Abstract
Background
In addition to their standard use to assess real-time symptom burden, patient-reported outcomes (PROs), such as the Patient-Reported Outcomes Measurement Information System (PROMIS), measures offer a potential opportunity to understand when patients are experiencing meaningful clinical decline. If PROs can be used to assess decline, such information can be used for informing medical decision making and determining patient-centered treatment pathways. We sought to use clinically implemented PROMIS measures to retrospectively characterize the final PROMIS report among all patients who completed at least one PROMIS assessment from December 2017-March 2020 in one large health system, stratified by decedents vs. survivors. We conducted a retrospective cohort analysis of decedents (N = 1,499) who received care from outpatient neurology clinical practice within a single, large health system as part of usual care. We also compared decedents to survivors (360 + days before death; N = 49,602) on PROMIS domains and PROMIS-Preference (PROPr) score, along with demographics and clinical characteristics. We used electronic health record (EHR) data with built-in PROMIS measures. Linear regressions assessed differences in PROMIS domains and aggregate PROPr score by days before death of the final PROMIS completion for each patient.
Results
Among decedents in our sample, in multivariable regression, only fatigue (range 54.48–59.38, p < 0.0029) and physical function (range 33.22–38.38, p < 0.0001) demonstrated clinically meaningful differences across time before death. The overall PROPr score also demonstrated statistically significant difference comparing survivors (0.19) to PROPr scores obtained 0–29 days before death (0.29, p < 0.0001).
Conclusions
Although clinic completion of PROMIS measures was near universal, very few patients had more than one instance of PROMIS measures reported, limiting longitudinal analyses. Therefore, patient-reported outcomes in clinical practice may not yet be robust enough for incorporation in prediction models and assessment of trajectories of decline, as evidenced in these specialty clinics in one health system. PROMIS measures can be used to effectively identify symptoms and needs in real time, and robust incorporation into EHRs can improve patient-level outcomes, but further work is needed for them to offer meaningful inputs for defining patient trajectories near the end of life.
Plain English Summary
Assessing symptom burden provides an opportunity to understand clinical decline, particularly as people approach the end of life. We sought to understand whether symptoms reported by patients can be used to assess decline in health. Such information can inform decision-making about care and treatments. Of eight symptoms that we assessed, patient reports of fatigue and physical function were associated with clinical decline, as was an overall score of symptom burden. Because few symptoms were associated with decline, patient-reported outcomes in clinical practice may not yet be robust enough for incorporation in prediction models and assessment of trajectories of decline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Identifying clinical decline before death is critical because decline and associated prognosis are essential elements of patient-centered medical decision-making and delivery of care consistent with patient goals and values (i.e., goal-concordant care) [1]. For example, as many patients approach the end of life, they and their families (especially for those who are cognitively incapacitated) shift goals to improving comfort and discontinuing treatments, as those treatments lose potential effectiveness in the context of progressing disease. One goal-driven treatment option is hospice, which requires a prognosis of ≤ 6 months, and many patients and families decline other intensive treatments, such as cardiopulmonary resuscitation (CPR) or ventilator support [2,3,4]. Therefore, it is important to explore opportunities to identify patient decline preceding death more precisely.
The Patient-Reported Outcomes Measurement Information System (PROMIS) offers an opportunity to identify patient-reported outcomes (PROs) that may be associated with clinical decline among people near the end of life [5]. Diehr et al. characterized longitudinal history of disease including acute events and tracked co-occurring patient-reported health; they found that declines in patient-perceived health precipitate acute events, and an additional drop in score resulted from the acute event [6, 7]. Evidence indicates that terminal decline begins 3–5 years before death, thought additional research is needed to identifying trajectories meaningful to health care delivery and practice [8]. One approach, integrating real-world outpatient assessment of symptom trajectories before death via PROMIS, has yet to be evaluated.
Therefore, we conducted a pragmatic study of real-world clinical implementation of PROMIS measures to retrospectively characterize differences in reported health-related quality of life before death among people who received care in neurology clinics across one large health system.
Methods
Study design
We used retrospective, structured electronic health record (EHR) data at an academic medical center in Pennsylvania to characterize clinical differences in PROMIS scores between decedents and survivors, and across decedents who completed PROMIS measures in the last year of life, to determine any potential patterns in PROMIS before death. Because PROMIS was systematically implemented across outpatient neurology within the health system, nearly all observations were obtained in standard neurology clinics, which had 82% completion rates during the study period.
Study procedures were approved by the RAND Corporation and University of Pittsburgh Institutional Review Boards.
