Abstract
Background
Insulin resistance (IR) and serum uric acid (SUA) are closely interconnected: SUA contributes to adversely affects the insulin signaling pathway and contributes to IR, while IR is a known predictor for the development of hyperuricemia. The triglyceride (TG) to high-density lipoprotein cholesterol (HDL-C) ratio has been proposed as an easily obtainable marker for IR. This research aimed to investigate the interaction between IR and glomerular filtration rate (GFR)-adjusted uricemia (SUA/GFR ratio) in determining CV risk in a large population cohort study.
Methods
Data from 18,694 subjects were analyzed from Uric acid Right foR heArt Healt (URRAH) database. The study evaluated the association between TG/HDL-C ratio and SUA/GFR ratio, as well as their impact on the development of outcomes during the follow-up study period. The primary endpoint was CV mortality.
Results
After a mean follow-up of 124 ± 64 months, 2,665 (14.2%) CV deaths occurred. The incidence of fatal and non-fatal CV events increased in parallel with the increase of TG/HDL-C quintiles. TG/HDL-C ratio showed a positive association with increasing of SUA/GFR ratio, even in non-diabetic patients. Multivariate analysis showed that the TG/HDL-C ratio increases the mortality risk even after adjustment for potential confounding factors. Finally, IR and GFR-adjusted hyperuricemia showed an additive effect on CV mortality.
Conclusions
Both IR and SUA/GFR ratio independently predict CV mortality, regardless of age, gender, BMI, diabetes, hypertension and statin use. The joint effect of the TG/HDL-C ratio and the elevated SUA/GFR ratio was greater than the presence of each single risk factor on CV mortality. This highlights the importance of monitoring these markers to better assess cardiovascular risk.
Similar content being viewed by others
Introduction
Insulin resistance (IR), a state of systemic insulin sensitivity decline, is a key mechanism of lipid metabolism disorders. Accordingly, an abnormal lipid profile is an essential characteristic of patients with metabolic syndrome (MS), a condition strongly associated with the development of both type 2 diabetes and cardiovascular (CV) disease [1]. Hyperuricemia is also strongly associated with MS [2, 3], as well as with kidney disease progression, non-alcoholic fatty liver disease (NAFLD), hypertension, CV disease and mortality risk [4,5,6,7]. Moreover, IR and hyperuricemia are interconnected: serum uric acid (SUA) contributes to adversely affecting the insulin signaling pathway, while IR predicts the development of hyperuricemia [8,9,10]. The role of SUA in metabolic syndrome and its pleiotropic effects in multiple organ systems has been a matter of discussion due to its complex effects on cellular metabolism and signaling pathways [11, 12]. Some authors have proposed hyperuricemia as a component of MS, but little is known about its prognostic role in this contest.
Kidney function impairment plays a role in both IR and hyperuricemia, strongly conditioning the CV risk stratification. Chronic kidney disease (CKD) predisposes individuals to the development both of hyperuricemia [13] by reducing renal excretion of SUA, and to IR, secondary to chronic inflammation, oxidative stress, vitamin D deficiency, metabolic acidosis, anemia, and adipokine derangement which typically characterize CKD patients [14]. On the other side, IR promotes kidney disease [15] by several mechanisms, including worsening renal hemodynamics. Patients with MS have microvascular disease characterized by microalbuminuria, decreased glomerular filtration rate, tubular atrophy, interstitial fibrosis, and glomerulosclerosis [16]. IR causes endothelial dysfunction and generation of oxidative stress, which contributes to the deterioration of kidney function [17, 18]. This complex interplay between SUA, IR, and kidney function strongly impacts on CV mortality.
While the definition of MS is based on standard clinical and laboratory criterions, the definition of the IR in clinical practice is challenging. While hyperinsulinemic euglycemic clamp (HEC) is the gold standard for the assessment of IR, due to its complexity, this test is only used in small-scale research and not for population studies. Homeostasis model assessment of insulin resistance (HOMA-IR) requires an assessment of insulin levels, which is not practical in clinical practice in the community. Triglyceride/high-density lipoprotein (HDL) cholesterol ratio (TG/HDL-C) has been proposed as surrogate markers for predicting MS [18] and it has been proved to be a reliable sign for IR, endothelial dysfunction and preclinical organ damage [19,20,21]. In the clinical scenario, the TG/HDL-C has been estimated to be an adequate tool for IR assessment [22,23,24].
The Working Group on SUA and cardiovascular risk of the Italian Society of Hypertension had devised and set up the URRAH project (Uric Acid Right for Heart Health) to study the relationship between SUA and CVD [25]. Using this extensive, prognostic registry, the role of SUA levels in improving further risk stratification of patients with MS was investigated, demonstrating mild hyperuricemia significantly associated with an increased risk of CV mortality (CVM) in patients with MS, independently from other conventional CV risk factors [26]. In a recent sub-analysis of URRAH database, triglyceride-glucose index (TyG) thresholds are shown to be predictive of an increased risk of mortality, showing as several components of MS independently contribute to the risk of mortality [27,28,29].
Given that CV risk constitutes by far the leading cause of morbidity and mortality worldwide, it has become essential to investigate the role played by each key player in this context to reduce the heavy burden of global risk. The aim of this research was to explore the extent of interaction between IR and SUA/GFR ratio in determining CV mortality risk in a large population cohort study.
Methods
Database and study protocol
The URRAH project is a multicenter retrospective observational cohort study collecting data obtained from subjects aged 18 to 95 years. Participants are recruited within the epidemiological network of the Italian Society of Hypertension and include representation from almost all regions in Italy. The study protocol has been previously described in detail [23, 30].
For all subjects, a standardized set of items was recorded, including demographics, metabolic parameters, smoking habit, systolic and diastolic blood pressure (BP), renal function, history of CV, renal and cerebrovascular disease, concomitant treatments and outcome.
Kidney function was assessed by serum creatinine and GFR was estimated for each person using a standardized serum creatinine assay and the Chronic Kidney Disease Epidemiology Collaboration formula [24, 31].
