Abstract
Background
With increasing attention given to host-specific lipid metabolism status, it is of urgent need to identify lipid metabolism indices with predictive or prognostic value in locally advanced breast cancer patients treated with neoadjuvant chemotherapy (NAC), and to evaluate the performance improvement by incorporating them into the existing Neo-Bioscore staging system.
Methods
Patients from a prospectively maintained database of locally advanced breast cancer patients who received radical surgery after NAC between January 2014 to December 2020 were enrolled in this study. The enrolled patients were randomly divided into a training set and a test set at a ratio of 6:4. The random forest algorithm was applied to rank the importance of prognostic factors, top-ranked lipid metabolism indices of which were then incorporated into Neo-Bioscore to construct an updated prognostic model. The performances of these two models were compared in both training set and test set from multiple perspectives. Study outcomes included disease-free survival (DFS), relapse-free survival (RFS), distance-recurrence-free survival (DRFS), locoregional-recurrence-free survival (LRFS) and overall survival (OS).
Results
A total of 200 eligible patients were included in this study. After a median follow-up of 4.73 years, it was demonstrated that the relative increase in total cholesterol (TC; DFS: HR = 4.782, 95%CI 1.410 ~ 16.217, P = 0.012) and low-density lipoprotein (LDL; DFS: HR = 4.622, 95%CI 1.517 ~ 14.088, P = 0.007) during NAC led to poorer survival outcomes. Patients with either a higher body mass index (BMI) or elevated LDL during NAC had a worse prognosis (DFS: HR = 6.351, 95%CI 1.938 ~ 20.809, P = 0.002; OS, HR = 6.919, 95%CI 1.296 ~ 36.932, P = 0.024). Incorporating BMI and LDL fluctuations during NAC into Neo-Bioscore improved the prognostic stratification, especially in terms of LRFS (P = 0.046 vs. P = 0.65) and OS (P = 0.013 vs. P = 0.61). Multidimensional evaluation confirmed the improvement in model fit and clinical use for the updated model in both training set and test set.
Conclusions
This is the first study to illustrate the relative elevation of LDL and TC levels during NAC as independent prognosticators for locally advanced breast cancer. This is also the first attempt to incorporate lipid metabolism indices into the original Neo-Bioscore staging system, which further improves the prognostic stratification of patients receiving NAC.
Similar content being viewed by others
Background
Neoadjuvant chemotherapy (NAC) occupies an increasingly vital position in the whole-course management of breast cancer, which is due to its advantages in shrinking tumors, making down-staging possible, and eliminating micro-metastatic foci prior to surgery. NAC is capable of rendering inoperable patients amenable to curative surgery, thus increasing the likelihood of breast conserving surgery, and even improving the survival outcomes of patients [1, 2]. In addition, NAC provides a platform for the early evaluation of tumor sensitivity to certain cytotoxic agents in vivo, which offers considerable guidance for tailoring subsequent strategies. It is well known that achieving pathological complete response (pCR) signifies an improved long-term survival benefit [3]. To more precisely stratify the prognosis of breast cancer patients who underwent NAC, specific prognostic scoring systems have been established. The Neo-Bioscore staging system, which evolved from the CPS + EG staging system, encompasses pretreatment clinical stage, posttreatment pathological stage, and tumor biological markers (estrogen receptor [ER], human epidermal growth factor receptor 2 [HER2], and grade), and has been recognized as being an excellent algorithm for assessing the prognosis of patients treated with NAC [4]. However, Neo-Bioscore merely includes the intrinsic characteristics of the tumor, whereas the patient's own metabolic factors have gradually become valuable. Accordingly, it is worthwhile to investigate whether Neo-Bioscore can be further optimized by incorporating the host's characteristics of a specific internal microenvironment.
Previous studies have demonstrated that in certain types of cancers, a high-fat diet, obesity and hyperlipidemia are not only closely related to the tumor initiation and growth [5,6,7], but are also strongly associated with increased metastatic capacity [8,9,10]. These findings indicate that lipid metabolism plays a preponderant role in the occurrence and development of multiple cancers.
The process by which tumor cells constantly adjust metabolic patterns to facilitate reproduction and adapt to the tumor microenvironment (TME) is generally referred to as "metabolic reprogramming", which is a novel hallmark of cancer [11, 12]. Lipids, as one of the major sources of energy, indispensable components of biofilms, and signaling molecules required for intra- and extracellular transmission, are key ingredients in metabolic rewiring [13,14,15,16]. Studies have shown that "lipid metabolism reprogramming" has a bearing on proliferation, invasion, energy generation, plasma membrane remodeling, oncogenic signal propagation, and chemotherapy resistance [17]. In an effort to meet the demand of excessive lipids, tumor cells regulate specific enzymes to boost the endogenous synthesis of lipids while also taking up exogenous lipids from the TME and peripheral circulating blood [18]. Although "lipid metabolism reprogramming" in breast cancer has been intensively studied in terms of both endogenous synthesis and the TME, few reports have clarified the relationship between serum lipids and patient prognosis in breast cancer patients receiving NAC [19, 20].