Setting & data source
We extracted EHR data for all patients who completed at least one PROMIS assessment from December 2017-March 2020. We stratified by survivors (N = 49,602) and decedents (N = 1,499) during the study period. We included all people with a cognitive function score from the PROMIS-16 in neurology clinics. We then subset to patients who had at least one PROMIS assessment, at least one PROMIS cognitive assessment, demographic data, diagnosis data ≤ 180 days before the date of the first PROMIS assessment, and who were at least 18 years old at the time of the first PROMIS assessment.
The EHR automatically assigns the PROMIS-16 at all neurology visit types. It is sent to the patient portal 7 days before the visit. If the patient or their proxy does not complete the questionnaire on the portal, the front desk staff provide a tablet computer in the waiting room for completion. If patients are unable or unwilling to use the tablet, questions are asked verbally by staff during rooming. All responses are immediately scored and available in the EHR.
Variables
Demographic & Clinical Characteristics: We obtained data on patient demographics (age, gender, race) and clinical characteristics (International Classification of Diseases (ICD)-10 diagnoses, PROMIS cognitive function) [9]. For each patient, we identified all ICD-10 diagnosis codes from clinical encounters that occurred within the six months prior to the first PROMIS assessment. We measured comorbidity burden using diagnoses from the Charlson Comorbidity Index with available EHR data, which included chronic pulmonary disease, diabetes, cancer, peripheral vascular disease, renal disease, hemiplegia/paraplegia, congestive heart failure, liver disease, myocardial infarction, and rheumatic disease [10]. In assessing comorbidities, we also included depression and hypertension diagnoses from the Elixhauser, due to their clinical association with cognitive impairment (CI) [11]. We used the Clinical Classifications Software Refined (CCS-R) and consultation with a physician (LBS) to categorize patients as having no CI, possible CI, or definite CI based on ICD-10 diagnoses.
Mortality: We obtained mortality indicators from vital statistics linked to EHR data. Among decedents, we defined time before death of the last PROMIS assessment categorically at 30-day intervals up to 90 days, then 90-day intervals up to 359 days. We aggregated “survivors” into one category those who died ≥ 360 days after most recent PROMIS assessment.
Symptom and Functional Assessment: We assessed symptoms and function with 16 questions from eight PROMIS domains, with 2 items per domain. The 16 items yielded scores for each of the eight domains: anxiety, cognitive function, depression, fatigue, pain interference, physical function, sleep disturbance, and ability to participate in social roles and activities. The PROMIS-Preference (PROPr) Score is the aggregate of seven of the domains (excluding anxiety) and has a meaningful clinically important difference of 0.04 [12, 13].
Analysis
We summarized demographic, clinical, and PROMIS descriptive characteristics for survivors and decedents with univariate and bivariate statistics. Based on inclusion criteria, we conducted a complete-case analysis. We ran chi-square tests and t-tests to compare decedents and survivors on demographic and clinical characteristics. We ran linear regressions adjusting for age, gender, race, and partial Charlson Comorbidity Score to compare decedents and survivors on PROMIS domains and PROPr score. Among decedents, we assessed PROMIS domain and PROPr scores by days before death of the final PROMIS completion using linear regression adjusting for the same covariates. We note that the analyses on the full population of decedents and survivors had a denominator of 51,101, while the analyses on the decedents had a denominator of 1,499. For t-tests using the full sample, we had 80% power to detect a Cohen’s d of 0.07345, accounting for the allocation ratio (N2/N1) resulting in uneven group sizes. For test among decedents, we have 80% power to detect an effect size of 0.0086. Thus, we are extremely powered to detect all effects, and our interpretations account for meaningful clinically important difference. All analyses were conducted in SAS 9.4.
Results
Participant characteristics
We identified 51,101 patients with at least one PROMIS assessment, including 1,499 decedents. Compared to survivors, decedents were less likely to be female (45.36% vs. 60.74%, p < 0.0001), and were older (mean 70.44 vs. 53.63, p < 0.0001); there was no difference by race. As expected, decedents were more likely thank survivors to have all comorbidities, including cognitive impairment (all p < 0.0001). Complete characteristics for survivors and decedents with corresponding chi-square and t-tests are presented in Table 1.
PROMIS completion
Most patients (58.82% of survivors and 68.71% of decedents) completed PROMIS measures at only one timepoint during the study period. The last PROMIS assessment before death for each decedent was most often in the 3–9 months preceding death; there was a drop-off in PROMIS completion in the last two months before death.