Study outcomes included CV mortality as primary outcome and non-fatal events due to acute myocardial infarction, heart failure, or stroke as secondary outcomes. Diagnosis of events was obtained from hospital records or death certificates.
Ethics
The study data were collected either routinely or specifically for authorized studies. Participants did not undergo any additional tests or interventions, and their care or outcomes were not affected. The URRAH was performed according to the Declaration of Helsinki for Human Research (41stWorld Medical Assembly, 1990). The processing of the patients’ personal data collected in this study complies with the European Directive on the Privacy of Data. All data to be collected, stored and processed are anonymized, and all study related documents are retained in a secure location. Personal information is not stored on individual local computers. Approval was sought from the Ethical Committee of the coordinating center at the Division of Internal Medicine of the University of Bologna (No. 77/2018/Oss/AOUBo). Informed consent was obtained from all subjects at recruitment.
Statistics
The patients’ baseline clinical and demographic characteristics are reported as mean ± SD for continuous variables that are normally distributed and as median values (interquartile ranges) for variables that are skewed.
TG/HDL-C ratio was calculated according to the formula TG (mg/dL) divided by HDL-C (mg/dL) and the ratio was used as a continuous parameter, as a marker of insulin resistance. SUA/eGFR ratio was calculated according to the formula SUA (mg/dL) divided by eGFR (mL/min/1.73m2) and the ratio was used as a continuous parameter.
Participants were grouped into TG/HDL-C quintiles, and statistical differences among groups were assessed using One-way ANOVA for normally distributed data and Kruskal–Wallis tests for non-normally distributed data. Comparisons of proportions among groups were made using the Pearson χ2 test. Linear regression models were used to estimate the association between TG/HDL-C and SUA/GFR ratios. Logarithmically transformed values of skewed variables were employed for the statistical analysis.
TG/HDL-C and SUA/GFR ratios were used as independent variable in Cox analyses having fatal CV events as dependent variables, and sex, age, systolic BP, diabetes, hypertension, body mass index, and treatment with statins as possible confounders. Hazard ratios (HR) with 95% CI were produced. The null hypothesis was rejected for values of p < 0.05.
Kaplan Meier survival analysis was used to assess the event free survival in patients with different values of TG/HDL-C ratio, and with or without SUA/GFR above the median of values of the cohort. The analysis was adjusted for main confounding factors, i.e. diabetes and BMI.
Results
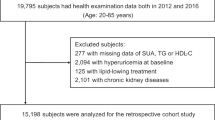
The main clinical characteristics of the entire study population, as well as when analyzed based on TG/HDL-C quintiles, are shown in Table 1. Altogether, out of 30,660 individuals, 18,694 for whom complete data on serum uric acid, GFR, triglycerides, HDL, and outcomes were available form the basis for the analyses.
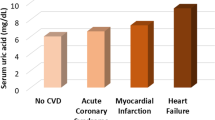
Mean age was 57 ± 15 years, mean SUA was 5.03 ± 1.42 mg/dl and mean GFR was 82 ± 20 ml/min per 1.73 m2, 46.7% were males, 67.2% had a history of hypertension and 10.5% of diabetes.
Data reported in Table 1 show some relevant differences among TG/HDL-C subgroups. Increasing values of age, BMI, intima media thickness (IMT), systolic blood pressure (SBP), and hypertension prevalence were observed progressively with rising IR, expressed as TG/HDL-C levels. Conversely, the mean eGFR decreased progressively as IR increased, going from 89 mL/min/1.73m2 in the lower TG/HDL-C quintile to 78 mL/min/1.73m2 in the upper TG/HDL-C quintile (p < 0.0001). As expected, glycemia and proportion of diabetes rose along with the increase in TG/HDL-C quintiles, as a surrogate of IR (Table 1).
The behavior of the association between SUA/GFR ratio and the TG/HDL-C ratio is shown in Supplemental Fig. 1. The surrogate of IR was directly associated to SUA/GFR in the whole cohort (data not shown, β = 12.5 [95% CI 11.7 to 13.4], p < 0.0001), and both in diabetic (Figure S1B, β = 5.6 [95% CI 3.0 to 8.2], p < 0.0001) and non-diabetic patients (Figure S1A, β = 13.5 [95% CI 12.6 to 14.4], p < 0.0001).
Over a median follow‐up of 10.4 ± 5.3 years, 1,394 (7.5%) CV deaths were recorded, including 395 (2.2%) fatal myocardial infarction, 339 (1.9%) fatal cerebrovascular events, and 398 (2.6%) fatal heart failures.
As shown in Table 2, our analysis delved into the incidence of CV events and mortality within patient groups stratified on the basis of TG/HDL-C quintiles. Remarkably, an ascending pattern in the prevalence of primary and secondary outcomes corresponded to increasing IR quintiles (P < 0.0001).
A Cox regression interaction analysis using the primary outcome assessed the interaction between TG/HDL-C and SUA/GFR ratio in determining CV mortality (p < 0.0001, data not shown).
Consistently, increased risk of CV mortality was observed along with increasing quintiles of TG/HDL-C, even after adjustment for the potential confounding factors, such as SUA/GFR ratio, renal function, BMI and the presence of diabetes (Fig. 1).
Kaplan–Meier survival curves for cardiovascular mortality according to TG/HDL-C quintiles adjusted for SUA/GFR ratio, diabetes and body mass index (BMI). Abbreviations: BMI, body mass index; GFR, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; SUA, serum uric acid
Both TG/HDL-C ratio and SUA/GFR ratio were independently associated to CV mortality in multivariable Cox regression models (Table 3). Being in the 4° or 5° quintile of TG/HDL-C led to a 20 and 37% increased risk of CV mortality (HR 1.20, 95% CI, 1.00–1.25, P = 0.05 and HR 1.37, 95% CI, 1.13–1.65, P = 0.001), respectively (Table 3).