On these premises, this study was performed to explore the correlation of serum lipid levels at baseline (pre-NAC) or before surgery (post-NAC) and their fluctuations during NAC with the efficacy and prognosis for breast cancer patients who received NAC. Moreover, this study aimed to identify lipid metabolism indices with predictive/prognostic value, and incorporated them into the Neo-Bioscore staging system to evaluate the reliability and feasibility of the updated model.
Methods
Patients
Patients were retrospectively recruited from a prospectively maintained database (NCT 05621564) who underwent radical surgery after NAC between January 2014 and December 2020 at the Department of Breast Surgery, Renji Hospital, School of Medicine, Shanghai Jiaotong University (Fig. 1). Patients were eligible if they were females aged 18 years or older with pathologically confirmed invasive breast cancer (T1 N1-3 or T2-4 N0-3, M0), available clinicopathological information and serum lipid level (at least pre-NAC and post-NAC) records. The key exclusion criteria included the administration of only endocrine therapy in the neoadjuvant setting, metastatic breast cancer and bilateral invasive breast cancer. This study was conducted in accordance with the Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK) statement [21] and the protocol was approved by the Independent Ethics Committee of Renji Hospital with approval number of LY2022-028-B.
Collection and processing of clinicopathological information
The clinicopathological information (including age, height, weight, menopausal status, pathological information, and clinical stage, among other information) of eligible breast cancer patients was prospectively collected at baseline (pre-NAC). Body mass index (BMI), which is one of the key indicators reflecting systemic lipid metabolism, was calculated as weight (kg) divided by the square of height (m). Hormone receptor status was considered to be positive if there were at least 1% positive tumor nuclei in the immunohistochemical (IHC) staining of either the ER or progesterone receptor (PR), and ER positivity was defined as at least 1% positive tumor nuclei in the IHC staining of the ER. In accordance with the 2018 recommendations of the American Society of Clinical Oncology/College of American Pathologists [22], HER2 was determined as positive for tumors of IHC 3 + or IHC 2 + with amplification by fluorescence in situ hybridization (FISH). Patients were followed up through outpatient visits or telephone interviews every 3 months in the first 2 years, every 6 months until the fifth year and then annually until death or any relapse.
Serum lipid levels
The serum lipid biomarker data, including triglyceride (TG), total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL) and non-high-density lipoprotein (NHDL) levels, were prospectively measured at baseline (pre-NAC) and before surgery (post-NAC). The fluctuation of serum lipids was obtained by subtracting the baseline serum lipid level (pre-NAC) from the preoperative serum lipid level (post-NAC).
Data separation and cross-validation
The enrolled patients were randomly divided into a training set and a test set at a ratio of 6:4. The test set was isolated for the final test for the prognostic models. For the training set, serum lipids with predictive and prognostic value were identified and K-fold cross validation was utilized based on Cox regression, wherein the training group (two-thirds of the training set) and validation group (one-third of the training set) were randomly generated, and the process was repeated 5 times to ensure the fitting degree of the original Neo-Bioscore model and the updated model.
Identification and incorporation of lipid metabolism indices
Random forest algorithm (ggRandomForests R package v2.2.1) was applied to rank the importance of prognostic factors in the Neo-Bioscore staging system (clinical stage, pathological stage, ER status, HER2 status and histological grade) as well as lipid metabolism indices (BMI, TG, TC, HDL, LDL, and NHDL) through the variable importance (VIMP) method and minimum depth method in the training set for estimating disease-free survival (DFS) and relapse-free survival (RFS). The top-ranked markers were then merged into the Neo-Bioscore staging system to construct an updated prognostic model (Neo-Bioscore + Lipid Metabolism).
Performance evaluation of prognostic models
The performances of the original model (Neo-Bioscore) and the updated model (Neo-Bioscore + Lipid Metabolism) were compared with those of multidimensional methods, including time-dependent receiver operating characteristic (ROC) curves and their area under the curve (AUC), decision curve analysis (DCA), the Akaike information criterion (AIC), the C-index, and Integrated Discrimination Improvement (IDI).
Validation with an external database
A detailed gene set (HP_INCREASED_LDL_CHOLESTEROL_CONCENTRATION) related to increased serum lipid concentrations was identified via Gene Set Enrichment Analysis (GSEA) (http://www.gsea-msigdb.org/gsea/msigdb/index.jsp). Afterwards, Kaplan–Meier plotter [Breast Cancer] (http://kmplot.com/analysis/index.php) was applied to verify the relationship between the expression of these genes and the prognosis of breast cancer patients.
