Abstract
Background
Vitamin D deficiency, a common occurrence among pregnant women, is an emerging public health concern worldwide. According to research, prenatal vitamin D deficiency is associated with various complications. This study assessed the vitamin D status of pregnant women in Yanbian, Jilin Province, as well as the correlation and predictive value of their vitamin D levels in relation to gestational length (weeks) and fetal weight, aiming to provide a basis for clinical diagnosis and treatment.
Methods
We conducted a population-based retrospective study involving 510 pregnant women from August 2019 to October 2022. Blood samples were collected at 16–20 weeks of gestation for the detection of serum vitamin D levels. Statistical analyses were performed using SPSS 28.0 and R 4.1.0 software. Multifactorial logistic regression analysis was employed to establish whether each variable was a risk factor for deliveries at ≤ 38 gestational weeks and low fetal weight. These results were used to construct a risk prediction model, and the model’s predictive efficacy was evaluated. Results or differences with p < 0.05 were considered statistically significant.
Results
Multifactorial logistic regression analysis revealed that vitamin D ≤ 14.7 ng/mL(OR: 1.611; 95% CI: 1.120–2.318; P = 0.010), Bone Mineral Density (BMD) T-value ≤-1(OR: 1.540; 95%CI: 1.067–2.223; P = 0.021), and gestational hypertension(OR: 7.173; 95% CI: 1.482–34.724; P = 0.014) were the independent risk factors for deliveries at ≤ 38 gestational weeks. Additionally, vitamin D ≤ 14.7 ng/mL(OR: 1.610; 95%CI: 1.123–2.307; P = 0.009), BMD T-value ≤ -1(OR: 1.560; 95%CI: 1.085–2.243; P = 0.016), and gestational hypertension(OR: 4.262; 95% CI: 1.058–17.167; P = 0.041) were the independent risk factors for low fetal weight (< 3400 g).
Conclusion
This study revealed that low vitamin D levels are an independent risk factor for a short gestational length and low fetal weight. Prenatal low BMD T-value and comorbid hypertensive disorders were also found to increase the risk of a short gestational length and low fetal weight.
Similar content being viewed by others
Introduction
Vitamin D, an essential nutrient closely linked to bone health, immune function, and cellular regulation, is involved in the metabolism of calcium and phosphorus in the body, which is vital during pregnancy. Vitamin D deficiency is a common occurrence among pregnant women in both high- and low-income countries [1]. According to research, prenatal vitamin D deficiency is associated with various complications, such as Pregnancy-Induced Hypertension (PIH) syndrome and Gestational Diabetes Mellitus (GDM). Furthermore, vitamin D deficiency in pregnant women could affect embryonic growth and development, leading to adverse pregnancy outcomes such as Intrauterine Growth Retardation (IUGR) and premature delivery. The effect of vitamin D on the prognosis of mothers and babies is currently being debated. Multiple small intervention studies reported the benefits of increased maternal vitamin D supplementation against several pregnancy complications, including preeclampsia and premature delivery [2, 3]. Conversely, Hossain et al. reported that an intervention of 100 µg vitamin D supplementation had no effect in 193 pregnant women [4].
Preterm labor and low birth weight are leading causes of neonatal mortality. Studies have shown that pregnant women with these outcomes often have inadequate or deficient serum 25-hydroxyvitamin D [25(OH)D], suggesting a correlation between serum 25(OH)D levels, gestational week, and neonatal weight. However, the predictive value of serum 25(OH)D levels remains unclear. Vitamin D deficiency during pregnancy is reported to increase the risk of low birth weight and neonatal skeletal and respiratory disorders, as the fetal serum level depends entirely on the mother’s 25(OH)D level [5]. Low birth weight (LBW) is strongly correlated with neonatal mortality worldwide.A prospective cohort study using the NICHD Global Maternal and Child Health Research Network developed a predictive model for LBW and discovered that mothers of LBW children were less likely to take calcium or vitamin supplements compared with mothers of non-LBW children (14 vs. 83%) [6]. Satoshi Mizuno et al. also created an early prediction model for LBW infants utilizing the XGBoost model, which indicated that daily fish intake (e.g., tuna and eel) was highly significant [7]. This correlation may be indirectly related to maternal serum vitamin D levels.
