dysfunction bidirectionally influences the extent of hyperinsulinemia and is quantitatively linked to the development of diabetes-related complications (reviewed by Rachfal et al [66]) [67].
Diet and exercise modifications promote weight loss and simultaneously improve insulin resistance, correct hyperinsulinemia, and increase beta cell functional capacity. Diet and exercise modifications have been shown repeatedly to be sufficient to reestablish normoglycemia in a subset of patients [67,68,69,70,71,72,73]. The ACT-NOW and STOP-Diabetes trials showed that correcting impaired insulin secretion and insulin resistance in normoglycemic people at high risk of diabetes (impaired glucose tolerance or prediabetes in these two studies, respectively) reduced progression to frank diabetes [74, 75].
The body of knowledge to date categorically overrides the premise that type 2 diabetes is an “inexorable” disease. Type 2 diabetes can possibly be rehabilitated, perhaps up to the advanced stages of the disease.
In routine practice, physicians restore normoglycemia in many patients through good adherence to diet and lifestyle modifications, especially in patients with early type 2 diabetes. The premise that type 2 diabetes is an “inexorable” disease traditionally assumed that once pharmacotherapy is initiated, there is no further rationale to treat the tractability of hyperglycemia.
The conceptual leap that we make herein is that early type 2 diabetes is not a one-way proposition. This restyles the slope of the natural history of the disease to a far more favorable trajectory for our patients and with ample opportunities to slow or stall type 2 diabetes—from prediabetes through early-onset disease, and even beyond, as will be detailed.
Resilience of the glucoregulatory apparatus: early vs late diabetes
Early- and late-stage type 2 diabetes can now be reframed as two distinct conditions based on the extent of beta cell function and warrant two distinct approaches to care. Until the advanced stages of hyperglycemia, the first mandate is to attempt to resume euglycemia if the beta cells can support adequate insulin production and metabolic gluco-stasis.
Consider the recent SARS-CoV-2 pandemic. Pandemic stay-at-home orders resulted in a record number of patients presenting with new-onset hyperglycemia, individuals who had been normoglycemic prior to the pandemic [76]. It is reasonable to assume that these individuals retain high-functioning, robust beta cells, regardless of their age. Diet modification and/or exercise can reestablish normoglycemia by easing the imposition of recently introduced insulin resistance and its sequelae on the glucoregulatory apparatus.
As a second example, treatment with antidepressants can lead to new-onset hyperglycemia via drug-induced changes in metabolic rate [77]. As in the above example, hyperglycemia is not associated with “petered out” beta cells; this patient population constitutes excellent candidates for reversing type 2 diabetes through diet and exercise. Gestational diabetes and glucocorticoid-induced diabetes are other instances of transient hyperglycemia, from which it can be anticipated that the glucoregulatory apparatus retains the ability to “right” itself.
In contrast, late-stage diabetes may correspond more closely to the “classical” construct of type 2 diabetes onset, which is represented by “exhausted” beta cells. Typically, beta cells in late-stage type 2 diabetes have been subjected to glucotoxicity and lipotoxicity for decades, which has detrimental effects on cell function, overall cell integrity, and cell viability [47, 51, 52].
Although more common in older patients, beta cell resilience is much more related to the status of the glucoregulatory apparatus than to patient age. Persisting dysglycemia, sustained hyperinsulinemia, unmitigated insulin resistance, and systemic glucotoxicity are highly detrimental to beta cells, damaging the cells and leading to loss of glucoregulation. Notably, glucolipotoxicity is detrimental to almost all other cell types. This damage results in a wide range of long-term complications associated with hyperglycemia and diabetes [47, 51, 52, 56]. As described above, the actual range of organ systems compromised by sustained hyperglycemia is more numerous than that deduced decades ago from the United Kingdom Prospective Diabetes Study (UKPDS) and other early investigations [50, 78].
The remission of type 2 diabetes in the clinic is one of the hottest contemporary topics and sits in the crosshairs of recent developments. On the one hand, the ability to remit hyperglycemia is within reach, in contrast to decades of teaching that type 2 diabetes is “inexorable.” Despite being routinely practiced in the first-line intervention of hyperglycemia through diet and exercise, it is typically abandoned after this initial, sometimes cursory effort.
On the other hand, accumulating evidence that GLP-1 receptor agonists and SGLT-2is confer cardiorenal protection has given pause to promote remission. According to the most recent consensus statement, guideline crafters have left remission in limbo, citing the need for large studies to first elucidate which patient types are the best candidates for cardiorenal prevention versus targeting remission of the disease. If hyperglycemia is remitted, a window of opportunity for the prevention of long-term complications may be lost.
The authors of the current review, however, urge physicians to prioritize and implement remission as a priority goal of therapy in advance of the years of studies needed to satisfy the above concerns of guideline crafters. Treating patients to remission benefits virtually all patients. Correcting hyperglycemia affords, in itself, protection against diabetes-related long-term complications. Practical clinical approaches to accomplish remission are described in this review.
New treatment algorithm for latent autoimmune diabetes in adults (LADA)
LADA presents a unique scenario within the diabetic state. LADA is a variant of diabetes accounting for 2–12% of all patients with adult-onset diabetes. Like type 1 diabetes, LADA is characterized by immunogenetic markers of beta cell destruction (albeit with slower destruction than is characteristic of type 1 diabetes). Akin to type 2 diabetes, on the other hand, LADA does not require the use of exogenous insulin, at least in its earlier stages [1, 79]. The clinical profile of LADA has long presented a quagmire for practitioners.
LADA makes our shortlist for this review article because of the introduction of a novel treatment algorithm—one that may reconcile the seemingly opposing features of LADA in determining treatment of choice (Fig. 1). This algorithm by an international expert panel, published in 2020, supersedes, in our opinion, the guidance provided by the American Diabetes Association (ADA)/European Association for the. Study of Diabetes (EASD). It can also be used to initially and subsequently distinguish the clinical presentation of LADA from that of type 2 diabetes.
Qualitative illustration of the spectrum of factors associated with different forms of DM, including the variable age at onset, lack of obesity, metabolic syndrome, genetic associations, different forms of immune changes, C-peptide secretion, and the need for insulin therapy. T1DM, type 1 DM; T2DM, type 2 diabetes. Adapted from Schwartz et al. “The Time Is Right for a New Classification System for Diabetes: Rationale and Implications of the Beta-Cell–Centric Classification Schema.” Diabetes Care 2016;39:179–186 [51]. Reuse permission granted
The Buzzetti et al. algorithm employs a two-step decision tree. Autoantibodies that target glutamic acid decarboxylase (GAD) are among the autoantibodies displayed in patients with type 1 diabetes; these autoantibodies serve as immune markers with high sensitivity. Approximately 75% of people with type 1 diabetes at diagnosis exhibit GAD autoantibodies. LADA is part of the autoimmune diabetes spectrum, and glutamic acid decarboxylase (GADA) testing serves as the first step in the algorithm.
For patients who test positive for GADA, the treatment of choice is determined by the concentration of C-peptide. C-peptide is used as a proxy for extent of beta cell function, which can vary greatly between patients with LADA. Low C-peptide (< 0.3 mmol/L) levels call for treatment with multiple-insulin regimen recommended (as for type 1 diabetes). Elevated C-peptide of > 0.7 nmol/L suggests a modified ADA/EASD algorithm, similar to type 2 diabetes but allows for the potentially progressive nature of LADA by monitoring C-peptide to adjust treatment. There should be additional C-peptide measurements if there is a deterioration of glucose control; some of these patients will have false-positive autoantibodies and therefore will have true type 2 diabetes.