Statistical analysis
The study outcomes were pCR, DFS, RFS, distance-recurrence-free survival (DRFS), locoregional-recurrence-free survival (LRFS) and overall survival (OS). Specifically, pCR was referred to as ypT0 ypN0; DFS was defined as the time from surgery to the first occurrence of local recurrence, regional recurrence, distant recurrence, second primary cancer, or death from any cause, and RFS was defined as the time from surgery to the first occurrence of local recurrence, regional recurrence, distant recurrence, or death from any cause. Similarly, the definition of DRFS is the period from surgery to the first occurrence of distant recurrence, and death from any cause, whereas the definition of LRFS is the period from surgery to the first occurrence of local recurrence, regional recurrence, and death from any cause. OS denoted the interval from surgery to death from any cause.
Continuous variables were compared by using t tests or Wilcoxon tests where appropriate. Categorical variables were compared by applying the chi-square or the Yates correction where appropriate. Correlations between variables are presented in the form of heatmaps. The best cutoffs of BMI and serum lipids were determined by using maximally selected rank statistics via the surv_cutpoint function in the survminer R package (v0.4.9). The associations between various factors and pCR were tested by using logistic regression. Kaplan–Meier analysis was performed to estimate survival outcomes, and survival differences between the groups were evaluated by using the log-rank test. Furthermore, a multivariate Cox proportional hazards regression model was used to estimate the hazard ratio (HR) and 95% confidence intervals (CIs). Adjustment factors for multivariate logistic and multivariate Cox regression analysis included ER status (positive vs. negative), HER2 status (positive vs. negative), Ki-67 level (> 30% vs. ≤ 30%) and clinical stage (II stage vs. III stage). Cox-based nomogram plots were used to show the contribution of each influencing factor in the model to survival outcomes. All of the statistical tests were two-sided, with P < 0.05 indicating statistical significance. The analyses were carried out in the R programming language (v4.2.2).
Results
Baseline clinicopathological characteristics
A total of 200 eligible patients were included in this study. The median age was 52 years (range 25 ~ 71 years) and most of the tumors were luminal-like (n = 154, 77%). Patients with a high BMI (BMI > 25 kg/m2) accounted for 22.5% of the overall population. The vast majority of the patients had cT2-4 (n = 198, 99.0%) or cN1-3 (n = 168, 84.0%) tumors. The correlations between clinicopathological parameters and serum lipid levels were detailed in Fig. 2. The entire study population was randomly divided into a training set and a test set in a 6:4 ratio, which presented a well-balanced distribution of clinicopathological features in general (Table 1; Supplementary Table S1). As of March 31, 2023, 11 patients had died, 24 experienced DFS events and 20 experienced RFS events after a median follow-up of 4.73 years (range 1.68 ~ 7.06 years). The specific numbers of events for different outcomes in the training set and the test set were described in detail in Supplementary Table S2.
Correlation heatmap of clinicopathological parameters and serum lipid levels (pre-NAC, post-NAC and changes during NAC)
Abbreviations: BMI, body mass index; ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; TG, triglyceride; TC, total cholesterol; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NHDL, non-high-density lipoprotein; pre, pre-neoadjuvant chemotherapy; post, post-neoadjuvant chemotherapy
Correlation of serum lipid levels with pCR in the training set
With regard to baseline (pre-NAC) and preoperative (post-NAC) serum lipid levels, higher TC at baseline was found to be significantly correlated with a higher pCR rate in both univariate (OR = 2.879, 95%CI 1.073 ~ 7.720, P = 0.036) and multivariate analyses (OR = 3.033, 95%CI 1.031 ~ 8.923, P = 0.044; Supplementary Table S3). On the other hand, the relative increase in TC during NAC was associated with a lower rate of pCR (OR = 0.248, 95%CI 0.087 ~ 0.708, P = 0.009). Besides, the change in TC during NAC remained to be an independent predictor of pCR after multivariate adjustment (OR = 0.300, 95%CI 0.098 ~ 0.916, P = 0.035; Supplementary Table S4).
Correlation of serum lipid levels with prognosis in the training set
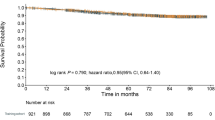
Although pre-NAC (Supplementary Figure S1) and post-NAC (Supplementary Figure S2) lipid levels were not significantly correlated with either DFS or RFS in the training set, a potential connection was discerned between the changes in lipid levels during NAC and various survival outcomes. Wherein, the Kaplan–Meier curves indicated that a relative increase in LDL led to significantly poorer DFS (P < 0.01; Fig. 3A), RFS (P = 0.01; Fig. 3B), DRFS (P = 0.01; Fig. 3C), and LRFS (P < 0.01; Fig. 3D). Additionally, the relative increase in TC (DFS: P < 0.01; Supplementary Fig. 3B) during the neoadjuvant period was significantly related to a worse prognosis.