The Kaplan–Meier curves for CV mortality on the basis of SUA/GFR ratio above or below the median) and TG/HDL-C in the lowest (1°−3°) or highest (4°−5°) quintiles are shown in Fig. 2. In particular, participants with a higher SUA/GFR ratio or higher TG/HDL-C ratio had a significantly greater likelihood of cardiovascular mortality compared to those without these risk factors. Those patients with both higher SUA/GFR ratio and higher TG/HDL-C ratio had a significantly higher probability of CV mortality than those with only one risk factors, independently by the presence of diabetes and BMI (log-rank test: P < 0.0001).
Kaplan–Meier survival curves for cardiovascular mortality according to SUA/GFR ratio (above or below the median) and TG/HDL-C quintiles (1°−2°−3° vs 4°−5° quintiles) adjusted for the presence of diabetes and body mass index (BMI). Abbreviations: BMI, body mass index; GFR, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; SUA, serum uric acid
Cox-regression analysis confirmed the predictive role of the presence of one or both the two risk factors, which showed a higher risk of CV mortality in participants with SUA/GFR ratio above the median and TG/HDL-C ratio belonging to the 4° and 5° quintiles (HR: 1.68, 95% CI: 1.42–1.99). This predictive role was still observed even after accounting for the main potential confounding factors (Table 4).
Discussion
Since hyperuricemia, dyslipidemia, and IR are all modifiable risk factors contributing to the progression of atherosclerosis and CV disease, understanding the relative contribution of each component on CV risk is of interest. Although all these risk factors have been investigated in large population studies, few analyses have examined their joint effect as commonly observed clinical traits [32,33,34].
This study explored the impact of TG/HDL-C, an easily obtainable and reliable marker of IR, on CV mortality risk in a high-risk population cohort. Using multivariate Cox regression analysis, we found both TG/HDL-C ratio and SUA/GFR ratio significantly predict CV mortality in high-risk population, regardless of other interconnected risk factors, including age, gender, diabetes, hypertension, BMI and statin treatment. Moreover, we found an additive (but not synergistic) effect of IR and GFR-adjusted SUA levels on CV mortality risk.
As expected, along with the rise in TG/HDL-C, we observed a progressive increase in age, BMI, SUA levels and prevalence of gout, hypertension and diabetes. Conversely, renal function decreases as IR increases (Table 1). The TG/HDL-C ratio has recently been proposed as a novel biomarker for predicting the risk of both MS and CV disease [35, 36], as well as a useful tool for monitoring and assessing the risk of CKD progression [37]. In fact, it has been shown to predict both a low GFR and the occurrence of micro/macroalbuminuria, even in non-diabetic patients [38]. Although the TG/glucose index (TyG) has also been proposed as surrogate marker for IR, its role is even less defined at this time. Accordingly, in a longitudinal study with a relatively small sample size (n = 732), the multivariable-adjusted hazard ratios (HR) for incident CV disease were statistically significant when evaluated by the TG/HDL-C ratio, but not by the TyG index [39]. The largest European study investigating the predictive role of TG/HDL-C ratio is a recent longitudinal analysis from 403,335 participants from UK Biobank which showed as the association between the TG/HDL-C ratio and increased risk for CV disease was largely mediated by a greater prevalence of dyslipidemia, type 2 diabetes, and hypertension [40]. Our findings of a strong association between higher TG/HDL-C levels and a greater risk for incidence of CV events (Table 2) confirm and extend previous studies showing that TG/HDL-C is a reliable marker for coronary atherosclerosis also in healthy non-diabetic individuals [41]. In line with the observation of a parallel increase in TG/HDL-C ratio and intima media thickness at the carotid level in the baseline picture of our study population (Table 1), elevated TG/HDL-C was found to predict unfavorable progression of arterial stiffness in a prospective cohort of hypertensive patients [42].
An important result, to our knowledge, which has not been previously reported, is the great impact of IR (expressed as TG/HDL-C) on CV mortality, independently by kidney function, SUA levels, BMI and diabetes (Table 3, Fig. 2). IR is known to be an important mediator of the association between SUA and vascular stiffness [43, 44], even in non-diabetic patients [45, 46]. In this study, we report a gradual increase in CV risk with incremental exposure to increasing quintiles of the TG/HDL ratio, independently by major confounding factors of IR, such as diabetes and BMI (Fig. 1).
The relationship between SUA/GFR and IR is further complicated for several reasons. First, the relationship between SUA and kidney function must be considered. SUA levels are highest in CKD patients due to impaired renal excretion, and the detrimental effects of SUA on kidney function [47, 48], as well as on vascular disease [43, 49,50,51,52,53], have been well documented. Evidence is accumulating regarding the need to index SUA to renal function [54, 55]. Previous studies have investigated the role of the serum creatinine (sCr)-normalized SUA (SUA/sCr) ratio in various contexts [56,57,58,59,60], identifying a threshold value of this index to predict CV mortality [56]. Interestingly, a significant positive correlation between SUA/Cr and metabolic syndrome has been reported in the Chinese population, suggesting it may be a novel predictive marker for metabolic syndrome risk [61].
A second point concerns the role of uric acid. SUA, while a major antioxidant in human plasma, is paradoxically linked to the development of obesity, hypertension, and CV disease—conditions associated with oxidative stress. This paradox may stem from uric acid acting as an antioxidant in plasma but as a pro-oxidant within cells. Evidence suggests that its pro-oxidative effects play a contributory role in the pathogenesis of CV disease and mortality risk. Nonetheless, the GFR estimate, taking into account gender, age and ethnicity is overall the best index of renal function, especially for large-scale use [62]. For this reason, in order to analyze the role of an increase in SUA levels due to altered uric acid production independently by the increased levels resulting from reduced renal excretion, we assess the role of SUA/GFR ratio in determining CV mortality risk. In this way, we aim to describe the unfavorable impact of uric acid overproduction independently by the detrimental effect of impaired renal function on CV outcome.
While the relationship between IR surrogates and CVD outcomes have been extensively investigated [63], even in non-diabetic patients [64], an assessment of the interplay between IR, SUA levels and kidney function in predicting CV risk in a community-based populations was lacking.
