Abstract
Objective
We aimed to summarize the association between gestational diabetes mellitus (GDM) and its intergenerational cardiovascular diseases (CVDs) impacts in both mothers and offspring post-delivery in existing literature.
Methods
PubMed, Embase, Web of Science, and Scopus were utilized for searching publications between January 1980 and June 2024, with data extraction and meta-analysis continuing until 31 July 2024. Based on a predefined PROSPERO protocol, studies published as full-length, English-language journal articles that reported the presence of GDM during pregnancy and its association with any CVD development post-delivery were selected. All studies were evaluated using the Newcastle-Ottawa Scale. Maximally adjusted risk estimates were pooled using random-effects meta-analysis to assess the risk ratio (RR) of GDM, and overall and subtypes of CVDs in both mothers and offspring post-delivery.
Results
The meta-analysis was based on 38 studies with a total of 77,678,684 participants. The results showed a 46% increased risk (RR 1.46, 95% CI 1.34–1.59) for mothers and a 23% increased risk (1.23, 1.05–1.45) for offspring of developing overall CVDs after delivery, following a GDM-complicated pregnancy. Our subgroup analysis revealed that mothers with a history of GDM faced various risks (20% to 2-fold) of developing different subtypes of CVDs, including cerebrovascular disease, coronary artery disease, heart failure, and venous thromboembolism.
Conclusions
These findings underscore the heightened risk of developing various CVDs for mothers and offspring affected by GDM, emphasizing the importance of preventive measures even right after birth to mitigate the burden of CVDs in these populations.
Similar content being viewed by others
Background
Gestational Diabetes Mellitus (GDM) is characterized by elevated blood sugar levels. It is primarily diagnosed during the second or third trimester of pregnancy in women who do not have a pre-existing diabetic condition [1]. It is a prevalent metabolic disorder, affecting approximately 1% to over 30% of pregnancies [2]. In the year 2021, the American Heart Association (AHA) issued a statement underscoring the importance of considering adverse outcomes during pregnancy, such as hypertensive disorders, gestational diabetes, preterm delivery, small-for-gestational-age delivery, pregnancy loss, and placental abruption, when evaluating the risk of cardiovascular diseases (CVDs) in individuals with a history of pregnancy [3]. Notably, the risk remains elevated up to 25 years after pregnancy, particularly in the window of 8 to 15 years after delivery [4].
Emerging evidence suggests that offspring born to pregnancies complicated by GDM are at elevated risk of developing cardiovascular disorders later in life [5, 6]. Exposure to GDM in utero has been linked to cardiovascular risks, including elevated levels of total cholesterol and systolic blood pressure in offspring from mid-childhood to adolescence [5, 7]. However, data on the intergenerational impact of GDM on CVDs remains scarce, let alone a notable absence of a comprehensive systematic review and meta-analysis examining these impacts on overall and various subtypes of CVDs among mother-offspring pairs affected by GDM-complicated pregnancies.
Our review sought to explore the connections between GDM and the subsequent occurrence of overall CVDs as well as distinct types of CVDs in both mothers and offspring following childbirth. Specifically, considering that the existing body of literature primarily originates from Western populations, our objective is to evaluate the potential differences in outcomes for the Asian demographic. We put forth the hypothesis that women with a history of GDM and their offspring might be confronted with an elevated risk of CVD development. Due to the intimate interplay between maternal and offspring health throughout the pregnancy period, our findings could offer valuable insights into the underlying pathophysiology linking GDM and the emergence of intergenerational CVDs, and subsequently raise public awareness regarding postnatal care, particularly emphasizing early intervention, to enhance cardiovascular well-being for both mothers and offspring.
Methods
Search Strategy and Selection Criteria
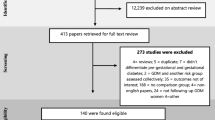
We conducted the systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement for standard protocols [8]. An investigator (L.-J.L.) oversaw the search strategy. References for this systematic review were identified through searches of four main databases (i.e., PubMed, Embase, Web of Science, and Scopus) for articles published between January 1, 1980, and June 30, 2024. Grey literature including case reports, working papers, government documents, white papers and evaluations were not included. Since we were interested in the intergenerational impact of maternal GDM on cardiovascular outcomes, we included two topics in our review. They are “Topic 1—maternal GDM and postpartum maternal CVD” and “Topic 2—maternal GDM and offspring CVD”. Search terms for these two topics are described in detail in Supplementary Table 1. Articles resulting from these searches and relevant references cited in those articles were reviewed, among which those reporting non-human subjects, written in non-English language or without full-text available were excluded. Flow charts of detailed literature searching on each topic are shown in Supplementary Fig. 1. This review was registered at PROSPERO International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/PROSPERO/) with the registration No. CRD42023438259.
Data Extraction and Assessment of Quality
During the literature searching phase, two investigators (C.S. & B.T.) independently selected eligible studies (based on title and abstract, followed by full-text articles) and extracted the relevant data. Results were verified and discrepancies (if any) were evaluated by a third investigator (L-J.L.). A clear set of pre-specified inclusion criteria and exclusion criteria was established prior to the data extraction. Studies published as full-length and English-language articles in peer-reviewed journals that reported the presence of GDM during pregnancy and its association with any CVD development post-delivery were included. Excluded studies were those published as case reports, reviews, letters, and conference abstracts. Non-full-length articles, non-English publications, and studies conducted on animal models were also excluded. The first phase was conducted in title and abstract screening (C.S., & B.T.), and the second phase was conducted in full-text screening (C.S., & B.T.). Subsequently, two investigators (C.S. & B.T.) performed the quality assessments for all papers based on the Newcastle-Ottawa Scale Criteria (NOSC) [9, 10] and a third investigator (L.-J.L.) assessed the findings independently. The maximum score of 9 points in the NOSC is distributed in three aspects based on the study groups, namely selection of study groups (four points), comparability of groups (two points), and ascertainment of exposure and outcomes (three points) for case–control and cohort studies. We used the points to further categorize the publication quality into low risk of bias (between 7 and 9 points), high risk of bias (between 4 and 6 points), and very high risk of bias (between 0 and 3 points) [9, 10]. The inter-rater agreement between the two investigators, C.S. and B.T., was 95% for the data extraction phase and 90% for the quality assessment phase. In cases of disagreement, the senior investigator, L.-J.L., reviewed the discrepancies and made the final decision.