Few studies have examined the relationship between serum 25(OH)D levels, gestational weeks of delivery, and neonatal weight in China. This study aimed to analyze the distribution characteristics of serum 25(OH)D in pregnant women in Yanbian, Jilin Province. We screened and analyzed vitamin D levels, gestational weeks, and neonatal weight, among other clinical parameters, to explore their relationships. Factors affecting gestational weeks and neonatal weight were also examined, providing valuable predictive indicators for guiding targeted maternal nutrient supplementation in clinical practice.
Materials and methods
Study design and population
To determine the serum vitamin D levels in pregnant women in the Yanbian region, this population-based retrospective study was conducted in Tumen, Yanbian Prefecture. The study population comprised pregnant women who were carded and underwent regular pregnancy check-ups at the Maternal and Child Health and Family Planning Service Centre in Tumen City from August 2019 to October 2022. Data on the deliveries of these pregnant women, as well as the newborns, were recorded. The inclusion criteria were as follows: (1) Pregnant women residing in the Tumen City area; (2) Pregnant women with regular pregnancy check-ups at the Maternal and Child Health and Family Planning Service Centre in Tumen City and with complete pregnancy outcomes; (3) Pregnant women aged 19–42 years; and (4) Pregnant women with complete information on serum vitamin D values at 16–20 weeks of gestation. On the other hand, the exclusion criteria were as follows: (1) Patients with Diabetes Mellitus (DM), Hypertension (HTN), hypothyroidism, cardiac diseases, hepatic or renal insufficiency, and concomitant psychiatric disorders; (2) Patients with incomplete clinical information prior to pregnancy; and (3) Patients who presented with fetal anomalies, intrauterine death, or abortions. After screening based on the above criteria, 510 eligible pregnant women were included (Table 1). The study protocol was approved by the local medical Ethics Committee.
Sample size determination: In this study, gestational age ≤ 38 weeks and birth weight < 3400 g were used as dependent variables for binary logistic regression. Following the principle of N = 100 + 50i (i = independent variables) [8], the formula will produce 450 subjects when there are 7 independent variables. All eligible samples within the study period were collected, and the current sample size meets the minimum requirement.
Testing methods
Vitamin D testing was performed during routine prenatal visits at 16–20 weeks of gestation to spare the patients the inconvenience of multiple blood draws. Blood samples were strictly collected in the morning on an empty stomach. The blood samples were centrifuged, and the isolated serum was sent to a third-party testing facility (Changchun KingMed Testing Centre) for “Tandem Mass Spectrometry.” Vitamin D levels were determined based on serum 25-(OH)D levels. The test facility set the normal range of vitamin D values at 30–100 ng/mL. Vitamin D insufficiency is defined as a 25(OH)D concentration of 21–29 ng/ml (51–74 nmol/L), whereas vitamin D deficiency is defined as a 25(OH)D concentration < 20 ng/mL (50 nmol/L) (Endocrine Society Clinical Practice Guidelines) [9]. However, there is no clear definition of vitamin D deficiency in pregnant women. Therefore, given the small number of pregnant women with normal vitamin D values in this study, the participants were divided into two groups based on a median vitamin D value of 14.7 ng/mL.
Predictive model development
To evaluate the predictive value for outcomes such as gestational length and neonatal weight, a logistic regression model was employed, represented by the following formula:
P = ex/(1 + ex)
where P denotes the probability of the outcome occurring (e.g., short gestational length or low fetal weight), and x is defined as:
x = β0 + β1 × 1 + β2 × 2 +…+ βn Xn
In this equation:
β0 is the intercept.
β1, β2, …, βn are the coefficients for the predictor variables X1, X2, …, Xn.
X1, X2, …, Xn represent the predictor variables, which include factors such as maternal 25(OH)D levels, maternal age, body mass index (BMI), presence of PIH, bone mineral density (BMD), gestational anemia, and gestational diabetes mellitus (GDM) status.
Model Fitting and Validation: The model was fitted using maximum likelihood estimation in SPSS (version 28.0). Model performance was evaluated using the area under the receiver operating characteristic curve (AUC), sensitivity, and specificity.
Explanation of the Model: The logistic regression model transforms the linear combination of predictor variables x into a probability P using the logistic function. The logistic function, ensuring P is always between 0 and 1.
Interpretation of Results: The coefficients ( β ) represent the change in the log odds of the outcome for a one-unit increase in the corresponding predictor variable. A positive coefficient indicates an increased probability of the outcome, while a negative coefficient indicates a decreased probability. For example, a positive coefficient for low maternal 25(OH)D levels ( β1 ) suggests that lower vitamin D levels increase the chances of a short gestational length or low fetal weight.