IR is a central component of the metabolic dysregulation observed in obesity, increasing the risk of developing type 2 diabetes and complications related to diabetes such as CKD [65,66,67]. Once again, the confounding factors are interrelated. In this study, the risk of CV mortality was significantly higher in participants with a higher TG/HDL-C ratio, independent of confounding factors (Table 3, p = 0.027). A previous URRAH analysis showed that SUA can predict both CV and all-cause mortality in patients without established cardiovascular disease, independently of TG levels [68]. The relationship between SUA levels and lipids, and their interaction in relation to prognosis were explored in specific settings [69,70,71]. In contrast, investigating the predictive role of SUA/GFR ratio and of a surrogate marker of IR in their potential interplay is novel in this context. We confirm the TG/HDL-C predictive power for CV mortality, reporting that TG/HDL-C ratio between 2.5 and 3.8 (4° quintile), and > 3.8 (5°quintile) increased CV mortality risk by 20 and 37%, respectively, independently by age, gender, SUA levels, kidney function, BMI, the presence of hypertension, diabetes and statins treatment (Table 3, p = 0.05 and p = 0.001, respectively). Moreover, no studies have explored the predictive role of SUA/GFR concerning CV mortality risk across TG/HDL-C strata.
The strength of the study shown herein is that, to our knowledge, it is the first aimed at reporting for the first time the potential interplay between these two factors, demonstrating an independent and additive effect on CV mortality risk (Fig. 2, Table 3 and 4). The limitations are represented by the fact that this was a retrospective evaluation, that the analysis was based on a single TG, HDL-C and SUA measurements without taking into consideration the dilution bias, and that the design was fit to demonstrate an association but not a causality in the relationship between TG/HDL-C, SUA and CV mortality. Another significant limitation is the inability to assess the muscle mass, which may represent a limitation in estimating GFR.
Conclusions
Our results provide substantial evidence for the TG/HDL-C ratio as an indicator of CV risk, independent of SUA levels and kidney function. This reinforces its importance as a useful and cost-effective early indicator for subclinical atherosclerosis and subsequent cardiac and cerebrovascular events, with significant implications for global health. The TG/HDL-C is a readily available measure that can be used in the future to predict CV mortality in clinical or epidemiological settings. For the first time, we assessed the impact of SUA/GFR ratio on CV mortality risk and described the additive effect of GFR-adjusted SUA levels and the TG/HDL-C ratio on CV risk. The implications of elevated TG/HDL-C in subjects with increased SUA compared to those with normal SUA, as well as in CKD and non-CKD patients, warrant further investigation and may shed light on the pathophysiology of IR and its consequences.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17:122. https://doi.org/10.1186/s12933-018-0762-4.
Copur S, Demiray A, Kanbay M. Uric acid in metabolic syndrome: does uric acid have a definitive role? Eur J Intern Med. 2022;103:4–12. https://doi.org/10.1016/j.ejim.2022.04.022.
Saito Y, Tanaka A, Node K, Kobayashi Y. Uric acid and cardiovascular disease: a clinical review. J Cardiol. 2021;78(1):51–7. https://doi.org/10.1016/j.jjcc.2020.12.013.
Kataria A, Trasande L, Trachtman H. The effects of environmental chemicals on renal function. Nat Rev Nephrol. 2015;11(10):610–25. https://doi.org/10.1038/nrneph.2015.94.
Ambrosio G, Leiro MGC, Lund LH, Coiro S, Cardona A, Filippatos G, Ferrari R, Piepoli MF, Coats AJS, Anker SD, Laroche C, Almenar-Bonet L, Poder P, Valero DB, Frisinghelli A, Maggioni AP. Serum uric acid and outcomes in patients with chronic heart failure through the whole spectrum of ejection fraction phenotypes: analysis of the ESC-EORP Heart Failure Long-Term (HF LT) registry. Eur J Intern Med. 2021;89:65–75. https://doi.org/10.1016/j.ejim.2021.04.001.
Heerkens L, van Westing AC, Voortman T, Kardys I, Boersma E, Geleijnse JM. Serum uric acid is related to liver and kidney disease and 12-year mortality risk after myocardial infarction. Front Endocrinol (Lausanne). 2023;14:1240099. https://doi.org/10.3389/fendo.2023.1240099.
Johnson RJ. Why focus on uric acid? Curr Med Res Opin. 2015;31(Suppl 2):3–7. https://doi.org/10.1185/03007995.2015.1087979.
Chen WY, Fu YP, Zhou M. The bidirectional relationship between metabolic syndrome and hyperuricemia in China: a longitudinal study from CHARLS. Endocrine. 2022;76(1):62–9. https://doi.org/10.1007/s12020-022-02979-z.
Shu J, Zhao R, Xu H, Liu X, Guo H, Lu C. Hyperuricemia is associated with metabolic syndrome: a cross-sectional analysis of the National Health and Nutrition Examination Survey (NHANES). Prev Med Rep. 2023;36:102520. https://doi.org/10.1016/j.pmedr.2023.102520.
Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008;359(17):1811–21. https://doi.org/10.1056/NEJMra0800885. Erratum in: N Engl J Med. 2010 Jun 10;362(23):2235.
Maloberti A, Dell’Oro R, Bombelli M, Quarti-Trevano F, Facchetti R, Mancia G, Grassi G. Long-term increase in serum uric acid and its predictors over a 25 year follow-up: results of the PAMELA study. Nutr Metab Cardiovasc Dis. 2024;34(1):223–9. https://doi.org/10.1016/j.numecd.2023.10.009.
Zhang Y, Chen S, Yuan M, Xu Y, Xu H. Gout and diet: a comprehensive review of mechanisms and management. Nutrients. 2022;14(17):3525. https://doi.org/10.3390/nu14173525.