The interim values for C-peptide, ≥ 0.3 and ≤ 0.7 nmol/L, should be treated with combination regimens; insulin in combination with other therapies should be considered to modulate beta-cell failure and limit diabetic complications. Consistent with practice guidelines, the presence of comorbidities is an additional factor to be weighed in treatment of choice (see [1]).
The expert panel also advised that general screening be conducted among all patients who were newly diagnosed with non-insulin-requiring diabetes to identify patients who met the criteria for LADA.
Hyperglycemia is not a single entity but rather the composite of multiple, varying drivers of dysglycemia
The glucoregulatory apparatus is a complex system of gluco-sensing instruments, hormones, physiologic gates, storage depots, feedback loops, and switchbacks. This multiorgan, multisystem regulation is as modifiable as it is fine-tuned.
In the updated, reimagined understanding of type 2 diabetes described herein—and based on state-of-the-art science—hyperglycemia is not a single entity, as it is usually regarded. Rather, it exists as an aggregate of drivers that contribute to the ensuing hyperglycemia. This is not a novel concept, as it was elucidated by these authors (RAD) in 2008 as the widely cited Ominous Octet. This roster was expanded in 2016 by these authors (SSS, MEH) to the Egregious Eleven, below [51] (Fig. 2). Identifying the specific drivers of hyperglycemia in a given patient constitutes a shift to individualized care and practically informs treatment of choice.
The Beta-Cell–Centric Model: The Egregious Eleven. Dysfunction of the beta cells is the final common denominator in DM. Eleven currently known mediating pathways of hyperglycemia are shown. Many of these contribute to beta cell dysfunction (liver, muscle, adipose tissue [shown in maroon to depict additional association with IR], brain, colon/biome, and immune dysregulation/inflammation [all shown in blue]), and others result from beta cell dysfunction through downstream effects (reduced insulin, hyperinsulinemia, decreased incretin effect, a-cell defect, stomach/small intestine via reduced amylin, and kidney [shown in green]). Adapted from Schwartz et al. “The Time Is Right for a New Classification System for Diabetes: Rationale and Implications of the Beta-Cell–Centric Classification Schema.” Diabetes Care 2016;39:179–186 [51]. Reuse permission granted
This differs from the current standard of care, which treats hyperglycemia as a single target, for which the treatment of choice is based on the quantitative (plasma glucose levels) rather than the qualitative (individual drivers) nature of the patient’s hyperglycemia.
The crux of our next take-away point is that hyperglycemia is the collective result of numerous physiologic levers that elevate plasma glucose. These factors contributing to hyperglycemia vary from individual to individual and may change in number (most likely, increase in number) as the disease progresses. Each driver of hyperglycemia presents the opportunity to apply targeted therapy.
In the revised paradigm described herein, the least number of agents are used to target the greatest number of pathways mediating hyperglycemia [51]. In current standards of care, treatment failure prompts one of several approaches to glucose-lowering therapy. The first option, if the combined regimen does not bring plasma glucose to target levels, is to abandon an agent within the regimen. That agent may, in actuality, target one of the drivers present in the patient. For example, drug switching from pioglitazone would leave insulin resistance unaddressed. As mentioned, insulin resistance is an almost ubiquitous driver of hyperglycemia in type 2 diabetes patients.
Another common adjustment is add-on therapy to the existing regimen. This is often done without regard to the mode of action(s) that align with one of the drivers of hyperglycemia in a given patient. Ineffective therapy is costly in terms of drug acquisition cost as well as the potential “physiologic costs” of unneeded polypharmacy.
As described, current standards of care do not prioritize treatment(s) of choice with the specific drivers giving rise to hyperglycemia in the given patient. In contrast, the stratification of first-, second-, and third-line treatment sequences establishes undue competition between classes, which should more rightly be viewed as complementary options rather than salvage therapy after managing patients to treatment failure [51, 80, 81].
Among the eleven pathways that mediate hyperglycemia and are currently known (the Egregious Eleven) [51], therapies are available that target each driver (Fig. 3). Trial-and-error may be required to determine some of the drivers; this effort is worthwhile. The recent commercialization of tirzepatide provides a new target: glucose-dependent insulinotropic polypeptide (GIP) [82]. By modulating GIP and GLP-1, tirzepatide stimulates the release of insulin and improves insulin sensitivity. It decreases the amount of glucose generated by the liver, slows digestion, and contributes to weight loss [83].
The use of the Egregious Eleven as a guide for patient-centric therapy. Targeted therapies for each of the current mediating pathways of hyperglycemia, weight reduction and CV benefits based on The Beta-Cell–Centric Model. GLP-1, glucagon-like peptide 1; QR, quick release. † - Weight reducing agent. * - Potential CV benefit shown for at least one member of the class. Adapted from Schwartz et al. “The Time Is Right for a New Classification System for Diabetes: Rationale and Implications of the Beta-Cell–Centric Classification Schema.” Diabetes Care 2016;39:179–186 [51]. Reuse permission granted
In the approach advocated herein, untargeted, sequential add-on therapy is replaced by treatments tailored to the drivers of hyperglycemia in that patient. This achieves “precision medicine,” the pinnacle of medical care. This approach helps circumvent managing patients to treatment failure, which can reduce the number of drugs prescribed for patients and help lower the risk of hypoglycemia [84]. Hypoglycemia can also be avoided by opting for targeted therapies in lieu of insulin or sulfonylureas. These agents are major culprits of hypoglycemia and contribute to weight gain, among other concerns. Successful management of the specific drivers of hyperglycemia may forestall the use of insulin therapy. Exogenous insulin is associated with poorer cardiovascular outcomes. These authors (SSS, MEH) have reviewed a body of literature suggesting that cardiovascular risk is associated with long-term use of exogenous insulin rather than being a consequence of the advanced stage of the disease, as is presumed (reviewed in Schwartz et al. Postgrad Med 2016; Herman et al. 2017) [85, 86]. There will always be a place for insulin therapy, although a reduced reliance on exogenous insulin is a goal due to its relatively unfavorable benefit–risk profile.
We regard sulfonylureas, though they are used liberally, as dark horses. Sulfonylureas are associated with increased risk of hypoglycemia, weight gain, cardiovascular events, and mortality [87, 88]. Importantly, treatment failure ensues quickly with sulfonylureas, as observed in clinical practice and in the recently published large-scale GRADE Study [89]. This has led to a vast speculation that sulfonylureas may place an undue burden on beta cells, pushing these cells toward exhaustion. This supposition is controvertible but supported by preclinical research showing that sulfonylureas promote beta cell death/apoptosis [90, 91]. It is the opinion of these authors that high levels of sulfonylurea-induced insulin secretion in already overworked beta cells should be eschewed, especially given the array of currently available “gentler,” more “beta cell-friendly” options.
Is there a “reset” button for early type 2 diabetes?