Kaplan–Meier curves for various survival outcomes by LDL changes during neoadjuvant chemotherapy in training set
Kaplan–Meier estimates of LDL changes on (A) DFS, (B) RFS, (C) DRFS and (D) LRFS
Abbreviations: DFS, disease-free survival; RFS, relapse-free survival; DRFS, distance-recurrence-free survival; LRFS, locoregional-recurrence-free survival; LDL, low-density lipoprotein
Multivariate Cox regression analysis revealed the detrimental impact of relatively increasing TC (HR = 4.782, 95%CI 1.410 ~ 16.217, P = 0.012) and LDL (HR = 4.622, 95%CI 1.517 ~ 14.088, P = 0.007) on DFS (Table 2).
Identification of lipid metabolism indices with prognostic value
The importance of lipid metabolism indices was sorted by random survival forest in the training set, which indicated that BMI and LDL changes were invariable in the top rank in terms of predicting both DFS (Fig. 4A) and RFS (Fig. 4B). Kaplan–Meier curves further revealed that patients with either a high BMI or elevated LDL during NAC had inferior DFS (P = 0.0011; Fig. 4C), RFS (P = 0.0011; Fig. 4D), DRFS (P = 0.0011; Fig. 4E), LRFS (P = 0.0099; Fig. 4F) and OS (P = 0.026; Fig. 4G). After multivariate adjustment, the unfavorable effect of higher BMI or elevated LDL on prognosis remained significant (DFS: HR = 6.351, 95%CI 1.938 ~ 20.809, P = 0.002; RFS: HR = 7.743, 95%CI 2.038 ~ 29.421, P = 0.003; DRFS: HR = 7.730, 95%CI 2.034 ~ 29.370, P = 0.003; LRFS: HR = 9.965, 95%CI 1.909 ~ 52.015, P = 0.006; OS: HR = 6.919, 95%CI 1.296 ~ 36.932, P = 0.024).
Identification of lipid metabolism indices with prognostic value in training set
Random Forest applied to rank the importance of variables in accordance with efficiency in predicting (A) DFS and (B) RFS. Kaplan–Meier estimates of BMI and LDL changes on (C) DFS; (D) RFS; (E) DRFS; (F) LRFS; (G) OS
Note: As for Fig. 4A & B, the horizontal axis is the importance ranking based on the VIMP method, with decreasing importance from left to right. VIMP < 0 (red points) indicates that the variable reduces the predictive accuracy, while VIMP > 0 (blue points) indicates that the variable improves the predictive accuracy. The vertical axis is used to sort the variable importance through minimal depth method, and the importance decreases from bottom to top. The closer it is to the bottom left corner, the higher ranking of the variable in both screening methods
Abbreviations: DFS, disease-free survival; RFS, relapse-free survival; DRFS, distance-recurrence-free survival; LRFS, locoregional-recurrence-free survival; OS, overall survival; BMI, body mass index; Cscore, Clinical staging score in Neo-Bioscore; Pscore, Pathological staging score in Neo-Bioscore; ERscore, ER status score in Neo-Bioscore; Hscore, HER2 status score in Neo-Bioscore; Gscore, grade score in Neo-Bioscore; VIMP, variable importance
Optimization of prognostic model
BMI and LDL fluctuations during NAC were incorporated into Neo-Bioscore as a representative indicators of lipid metabolism. For patients with a higher BMI or elevated LDL during NAC, an extra one point was added on the basis of the original Neo-Bioscore staging system (Table 3). The nomograms of the updated model (Neo-Bioscore + Lipid Metabolism) in the training set for DFS (Fig. 5A) and RFS (Fig. 5B) indicated that clinical stage, pathological stage and lipid metabolism index were the three most significant factors affecting the prognosis of patients receiving NAC. Besides, the updated model was more capable of stratifying patient prognosis than was Neo-Bioscore (Fig. 6), especially in terms of LRFS (P = 0.046 vs. P = 0.65, respectively; Fig. 6D, I) and OS (P = 0.013 vs. P = 0.61, respectively; Fig. 6E, J).