Russo E, Viazzi F, Pontremoli R, Barbagallo CM, Bombelli M, Casiglia E, Cicero AFG, Cirillo M, Cirillo P, Desideri G, D’Elia L, Ferri C, Galletti F, Gesualdo L, Giannattasio C, Iaccarino G, Leoncini G, Mallamaci F, Maloberti A, Masi S, Mengozzi A, Mazza A, Muiesan ML, Nazzaro P, Palatini P, Parati G, Rattazzi M, Rivasi G, Salvetti M, Tikhonoff V, Tocci G, Ungar A, Verdecchia P, Virdis A, Volpe M, Grassi G, Borghi C, Working Group on UricAcid and Cardiovascular Risk of the Italian Society of Hypertension. Association of uric acid with kidney function and albuminuria: the Uric Acid Right for heArt Health (URRAH) project. J Nephrol. 2022;35(1):211–21. https://doi.org/10.1007/s40620-021-00985-4.
Ricardo AC, Anderson CA, Yang W, Zhang X, Fischer MJ, Dember LM, Fink JC, Frydrych A, Jensvold NG, Lustigova E, Nessel LC, Porter AC, Rahman M, Wright Nunes JA, Daviglus ML, Lash JP, CRIC Study Investigators. Healthy lifestyle and risk of kidney disease progression, atherosclerotic events, and death in CKD: findings from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis. 2015;65(3):412–24. https://doi.org/10.1053/j.ajkd.2014.09.016.
Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6(10):2364–73. https://doi.org/10.2215/CJN.02180311.
Kurella M, Lo JC, Chertow GM. Metabolic syndrome and the risk for chronic kidney disease among nondiabetic adults. J Am Soc Nephrol. 2005;16(7):2134–40. https://doi.org/10.1681/ASN.2005010106.
Watt NT, Gage MC, Patel PA, Viswambharan H, Sukumar P, Galloway S, Yuldasheva NY, Imrie H, Walker AMN, Griffin KJ, Makava N, Skromna A, Bridge K, Beech DJ, Schurmans S, Wheatcroft SB, Kearney MT, Cubbon RM. Endothelial SHIP2 suppresses Nox2 NADPH oxidase-dependent vascular oxidative stress, endothelial dysfunction, and systemic insulin resistance. Diabetes. 2017;66(11):2808–21. https://doi.org/10.2337/db17-0062.
Chu SY, Jung JH, Park MJ, Kim SH. Risk assessment of metabolic syndrome in adolescents using the triglyceride/high-density lipoprotein cholesterol ratio and the total cholesterol/high-density lipoprotein cholesterol ratio. Ann Pediatr Endocrinol Metab. 2019;24(1):41–8. https://doi.org/10.6065/apem.2019.24.1.41.
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146. https://doi.org/10.1186/s12933-014-0146-3.
de Giorgis T, Marcovecchio ML, Di Giovanni I, Giannini C, Chiavaroli V, Chiarelli F, Mohn A. Triglycerides-to-HDL ratio as a new marker of endothelial dysfunction in obese prepubertal children. Eur J Endocrinol. 2014;170:173–80.
Di Bonito P, Moio N, Scilla C, Cavuto L, Sibilio G, Sanguigno E, Forziato C, Saitta F, Iardino MR, Di Carluccio C, Capaldo B. Usefulness of the high triglyceride-to-HDL cholesterol ratio to identify cardiometabolic risk factors and preclinical signs of organ damage in outpatient children. Diabetes Care. 2012;35(1):158–62. https://doi.org/10.2337/dc11-1456.
Murguía-Romero M, Jiménez-Flores JR, Sigrist-Flores SC, Espinoza-Camacho MA, Jiménez-Morales M, Piña E, Méndez-Cruz AR, Villalobos-Molina R, Reaven GM. Plasma triglyceride/HDL-cholesterol ratio, insulin resistance, and cardiometabolic risk in young adults. J Lipid Res. 2013;54(10):2795–9. https://doi.org/10.1194/jlr.M040584.
Baneu P, Văcărescu C, Drăgan SR, Cirin L, Lazăr-Höcher AI, Cozgarea A, Faur-Grigori AA, Crișan S, Gaiță D, Luca CT, Cozma D. The triglyceride/HDL ratio as a surrogate biomarker for insulin resistance. Biomedicines. 2024;12(7):1493. https://doi.org/10.3390/biomedicines12071493.
Okosun IS, Okosun B, Lyn R, Airhihenbuwa C. Surrogate indexes of insulin resistance and risk of metabolic syndrome in non-Hispanic White, non-Hispanic Black and Mexican American. Diabetes Metab Syndr. 2020;14(1):3–9. https://doi.org/10.1016/j.dsx.2019.11.012.
Virdis A, Masi S, Casiglia E, Tikhonoff V, Cicero AFG, Ungar A, Rivasi G, Salvetti M, Barbagallo CM, Bombelli M, Dell’Oro R, Bruno B, Lippa L, D’Elia L, Verdecchia P, Mallamaci F, Cirillo M, Rattazzi M, Cirillo P, Gesualdo L, Mazza A, Giannattasio C, Maloberti A, Volpe M, Tocci G, Georgiopoulos G, Iaccarino G, Nazzaro P, Parati G, Palatini P, Galletti F, Ferri C, Desideri G, Viazzi F, Pontremoli R, Muiesan ML, Grassi G, Borghi C, from the Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension. Identification of the uric acid thresholds predicting an increased total and cardiovascular mortality over 20 years. Hypertension. 2020;75(2):302–8. https://doi.org/10.1161/HYPERTENSIONAHA.119.13643.
Cui K, Song Y, Yin D, Song W, Wang H, Zhu C, Feng L, Fu R, Jia L, Lu Y, Zhang D, Song C, Yang Y, Dong Q, Dou K. Uric acid levels, number of standard modifiable cardiovascular risk factors, and prognosis in patients with coronary artery disease: a large cohort study in Asia. J Am Heart Assoc. 2023;12(20):e030625. https://doi.org/10.1161/JAHA.123.030625.