PROMIS scores preceding death
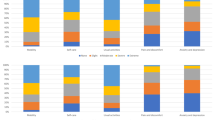
All PROMIS domain scores (anxiety, cognitive function, depression, fatigue, physical function, and ability to participate in social roles and activities) except pain interference and sleep disturbance were significantly worse for decedents compared to survivors in linear regressions controlling for demographic and clinical characteristics. Only physical function (36.33 in decedents vs. 44.23 in survivors, p < 0.0001) and ability to participate in social roles and activities (44.39 in decedents vs. 50.17 in survivors, p < 0.0001) demonstrated a minimal clinically important difference. The overall PROPr score was also statistically and clinically significantly lower among decedents (0.25) compared to survivors (0.36, p < 0.0001) (Table 2).
Among all decedents, five of the eight PROMIS domains were statistically significant in linear regressions when comparing across those who had a final PROMIS assessment closer vs. further from the time of death (Table 3): cognitive function (p = 0.0031), depression (p = 0.0161), fatigue (p = 0.0029), physical function (p < 0.0001), and ability to participate in social roles and activities (p = 0.0004). However, only fatigue (range 54.48–59.38) and physical function (range 33.22–38.38) demonstrated clinically meaningful differences [13]. The overall PROPr score was also statistically significantly lower among decedents 0–29 days before death (0.19) compared to those 360 + days from death (0.29, p < 0.0001) in the multivariable model.
Discussion
While models can help guide clinician practice, predictive models are notably limited in their ability to guide decision making for individual patients due to inherent error and uncertainty at the patient level. In a pragmatic study of real-world clinical implementation of PROMIS measures, we found little practical association between PROMIS scores and mortality. We identified three reasons the PROMIS may not be associated with clinically meaningful differences in most measured domains. First, upon assessment of available longitudinal data, we found very few repeat measures, even in clinics in which nearly all patients completed PROMIS measures at each visit. This may be due to longer-than-expected time between appointments or frequent appointment cancelation, particularly as people approach the end of life. Second, in absolute terms, PROMIS reporting in clinic was even lower in the two months preceding death than in prior months. This may be driven by acute decline (including hospitalization) that keeps patients from attending outpatient neurology appointments and completing PROMIS measures. Likewise, increasing symptom burden may lead to canceled appointments, whereupon PROMIS reports might indicate significant symptom burden. Further, patients may enroll in hospice and appropriately discontinue their usual clinical follow-up before death. Third, though sensitive to longitudinal change in empirical settings, changes in PROMIS may not be sensitive enough to be associated with clinically meaningful decline [14]. It is important that clinical screeners do not over-promise what they are able to reasonably support: while PROMIS can guide symptom management, it may not be able to predict or anticipate outcomes with any reliability. Notable, the domains that were associated with clinically meaningful differences before death were fatigue and physical function, two overarching domains that have been demonstrated to decline in the end-stages of serious illness, along with other functional status [15,16,17]. PROs continue to be one way to assess functional status and fatigue as predictors of mortality.
These findings are important both for clinical prediction and pragmatic research that uses PROs as part of clinical evaluation. Of note, PROMIS was not designed for prediction; it was designed to screen symptoms and prompt a conversation between clinicians and patients about goals of care and effective approaches to symptom management at the patient level [18]. At the population level, the signal is not as pronounced as researchers might anticipate. Although the denominator could be redefined to improve precision and accuracy in the sample, that approach may lead to less pragmatic, generalizable application.
Future work can test the effects of incorporating PROMIS measures, particularly for domains of functional status and fatigue, with other prognostic domains to build more robust prediction models of disease trajectories. Even if a prediction works well in a sample, attention must be paid to whether the prediction is clinically meaningful for care and decision making at the patient level. Still, it remains important to be mindful of the degree to which PROMIS measures are (or are not) incorporated into traditional data sources (e.g., EHRs) used for prediction. Generalizability of models that include PROMIS is limited to institutions that incorporate such measures. To that end, efforts to incorporate patient-reported outcomes into EHRs continues to be of high importance [19].
Limitations
This study has several limitations. First, it was conducted in a single academic medical system with limited patient diversity and may lack generalizability to other health systems with a differing patient mix. Although longitudinal data were limited for this analysis and prevented a quasi-experimental design, these EHR data reflect data available in real-world clinical practice, thereby indicating that patient-reported outcomes may indeed be best used for real-time symptom assessment and treatment rather than for incorporation into prediction models.
Conclusions
Though screeners such as PROMIS provide clinical utility for identifying and treating symptoms, their predictive power was limited in a system of neurology clinics. PROMIS continues to provide real-time symptom screening to support clinicians in identifying and meeting patient needs to support quality of life and may provide an opportunity to capture patient-reported decline, particular with respect to fatigue and functional status, near the end of life.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available because they are protected health information (PHI) from the electronic health record (EHR).