Once all papers were identified for both topics, study characteristics such as the name of the first author, country of study conduction, number of participants, mean age, race/ethnicity, years of follow-up, GDM diagnostic guidelines, assessment of CVDs outcomes, effect size, and adjustments model were tabulated. Studies that detailed information on maternal GDM during index pregnancy and intergenerational CVDs diagnosis after delivery were further included in the meta-analysis. Studies that were identified to be at higher risk of bias were assigned a lower weightage in the calculation for overall effect size.
Data synthesis and analysis
Data analysis was conducted between 1st August 2023 and 31 July 2024. Due to the various effect sizes reported in papers, we calculated risk ratio (RR) using random-effects meta-analysis to represent estimates reported from different studies, including hazard ratio (HR), incidence rate ratio (IRR), and odds ratio (OR). For studies’ estimates stratified by comorbidity of type 2 diabetes (T2D) or overweight/obesity, an overall estimate was calculated based on the prevalence of within population T2D or overweight/obesity [9].
The risk estimate with the greatest degree of statistical adjustment was included in the meta-analysis. Statistical heterogeneity was assessed with the Cochran Q-test [10] and I2 statistic, defining levels as mild, moderate, substantial, and high heterogeneity based on I2 values falling within the ranges of 0–25%, 25–50%, 50–75%, and 75–100%, respectively [11, 12]. Publication bias was assessed visually with funnel plots and with the Egger [13, 14] (linear regression method) and Begg-Mazumdar [15] regression tests (rank correction method), and a p-value < 0.05 was considered representative of statistically significant publication bias [13, 15]. All analyses were conducted with Stata, version 17.0 (Stata Corporation, College Station, Texas, USA). All P values were from 2-sided tests, and the results were deemed statistically significant at p < 0.05 unless stated otherwise.
Subgroup Analysis
To comprehensively explore subgroup differences and potential sources of observed heterogeneity, we conducted a series of subgroup analyses based on various study characteristics. Firstly, we presented overall CVDs outcomes, and stratified further based on subtypes of CVDs outcomes based on individual studies. We categorized different CVDs conditions into the following subtypes: coronary artery disease (CAD), angina pectoris, heart failure, arrhythmia, valve disorders, peripheral artery disease, venous thromboembolism (VTE), cardiovascular procedures, cerebrovascular disease (CeVD) and aortic dissection (Supplementary Table 2). Secondly, based on the overall CVDs, we performed stratified meta-analyses based on study characteristics, such as study race/ethnicity (exclusive Asian vs. mixed population yet primarily composed of Caucasians), median duration of follow-up (> 10 years vs. ≤ 10 years), method for ascertaining GDM (medical code vs. self-reporting), and study quality (low risk of bias vs. moderate-to-high risk of bias). To assess the potential mediating role of subsequent development of T2D underlying the association between GDM and overall CVDs, we examined the risk ratio for overall CVDs in women who had T2D comorbidity and those who did not specify. Thirdly, we conducted subgroup analyses in associations of overall CVDs stratified by major covariates, such as BMI, lifestyle factors, socioeconomic status, pregnancy complications, and systemic comorbidities. Q-test based on one-way ANOVA was conducted using the R package (R 4.2.2), and statistical significance for any difference in estimates between subgroups was determined with a two-sided p-value threshold of < 0.10.
Results
Study characteristics and summaries in systematic review
Supplementary Table 3 summarizes the characteristics and quality scores of the 36 studies involving mothers (n = 74,890,936, follow-up range: 1 day to 46 years after index pregnancy) and the 6 studies involving offspring (n = 14,260,765, follow-up range: at birth to 40 years after index pregnancy) within the context of GDM-related pregnancies. The majority of these studies were cohort studies (n = 33), with a small subset being cross-sectional studies (n = 7), and two identified as case-control studies. These studies were further analysed to categorize the studied outcomes of interest into overall CVD outcomes and various subtypes of CVDs, as illustrated above.
GDM and overall CVD outcomes in mothers
Among the studies that presented CVDs outcomes in mothers, fourteen out of the 33 studies were conducted in the US [16,17,18,19,20,21,22,23,24,25,26,27,28,29], four in Canada [4, 30,31,32], five in Sweden [33,34,35,36,37], two in Iran [38, 39], three in the UK [40,41,42], while the remaining six were in Denmark [43], France [44], Netherlands [45], South Korea [46], China [47], Israel [48], and New Zealand [49], respectively. The sample sizes in these studies ranged from 391 to 2,201,352, and the ages of the study populations spanned from under 20 to over 65 years old. The reported incidence rates of overall CVDs varied from 14 to 1,818 cases per 1000 person-years (Supplementary Table 3). GDM was defined based on either medical reports/diagnostic codes or self-reported. Aside from medical reports and self-reported CVDs definition, clinical diagnostic assessments for CVDs included coronary computed tomography angiography [34, 38], electrocardiogram findings [19, 24, 38], echocardiogram [50], and cardiac-specific enzymes [19]. While the majority of articles reported a positive association between GDM and a 1.04- to 3.18-fold increased risk of maternal overall CVD outcomes post-index pregnancy, five studies reported a null association [22, 27, 29, 38, 45].
GDM and overall CVD outcomes in offspring
The six papers that reported CVD outcomes amongst offspring were conducted in the United States [51], the Czech Republic [52], Canada [53], Denmark [54], Israel [55], and France [56], respectively. The sample sizes ranged from 128 to 11,318,691, and the ages of the study populations spanned from birth to 40 years. The reported incidence rates ranged from 22 to 94 cases per 100,000 person-years (Supplementary Table 3). GDM at index pregnancy was all defined via clinical guidelines or diagnostic codes [51,52,53,54,55,56], while offspring CVDs outcomes were defined via national registries [51, 53, 54], hospital databases [55], or clinical diagnostic assessments such as two-dimensional electrocardiography [52] and neuroimaging or pathohistological examination [56].