D'Elia L, Masulli M, Virdis A, Casiglia E, Tikhonoff V, Angeli F, Barbagallo CM, Bombelli M, Cappelli F, Cianci R, Ciccarelli M, Cicero AFG, Cirillo M, Cirillo P, Dell'Oro R, Desideri G, Ferri C, Gesualdo L, Giannattasio C, Grassi G, Iaccarino G, Lippa L, Mallamaci F, Maloberti A, Masi S, Mazza A, Mengozzi A, Muiesan ML, Nazzaro P, Palatini P, Parati G, Pontremoli R, Quarti-Trevano F, Rattazzi M, Reboldi G, Rivasi G, Russo E, Salvetti M, Tocci G, Ungar A, Verdecchia P, Viazzi F, Volpe M, Borghi C, Galletti F. Triglyceride-glucose index and mortality in a large regional-based italian database (Urrah Project). J Clin Endocrinol Metab. 2024:dgae170. https://doi.org/10.1210/clinem/dgae170.
Liu X, Tan Z, Huang Y, Zhao H, Liu M, Yu P, Ma J, Zhao Y, Zhu W, Wang J. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21(1):124. https://doi.org/10.1186/s12933-022-01546-0.
Chen J, Wu K, Lin Y, Huang M, Xie S. Association of triglyceride glucose index with all-cause and cardiovascular mortality in the general population. Cardiovasc Diabetol. 2023;22(1):320. https://doi.org/10.1186/s12933-023-02054-5.
Desideri G, Virdis A, Casiglia E, Borghi C, Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension. Exploration into uric and cardiovascular disease: Uric Acid Right for heArt Health (URRAH) project, a study protocol for a retrospective observational study. High Blood Press Cardiovasc Prev. 2018;25(2):197–202. https://doi.org/10.1007/s40292-018-0250-7.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Liu F, Du GL, Song N, et al. Hyperuricemia and its association with adiposity and dyslipidemia in Northwest China: results from cardiovascular risk survey in Xinjiang (CRS 2008–2012). Lipids Health Dis. 2020;19:58. https://doi.org/10.1186/s12944-020-01211-z.
Acevedo-Fernández M, Porchia LM, Elguezabal-Rodelo RG, López-Bayghen E, Gonzalez-Mejia ME. Concurrence of hyperinsulinemia and hyperuricemia significantly augmented all-cause mortality. Nutr Metab Cardiovasc Dis. 2023;33(9):1725–32. https://doi.org/10.1016/j.numecd.2023.05.023.
Xu F, Ma C, Wang S, Li Q, Zhang Z, He M. Higher atherogenic index of plasma is associated with hyperuricemia: a national longitudinal study. Int J Endocrinol. 2024;2024:4002839. https://doi.org/10.1155/2024/4002839.
Kosmas CE, Rodriguez Polanco S, Bousvarou MD, Papakonstantinou EJ, Peña Genao E, Guzman E, Kostara CE. The Triglyceride/High-Density Lipoprotein Cholesterol (TG/HDL-C) ratio as a risk marker for metabolic syndrome and cardiovascular disease. Diagnostics (Basel). 2023;13(5):929. https://doi.org/10.3390/diagnostics13050929.
Xiao D, Sun H, Chen L, Li X, Huo H, Zhou G, Zhang M, He B. Assessment of six surrogate insulin resistance indexes for predicting cardiometabolic multimorbidity incidence in Chinese middle-aged and older populations: insights from the China health and retirement longitudinal study. Diabetes Metab Res Rev. 2024;40(1):e3764. https://doi.org/10.1002/dmrr.3764.
Nguyen HH, Tran HH, Nguyen LT, Nguyen T, Nguyen NA, Vi MT, Nguyen KT. TG/HDL-C ratio is a risk factor associated with CKD: use in assessing the risk of progression of CKD. Pathophysiology. 2022;29(3):374–82. https://doi.org/10.3390/pathophysiology29030029.
Raikou VD, Kyriaki D, Gavriil S. Triglycerides to high-density lipoprotein cholesterol ratio predicts chronic renal disease in patients without diabetes mellitus (STELLA study). J Cardiovasc Dev Dis. 2020;7(3):28. https://doi.org/10.3390/jcdd7030028.
Salazar MR, Carbajal HA, Espeche WG, Aizpurúa M, Dulbecco CA, Reaven GM. Comparison of two surrogate estimates of insulin resistance to predict cardiovascular disease in apparently healthy individuals. Nutr Metab Cardiovasc Dis. 2017;27(4):366–73.
Che B, Zhong C, Zhang R, Pu L, Zhao T, Zhang Y, Han L. Triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio as potential cardiovascular disease risk factors: an analysis of UK biobank data. Cardiovasc Diabetol. 2023;22(1):34. https://doi.org/10.1186/s12933-023-01762-2.
Patil S, Rojulpote C, Gonuguntla K, Karambelkar P, Bhattaru A, Raynor WY, Borja AJ, Vuthaluru K, Zhang V, Werner TJ, Gerke O, Høilund-Carlsen PF, Alavi A. Association of triglyceride to high density lipoprotein ratio with global cardiac microcalcification to evaluate subclinical coronary atherosclerosis in non-diabetic individuals. Am J Cardiovasc Dis. 2020;10(3):241–6.
Wu Z, Zhou D, Liu Y, Li Z, Wang J, Han Z, Miao X, Liu X, Li X, Wang W, et al. Association of TyG index and TG/HDL-C ratio with arterial stiffness progression in a non-normotensive population. Cardiovasc Diabetol. 2021;20(1):134.
Genovesi S, Montelisciani L, Viazzi F, Giussani M, Lieti G, Patti I, Orlando A, Antolini L, Salvi P, Parati G. Uric acid and arterial stiffness in children and adolescents: role of insulin resistance and blood pressure. Front Cardiovasc Med. 2022;9:978366. https://doi.org/10.3389/fcvm.2022.978366.
Ramirez AJ, Christen AI, Sanchez RA. Serum uric acid elevation is associated to arterial stiffness in hypertensive patients with metabolic disturbances. Curr Hypertens Rev. 2018;14(2):154–60. https://doi.org/10.2174/1573402114666180413143312.