The most striking demonstrations of diabetes remission arose from bariatric surgery studies [92,93,94,95,96,97,98,99]. With Roux-en-Y gastric bypass, in particular, remission of hyperglycemia has been so successful that these procedures have been renamed “metabolic surgery.” The wide-ranging physiological benefits of metabolic surgery include improvements in insulin sensitivity, beta cell function, and incretin responses; changes in bile acid composition and flow; alterations in the gut microbiota; shifts in intestinal glucose metabolism; and increased adipose metabolic activity (reviewed in Xu 2021 [100]). The remission of diabetes through metabolic surgery has been more successful in patients with early-stage type 2 diabetes than in those with late-stage type 2 diabetes. This is presumably due to the retained robustness of the beta cells and the responsiveness of the glucoregulatory apparatus to “right” the various defects that give rise to dysglycemia. In addition to remitting frank type 2 diabetes, metabolic surgery has been shown to reduce the onset of diabetes in normoglycemic obese individuals.
As mentioned earlier, diet and lifestyle modifications early in diabetes have proven adequate to shift hyperglycemia back to normoglycemia. This was also reproducibly demonstrated in seminal studies, including those by Look Ahead [68, 69, 101], DIADEM-I [70], DiRECT [71, 72], and U-TURN [67]. A meta-analysis by Goldenberg and coworkers [2021] of 1357 participants across 23 trials concluded that a low-carbohydrate diet for 6 months may be adequate to remit diabetes without adverse consequences.
Importantly, remission can also be achieved in clinical practice by the use of short-term, intensive pharmacotherapy regimens (alternating approaches to either diet or surgery). As published by these authors (RAD), the EDICT study showed that a regimen of metformin, pioglitazone and exenatide achieved glycemic control, improved insulin sensitivity (threefold), and increased beta cell function (30-fold) in recently diagnosed patients with type 2 diabetes [102,103,104]. In contrast, the EDICT study revealed that “conventional therapy” (metformin followed by add-on therapy with sulfonylurea and glargine insulin), while also achieving glycemic control in the EDICT study, did not simultaneously aid insulin sensitivity or substantially improve beta cell function. This finding supports the notion that intentional combination regimens reset the glucoregulatory apparatus by correcting each of the core defects of type 2 diabetes. In combination, metformin, pioglitazone, and exenatide address the core defects of insulin resistance, beta cell dysfunction, hyperinsulinemia, and hyperglucagonemia.
These authors (BC) have also explored hyperinsulinemia as a primary defect in type 2 diabetes [105] (Fig. 4). According to the results from Roux-en-Y gastric bypass, the restoration of normoglycemia was accompanied by the normalization of hyperinsulinemia [105, 106]. Interestingly, corrections in insulin output were achieved without changes in insulin resistance.
Potential mechanisms for hyperinsulinemia as a major defect in metabolic disease. Chronic hyperinsulinemia of any potential etiology is associated with chronic hyperglucagonemia, which may lead to increased hepatic glucose output. Nutrient excess and hyperlipidemia contribute to adipose tissue expansion and dysfunction with eventual ectopic lipid deposition, which is associated with reduced muscle glucose disposal. Reprinted from Thomas et al. 2019 [105]. Reuse permission granted
Some studies have demonstrated the ability to reset the glucoregulatory apparatus in advanced-stage type 2 diabetes patients. The Qatar Study evaluated poorly controlled patients with an A1c of 10% and a duration of disease of 10 years or more. Combination therapy with pioglitazone and exenatide achieved an A1c target of 7.0% in 86% of these subjects, compared to only 44% in a comparative group treated with insulin therapy (P < 0.0001) [107]. Again, the use of agents targeting the core defects of diabetes is key. Compared with treatment with exogenous insulin, treatment with pioglitazone/exenatide was found to bolster beta-cell function, with 2.5-fold greater insulin secretion.
Specifically, diet modification, metabolic surgery, and pharmacotherapy studies have each demonstrated “reset” the body’s glucose machinery. This remission is typically accompanied by improvements in beta cell functional capacity [108,109,110,111,112], reversing the origin of hyperglycemia. These authors [SSS, MEH] consider the beta cell as the final common denominator of hyperglycemia [52, 66].
We shortlisted type 2 diabetes remission in this review article, as it represents a highly controversial yet timely area. The medical community has waffled for nearly a decade on the vernacular for this reversal of fortune. In 2023, a consensus was reached to use the terminology “remission” (not “cure” or “reversal”) to best suit this outcome. An expert panel defined remission as a “return of HbA1c to < 6.5% (< 48 mmol/mol) that occurs spontaneously or following an intervention and that persists for at least 3 months in the absence of usual glucose-lowering pharmacotherapy” [113]. Proceeding from that point, the questions become more provocative. Can we truly characterize the return to normoglycemia as full “remission” when unalterable defects, such as genetic factors, may not be remittable? Can remission of hyperglycemia be considered a categorical “win” for patients after glucolipotoxicity has caused permanent organ damage?
According to the consensus report by Riddle and colleagues [113], those authors feel that open questions call for more research to determine who are candidate patients for remission. Critically, however, they stipulate that their consensus statement “is not intended to provide guidance regarding how or when glycemic control qualifying as a remission should be sought. It also does not aim to clarify the role of preventive pharmacotherapy after a remission is identified.” [113].
These authors express concern, however, that the Riddle et al. consensus report inadvertently thwarted open discussions, appreciation, and adoption of remission in clinical practice. The literature on the issue of remission has fallen rather quiet from the time of its publication in October 2021 to the time of writing of this review in 2024.
These authors believe that the wealth of evidence demonstrates that the glucoregulatory apparatus can reset itself in many patients. These authors (SSS; RAD) have successfully and routinely reverted frank type 2 diabetes in their respective private practices in patients presenting with low as well as high A1c values. Readers can find detailed strategies to accomplish this from the clinics of two of these authors in Miller et al. 2019 [114] and in Lavynenko et al. 2022 [104].
Accordingly, the first goal of management in routine practice is to reestablish normoglycemia. Remission should have a prominent place in patient treatment plans. It should be approached with diet and lifestyle modifications, with which all physicians have seen success, and, if needed, through the use of established protocols for short-term, intensive pharmacotherapy.
Continuous glucose monitoring in type 2 diabetes: current status on this very “open” question
The adoption of continuous glucose monitoring (CGM) devices has been slow. This is despite American Diabetes Association recommendations for use in individuals with diabetes using multiple daily injections, continuous subcutaneous insulin infusion, and other forms of insulin therapy [115]. CGM is also recommended for individuals whose glucose levels are not at goal, who have frequent hypoglycemia and/or hypoglycemia unawareness, who are taking other medications that cause low blood glucose, who have kidney disease, or who have varying and/or intensive physical activity patterns. The American Association of Clinical Endocrinology Clinical Practice (AACE) guidelines have recommended the use of CGM in all patients with diabetes since 2021 [116].
CGM is a valuable tool for the diagnosis or treatment of hyperglycemia [117,118,119,120]. The benefits of CGM should be fully appreciated, especially in cases where hyperglycemia management is suboptimal. CGM can detect recurrent hypoglycemic episodes, including nocturnal or “silent” hypoglycemia, and can reveal glycemic variability, which in itself is now understood to be problematic. CGM can detect severe fluctuations on an hourly basis, which cannot be captured using A1c measurements.