All studies demonstrated a positive association between GDM-complicated pregnancy and a 1.19 to 2.24-fold increased risk of offspring overall CVDs following birth. Notably, Leybovitz-Haleluya et al. [55] observed a 60% higher risk of CVDs development in offspring born to mothers managed with oral treatment of insulin compared to those managed with diet and exercise alone. Moreover, Darmency-Stamboul et al. [56] reported a higher incidence of perinatal arterial ischemic stroke among boys compared to girls (59% vs. 41%), while Guillemette et al. [53] did not find any significant interaction between the sex of offspring and CVDs outcomes.
Meta-analysis of GDM and postpartum CVDs development in mothers
Table 1; Fig. 1A summarizes key study characteristics, including study population details, locations, follow-up periods, pre-pregnancy BMI, sample sizes, methods for defining GDM and CVDs, and effect sizes with 95% confidence intervals. Most studies made statistical adjustments for maternal age, race/ethnicity, and BMI. In a meta-analysis of thirty-three studies, women with GDM were found to have a higher risk of developing overall CVDs (RR 1.46, 95% CI 1.34–1.59) over follow-up periods from one day to 46 years. Among these studies, 19 had low bias risk [4, 16, 18, 19, 23, 29,30,31,32, 34, 36, 38, 40,41,42,43, 45, 46, 48], while 13 had high bias risk [17, 20, 21, 24, 27, 28, 34, 35, 37, 39, 44, 47, 49], and one had very high bias risk [26] (Table 1). The analysis showed significant heterogeneity (I2 = 95.44%), and a p-value less than 0.001 from Cochran’s Q test, indicating significantly substantial variability among all publications (Fig. 1A). Publication bias assessment using Egger’s and Begg’s tests, along with a funnel plot (Supplementary Fig. 2), indicated no evidence of bias, with Egger’s test result (p = 0.76) and Begg’s test result (p = 0.61) supporting this conclusion.
Meta-analysis Results. Evidence of risk ratio (RR) and 95% confidence interval (CI) of maternal GDM and maternal postpartum overall CVDs (A) and offspring overall CVDs (B), using unadjusted random-effects model. Heterogeneity was presented in both I2 (describing the percentage of variation across studies that is due to heterogeneity rather than chance) and T2 (reflecting the variance of the true effect sizes). Abbreviations: RR: risk ratio; confidence interval; %, percentage
For various CVDs subtypes, women with GDM exhibited significantly elevated risks in different categories: coronary artery disease (1.53; 1.32–1.76), heart failure (1.38; 1.17–1.62), venous thromboembolism (1.18; 1.00-1.39), cardiovascular procedures (2.10; 1.63–2.70), peripheral artery disease (2.00; 1.62–2.48), arrhythmia (1.48; 1.46–1.50), angina pectoris (2.03; 1.44–2.85), as well as overall CeVDs (1.27; 1.11–1.44) including ischemic stroke/TIA (1.52; 1.30–1.78), and haemorrhagic stroke/intracranial haemorrhage (1.44; 1.15–1.78), compared to women without a history of GDM (Fig. 2).
Subgroup analyses stratified by subtypes of CVDs. Evidence of risk ratio (RR) and 95% confidence interval (CI) of maternal GDM and subtypes of CVDs in both mothers and offspring using unadjusted random-effects model. Heterogeneity was presented in both I2 (describing the percentage of variation across studies that is due to heterogeneity rather than chance) and T2 (reflecting the variance of the true effect sizes)
Subgroup analyses based on study characteristics such as race/ethnicity, sample size, follow-up duration, diagnostic methods for GDM, comorbidities of Type 2 Diabetes (T2D), overweight or obesity, and study quality grading did not show significant differences in pooled risk ratios (Supplementary Fig. 3) (all Q-test p > 0.10). For instance, studies indicated a similar heightened risk of overall CVDs outcomes in women who are overweight or obese (1.51; 1.27–1.80) compared to the general population of women (1.47; 1.34–1.62) (p = 0.44). Additionally, findings revealed that women with T2D did not have an increased risk of overall CVDs outcomes (1.40, 1.13–1.75) in comparison to those without T2D (1.47, 1.34–1.62) (p = 0.69).
Further subgroup analyses revealed significant differences between subgroups when adjusting for major confounders. Notably, it showed significant differences if certain key confounders were not adjusted for in the association between GDM and postpartum CVDs in mothers, namely maternal pre-pregnancy BMI at study entry (Yes vs. No: 1.39, 1.32–1.56 vs. 1.63, 1.36–1.94; p = 0.06), parity (Yes vs. No: 1.36, 1.25–1.48 vs. 1.55, 1.34–1.81; p = 0.095), and comorbidities (Yes vs. No: 1.37, 1.26–1.49 vs. 1.60, 1.37–1.86; p = 0.07) (Supplementary Fig. 4).
Meta-analysis of GDM and CVDs development in offspring
Table 2; Fig. 1B summarizes key characteristics of the five included studies, detailing study population, location, follow-up years, pre-pregnancy BMI, offspring BMI, ascertainment methods, sample sizes for GDM in mothers and CVDs in offspring, and effect sizes with 95% CI. The meta-analysis revealed that offspring born to mothers with GDM showed a 20% higher risk of developing overall CVDs (1.23; 1.05–1.45) over 0 to 40 years of follow-up period, with high heterogeneity (I2 = 78.07%) (Fig. 1B) and high publication bias, which was supported the funnel plot (Supplementary Fig. 5). Due to few publications, subgroup analysis was only successful for CeVD, in which the increased risk of CeVD outcomes in offsprings of mothers with GDM was not statistically significant (1.26; 0.88–1.80) (Fig. 2).