Vyssoulis GP, Pietri PG, Karpanou EA, Vlachopoulos CV, Kyvelou SM, Spanos P, Cokkinos DV, Stefanadis CI. Differential impact of metabolic syndrome on arterial stiffness and wave reflections: focus on distinct definitions. Int J Cardiol. 2010;138(2):119–25. https://doi.org/10.1016/j.ijcard.2008.08.005.
Zhang X, Li J, Zheng S, Luo Q, Zhou C, Wang C. Fasting insulin, insulin resistance, and risk of cardiovascular or all-cause mortality in non-diabetic adults: a meta-analysis. Biosci Rep. 2017;37(5):BSR20170947. https://doi.org/10.1042/BSR20170947.
Viazzi F, Piscitelli P, Giorda C, Ceriello A, Genovese S, Russo G, Guida P, Fioretto P, De Cosmo S, Pontremoli R, AMD-Annals Study Group. Metabolic syndrome, serum uric acid and renal risk in patients with T2D. PLoS One. 2017;12(4):e0176058. https://doi.org/10.1371/journal.pone.0176058.
Johnson RJ, Nakagawa T, Jalal D, Sánchez-Lozada LG, Kang DH, Ritz E. Uric acid and chronic kidney disease: which is chasing which? Nephrol Dial Transplant. 2013;28(9):2221–8. https://doi.org/10.1093/ndt/gft029.
Russo E, Bertolotto M, Zanetti V, Picciotto D, Esposito P, Carbone F, Montecucco F, Pontremoli R, Garibotto G, Viazzi F, Verzola D. Role of uric acid in vascular remodeling: cytoskeleton changes and migration in VSMCs. Int J Mol Sci. 2023;24(3):2960. https://doi.org/10.3390/ijms24032960.
Kırça M, Oğuz N, Çetin A, Uzuner F, Yeşilkaya A. Uric acid stimulates proliferative pathways in vascular smooth muscle cells through the activation of p38 MAPK, p44/42 MAPK and PDGFRβ. J Recept Signal Transduct Res. 2017;37(2):167–73. https://doi.org/10.1080/10799893.2016.1203941.
Corry DB, Eslami P, Yamamoto K, Nyby MD, Makino H, Tuck ML. Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin-angiotensin system. J Hypertens. 2008;26:269–75. https://doi.org/10.1097/HJH.0b013e3282f240bf.
Ouyang R, Zhao X, Zhang R, Yang J, Li S, Deng D. FGF21 attenuates high uric acid-induced endoplasmic reticulum stress, inflammation and vascular endothelial cell dysfunction by activating Sirt1. Mol Med Rep. 2022;25:35. https://doi.org/10.3892/mmr.2021.12551.
Xu J, Du X, Zhang S, Zang X, Xiao Z, Su R, Huang X, Liu L. Diagnostic value of uric acid to high-density lipoprotein cholesterol ratio in abdominal aortic aneurysms. Ann Med. 2024;56(1):2357224. https://doi.org/10.1080/07853890.2024.2357224.
Russo E, Viazzi F, Pontremoli R, Barbagallo CM, Bombelli M, Casiglia E, Cicero AFG, Cirillo M, Cirillo P, Desideri G, D’Elia L, Dell’Oro R, Ferri C, Galletti F, Gesualdo L, Giannattasio C, Iaccarino G, Leoncini G, Mallamaci F, Maloberti A, Masi S, Mengozzi A, Mazza A, Muiesan ML, Nazzaro P, Palatini P, Parati G, Rattazzi M, Rivasi G, Salvetti M, Tikhonoff V, Tocci G, Quarti Trevano FAL, Ungar A, Verdecchia P, Virdis A, Volpe M, Grassi G, Borghi C. Serum uric acid and kidney disease measures independently predict cardiovascular and total mortality: the Uric Acid Right for Heart Health (URRAH) project. Front Cardiovasc Med. 2021;27(8):713652. https://doi.org/10.3389/fcvm.2021.713652.
Matsushita K, Coresh J, Sang Y, Chalmers J, Fox C, Guallar E, Jafar T, Jassal SK, Landman GW, Muntner P, Roderick P, Sairenchi T, Schöttker B, Shankar A, Shlipak M, Tonelli M, Townend J, van Zuilen A, Yamagishi K, Yamashita K, Gansevoort R, Sarnak M, Warnock DG, Woodward M, Ärnlöv J, CKD Prognosis Consortium. Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 2015;3(7):514–25. https://doi.org/10.1016/S2213-8587(15)00040-6.
D’Elia L, Masulli M, Cirillo P, Virdis A, Casiglia E, Tikhonoff V, Angeli F, Barbagallo CM, Bombelli M, Cappelli F, Cianci R, Ciccarelli M, Cicero AFG, Cirillo M, Dell’Oro R, Desideri G, Ferri C, Gesualdo L, Giannattasio C, Grassi G, Iaccarino G, Lippa L, Mallamaci F, Maloberti A, Masi S, Mazza A, Mengozzi A, Muiesan ML, Nazzaro P, Palatini P, Parati G, Pontremoli R, Quarti-Trevano F, Rattazzi M, Reboldi G, Rivasi G, Russo E, Salvetti M, Tocci G, Ungar A, Verdecchia P, Viazzi F, Volpe M, Borghi C, Galletti F, Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension (SIIA). Serum uric acid/serum creatinine ratio and cardiovascular mortality in diabetic individuals-the Uric Acid Right for Heart Health (URRAH) Project. Metabolites. 2024;14(3):164. https://doi.org/10.3390/metabo14030164.
Choi J, Joe H, Oh JE, Cho YJ, Shin HS, Heo NH. The correlation between NAFLD and serum uric acid to serum creatinine ratio. PLoS One. 2023;18(7):e0288666. https://doi.org/10.1371/journal.pone.0288666. Erratum in: PLoS One. 2023 Nov 16;18(11):e0294801. 10.1371/journal.pone.0294801.
Baral S, Uprety AB, Kshetri R. Serum uric acid to creatinine ratio with estimated glomerular filtration rate in type 2 diabetes patients. J Nepal Health Res Counc. 2023;21(2):271–6. https://doi.org/10.33314/jnhrc.v21i02.4565.