Prognostic stratification ability of the Neo-Bioscore and the updated model in training set
Prognostic stratification of DFS (A, F), RFS (B, G), DRFS (C, H), LRFS (D, I), and OS (E, J) based on the updated model (A ~ E) and the Neo-Bioscore (F ~ J) in the training set. No patients scored 8 in updated model
Abbreviations: DFS, disease-free survival; RFS, relapse-free survival; DRFS, distance-recurrence-free survival; LRFS, locoregional-recurrence-free survival; OS, overall survival
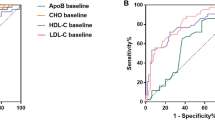
Performance comparison between the Neo-Bioscore and the updated model in the training set and test set
In the training set, the time-dependent ROC curves of the updated model (red series) were always greater than those of Neo-Bioscore (blue series). Regardless of the analysis time, the AUC of the updated model was greater than that of Neo-Bioscore in terms of both DFS (Fig. 7A) and RFS (Fig. 7B), thus indicating that the sensitivity and specificity of the updated model were superior to those of the original model. Furthermore, threefold 5-times cross validation was carried out in the training set (Table 4), which verified the superiority of the performance of the updated model to that of Neo-Bioscore. A similar conclusion was obtained in the test set (Fig. 7C, 7D). The DCA also displayed an improvement in the clinical net benefit of the updated model in both training set and test set (Fig. 8). After incorporating the lipid metabolism index into Neo-Bioscore, the AIC value in the training set decreased (DFS: 128.96 to 125.06; RFS: 109.94 to 105.79; Table 5), and the C-index significantly increased (DFS: 0.644 to 0.749, P = 0.001; RFS: 0.680 to 0.790, P = 0.003; Table 5). Moreover, the IDI significantly improved the predictive ability of the updated model. In addition, similar conclusions were drawn when the AIC, C-index and IDI of the two models were compared in the test set (Table 5).
Time-dependent ROC curves and AUC in training set and test set
Time-dependent ROC comparison between Neo-Bioscore (blue series) and updated model (red series) in the training set (A, B) and AUC comparison in the test set (C, D) in terms of DFS (A, C) and RFS (B, D)
Abbreviations: ROC, receiver operating characteristic; AUC, area under curve; DFS, disease-free survival; RFS, relapse-free survival
Decision Curve Analysis of Neo-Bioscore and the updated model in training set and test set
Decision Curve Analysis of 3-year DFS (A, F), 3-year RFS (B, G), 3-year DRFS (C, H), 3-year LRFS (D, I) and 3-year OS (E, J) in the training set (A ~ E) and the test set (F ~ J)
Abbreviations: DFS, disease-free survival; RFS, relapse-free survival; DRFS, distance-recurrence-free survival; LRFS, locoregional-recurrence-free survival; OS, overall survival
Validation with an external database
According to the GSEA database, a total of 31 genes (such as CYP7A1, TTPA, SLC7A7, FHL1, SYNE1, and LMNA etc.) related to the increase in LDL concentration in the circulating blood were identified. Analysis using the Kaplan–Meier Plotter database showed that the overexpression of these genes implied a worse RFS in breast cancer patients who received NAC (Fig. 9, also see supplementary Figure S4).
Discussion
This is the first study to elucidate the influence of serum lipid fluctuations during NAC on the prognosis of patients with locally advanced breast cancer. Beyond that, this was the very first attempt to integrate the lipid metabolism index into Neo-Bioscore. The combination of local and systemic factors as well as tumor and host characteristics could stratify the prognosis of these patients more accurately.
This study first demonstrated that the relative increases in TC and LDL during the neoadjuvant period were independent prognostic risk factors for breast cancer patients, which indicated that changes in serum lipids, which were reportedly unfavorable to the cardiovascular system [23], also have a detrimental impact on survival outcomes in patients with breast cancer. However, the underlying mechanism is still open to investigation. This analysis of data from external database showed that several genes related to elevated circulating LDL were associated with prognosis. In addition, Nelson and colleagues reported that 27-hydroxycholesterol (27HC), the main metabolite of cholesterol, increased ER dependent tumor growth and enhanced liver X receptor (LXR) dependent metastasis in mouse models of breast cancer [24]. It was demonstrated subsequently that 27HC acted on immune myeloid cells at distal metastatic sites to create an immunosuppressive environment and helped to select cells that are resistant to ferroptosis, thus facilitating tumorigenicity and metastasis [25, 26]. These previous studies and the present external validation at least partially or indirectly supported the findings of this study from the front side. Conversely, the utilization of cholesterol-lowering drugs during endocrine therapy improved multiple survival outcomes, such as DFS, breast cancer free intervals, and distant recurrence free intervals, in patients with hormone receptor-positive breast cancer in the BIG1-98 trial [27], which partially supported the findings of this study from the reverse side.