Discussion
This systematic review and meta-analysis synthesized available evidence on GDM and its association with a higher incidence of CVDs in both mothers and offspring post-delivery. Our analysis revealed a 45% increased risk of postpartum CVDs in mothers and a 31% increased risk in offspring over follow-up periods ranging from day 1 to over 40 years after delivery. In mothers, subtypes of CVDs such as coronary artery disease, heart failure, cardiovascular procedures, peripheral artery disease, arrhythmia, and angina pectoris showed increased risks ranging from 45% to 2-fold, while the risk of stroke was enhanced by 20%.
GDM and postpartum CVDs development in mothers
The mechanisms involved in GDM-associated CVDs development among mothers are related to cardiovascular risk factors, endothelial dysfunction, and myocardial remodelling [19, 40, 57]. To begin with, an elevated cardiovascular risk profile that includes conditions such as dyslipidaemia [58] and metabolic syndrome [59, 60], characterizes women with a history of GDM. These predisposing factors heighten their risk of developing CVDs in comparison to their non-GDM counterparts. Additionally, women with GDM have a seven to tenfold higher risk of transitioning to T2D in their later years [61,62,63]. This increased risk has been attributed to elevated markers of inflammation and reduced levels of adiponectin present in women with prior GDM [64].
Secondly, vascular dysfunction is recognized as an independent risk factor for CVDs [65]. It has been strongly suggested that even though GDM induces a temporary phase of significant glucose intolerance during pregnancy, it might result in substantial and irreversible changes within the endothelium [4]. Research indicates that women with a history of GDM exhibit decreased coronary flow reserve [66], which is a marker of potential cardiovascular issues. They also have a higher incidence of impaired endothelial vasodilation [30, 67], and increased carotid intima-media thickness (cIMT) [30, 64] when compared to their counterparts.
Thirdly, although normal pregnancy brings hemodynamic and physiological changes to the cardiovascular system [68], these are more pronounced in GDM. Advanced glycation end products in GDM can lead to critical alterations like altered preload, contractility, and heart rate, causing physiological left ventricular (LV) remodelling [69], endothelial damage, and reduced arterial elasticity [70]. These changes can persist after delivery, potentially leading to overt CVDs in women with GDM [71]. Emerging evidence has shown that women with a history of GDM manifested lower LV diastolic and systolic function during late pregnancy [72], and greater left ventricular mass, impaired LV relaxation, and lower LV systolic function years after delivery [73], compared with their counterparts.
GDM and CVDs development in offspring
Although research exploring the link between GDM and the subsequent development of CVDs in offspring is relatively limited, our analysis revealed a consistent and strong positive correlation across the five studies included in our review. Notably, some evidence even indicated the early onset of CVDs soon after birth in infants born to mothers with GDM [74].
Firstly, the intrauterine environment characterized by hyperglycemic level can adversely affect placental morphology and vasculature, leading to conditions such as villous immaturity, villous edema, villous fibrinoid necrosis, and chorangiosis [75]. These changes could cause fetal hypoxia, which prompts the release of reactive oxygen and nitrogen species, ultimately resulting in an overstimulation of nitrogen oxide [76]. Such pathological changes can increase inflammation [77] and lead to vascular endothelial dysfunction [78] in the fetoplacental unit, culminating in intrauterine growth restriction (IUGR) [79]. This has been concluded to be the underlying mechanism of the development of hypertension and other types of CVDs [65, 80].
Secondly, fetal hyperinsulinemia can occur as a result of constant maternal hyperglycemia experienced in utero [81]. Over time, this sustained elevation in insulin production within the fetoplacental circulation may harm the fetal pancreatic islet beta cells, diminishing their ability to respond to hyperglycemia by secreting insulin [82]. This state of hyperinsulinemia could subsequently contribute to cardiac dysfunction in the offspring. For instance, studies indicated that up to 40% of pregnancies complicated by diabetes will result in offspring with myocardial hypertrophy, characterized by a thickened interventricular septum and ventricular walls, along with systolic and diastolic dysfunction [83].
Thirdly, maternal hyperglycemia may induce fetal hypoxia that results in an increased release of reactive oxygen species in both the fetus and placenta [76]. This can trigger oxidative damage to membrane lipids and deteriorate mitochondrial DNA [84]. Research has demonstrated that placentas impacted by GDM exhibit reduced gene and protein expression of markers associated with mitochondrial fusion and proteins related to mitochondrial biogenesis [84]. Such mitochondrial dysfunction can also extend to the myocardiocytes in the fetal heart, disrupting normal cardiac development [85].
Clinical implications
As a result of endothelial dysfunction and cardiac remodelling, against a background of CVD risks, women with a history of GDM have elevated risks of developing CVDs in the postpartum period and years after. Our study presents substantial evidence indicating that not only mothers with GDM but also their offspring face a similarly elevated risk of developing CVDs after birth. These findings underscore the importance of developing early prevention strategies that prevent the development of CVDs in GDM-complicated pregnancies. Future public health policies might incorporate these insights, by considering a history of GDM as a unique standalone CVD risk factor for both the mother and the offspring. The inclusion of GDM as a risk factor in CVD risk scoring systems might form the initial steps into public health strategies. Further assessment strategies might include targeted cardiac evaluation via easy-to-use tools such as measures of arterial stiffness, ultrasonography, or cardiac biomarkers.
Strengths and limitations
The primary strength of this systematic review lies in its extensive analysis of research evidence regarding the association of GDM and overall and subtypes of CVDs in both maternal and offspring. The robustness of our study is fortified by a meticulous search strategy, ensuring the thorough identification of all eligible studies, and subgroup analyses. However, the study is not without its limitations. Firstly, our paper exclusively incorporated pertinent papers procured from four distinct search engines, limited to English-language publications. This approach could potentially introduce information bias if pertinent content is present but published in languages other than English or not covered within the predetermined quartet of databases. Secondly, there may be significant heterogeneity observed across studies. This variance stems from divergent follow-up durations, distinct protocols for data collection and screening methodologies, as well as variations in the diagnostic criteria or self-reported definition for GDM and CVDs. Thirdly, reporting risk over such an extended time frame, drawn from various papers without assessing the stability of risk over time, may complicate the contextualization of the reported estimates. Fourthly, pooled risk ratios derived from only two studies in the subgroup analysis should be interpreted with caution. Lastly, while GDM not only heightens the risk of CVDs, it also increases the likelihood of overweight/obesity and type 2 diabetes (T2D) in both mothers and their children, potentially mediating the development of CVDs in both generations. Nonetheless, our subgroup analyses, stratified by overweight/obesity status or T2D comorbidity, did not support these hypotheses. Further investigations utilizing a prospective longitudinal study design with more frequent follow-ups are essential to comprehensively grasp the potential mediating role of metabolic disorders underlying GDM and the development of intergenerational CVDs.