Chen L, Zhu Z, Ye S, Zheng M. The serum uric acid to serum creatinine ratio is an independent risk factor for diabetic kidney disease. Diabetes Metab Syndr Obes. 2022;15:3693–703. https://doi.org/10.2147/DMSO.S387426.
Xi X, Cai J, Zhang C, Wang X. Does serum uric acid to creatinine ratio predict mortality risk in patients with heart failure? Tex Heart Inst J. 2024;51(1):e238210. https://doi.org/10.14503/THIJ-23-8210.
Cao T, Tong C, Halengbieke A, Ni X, Tang J, Zheng D, Guo X, Yang X. Serum uric acid to creatinine ratio and metabolic syndrome in middle-aged and elderly population: based on the 2015 CHARLS. Nutr Metab Cardiovasc Dis. 2023;33(7):1339–48. https://doi.org/10.1016/j.numecd.2023.05.004.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-266.
Penno G, Solini A, Orsi E, Bonora E, Fondelli C, Trevisan R, Vedovato M, Cavalot F, Zerbini G, Lamacchia O, Nicolucci A, Pugliese G, Renal Insufficiency And Cardiovascular Events (RIACE) Study Group. Insulin resistance, diabetic kidney disease, and all-cause mortality in individuals with type 2 diabetes: a prospective cohort study. BMC Med. 2021;19(1):66. https://doi.org/10.1186/s12916-021-01936-3.
Ausk KJ, Boyko EJ, Ioannou GN. Insulin resistance predicts mortality in nondiabetic individuals in the U.S. Diabetes Care. 2010;33(6):1179–85. https://doi.org/10.2337/dc09-2110.
Whaley-Connell A, Sowers JR. Insulin resistance in kidney disease: is there a distinct role separate from that of diabetes or obesity? Cardiorenal Med. 2017;8(1):41–9. https://doi.org/10.1159/000479801. Epub 2017 Sep 30.
Fan Y, Yan Z, Li T, Li A, Fan X, Qi Z, Zhang J. Primordial drivers of diabetes heart disease: comprehensive insights into insulin resistance. Diabetes Metab J. 2024;48(1):19–36. https://doi.org/10.4093/dmj.2023.0110.
Artunc F, Schleicher E, Weigert C, Fritsche A, Stefan N, Häring HU. The impact of insulin resistance on the kidney and vasculature. Nat Rev Nephrol. 2016;12(12):721–37. https://doi.org/10.1038/nrneph.2016.145.
Mengozzi A, Pugliese NR, Desideri G, Masi S, Angeli F, Barbagallo CM, Bombelli M, Cappelli F, Casiglia E, Cianci R, Ciccarelli M, Cicero AFG, Cirillo M, Cirillo P, Dell’Oro R, D’Elia L, Ferri C, Galletti F, Gesualdo L, Giannattasio C, Grassi G, Iaccarino G, Lippa L, Mallamaci F, Maloberti A, Masulli M, Mazza A, Muiesan ML, Nazzaro P, Palatini P, Parati G, Pontremoli R, Quarti-Trevano F, Rattazzi M, Reboldi G, Rivasi G, Russo E, Salvetti M, Tikhonoff V, Tocci G, Ungar A, Verdecchia P, Viazzi F, Volpe M, Borghi C, Virdis A, Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension (SIIA). Serum uric acid predicts all-cause and cardiovascular mortality independently of hypertriglyceridemia in cardiometabolic patients without established CV disease: a sub-analysis of the URic acid Right for heArt Health (URRAH) study. Metabolites. 2023;13(2):244. https://doi.org/10.3390/metabo13020244.
Kawamoto R, Ninomiya D, Akase T, et al. Serum uric acid to creatinine ratio independently predicts incident metabolic syndrome among community-dwelling persons. Metab Syndr Relat Disord. 2019;17(2):81–9. https://doi.org/10.1089/met.2018.0055.
Huang L, Lu Z, You X, Zou C, He L, Xie J, Zhou X. U-shaped association of serum uric acid with all-cause mortality in patients with hyperlipidemia in the United States: a cohort study. Front Cardiovasc Med. 2023;23(10):1165338. https://doi.org/10.3389/fcvm.2023.1165338.
Yang Y, Zhang J, Jia L, Su J, Ma M, Lin X. The interaction between uric acid and high-density lipoprotein cholesterol on the prognosis of patients with acute myocardial infarction. Front Cardiovasc Med. 2023;10:1226108. https://doi.org/10.3389/fcvm.2023.1226108.
Funding
This work has been conducted with an unrestricted grant from the Fondazione of the Italian Society of Hypertension (grant: MIOL).
Author information
Authors and Affiliations
Consortia
Contributions
FV, RP, CB: Conceptualization, EC, GD, GG,CF, MLM, GP, AV: Methodology, FA, CMB, BB, MB, FC, RC, MC, AFGC, MM, AM, PN, PP: Data curation, ER, FV; RP: Writing- Original draft preparation. MC, PC, LD, FG, LG, CG, GI, EI, LL, AM, SM: Visualization, Investigation. EC, GD, GG, GP, AV: Supervision. FQT, MR, GR, GR, MS, VT, GT, AU, PV: Validation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The URRAH project was performed according to the Declaration of Helsinki for Human Research (41stWorld Medical Assembly, 1990). The processing of the patients’ personal data collected in this study complies with the European Directive on the Privacy of Data. Approval was sought from the Ethical Committee of the coordinating center at the Division of Internal Medicine of the University of Bologna (No. 77/2018/Oss/AOUBo). Informed consent was obtained from all subjects at recruitment.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Russo, E., Viazzi, F., Pontremoli, R. et al. Predictive value of TG/HDL-C and GFR-adjusted uric acid levels on cardiovascular mortality: the URRAH study. Lipids Health Dis 24, 21 (2025). https://doi.org/10.1186/s12944-025-02440-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1186/s12944-025-02440-w