The change in LDL level ranked first in terms of variable importance according to random forest algorithms. Several studies have shown that de novo lipogenesis increases the intracullular amounts of saturated and mono-unsaturated phospholipids intracellularly, thus resulting in a relative decrease in polyunsaturated acyl chains, which are susceptible to peroxidation, thereby protecting cells from cell death induced by reactive oxygen species (ROS)-related lipid peroxidation [28, 29]. Interestingly, LDL can also block these unfavorable polyunsaturated fatty acids in tumor cells [18], which may explain why increased LDL can act as a prognostic factor. Another promising prognosticator that is relevant to lipid metabolism is BMI, a variable that has been identified due to its high-ranking importance in the random survival forest. It is generally accepted that higher BMI is associated with the progression of multiple cancers [30, 31]. A retrospective meta-analysis revealed that increased BMI was linked to a greater risk of breast cancer, and the correlation was more intense in the Asia–Pacific population [6]. Moreover, several studies have demonstrated that breast cancer patients with overweight BMI turned out to have worse survival outcomes [32,33,34,35]. Compared with lipidomic analysis, BMI and serum LDL levels are readily available and highly feasible in clinical practice. The combination of the two parameters may provide a more comprehensive picture of lipid metabolism in vivo, which was successfully corroborated as a prognosticator for breast cancer patients undergoing NAC in this study.
Nowadays, metabolic reprogramming has been considered as one of the conspicuous hallmarks of cancer [12], especially regarding rewired lipid metabolism, which is the most prominent metabolic alteration in cancer [14]. Cancer cells are overdependent on fatty acids and cholesterol for rapid proliferation, division, invasion, metastasis, and membrane remodeling [13, 36, 37]. Moreover, lipid metabolism reprogramming also plays a crucial role in chemotherapy resistance and tumor immunology [17, 18]. Findings in this study illustrated better prognostic stratification of the updated prognostic model with the incorporation of the lipid metabolism index into Neo-Bioscore. After multidimensional assessment in both training and test sets, the updated model, which merged both intrinsic tumor characteristics and the host-specific lipid metabolism index, had superior predictive performance and clinical application. These data reinforced the prognostic significance of metabolic profiles in patients receiving NAC.
Study strengths and limitations
The strength of this study lied in its originality and close relevance to clinical practice. Firstly, the updated model might serve as a conceptual paradigm to combine tumor characteristics and host metabolic profiles to assess the prognosis of breast cancer patients treated with NAC. Secondly, compared to other detection methods such as lipidomics, it is much easier and less costly to monitor serum lipids in the whole-course management of these patients.
This study had several limitations. Firstly, as a retrospective study based on prospective cohorts, the use of lipid-modifying medications during treatment is likely somewhat underestimated. Despite the fact that lipid levels at a certain time point may be affected by lipid-modifying drugs, this research explored the relationship between lipid fluctuations during the neoadjuvant period and prognosis to minimize the impact of specific individual differences on the results. Secondly, both the sample size and follow-up interval were not sufficient. However, this is an exploratory analysis for hypothesis generation based on a prospective cohort. A prospective study with a larger sample size and longer follow-up period is warranted for further verification.
Conclusion
In conclusion, this study has not only identified a novel and reliable index of lipid metabolism as a prognostic indicator but also further optimized the prognostic stratification model by incorporating such an index for patients receiving NAC. The results of this study suggest that the medical staff should attach more importance to the management of serum lipids during neoadjuvant treatment. The findings of this study also lay a solid foundation for future in-depth explorations of lipid metabolism as an effective therapeutic target, thus providing new insights into the impact of host-specific factors on survival outcomes.
Availability of data and materials
Data described in the manuscript will be made available upon reasonable request.
Abbreviations
- NAC:
-
Neoadjuvant chemotherapy
- DFS:
-
Disease-free survival
- RFS:
-
Relapse-free survival
- DRFS:
-
Distance-recurrence-free survival
- LRFS:
-
Locoregional-recurrence-free survival
- OS:
-
Overall survival
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- NHDL:
-
Non-high-density lipoprotein
- BMI:
-
Body mass index
- pCR:
-
Pathological complete response
- TME:
-
Tumor microenvironment
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under curve
- DCA:
-
Decision curve analysis
- AIC:
-
Akaike information criterion
- IDI:
-
Integrated Discrimination Improvement
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
References
Heil J, Kuerer HM, Pfob A, Rauch G, Sinn HP, Golatta M, Liefers GJ, Vrancken Peeters MJ. Eliminating the breast cancer surgery paradigm after neoadjuvant systemic therapy: current evidence and future challenges. Ann Oncol. 2020;31:61–71.