References
Beck JR, Pauker SG. The Markov Process in Medical Prognosis. 2016;3(4):419–458. https://doi.org/10.1177/0272989X8300300403.
Ernecoff NC, Zimmerman S, Mitchell SL, et al. Concordance between goals of Care and Treatment decisions for persons with dementia. J Palliat Med. 2018;21(10):1442–7. https://doi.org/10.1089/jpm.2018.0103.
Stevenson DG, Bramson JS. Hospice Care in the nursing home setting: a review of the literature. J Pain Symptom Manage. 2009;38(3):440–51. https://doi.org/10.1016/j.jpainsymman.2009.05.006.
Centers for Medicare and Medicaid Services. Hospice Care. Medicare.gov.
Yount SE, Cella D, Blozis S, PROMIS®. Standardizing the patient voice in health psychology research and practice. Health Psychol. 2019;38(5):343. https://doi.org/10.1037/HEA0000741.
Diehr P, Williamson J, Patrick DL, Bild DE, Burke GL. Patterns of self-rated health in older adults before and after Sentinel Health events. J Am Geriatr Soc. 2001;49(1):36–44. https://doi.org/10.1046/J.1532-5415.2001.49007.X.
Diehr P, Patrick DL. Trajectories of Health for older adults over time: accounting fully for death. Ann Intern Med. 2003;139(5 II):416–20. https://doi.org/10.7326/0003-4819-139-5_PART_2-200309021-00007.
Cohen-Mansfield J, Skornick-Bouchbinder M, Brill S. Trajectories of end of life: a systematic review. https://doi.org/10.1093/geronb/gbx093.
World Health Organization. ICD-10 : International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd Ed.; 2004.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51. https://doi.org/10.1016/0895-4356(94)90129-5.
Metcalfe D, Masters J, Delmestri A, et al. Coding algorithms for defining Charlson and Elixhauser co-morbidities in Read-coded databases. BMC Med Res Methodol. 2019;19(1):115. https://doi.org/10.1186/s12874-019-0753-5.
Dewitt B, Feeny D, Fischhoff B, et al. Estimation of a preference-based Summary score for the patient-reported outcomes Measurement Information System: the PROMIS®-Preference (PROPr) Scoring System. Med Decis Making. 2018;38(6):683–98. https://doi.org/10.1177/0272989X18776637.
Hanmer J, Dewitt B, Yu L, et al. Cross-sectional validation of the PROMIS-Preference scoring system. PLoS ONE. 2018;13(7). https://doi.org/10.1371/JOURNAL.PONE.0201093.
Schalet BD, Hays RD, Jensen SE, Beaumont JL, Fries JF, Cella D. Validity of PROMIS physical function measured in diverse clinical samples. J Clin Epidemiol. 2016;73:112–8. https://doi.org/10.1016/J.JCLINEPI.2015.08.039.
Reuben DB, Rubenstein LV, Hirsch SH, Hays RD. Value of functional status as a predictor of mortality: results of a prospective study. Am J Med. 1992;93(6):663–9. https://doi.org/10.1016/0002-9343(92)90200-U.
Hardy SE, Studenski SA. Fatigue predicts mortality in older adults. J Am Geriatr Soc. 2008;56(10):1910–4. https://doi.org/10.1111/J.1532-5415.2008.01957.X.
Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. The Journals of Gerontology: Series A. 2010;65A(8):887–95. https://doi.org/10.1093/GERONA/GLQ064.
Cella D, Riley W, Stone A, et al. The patient-reported outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. https://doi.org/10.1016/J.JCLINEPI.2010.04.011.
Grossman LV, Mitchell EG. Visualizing the patient-reported outcomes Measurement Information System (PROMIS) measures for Clinicians and Patients. AMIA Annual Symposium Proceedings. 2017;2017:2289. /pmc/articles/PMC5977703/. Accessed June 20, 2022.
Acknowledgements
N/A.
Correspondence to nernecof@rand.org.
Funding
This project was funding by a grant through the National Institute on Aging (R61AG069776).
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Contributions
All authors contributed to study design, conceptualization, interpretation of results, and text revision. NCE and RW drafted text and conducted the analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work was approved by the RAND Corporation Human Subjects Projection Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ernecoff, N.C., Weir, R., Rodriguez, A. et al. Electronic health record (EHR)-based PROMIS measures among neurology clinic decedents and survivors: a retrospective cohort analysis. Health Qual Life Outcomes 21, 95 (2023). https://doi.org/10.1186/s12955-023-02176-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-023-02176-0