Conclusion
Our systematic review and meta-analysis unveiled increased risks of developing overall and subtypes of CVDs in both mothers and offspring impacted by GDM. These staggering and enduring risks of GDM across two generations highlight an urgent public health need to increase awareness of CVD risks associated with GDM. Future population health strategies that include dedicated CVD risk assessment and cardiac evaluation represent crucial next steps for the field of GDM.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AHA:
-
American Heart Association
- CAD:
-
Coronary Artery Disease
- CeVD:
-
Cerebrovascular Disease
- CI:
-
Confidence Interval
- cIMT:
-
Carotid Intima-media Thickness
- CVD:
-
Cardiovascular disease
- GDM:
-
Gestational Diabetes Mellitus
- HR:
-
Hazard Ratio
- IRR:
-
Incidence Rate Ratio
- IUGR:
-
Intrauterine Growth Restriction
- LV:
-
Left Ventricular
- OR:
-
Odds Ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- RR:
-
Risk Ratio
- T2D:
-
Type 2 Diabetes
- VTE:
-
Venous Thromboembolism
References
American Diabetes A. 2. Classification and diagnosis of diabetes: standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–31.
McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Parikh NI, Gonzalez JM, Anderson CAM, Judd SE, Rexrode KM, Hlatky MA, Gunderson EP, Stuart JJ, Vaidya D, American Heart Association Council on E. Adverse pregnancy outcomes and Cardiovascular Disease Risk: Unique Opportunities for Cardiovascular Disease Prevention in Women: A Scientific Statement from the American Heart Association. Circulation. 2021;143(18):e902–16.
McKenzie-Sampson S, Paradis G, Healy-Profitos J, St-Pierre F, Auger N. Gestational diabetes and risk of cardiovascular disease up to 25 years after pregnancy: a retrospective cohort study. Acta Diabetol. 2018;55(4):315–22.
Perng W, Hockett CW, Sauder KA, Dabelea D. In utero exposure to gestational diabetes mellitus and cardiovascular risk factors in youth: a longitudinal analysis in the EPOCH cohort. Pediatr Obes. 2020;15(5):e12611.
Tam WH, Ma RCW, Ozaki R, Li AM, Chan MHM, Yuen LY, Lao TTH, Yang X, Ho CS, Tutino GE, et al. In Utero exposure to maternal hyperglycemia increases Childhood Cardiometabolic risk in offspring. Diabetes Care. 2017;40(5):679–86.
West NA, Crume TL, Maligie MA, Dabelea D. Cardiovascular risk factors in children exposed to maternal diabetes in utero. Diabetologia. 2011;54(3):504–7.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2(2):121–45.
Hoaglin DC. Misunderstandings about Q and ‘Cochran’s Q test’ in meta-analysis. Stat Med. 2016;35(4):485–95.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Xie W, Wang Y, Xiao S, Qiu L, Yu Y, Zhang Z. Association of gestational diabetes mellitus with overall and type specific cardiovascular and cerebrovascular diseases: systematic review and meta-analysis. BMJ. 2022;378:e070244.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–80.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Arnaout R, Nah G, Marcus G, Tseng Z, Foster E, Harris IS, Divanji P, Klein L, Gonzalez J, Parikh N. Pregnancy complications and premature cardiovascular events among 1.6 million California pregnancies. Open Heart. 2019;6(1):e000927.
Mao Y, Hu W, Xia B, Liu L, Han X, Liu Q. Association between Gestational Diabetes Mellitus and the risks of Type-Specific Cardiovascular diseases. Front Public Health. 2022;10:940335.
Savitz DA, Danilack VA, Elston B, Lipkind HS. Pregnancy-induced hypertension and diabetes and the risk of cardiovascular disease, stroke, and diabetes hospitalization in the year following delivery. Am J Epidemiol. 2014;180(1):41–4.
Tobias DK, Stuart JJ, Li S, Chavarro J, Rimm EB, Rich-Edwards J, Hu FB, Manson JE, Zhang C. Association of History of Gestational Diabetes with Long-Term Cardiovascular Disease Risk in a large prospective cohort of US women. JAMA Intern Med. 2017;177(12):1735–42.
Wichmann JL, Takx RAP, Nunez JH, Vliegenthart R, Otani K, Litwin SE, Morris PB, De Cecco CN, Rosenberg RD, Bayer RR 2, et al. Relationship between pregnancy complications and subsequent coronary artery Disease assessed by Coronary Computed Tomographic Angiography in Black women. Circ Cardiovasc Imaging. 2019;12(7):e008754.
Zahid S, Hashem A, Minhas AS, Bennett WL, Honigberg MC, Lewey J, Davis MB, Michos ED. Trends, Predictors, and outcomes of Cardiovascular complications at Delivery Associated with Gestational Diabetes: A National Inpatient Sample Analysis (2004–2019). J Am Heart Assoc. 2022;11(21):e026786.
Shostrom DCV, Sun Y, Oleson JJ, Snetselaar LG, Bao W. History of gestational diabetes Mellitus in Relation to Cardiovascular Disease and Cardiovascular Risk factors in US women. Front Endocrinol (Lausanne). 2017;8:144.