CGM can also inform and influence lifestyle decisions. Even when used as a short-term tool, CGM can identify remediable causes of highly refractory hyperglycemia, such as the timing or content of the patient’s diet, exercise regimens, sleep patterns, or travel [116]. With awareness of the effects on plasma glucose, patients can adjust their daily schedules to minimize fluctuations.
The slow uptake of CGM is partly due to cost considerations, although private health insurance plans are increasingly covering CGM. Medicare covers CGM through its durable medical equipment for patients receiving exogenous insulin (fortunately, Medicare has removed the onerous prior requirement of extensive blood glucose log data). Dexcom and Abbott have each marketed an over-the-counter CGM device.
Conclusions
Up to 40% of refractory dysglycemia cases may, in fact, be beyond the reach of our approaches and interventions [60, 61, 121], including patient adherence. Environmental exposure, genetics, and the gut microbiota are three such examples. Environmental exposure occurs at all life stages, beginning with gestation, during which glucose regulation is programmed by maternal metabolic status [122]. This has been found to influence glucoregulation not only in offspring but also in the next generation. Genetics and epigenetics are important contributors to hyperglycemia and remain largely beyond our interventions [51, 61, 66, 123, 124]. The role of the gut microbiota in type 2 diabetes is well documented and an area of intense current research [51, 60, 125]. This relationship is bidirectional, highly complex, and still unresolved.
This still leaves a great deal that we can impact therapeutically. To achieve this optimally, an excavation of past dogmas—belief systems that are out of sync with modern understanding of the defects, progression, and revertability of type 2 diabetes—is necessary. Management of hyperglycemia should be more directed by the resilience of beta cells than by A1c elevation. Gluco-homeostasis may be restored in many patients by simply “resetting” insulin resistance, thereby easing the burden on beta cells. Diet and lifestyle may prove adequate to accomplish this; short-term, intensive pharmacotherapy, as described herein, is a powerful approach to revert hyperglycemia.
When long-term pharmacotherapy is used, precision medicine should be practiced. The specific drivers of hyperglycemia at work in a given patient govern the choice of treatment(s). This represents a departure from treating all type 2 diabetes as a single, uniform condition from the laundry list of available agents. Targeted therapy limits the retention of ineffective therapies, which reduces adverse events, the physiologic burden of polypharmacy, and excess drug costs.
The UKPDS and other early seminal trials placed an emphasis on tight glucose control in real-world practice. This inadvertence created a conundrum for physicians to achieve target A1c levels without teetering towards hypoglycemic episodes. It ultimately dissuaded achieving glucose targets. Hypoglycemia is less of a concern with today’s range of antidiabetic agents. Physicians are now encouraged to practice “intensive glucose control,” i.e., attaining A1c values as close to 7.0% as possible while avoiding glucose variability. It is now understood that small, “silent” excursions of plasma glucose levels, including hypoglycemia, are as detrimental as major hypoglycemic episodes. CGM is a new tool for assessing and managing glycemic variability. The approaches to care outlined in this review can help physicians reach A1c goals without these attendant risks [84, 126, 127].
Large-scale clinical studies in patients with type 2 diabetes have provided a wealth of information. These trials helped identify the individual defects leading to hyperglycemia and develop drugs for these targets. These studies also highlighted the full complement of diabetes-related complications, including far-reaching outcomes such as inflammation, cancer, and Alzheimer’s disease. “Complication-centric prescribing” is now the new gold standard in treatment guidelines and strongly encourages physicians to stay pace with the various modes of action of agents, including GLP-1 receptor agonists, SGLT-2 inhibitors, and pioglitazone, as our understanding of the pleiotropic benefits of our glucose-lowering agents is evolving quickly. These trials clarified that longevity is associated with good gluco-stasis control, in part by its direct influence on the cardiorenal axis.
In one retrospective cohort study including ~ 100,000 patients, among patients with newly diagnosed type 2 diabetes, 22% remained under poor glycemic control over 2 years. A delay in intensive therapy of as little as one year in conjunction with poor glycemic control significantly increased the risk of myocardial infarction, health failure, stroke and composite cardiovascular events [22]. Critically, however, this study also revealed that 26% of patients never received intensive therapy.
Many patients are yet to benefit from the advances and approaches that we now have at our disposal, despite our impressive range of pharmacological tools. The lengthy process of incorporating evidence into guideline recommendations is one contributing factor. Another is outdated medical education that tethers physicians to fundamentally erroneous notions about the diabetic state. This contributes to clinical inertia through “physician habituation” to mainstream concepts and approaches that have fallen behind state-of-the-art research and care [4, 21, 22]. Fortunately, this problem is “treatable.” This review highlights selected advances and counterpoints (including several that are ahead of the guidelines) that are geared toward provisioning physicians to dispense up-to-date and optimal management of type 2 diabetes to their patients ahead of the sometimes sluggish incorporation into treatment guidelines.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- GLP-1:
-
Long-acting glucagon-like peptide-1 receptor agonists
- AACE:
-
American Association of Clinical Endocrinology
- CGM:
-
Continuous glucose monitoring
- EASD:
-
European Association for the Study of Diabetes
- GIP:
-
Glucose-dependent insulinotropic polypeptide
- GADA:
-
Glutamic acid decarboxylase
- LADA:
-
Latent autoimmune diabetes in adults
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- NAFLD:
-
Nonalcoholic fatty liver disease
- SGLT-2is:
-
Sodium-glucose cotransporter-2 inhibitors
- UKPDS:
-
United Kingdom Prospective Diabetes Study
References
Buzzetti R, Tuomi T, Mauricio D, Pietropaolo M, Zhou Z, Pozzilli P, et al. Management of latent autoimmune diabetes in adults: a consensus statement from an international expert panel. Diabetes. 2020;69(10):2037–47.
American Diabetes Association. Standards of medical care in diabetes—2009. Diabetes Care. 2009;32(Supplement_1):S13-61. Available from: https://diabetesjournals.org/care/article/32/Supplement_1/S13/25055/Standards-of-Medical-Care-in-Diabetes-2009.
Henry RR, Murray A V., Marmolejo MH, Hennicken D, Ptaszynska A, List JF. Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial. Int J Clin Pract. 2012;66(5):446–56. Available from: https://www.onlinelibrary.wiley.com/doi/10.1111/j.1742-1241.2012.02911.x.
Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract. 2018;137:137–48. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0168822717314468.
Unger J, Schwartz Z. Introduction to diabetes. In: Diabetes management in primary care- second edition. 2nd ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2012. p. 1–37.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):s49-s67.2. Available from: https://www.diabetesjournals.org/care/article/46/Supplement_1/s49/148058/4-Comprehensive-Medical-Evaluation-and-Assessment.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 13. Older adults: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):S216. Available from: https://www.diabetesjournals.org/care/article/46/Supplement_1/S216/148044/13-Older-Adults-Standards-of-Care-in-Diabetes-2023.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Cusi K, et al. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S52. Available from: https://www.diabetesjournals.org/care/article/47/Supplement_1/S52/153956/4-Comprehensive-Medical-Evaluation-and-Assessment.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes–2024. Diabetes Care. 2024;47(Supplement_1):S145-57. Available from: https://www.diabetesjournals.org/care/article/47/Supplement_1/S145/153942/8-Obesity-and-Weight-Management-for-the-Prevention.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S158-78. Available from: https://www.diabetesjournals.org/care/article/47/Supplement_1/S158/153955/9-Pharmacologic-Approaches-to-Glycemic-Treatment.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Das SR, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S179. Available from: https://www.diabetesjournals.org/care/article/47/Supplement_1/S179/153957/10-Cardiovascular-Disease-and-Risk-Management.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 11. Chronic kidney disease and risk management: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S219 Available from: https://diabetesjournals.org/care/article/47/Supplement_1/S219/153938/11-Chronic-Kidney-Disease-and-Risk-Management.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 11. Chronic kidney disease and risk management: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):S191-202.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):S140-57.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):S158-90.