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12:335–43.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Mittendorf EA, Vila J, Tucker SL, Chavez-MacGregor M, Smith BD, Symmans WF, Sahin AA, Hortobagyi GN, Hunt KK. The neo-bioscore update for staging breast cancer treated with neoadjuvant chemotherapy: incorporation of prognostic biologic factors into staging after treatment. JAMA Oncol. 2016;2:929–36.
Gallagher EJ, LeRoith D. Obesity and diabetes: the increased risk of cancer and cancer-related mortality. Physiol Rev. 2015;95:727–48.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78.
Neuhouser ML, Aragaki AK, Prentice RL, Manson JE, Chlebowski R, Carty CL, Ochs-Balcom HM, Thomson CA, Caan BJ, Tinker LF, et al. Overweight, obesity, and postmenopausal invasive breast cancer risk: a secondary analysis of the women’s health initiative randomized clinical trials. JAMA Oncol. 2015;1:611–21.
Martin-Perez M, Urdiroz-Urricelqui U, Bigas C, Benitah SA. The role of lipids in cancer progression and metastasis. Cell Metab. 2022;34:1675–99.
Ghahremanfard F, Mirmohammadkhani M, Shahnazari B, Gholami G, Mehdizadeh J. The valuable role of measuring serum lipid profile in cancer progression. Oman Med J. 2015;30:353–7.
Emaus A, Veierød MB, Tretli S, Finstad SE, Selmer R, Furberg AS, Bernstein L, Schlichting E, Thune I. Metabolic profile, physical activity, and mortality in breast cancer patients. Breast Cancer Res Treat. 2010;121:651–60.
Faubert B, Solmonson A, DeBerardinis RJ: Metabolic reprogramming and cancer progression. Science. 2020, 368.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Broadfield LA, Pane AA, Talebi A, Swinnen JV, Fendt S-M. Lipid metabolism in cancer: new perspectives and emerging mechanisms. Dev Cell. 2021;56:1363–93.
Snaebjornsson MT, Janaki-Raman S, Schulze A. Greasing the wheels of the cancer machine: the role of lipid metabolism in cancer. Cell Metab. 2020;31:62–76.
Cheng C, Geng F, Cheng X, Guo D. Lipid metabolism reprogramming and its potential targets in cancer. Cancer Commun (Lond). 2018;38:27.
Bian X, Liu R, Meng Y, Xing D, Xu D, Lu Z: Lipid metabolism and cancer. J Exp Med. 2021, 218.
Vasseur S, Guillaumond F. Lipids in cancer: a global view of the contribution of lipid pathways to metastatic formation and treatment resistance. Oncogenesis. 2022;11:46.
Butler LM, Perone Y, Dehairs J, Lupien LE, de Laat V, Talebi A, Loda M, Kinlaw WB, Swinnen JV. Lipids and cancer: emerging roles in pathogenesis, diagnosis and therapeutic intervention. Adv Drug Deliv Rev. 2020;159:245–93.
Cedó L, Reddy ST, Mato E, Blanco-Vaca F, Escolà-Gil JC: HDL and LDL: Potential New Players in Breast Cancer Development. J Clin Med. 2019, 8.
Luo J, Yang H, Song B-L. Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol. 2020;21:225–45.
Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting recommendations for tumor marker prognostic studies (REMARK): explanation and elaboration. PLoS Med. 2012;9:e1001216.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, Bilous M, Ellis IO, Fitzgibbons P, Hanna W, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American pathologists clinical practice guideline focused update. J Clin Oncol. 2018;36:2105–22.
O’Donoghue ML, Giugliano RP, Wiviott SD, Atar D, Keech A, Kuder JF, Im K, Murphy SA, Flores-Arredondo JH, López JAG, et al. Long-term evolocumab in patients with established atherosclerotic cardiovascular disease. Circulation. 2022;146:1109–19.
Nelson ER, Wardell SE, Jasper JS, Park S, Suchindran S, Howe MK, Carver NJ, Pillai RV, Sullivan PM, Sondhi V, et al. 27-Hydroxycholesterol links hypercholesterolemia and breast cancer pathophysiology. Science. 2013;342:1094–8.
Baek AE, Yu Y-RA, He S, Wardell SE, Chang C-Y, Kwon S, Pillai RV, McDowell HB, Thompson JW, Dubois LG, et al: The cholesterol metabolite 27 hydroxycholesterol facilitates breast cancer metastasis through its actions on immune cells. Nat Commun. 2017, 8:864.
Liu W, Chakraborty B, Safi R, Kazmin D, Chang C-Y, McDonnell DP. Dysregulated cholesterol homeostasis results in resistance to ferroptosis increasing tumorigenicity and metastasis in cancer. Nat Commun. 2021;12:5103.