Safdar B, Spatz ES, Dreyer RP, Beltrame JF, Lichtman JH, Spertus JA, Reynolds HR, Geda M, Bueno H, Dziura JD et al. (2018) Presentation, clinical profile, and prognosis of young patients with myocardial infarction with nonobstructive coronary arteries (MINOCA): results from the VIRGO study. J Am Heart Assoc 7(13)
Perera MJ, Reina SA, Elfassy T, Potter JE, Sotres Alvarez D, Simon MA, Isasi CR, Stuebe AM, Schneiderman N, Llabre MM. Gestational diabetes and cardiovascular risk factors and disease in U.S. Hispanics/Latinas in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Women Health. 2019;59(5):481–95.
Freibert SM, Mannino DM, Bush H, Crofford LJ. The association of adverse pregnancy events and cardiovascular disease in women 50 years of age and older. J Womens Health (Larchmt). 2011;20(2):287–93.
Carr DB, Utzschneider KM, Hull RL, Tong J, Wallace TM, Kodama K, Shofer JB, Heckbert SR, Boyko EJ, Fujimoto WY, et al. Gestational diabetes mellitus increases the risk of cardiovascular disease in women with a family history of type 2 diabetes. Diabetes Care. 2006;29(9):2078–83.
Ackerman-Banks CM, Palmsten K, Lipkind HS, Ahrens KA. Association between gestational diabetes and cardiovascular disease within 24 months postpartum. Am J Obstet Gynecol MFM. 2024;6(6):101366.
Bucci T, Meek CL, Awor S, Lip GYH, Merriel A. Five-year risk of all-cause death and cardiovascular events in women with gestational diabetes and hypertensive disorders of pregnancy. Curr Probl Cardiol. 2024;49(9):102698.
Countouris ME, Koczo A, Reynolds HR, Hausvater A, Mann H, Wang Y, Sharbaugh D, Thoma FW, Mulukutla SR, Catov JM. (2023) Characteristics of premature myocardial infarction among women with prior adverse pregnancy outcomes. JACC Adv 2(5)
Retnakaran R, Shah BR. Role of type 2 diabetes in determining Retinal, Renal, and Cardiovascular outcomes in Women with previous gestational diabetes Mellitus. Diabetes Care. 2017;40(1):101–8.
Echouffo-Tcheugui JB, Guan J, Retnakaran R, Shah BR. Gestational diabetes and Incident Heart failure: a Cohort Study. Diabetes Care. 2021;44(10):2346–52.
Kaul P, Savu A, Nerenberg KA, Donovan LE, Chik CL, Ryan EA, Johnson JA. Impact of gestational diabetes mellitus and high maternal weight on the development of diabetes, hypertension and cardiovascular disease: a population-level analysis. Diabet Med. 2015;32(2):164–73.
Taufer Cederlof E, Lundgren M, Lindahl B, Christersson C. Pregnancy complications and risk of Cardiovascular Disease later in life: a Nationwide Cohort Study. J Am Heart Assoc. 2022;11(2):e023079.
Sederholm Lawesson S, Swahn E, Pihlsgard M, Andersson T, Angeras O, Bacsovics Brolin E, Bergdahl E, Blomberg M, Christersson C, Goncalves I, et al. Association between History of Adverse Pregnancy Outcomes and coronary artery Disease assessed by Coronary computed Tomography Angiography. JAMA. 2023;329(5):393–404.
Fadl H, Magnuson A, Ostlund I, Montgomery S, Hanson U, Schwarcz E. Gestational diabetes mellitus and later cardiovascular disease: a Swedish population based case-control study. BJOG. 2014;121(12):1530–6.
Crump C, Sundquist J, McLaughlin MA, Dolan SM, Govindarajulu U, Sieh W, Sundquist K. Adverse pregnancy outcomes and long term risk of ischemic heart disease in mothers: national cohort and co-sibling study. BMJ. 2023;380:e072112.
Hilden K, Magnuson A, Montgomery S, Schwarcz E, Hanson U, Simmons D, Backman H. Previous pre-eclampsia, gestational diabetes mellitus and the risk of cardiovascular disease: a nested case-control study in Sweden. BJOG. 2023;130(10):1209–16.
Kabootari M, Hasheminia M, Guity K, Ramezankhani A, Azizi F, Hadaegh F. Gestational diabetes mellitus in mothers and long term cardiovascular disease in both parents: results of over a decade follow-up of the Iranian population. Atherosclerosis. 2019;288:94–100.
Hadaegh F, Asgari S, Moosaie F, Orangi M, Sarvghadi F, Khalili D, Azizi F. The risk and added values of the atherosclerotic cardiovascular risk enhancers on prediction of cardiovascular events: Tehran lipid and glucose study. J Transl Med. 2021;19(1):25.
Lee SM, Shivakumar M, Park JW, Jung YM, Choe EK, Kwak SH, Oh S, Park JS, Jun JK, Kim D, et al. Long-term cardiovascular outcomes of gestational diabetes mellitus: a prospective UK Biobank study. Cardiovasc Diabetol. 2022;21(1):221.
Daly B, Toulis KA, Thomas N, Gokhale K, Martin J, Webber J, Keerthy D, Jolly K, Saravanan P, Nirantharakumar K. Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study. PLoS Med. 2018;15(1):e1002488.
Michalopoulou M, Piernas C, Jebb SA, Gao M, Astbury NM. Association of gestational diabetes with long-term risk of premature mortality, and cardiovascular outcomes and risk factors: a retrospective cohort analysis in the UK Biobank. Diabetes Obes Metab. 2024;26(7):2915–24.
Yu Y, Soohoo M, Sorensen HT, Li J, Arah OA. Gestational diabetes Mellitus and the risks of overall and type-specific Cardiovascular diseases: a Population- and sibling-matched cohort study. Diabetes Care. 2022;45(1):151–9.
Goueslard K, Cottenet J, Mariet AS, Giroud M, Cottin Y, Petit JM, Quantin C. Early cardiovascular events in women with a history of gestational diabetes mellitus. Cardiovasc Diabetol. 2016;15:15.
Heida KY, Franx A, van Rijn BB, Eijkemans MJ, Boer JM, Verschuren MW, Oudijk MA, Bots ML, van der Schouw YT. Earlier age of onset of chronic hypertension and type 2 diabetes Mellitus after a hypertensive disorder of pregnancy or gestational diabetes Mellitus. Hypertension. 2015;66(6):1116–22.