Samson SL, Vellanki P, Blonde L, Christofides EA, Galindo RJ, Hirsch IB, et al. American Association of Clinical Endocrinology Consensus statement: comprehensive type 2 diabetes management algorithm - 2023 Update. Endocr Pract. 2023;29(5):305–40.
Riddle MC, Cefalu WT, Evans PH, Gerstein HC, Nauck MA, Oh WK, et al. Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetes Care. 2021;44(10):2438–44.
Handelsman Y, Butler J, Bakris GL, DeFronzo RA, Fonarow GC, Green JB, et al. Early intervention and intensive management of patients with diabetes, cardiorenal, and metabolic diseases. J Diabetes Complications. 2023;37:108389. Elsevier Inc.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 2. Diagnosis and classification of diabetes: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S20-42. Available from: https://www.diabetesjournals.org/care/article/47/Supplement_1/S20/153954/2-Diagnosis-and-Classification-of-Diabetes.
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Ekhlaspour L, et al. 3. Prevention or delay of diabetes and associated comorbidities: standards of care in diabetes—2024. Diabetes Care. 2024;47(Supplement_1):S43-51. Available from: https://www.diabetesjournals.org/care/article/47/Supplement_1/S43/153945/3-Prevention-or-Delay-of-Diabetes-and-Associated.
Khunti K, Wolden ML, Thorsted BL, Andersen M, Davies MJ. Clinical inertia in people with type 2 diabetes. Diabetes Care. 2013;36(11):3411–7. Available from: https://www.diabetesjournals.org/care/article/36/11/3411/38071/Clinical-Inertia-in-People-With-Type-2-DiabetesA .
Paul SK, Klein K, Thorsted BL, Wolden ML, Khunti K. Delay in treatment intensification increases the risks of cardiovascular events in patients with type 2 diabetes. Cardiovasc Diabetol. 2015;14(1):100. Available from: http://www.cardiab.com/content/14/1/100 .
United States Renal Data System. 2021. USRDS Annual Data Report: epidemiology of kidney disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease; 2021. Available from: https://usrds-adr.niddk.nih.gov/2021.
Wen CP, Chang CH, Tsai MK, Lee JH, Lu PJ, Tsai SP, et al. Diabetes with early kidney involvement may shorten life expectancy by 16 years. Kidney Int. 2017;92(2):388–96.
DeFronzo RA, Tripathy D, Schwenke DC, Banerji M, Bray GA, Buchanan TA, et al. Pioglitazone for diabetes prevention in impaired glucose tolerance. N Engl J Med. 2011;364(12):1104–15.
Doehner W, Erdmann E, Cairns R, Clark AL, Dormandy JA, Ferrannini E, et al. Inverse relation of body weight and weight change with mortality and morbidity in patients with type 2 diabetes and cardiovascular co-morbidity: an analysis of the PROactive study population. Int J Cardiol. 2012;162(1):20–6. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0167527311017682 .
Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366(9493):1279–89. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0140673605675289 .
Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, et al. Pioglitazone after Ischemic Stroke or Transient Ischemic Attack. N Engl J Med. 2016;374(14):1321–31.
Rabbat MG, Lakshmanan S, Benjamin MM, Doros G, Kinninger A, Budoff MJ, et al. Benefit of icosapent ethyl on coronary physiology assessed by computed tomography angiography fractional flow reserve: EVAPORATE-FFRCT. Eur Hear J - Cardiovasc Imaging 2023;24(7):866–73. Available from: https://www.academic.oup.com/ehjcimaging/article/24/7/866/7135508.
Olshansky B, Bhatt DL, Miller M, Steg PG, Brinton EA, Jacobson TA, et al. Cardiovascular benefits of icosapent ethyl in patients with and without atrial fibrillation in REDUCE-IT. J Am Heart Assoc. 2023;12(5):e026756.
Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383(23):2219–29. Available from: http://www.nejm.org/doi/10.1056/NEJMoa2025845 .
Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL, Rossing P, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021;385(24):2252–63.
Fraccarollo D, Thomas S, Scholz C-J, Hilfiker-Kleiner D, Galuppo P, Bauersachs J. Macrophage mineralocorticoid receptor is a pleiotropic modulator of myocardial infarct healing. Hypertension. 2019;73(1):102–11. Available from: https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.12162 .
Baggio LL, Drucker DJ. Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. J Clin Invest. 2014;124(10):4223–6. Available from: http://www.jci.org/articles/view/78371 .
Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9(10):653–62.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1811744 .
Bailey CJ. GIP analogues and the treatment of obesity-diabetes. Peptides. 2020;125:170202. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0196978119301809 .
Ferreira JP, Verma S, Fitchett D, Ofstad AP, Lauer S, Zwiener I, et al. Metabolic syndrome in patients with type 2 diabetes and atherosclerotic cardiovascular disease: a post hoc analyses of the EMPA-REG OUTCOME trial. Cardiovasc Diabetol. 2020;19(1):200.
Oyama K, Raz I, Cahn A, Kuder J, Murphy SA, Bhatt DL, et al. Obesity and effects of dapagliflozin on cardiovascular and renal outcomes in patients with type 2 diabetes mellitus in the DECLARE–TIMI 58 trial. Eur Heart J. 2022;43(31):2958–67.
Pratley RE, Cannon CP, Cherney DZI, Cosentino F, McGuire DK, Essex MN, et al. Cardiorenal outcomes, kidney function, and other safety outcomes with ertugliflozin in older adults with type 2 diabetes (VERTIS CV): secondary analyses from a randomised, double-blind trial. Lancet Heal Longev. 2023;4(4):e143-54. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S2666756823000326.
Widiarti W, Sukmajaya AC, Nugraha D, Alkaff FF. Cardioprotective properties of glucagon-like peptide-1 receptor agonists in type 2 diabetes mellitus patients: a systematic review. Diabetes Metab Syndr Clin Res Rev. 2021;15(3):837–43.
Shaman AM, Bain SC, Bakris GL, Buse JB, Idorn T, Mahaffey KW, et al. Effect of the glucagon-like peptide-1 receptor agonists semaglutide and liraglutide on kidney outcomes in patients with type 2 diabetes: pooled analysis of SUSTAIN 6 and LEADER. Circulation. 2022;145(8):575–85. Available from: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.121.055459.
Cukierman-Yaffe T, Gerstein HC, Colhoun HM, Diaz R, García-Pérez L-E, Lakshmanan M, et al. Effect of dulaglutide on cognitive impairment in type 2 diabetes: an exploratory analysis of the REWIND trial. Lancet Neurol. 2020;19(7):582–90. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S1474442220301733.