Borgquist S, Giobbie-Hurder A, Ahern TP, Garber JE, Colleoni M, Láng I, Debled M, Ejlertsen B, von Moos R, Smith I, et al. Cholesterol, Cholesterol-Lowering Medication Use, and Breast Cancer Outcome in the BIG 1–98 Study. J Clin Oncol. 2017;35:1179–88.
Rysman E, Brusselmans K, Scheys K, Timmermans L, Derua R, Munck S, Van Veldhoven PP, Waltregny D, Daniëls VW, Machiels J, et al. De novo lipogenesis protects cancer cells from free radicals and chemotherapeutics by promoting membrane lipid saturation. Cancer Res. 2010;70:8117–26.
Xie Y, Wang B, Zhao Y, Tao Z, Wang Y, Chen G, Hu X. Mammary adipocytes protect triple-negative breast cancer cells from ferroptosis. J Hematol Oncol. 2022;15:72.
Recalde M, Davila-Batista V, Díaz Y, Leitzmann M, Romieu I, Freisling H, Duarte-Salles T. Body mass index and waist circumference in relation to the risk of 26 types of cancer: a prospective cohort study of 3.5 million adults in Spain. BMC Med. 2021;19:10.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer-viewpoint of the IARC working group. N Engl J Med. 2016;375:794–8.
Caan BJ, Kwan ML, Hartzell G, Castillo A, Slattery ML, Sternfeld B, Weltzien E. Pre-diagnosis body mass index, post-diagnosis weight change, and prognosis among women with early stage breast cancer. Cancer Causes Control. 2008;19:1319–28.
Mazzarella L, Disalvatore D, Bagnardi V, Rotmensz N, Galbiati D, Caputo S, Curigliano G, Pelicci PG. Obesity increases the incidence of distant metastases in oestrogen receptor-negative human epidermal growth factor receptor 2-positive breast cancer patients. Eur J Cancer. 2013;49:3588–97.
Ligorio F, Zambelli L, Bottiglieri A, Castagnoli L, Zattarin E, Lobefaro R, Ottini A, Vingiani A, Pupa SM, Bianchi GV, et al. Hormone receptor status influences the impact of body mass index and hyperglycemia on the risk of tumor relapse in early-stage HER2-positive breast cancer patients. Ther Adv Med Oncol. 2021;13:17588359211006960.
Kohls M, Freisling H, Charvat H, Soerjomataram I, Viallon V, Davila-Batista V, Kaaks R, Turzanski-Fortner R, Aleksandrova K, Schulze MB, et al. Impact of cumulative body mass index and cardiometabolic diseases on survival among patients with colorectal and breast cancer: a multi-centre cohort study. BMC Cancer. 2022;22:546.
Wang YY, Attané C, Milhas D, Dirat B, Dauvillier S, Guerard A, Gilhodes J, Lazar I, Alet N, Laurent V, et al. Mammary adipocytes stimulate breast cancer invasion through metabolic remodeling of tumor cells. JCI Insight. 2017;2:e87489.
Choi J, Cha YJ, Koo JS. Adipocyte biology in breast cancer: from silent bystander to active facilitator. Prog Lipid Res. 2018;69:11–20.
Acknowledgements
The authors appreciate all the patients involved in this study.
Funding
This study was funded by National Natural Science Foundation of China (No. 82173115 and 82103695), Science and Technology Commission of Shanghai Municipality (No. 20DZ2201600), Shanghai Municipal Key Clinical Specialty, Shanghai Rising-Star Program (No. 22QC1400200), Innovative Research Team of High-level Local Universities in Shanghai (SHSMU-ZLCX20212601), Shanghai Municipal Health Commission Health Industry Clinical Research Special Project (No. 202340085) and Nurturing Fund of Renji Hospital (No. PYIII20-09 and RJPY-LX-002).
Author information
Authors and Affiliations
Contributions
X.C. wrote the original draft of the manuscript. X.C. and Y.Z.: Data curation, formal analysis, investigation, methodology, software and visualisation. Y.Z., Y.W. and W.Y.: Data curation and Validation. S.X., L.Z., Y.L. and Y.Y.: Investigation and project administration. J.L. and W.Y.: Conceptualisation. Y.W., J.L. and W.Y.: Funding acquisition, supervision and writing-review and editing. X.C. and Y.Z. contributed equally to this manuscript. All authors contributed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with REMARK statement and the protocol was approved by the Independent Ethics Committee of Renji Hospital (Approval number: LY2022-028-B).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, X., Zhao, Y., Wang, Y. et al. Fluctuations in serum lipid levels during neoadjuvant treatment as novel predictive and prognostic biomarkers for locally advanced breast cancer: a retrospective analysis based on a prospective cohort. Lipids Health Dis 23, 261 (2024). https://doi.org/10.1186/s12944-024-02140-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02140-x