Sun J, Kim GR, Lee SJ, Kim HC. Gestational diabetes mellitus and the role of intercurrent type 2 diabetes on long-term risk of cardiovascular events. Sci Rep. 2021;11(1):21140.
Wen J, Shuai W, Ding T, Feng Y, Zhang J, Wang S. Reproductive risk factors for angiographic obstructive coronary artery disease among postmenopausal women. Menopause. 2020;27(12):1403–10.
Kessous R, Shoham-Vardi I, Pariente G, Sherf M, Sheiner E. An association between gestational diabetes mellitus and long-term maternal cardiovascular morbidity. Heart. 2013;99(15):1118–21.
Daly BM, Wu Z, Nirantharakumar K, Chepulis L, Rowan JA, Scragg RKR. Increased risk of cardiovascular and renal disease, and diabetes for all women diagnosed with gestational diabetes mellitus in New Zealand-A national retrospective cohort study. J Diabetes. 2024;16(4):e13535.
Bakhsh A, AlSayed A, AlTamimi M, Alodhaib R, Binhudhud M, Ghazal H, Al Hebaishi Y. The outcome of heart failure in women: a study from a tertiary heart function clinic. Am J Cardiovasc Dis. 2023;13(5):300–8.
Farghaly MAA, Qattea I, Ali MAM, Saker F, Mohamed MA, Aly H. Intracranial hemorrhages in infants of diabetic mothers: a national cohort study. Early Hum Dev. 2023;183:105796.
Hromadnikova I, Kotlabova K, Dvorakova L, Krofta L, Sirc J. (2020) Substantially altered expression profile of diabetes/cardiovascular/cerebrovascular disease associated microRNAs in children descending from pregnancy complicated by gestational diabetes mellitus-one of several possible reasons for an increased cardiovascular risk. Cells 9(6)
Guillemette L, Wicklow B, Sellers EAC, Dart A, Shen GX, Dolinsky VW, Gordon JW, Jassal DS, Nickel N, Duhamel TA, et al. Intrauterine exposure to diabetes and risk of cardiovascular disease in adolescence and early adulthood: a population-based birth cohort study. CMAJ. 2020;192(39):E1104–13.
Yu Y, Arah OA, Liew Z, Cnattingius S, Olsen J, Sorensen HT, Qin G, Li J. Maternal diabetes during pregnancy and early onset of cardiovascular disease in offspring: population based cohort study with 40 years of follow-up. BMJ. 2019;367:l6398.
Leybovitz-Haleluya N, Wainstock T, Landau D, Sheiner E. Maternal gestational diabetes mellitus and the risk of subsequent pediatric cardiovascular diseases of the offspring: a population-based cohort study with up to 18 years of follow up. Acta Diabetol. 2018;55(10):1037–42.
Darmency-Stamboul V, Chantegret C, Ferdynus C, Mejean N, Durand C, Sagot P, Giroud M, Bejot Y, Gouyon JB. Antenatal factors associated with perinatal arterial ischemic stroke. Stroke. 2012;43(9):2307–12.
Ormazabal V, Nair S, Carrion F, McIntyre HD, Salomon C. The link between gestational diabetes and cardiovascular diseases: potential role of extracellular vesicles. Cardiovasc Diabetol. 2022;21(1):174.
Retnakaran R, Qi Y, Connelly PW, Sermer M, Hanley AJ, Zinman B. The graded relationship between glucose tolerance status in pregnancy and postpartum levels of low-density-lipoprotein cholesterol and apolipoprotein B in young women: implications for future cardiovascular risk. J Clin Endocrinol Metab. 2010;95(9):4345–53.
Li LJ, Tan KH, Aris IM, Man REK, Gan ATL, Chong YS, Saw SM, Gluckman P, Wong TY, Lamoureux E. Retinal vasculature and 5-year metabolic syndrome among women with gestational diabetes mellitus. Metabolism. 2018;83:216–24.
Retnakaran R, Qi Y, Connelly PW, Sermer M, Zinman B, Hanley AJ. Glucose intolerance in pregnancy and postpartum risk of metabolic syndrome in young women. J Clin Endocrinol Metab. 2010;95(2):670–7.
Adam S, McIntyre HD, Tsoi KY, Kapur A, Ma RC, Dias S, Okong P, Hod M, Poon LC, Smith GN, et al. Pregnancy as an opportunity to prevent type 2 diabetes mellitus: FIGO Best Practice advice. Int J Gynaecol Obstet. 2023;160(Suppl 1):56–67.
Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–9.
Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361.
Gunderson EP, Chiang V, Pletcher MJ, Jacobs DR, Quesenberry CP, Sidney S, Lewis CE. History of gestational diabetes mellitus and future risk of atherosclerosis in mid-life: the coronary artery risk development in young adults study. J Am Heart Assoc. 2014;3(2):e000490.
Weber T, Auer J, O’Rourke MF, Kvas E, Lassnig E, Berent R, Eber B. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation. 2004;109(2):184–9.
Caliskan M, Turan Y, Caliskan Z, Gullu H, Ciftci FC, Avci E, Duran C, Kostek O, Telci Caklili O, Koca H, et al. Previous gestational diabetes history is associated with impaired coronary flow reserve. Ann Med. 2015;47(7):615–23.
Anastasiou E, Lekakis JP, Alevizaki M, Papamichael CM, Megas J, Souvatzoglou A, Stamatelopoulos SF. Impaired endothelium-dependent vasodilatation in women with previous gestational diabetes. Diabetes Care. 1998;21(12):2111–5.
Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130(12):1003–8.
Kametas NA, McAuliffe F, Hancock J, Chambers J, Nicolaides KH. Maternal left ventricular mass and diastolic function during pregnancy. Ultrasound Obstet Gynecol. 2001;18(5):460–6.
Li S, Yang H. Relationship between advanced glycation end products and gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2019;32(17):2783–9.
Smith GC, Pell JP, Walsh D. Pregnancy complications and maternal risk of ischaemic heart disease: a retrospective cohort study of 129,290 births. Lancet. 2001;357(9273):2002–6.