Liu X, Liu Y, Liu H, Li H, Yang J, Hu P, et al. Dipeptidyl-peptidase-IV inhibitors, imigliptin and alogliptin, improve beta-cell function in type 2 diabetes. Front Endocrinol (Lausanne). 2021;12. Available from: https://www.frontiersin.org/articles/10.3389/fendo.2021.694390/full.
Bifari F, Manfrini R, Dei Cas M, Berra C, Siano M, Zuin M, et al. Multiple target tissue effects of GLP-1 analogues on non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH). Pharmacol Res. 2018;137:219–29. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S1043661818311071.
DeFronzo RA, Hompesch M, Kasichayanula S, Liu X, Hong Y, Pfister M, et al. Characterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetes. Diabetes Care. 2013;36(10):3169–76. Available from: https://www.diabetesjournals.org/care/article/36/10/3169/30454/Characterization-of-Renal-Glucose-Reabsorption-in.
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Prim. 2015;1(1):15019. Available from: https://www.nature.com/articles/nrdp201519 .
Merovci A, Mari A, Solis C, Xiong J, Daniele G, Chavez-Velazquez A, et al. Dapagliflozin lowers plasma glucose concentration and improves β-cell function. J Clin Endocrinol Metab. 2015;100(5):1927–32. Available from: https://www.academic.oup.com/jcem/article/100/5/1927/2829691.
Packer M. Critical reanalysis of the mechanisms underlying the cardiorenal benefits of SGLT2 inhibitors and reaffirmation of the nutrient deprivation signaling/autophagy hypothesis. Circulation. 2022;146:1383–405 Lippincott Williams and Wilkins.
Matthews DR, Cull CA, Stratton IM, Holman RR, Turner RC. UKPDS 26: sulphonylurea failure in non-insulin-dependent diabetic patients over six years. Diabet Med. 1998;15(4):297–303. Available from: https://doi.org/10.1002/(SICI)1096-9136(199804)15:4/3C297::AID-DIA572/3E3.0.CO;2-W.
Schwartz SS, Epstein S, Corkey BE, Grant SFA, Gavin JR, Aguilar RB. The time is right for a new classification system for diabetes: rationale and implications of the β-cell-centric classification schema. Diabetes Care. 2016;39:179–86 American Diabetes Association Inc.
Schwartz SS, Epstein S, Corkey BE, Grant SFA, Gavin JR III, Aguilar RB, et al. A unified pathophysiological construct of diabetes and its complications. Trends Endocrinol Metab. 2017;28(9):645–55.
DeFronzo RA, Lewin A, Patel S, Liu D, Kaste R, Woerle HJ, et al. Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care. 2015;38(3):384–93. Available from: https://www.diabetesjournals.org/care/article/38/3/384/37579/Combination-of-Empagliflozin-and-Linagliptin-as.
Norton L, Shannon C, Gastaldelli A, DeFronzo RA. Insulin: the master regulator of glucose metabolism. Metabolism. 2022;129:155142. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0026049522000208 .
Pories WJ, Dohm GL. Diabetes: have we got it all wrong? Diabetes Care. 2012;35(12):2438–42 Available from: https://diabetesjournals.org/care/article/35/12/2438/38577/Diabetes-Have-We-Got-It-All-Wrong-Hyperinsulinism .
Corkey BE, Deeney JT, Merrins MJ. What regulates basal insulin secretion and causes hyperinsulinemia? Diabetes. 2021;70(10):2174–82. Available from: https://www.diabetesjournals.org/diabetes/article/70/10/2174/137902/What-Regulates-Basal-Insulin-Secretion-and-Causes .
Su C, Gao L, May CL, Pippin JA, Boehm K, Lee M, et al. 3D chromatin maps of the human pancreas reveal lineage-specific regulatory architecture of T2D risk. Cell Metab. 2022;34(9):1394-1409.e4.
McCarthy MI. Genomic medicine at the heart of diabetes management. Diabetologia. 2015;58(8):1725–9. Available from: http://www.springerlink.fh-diploma.de/10.1007/s00125-015-3588-6 .
Fanelli CG, Porcellati F, Pampanelli S, Bolli GB. Insulin therapy and hypoglycaemia: the size of the problem. Diabetes Metab Res Rev. 2004;20(S2):S32-42. Available from: https://doi.org/10.1002/dmrr.514.
Letchumanan G, Abdullah N, Marlini M, Baharom N, Lawley B, Omar MR, et al. Gut microbiota composition in prediabetes and newly diagnosed type 2 diabetes: a systematic review of observational studies. Front Cell Infect Microbiol. 2022;12. Available from: https://doi.org/10.3389/fcimb.2022.943427/full.
Hoffman DJ, Powell TL, Barrett ES, Hardy DB. Developmental origins of metabolic diseases. Physiol Rev. 2021;101(3):739–95. Available from: https://www.journals.physiology.org/doi/10.1152/physrev.00002.2020 .
GRADE Study Research Group, Nathan DM, Lachin JM, Bebu I, Burch HB, Buse JB, Cherrington AL, Fortmann SP, Green JB, Kahn SE, Kirkman MS, Krause-Steinrauf H, Larkin ME, Phillips LS, Pop-Busui R, Steffes M, Tiktin M, Tripputi M, Wexler DJYN. Glycemia reduction in type 2 diabetes — microvascular and cardiovascular outcomes. N Engl J Med. 2022;387(12):1075–88. Available from: http://www.nejm.org/doi/10.1056/NEJMoa2200436 .
Shanik MH, Xu Y, Skrha J, Dankner R, Zick Y, Roth J. Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Diabetes Care. 2008;31 Suppl 2:S262-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18227495.
Abdul-Ghani M, DeFronzo RA. Insulin resistance and hyperinsulinemia: the egg and the chicken. J Clin Endocrinol Metab. 2021;106(4):1897–9. Available from: https://www.academic.oup.com/jcem/article/106/4/1897/6125328.
Prentki M. Islet cell failure in type 2 diabetes. J Clin Invest. 2006;116(7):1802–12. Available from: https://doi.org/10.1172/JCI29103.
Rachfal AW, Grant SF, Schwartz SS. The diabetes syndrome – a collection of conditions with common, interrelated pathophysiologic mechanisms. Int J Gen Med. 2021;14:923–36.
MacDonald CS, Nielsen SM, Bjørner J, Johansen MY, Christensen R, Vaag A, et al. One-year intensive lifestyle intervention and improvements in health-related quality of life and mental health in persons with type 2 diabetes: a secondary analysis of the U-TURN randomized controlled trial. BMJ Open Diabetes Res Care. 2021;9(1): e001840.
Garvey WT. Long-term health benefits of intensive lifestyle intervention in the Look AHEAD study. Obesity. 2021;29(8):1242–3.
Wing RR. Does lifestyle intervention improve health of adults with overweight/obesity and type 2 diabetes? Findings from the Look AHEAD Randomized Trial. Obesity. 2021;29(8):1246–58.
Taheri S, Zaghloul H, Chagoury O, Elhadad S, Ahmed SH, El Khatib N, et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): an open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020;8(6):477–89.
Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7(5):344–55.
Al-Mrabeh A, Hollingsworth KG, Shaw JAM, McConnachie A, Sattar N, Lean MEJ, et al. 2-year remission of type 2 diabetes and pancreas morphology: a post-hoc analysis of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2020;8(12):939–48. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S221385872030303X.