Aguilera J, Semmler J, Coronel C, Georgiopoulos G, Simpson J, Nicolaides KH, Charakida M. Paired maternal and fetal cardiac functional measurements in women with gestational diabetes mellitus at 35–36 weeks’ gestation. Am J Obstet Gynecol. 2020;223(4):574. e571-574 e515.
Gasic S, Winzer C, Bayerle-Eder M, Roden A, Pacini G, Kautzky-Willer A. Impaired cardiac autonomic function in women with prior gestational diabetes mellitus. Eur J Clin Invest. 2007;37(1):42–7.
Lee H, Jang HC, Park HK, Cho NH. Early manifestation of cardiovascular disease risk factors in offspring of mothers with previous history of gestational diabetes mellitus. Diabetes Res Clin Pract. 2007;78(2):238–45.
Ehlers E, Talton OO, Schust DJ, Schulz LC. Placental structural abnormalities in gestational diabetes and when they develop: a scoping review. Placenta. 2021;116:58–66.
de Mendonca E, Fragoso MBT, de Oliveira JM, Xavier JA, Goulart MOF, de Oliveira ACM. (2022) Gestational diabetes mellitus: the crosslink among inflammation, nitroxidative stress, intestinal microbiota and alternative therapies. Antioxid (Basel) 11(1)
Yang X, Leng J, Liu H, Wang L, Li W, Li W, Yang X, Liu M, Hu G. Maternal gestational diabetes and childhood hyperlipidemia. Diabet Med. 2021;38(11):e14606.
Lu J, Zhang S, Li W, Leng J, Wang L, Liu H, Li W, Zhang C, Qi L, Tuomilehto J, et al. Maternal gestational diabetes is Associated with offspring’s hypertension. Am J Hypertens. 2019;32(4):335–42.
Tocantins C, Diniz MS, Grilo LF, Pereira SP. The birth of cardiac disease: mechanisms linking gestational diabetes mellitus and early onset of cardiovascular disease in offspring. WIREs Mech Dis. 2022;14(4):e1555.
Benagiano M, Mancuso S, Brosens JJ, Benagiano G. (2021) Long-term consequences of placental vascular pathology on the maternal and offspring cardiovascular systems. Biomolecules 11(11)
Paauw ND, Stegeman R, de Vroede M, Termote JUM, Freund MW, Breur J. Neonatal cardiac hypertrophy: the role of hyperinsulinism-a review of literature. Eur J Pediatr. 2020;179(1):39–50.
Agarwal P, Morriseau TS, Kereliuk SM, Doucette CA, Wicklow BA, Dolinsky VW. Maternal obesity, diabetes during pregnancy and epigenetic mechanisms that influence the developmental origins of cardiometabolic disease in the offspring. Crit Rev Clin Lab Sci. 2018;55(2):71–101.
Al-Biltagi M, El Razaky O, El Amrousy D. Cardiac changes in infants of diabetic mothers. World J Diabetes. 2021;12(8):1233–47.
Kolac UK, Kurek Eken M, Unubol M, Donmez Yalcin G, Yalcin A. The effect of gestational diabetes on the expression of mitochondrial fusion proteins in placental tissue. Placenta. 2021;115:106–14.
Zhao Q, Sun Q, Zhou L, Liu K, Jiao K. Complex regulation of mitochondrial function during Cardiac Development. J Am Heart Assoc. 2019;8(13):e012731.
Acknowledgements
The research of the authors is supported in part by the Yong Loo Lin School of Medicine, National University of Singapore, and the National University Hospital.
Author information
Authors and Affiliations
Contributions
L.-J.L. conceived the idea of the study; C.A., T.B. & L.-J.L. screened the studies and extracted the data; R.D. carried out the statistical analysis; L.-J.L. supervised the analysis. C.A., T.B. & L.-J.L. interpreted the findings and drafted the manuscript. C.Y.S., C.Z., K.A., and L.-J.L. edited and revised the manuscript. All authors critically revised and revised the manuscript for final submission. All authors have approved the final draft of the manuscript. L.-J.L. is guarantor. L.-J.L accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ashley Chen and Breanna Tan contributed equally to the first authorship.
Supplementary Information
12933_2024_2416_MOESM3_ESM.jpg
Supplementary Figure 3: Subgroup analysis stratified by study features. Evidence of risk ratio (RR) and 95% confidence interval (CI) of maternal GDM and maternal postpartum overall CVDs was reported in all subgroups, using unadjusted random-effects model. Heterogeneity was presented in both I2 (describing the percentage of variation across studies that is due to heterogeneity rather than chance) and T2 (reflecting the variance of the true effect sizes). Cochran's Q test is used to determine if there are differences of overall CVDs within subgroups or between subgroups. P value < 0.10 for Q-test is considered significant. Abbreviations: CI: confidence interval; GDM, gestational diabetes mellitus; CVDs, cardiovascular diseases; T2D, type 2 diabetes; NOSC, Newcastle-Ottawa Scale
12933_2024_2416_MOESM4_ESM.jpg
Supplementary Figure 4: Subgroup analysis stratified by covariates adjustment. Evidence of risk ratio (RR) and 95% confidence interval (CI) of maternal GDM and maternal postpartum overall CVDs was reported in all subgroups, using unadjusted random-effects model. Heterogeneity was presented in both I2 (describing the percentage of variation across studies that is due to heterogeneity rather than chance) and T2 (reflecting the variance of the true effect sizes). Cochran's Q test is used to determine if there are differences of overall CVDs within subgroups or between subgroups. P value < 0.10 for Q-test is considered significant. Abbreviations: CI, confidence interval; BMI, body mass index, HDP, hypertensive disorder during pregnancy; HTN, hypertension; T2D, type 2 diabetes
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, A., Tan, B., Du, R. et al. Gestational diabetes mellitus and development of intergenerational overall and subtypes of cardiovascular diseases: a systematic review and meta-analysis. Cardiovasc Diabetol 23, 320 (2024). https://doi.org/10.1186/s12933-024-02416-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02416-7