Goldenberg JZ, Day A, Brinkworth GD, Sato J, Yamada S, Jönsson T, et al. Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ. 2021;372:m4743.
DeFronzo RA, Tripathy D, Schwenke DC, Banerji M, Bray GA, Buchanan TA, et al. Prevention of diabetes with pioglitazone in ACT NOW. Diabetes. 2013;62(11):3920–6. Available from: https://www.diabetesjournals.org/diabetes/article/62/11/3920/33911/Prevention-of-Diabetes-With-Pioglitazone-in-ACT.
Armato JP, DeFronzo RA, Abdul-Ghani M, Ruby RJ. Successful treatment of prediabetes in clinical practice using physiological assessment (STOP DIABETES). Lancet Diabetes Endocrinol. 2018;6(10):781–9. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S2213858718302341.
Bakaloudi DR, Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Chourdakis M. Impact of the first COVID-19 lockdown on body weight: a combined systematic review and a meta-analysis. Clin Nutr. 2022;41(12):3046–54. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0261561421002077.
Serretti A, Mandelli L. Antidepressants and body weight. J Clin Psychiatry. 2010;71(10):1259–72. Available from: http://www.article.psychiatrist.com/?ContentType=START&ID=10007128.
Cao Z, Li W, Wen CP, Li S, Chen C, Jia Q, et al. Risk of death associated with reversion from prediabetes to normoglycemia and the role of modifiable risk factors. JAMA Netw Open. 2023;6(3):e234989.
Cousminer DL, Ahlqvist E, Mishra R, Andersen MK, Chesi A, Hawa MI, et al. First genome-wide association study of latent autoimmune diabetes in adults reveals novel insights linking immune and metabolic diabetes. Diabetes Care. 2018;41(11):2396–403.
Abdul-Ghani MA, Puckett C, Triplitt C, Maggs D, Adams J, Cersosimo E, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT. Diabetes, Obes Metab. 2015;17(3):268–75. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/dom.12417.
DeFronzo RA, Eldor R, Abdul-Ghani M. Pathophysiologic approach to therapy in patients with newly diagnosed type 2 diabetes. Diabetes Care. 2013;36(Supplement_2):S127-38.
Administration USF and D. FDA approves new medication for chronic weight management. 2023. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-new-medication-chronic-weight-management.
Garvey WT, Frias JP, Jastreboff AM, le Roux CW, Sattar N, Aizenberg D, et al. Tirzepatide once weekly for the treatment of obesity in people with type 2 diabetes (SURMOUNT-2): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2023;402(10402):613–26. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S014067362301200X.
Stanley SS. Changing the face of diabetes. Int J Diabetes Clin Res. 2022;9(2):157.
Schwartz SS, Jellinger PS, Herman ME. Obviating much of the need for insulin therapy in type 2 diabetes mellitus: a re-assessment of insulin therapy’s safety profile. Postgrad Med. 2016;128(6):609–19. Available from: http://www.tandfonline.com/doi/full/10.1080/00325481.2016.1191955.
Herman ME, O’Keefe JH, Bell DSH, Schwartz SS. Insulin therapy increases cardiovascular risk in type 2 diabetes. Prog Cardiovasc Dis. 2017;60(3):422–34. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0033062017301391.
Azoulay L, Suissa S. Sulfonylureas and the risks of cardiovascular events and death: a methodological meta-regression analysis of the observational studies. Diabetes Care. 2017;40(5):706–14. Available from: https://www.diabetesjournals.org/care/article/40/5/706/36863/Sulfonylureas-and-the-Risks-of-Cardiovascular.
Volke V, Katus U, Johannson A, Toompere K, Heinla K, Rünkorg K, et al. Systematic review and meta-analysis of head-to-head trials comparing sulfonylureas and low hypoglycaemic risk antidiabetic drugs. BMC Endocr Disord. 2022;22(1):251.
GRADE Study Research Group, Nathan DM, Lachin JM, Balasubramanyam A, Burch HB, Buse JB, Butera NM, Cohen RM, Crandall JP, Kahn SE, Krause-Steinrauf H, Larkin ME, Rasouli N, Tiktin M, Wexler DJYN. Glycemia reduction in type 2 diabetes — glycemic outcomes. N Engl J Med. 2022;387(12):1063–74. Available from: http://www.nejm.org/doi/10.1056/NEJMoa2200433.
Qian L, Zhang S, Xu L, Peng Y. Endoplasmic reticulum stress in beta cells: latent mechanism of secondary sulfonylurea failure in type 2 diabetes? Med Hypotheses. 2008;71(6):889–91. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S030698770800368X.
Shi Y, Taylor SI, Tan S-L, Sonenberg N. When translation meets metabolism: multiple links to diabetes. Endocr Rev. 2003;24(1):91–101. Available from: https://www.academic.oup.com/edrv/article/24/1/91/2424303.
Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1700459.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric surgery versus intensive medical therapy for diabetes — 5-year outcomes. N Engl J Med. 2017;376(7):641–51. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1600869.
Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults. JAMA. 2020;324(9):879. Available from: https://www.jamanetwork.com/journals/jama/fullarticle/2770015.
Ikramuddin S, Billington CJ, Lee W-J, Bantle JP, Thomas AJ, Connett JE, et al. Roux-en-Y gastric bypass for diabetes (the Diabetes Surgery Study): 2-year outcomes of a 5-year, randomised, controlled trial. Lancet Diabetes Endocrinol. 2015;3(6):413–22. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S2213858715000893.
Courcoulas AP. New indications for metabolic and bariatric surgery. Lancet Diabetes Endocrinol. 2023;11(3):151–3. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S2213858723000359.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Capristo E, et al. Metabolic surgery versus conventional medical therapy in patients with type 2 diabetes: 10-year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2021;397(10271):293–304. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0140673620326490.
Salminen P, Helmiö M, Ovaska J, Juuti A, Leivonen M, Peromaa-Haavisto P, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity. JAMA. 2018;319(3):241. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2017.20313.
Courcoulas AP, Belle SH, Neiberg RH, Pierson SK, Eagleton JK, Kalarchian MA, et al. Three-year outcomes of bariatric surgery vs lifestyle intervention for type 2 diabetes mellitus treatment. JAMA Surg. 2015;150(10):931. Available from: http://www.archsurg.jamanetwork.com/article.aspx?doi=https://doi.org/10.1001/jamasurg.2015.1534.
Xu G, Song M. Recent advances in the mechanisms underlying the beneficial effects of bariatric and metabolic surgery. Surg Obes Relat Dis. 2021;17(1):231–8. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S1550728920304950.
Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, Coday M, et al. Implications of Look AHEAD for clinical trials and clinical practice. Diabetes, Obesity and Metabolism. 2014;16:1183–91 Blackwell Publishing Ltd.
Abdul-Ghani MA, Puckett C, Triplitt C, Maggs D, Adams J, Cersosimo E, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT. Diabetes, Obes Metab. 2015;17(3):268–75.
Abdul-Ghani M, Puckett C, Adams J, Khattab A, Baskoy G, Cersosimo E, et al. Durability of triple combination therapy versus stepwise addition therapy in patients with new-onset T2DM: 3-year follow-up of EDICT. Diabetes Care. 2021;44(2):433–9. Available from: https://diabetesjournals.org/care/article/44/2/433/35501/Durability-of-Triple-Combination-Therapy-Versus.
Lavynenko O, Abdul-Ghani M, Alatrach M, Puckett C, Adams J, Abdelgani S, et al. Combination therapy with pioglitazone/exenatide/metformin reduces the prevalence of hepatic fibrosis and steatosis: the efficacy and durability of initial combination therapy for type 2 diabetes (EDICT ). Diabetes, Obes Metab. 2022;24:899–907. Available from: https://doi.org/10.1111/dom.14650.
Thomas DD, Corkey BE, Istfan NW, Apovian CM. Hyperinsulinemia: an early indicator of metabolic dysfunction. J Endocr Soc. 2019;3(9):1727–47. Available from: https://www.academic.oup.com/jes/article/3/9/1727/5537533.
Reed MA, Pories WJ, Chapman W, Pender J, Bowden R, Barakat H, et al. Roux-en-Y gastric bypass corrects hyperinsulinemia implications for the remission of type 2 diabetes. J Clin Endocrinol Metab. 2011;96(8):2525–31. Available from: https://www.academic.oup.com/jcem/article-lookup/doi/10.1210/jc.2011-0165.
Abdul-Ghani M, Migahid O, Megahed A, DeFronzo RA, Al-Ozairi E, Jayyousi A. Combination therapy with pioglitazone/exenatide improves beta-cell function and produces superior glycaemic control compared with basal/bolus insulin in poorly controlled type 2 diabetes: a 3- year follow-up of the Qatar study. Diabetes, Obes Metab. 2020;22(12):2287–94. Available from: https://www.dom-pubs.pericles-prod.literatumonline.com/doi/10.1111/dom.14153.
Kramer CK, Zinman B, Retnakaran R. Short-term intensive insulin therapy in type 2 diabetes mellitus: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013;1(1):28–34. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S2213858713700068.
Al Jobori H, Daniele G, Adams J, Cersosimo E, Solis-Herrera C, Triplitt C, et al. Empagliflozin treatment is associated with improved β-cell function in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2018;103(4):1402–7. Available from: https://www.academic.oup.com/jcem/article/103/4/1402/4801231.
Liu X, Wu S, Song Q, Wang X. Reversion from pre–diabetes mellitus to normoglycemia and risk of cardiovascular disease and all-cause mortality in a chinese population: A prospective cohort study. J Am Heart Assoc. 2021;10(3):1–9.
Fatima F, Hjelmesæth J, Birkeland KI, Gulseth HL, Hertel JK, Svanevik M, et al. Gastrointestinal hormones and β-cell function after gastric bypass and sleeve gastrectomy: a randomized controlled trial (Oseberg). J Clin Endocrinol Metab. 2022;107(2):e756-66. Available from: https://www.academic.oup.com/jcem/article/107/2/e756/6360504.
Zhyzhneuskaya SV, Al-Mrabeh A, Peters C, Barnes A, Aribisala B, Hollingsworth KG, et al. Time course of normalization of functional β-cell capacity in the diabetes remission clinical trial after weight loss in type 2 diabetes. Diabetes Care. 2020;43(4):813–20. Available from: https://www.diabetesjournals.org/care/article/43/4/813/35800/Time-Course-of-Normalization-of-Functional-Cell.
Riddle MC, Cefalu WT, Evans PH, Gerstein HC, Nauck MA, Oh WK, et al. Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetologia. 64(11). https://doi.org/10.1007/s00125-021-05542-z.
Miller E, Aguilar RB, Herman ME, Schwartz SS. Type 2 diabetes: evolving concepts and treatment. Cleve Clin J Med. 2019;86(7):494–504. Available from: https://www.ccjm.org//lookup/doi/10.3949/ccjm.86a.17107.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RCGR. 7. Diabetes technology: standards of medical care in diabetes—2022. Diabetes Care. 2022;45(Supplement_1):S97-112.
Grunberger G, Sherr J, Allende M, Blevins T, Bode B, Handelsman Y, et al. American Association of Clinical Endocrinology clinical practice guideline: the use of advanced technology in the management of persons with diabetes mellitus. Endocr Pract. 2021;27(6):505–37. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S1530891X21001658.
Miller E, Gavin JR, Kruger DF, Brunton SA. Continuous glucose monitoring: optimizing diabetes care: executive summary. Clin Diabetes. 2022;40(4):394–8.
Bailey CJ, Gavin JR. Flash continuous glucose monitoring: a summary review of recent real-world evidence. Clin Diabetes. 2021;39(1):64–71.
Gavin JR, Bailey CJ. Real-world studies support use of continuous glucose monitoring in type 1 and type 2 diabetes independently of treatment regimen. Diabetes Technol Ther. 2021;23(S3):S-19-S−27.
Martens T, Beck RW, Bailey R, Ruedy KJ, Calhoun P, Peters AL, et al. Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin. JAMA. 2021;325(22):2262.
Fang Y, Zhang C, Shi H, Wei W, Shang J, Zheng R, et al. Characteristics of the gut microbiota and metabolism in patients with latent autoimmune diabetes in adults: a case-control study. Diabetes Care. 2021;44(12):2738–46.
Amrom D, Schwartz SS. Maternal metabolic health, lifestyle, and environment – understanding how epigenetics drives future offspring health. Curr Diabetes Rev. 2023;19(2):e220422203919. Available from: https://www.eurekaselect.com/203919/article.
Leslie RD, Grant SFA. Teasing diabetes apart, one locus at a time. Diabetes Care. 2018;41(2):224–6.
Schwartz SS, Grant SFA, Herman ME. Intersections and clinical translations of diabetes mellitus with cancer promotion, progression and prognosis. Postgrad Med. 2019;131(8):597–606.
Yang G, Wei J, Liu P, Zhang Q, Tian Y, Hou G, et al. Role of the gut microbiota in type 2 diabetes and related diseases. Metabolism. 2021;117:154712. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0026049521000123.
Schwartz S, Herman M. Revisiting weight reduction and management in the diabetic patient: novel therapies provide new strategies. Postgrad Med. 2015;127(5):480–93. Available from: https://www.tandfonline.com/doi/full/10.1080/00325481.2015.1043182.
Abdelgani S, Puckett C, Adams J, Triplitt C, DeFronzo RA, Abdul-Ghani M. Insulin secretion is a strong predictor for need of insulin therapy in patients with new-onset diabetes and HbA1c of more than 10%: post hoc analysis of the EDICT study. Diabetes, Obes Metab. 2021;23(7):1631–9. Available from: https://doi.org/10.1111/dom.14383.
Acknowledgements
None.
Funding
No funding was received directly or indirectly in the drafting of this article or views expressed.
Author information
Authors and Affiliations
Contributions
M.E.H. was integral to the synthesis of the article, as well as researched and drafted the manuscript. S.S.S. is the impetus for the article and highlighted key points. B.E.C.. J.R.G. and R.A.D. contributed to the key points. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No patients were used in the production of this review article.
Consent for publication
None relevant for this review article.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Schwartz, S.S., Corkey, B.E., R Gavin, J. et al. Advances and counterpoints in type 2 diabetes. What is ready for translation into real-world practice, ahead of the guidelines. BMC Med 22, 356 (2024). https://doi.org/10.1186/s12916-024-03518-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03518-5