Statistical analysis
Statistical analyses were performed using SPSS 28.0 and R 4.1.0 software. Count data were expressed as frequencies (N) and percentages (%), and the chi-square test was used for inter-group comparisons. Multifactorial logistic regression analysis was employed to establish whether age, pre-pregnancy Body Mass Index (BMI), vitamin D, Bone Mineral Density, gestational anemia, GDM, and PIH were risk factors for deliveries at ≤ 38 gestational weeks and low fetal weight. These results were used to construct a risk prediction model, and the model’s predictive efficacy was evaluated using the Hosmer-Lemeshow goodness-of-fit test, Receiver Operating Characteristic (ROC) curves, and calibration curves. Results or differences with P < 0.05 were considered statistically significant.
Results
Description of the study population
Table 1 summarizes the basic information of the 510 participants included herein. The median vitamin D value was 14.7 ng/mL, and ~ 50% of patients had below normal BMD values. The median newborn weight was 3400 g, and about two-thirds of all pregnancies were delivered at > 38 weeks of gestation.
Based on the maternal vitamin D status at 16–20 weeks of gestation, the participants were divided into two groups: Vitamin D > 14.7 ng/mL and vitamin D ≤ 14.7 ng/mL (Table 2). Compared to the vitamin D ≤ 14.7 ng/mL group, the vitamin D > 14.7 group exhibited a significantly lower gestational anemia prevalence (12.94% vs. 20.39%, P = 0.024), as well as a lower incidence of deliveries at ≤ 38 weeks of gestation (37.65% vs. 48.63%, P = 0.012), fetal weight < 3400 g (40.78% vs. 52.94%, P = 0.006), and BMD (at 16–20 weeks of gestation) ≤-1 (38.04% vs. 48.63%, P = 0.016), at the time of delivery.
Data from patients tested at 16–18 and 19–20 weeks of gestation were subjected to the chi-square test to determine whether the specific time of blood draw in the fourth month of pregnancy affected vitamin D values. Table 3 shows the correlation analysis between the time of blood draw and vitamin D levels, indicating that there was no correlation (P > 0.05).
Analysis of risk factors for delivery at ≤ 38 weeks of gestation and development of the predictive model
Among the 510 pregnant women included herein, there were 290 and 220 cases with gestational periods of >38 weeks and ≤ 38 weeks, respectively. Compared to the group with a gestational period of ≤ 38 weeks, the group with a gestational period of >38 weeks had significantly higher vitamin D and BMD values and a significantly lower PIH incidence rate (P < 0.05) (Table 4).
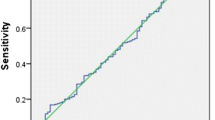
Univariate and multivariate logistic regression analyses were performed using ‘whether or not the gestational week was ≤ 38 weeks’ as the dependent variable. Multifactorial logistic regression analysis results revealed that vitamin D ≤ 14.7 ng/mL [Odds Ratio (OR): 1.611; 95% Confidence Interval (CI): 1.120–2.318; P = 0.010), BMD T-value ≤-1 (OR: 1.540; 95%CI: 1.067–2.223; P = 0.021), and gestational hypertension (OR: 7.173; 95% CI: 1.482–34.724; P = 0.014) were independent risk factors for delivery at ≤ 38 weeks of gestation, whereas anaemia was a protective factor for delivery at ≤ 38 weeks of gestation (OR: 0.590; 95%CI: (0.356–0.977); P = 0.040) (Table 4). A prediction model was constructed based on these results, and ROC curves were plotted [Fig. 1; AUC = 0.618 (0.575–0.661), sensitivity = 77.73%, and specificity = 39.66%]. Model calibration was assessed using the Hosmer-Lemeshow test (χ²=1.386, P = 0.986) (Fig. 2), indicating no significant difference between actual observations and predictions.
Analysis of risk factors for fetal weight < 3400 g and development of the predictive model
Among the 510 pregnant women included herein, 271 and 239 cases had fetal weights of ≥ 3400 g and < 3400 g, respectively. Compared to the group with a fetal weight of < 3400 g, the group with a foetal weight of ≥ 3400 g had significantly higher vitamin D and BMD values (P < 0.05, Table 5).
Univariate and multivariate logistic regression analyses were performed with ‘fetal weight < 3400 g’ as the dependent variable. The analysis revealed that vitamin D ≤ 14.7 ng/mL (OR: 1.610; 95%CI: 1.123–2.307; P = 0.009), BMD T-value ≤-1 (OR: 1.560; 95%CI: 1.085–2.243; P = 0.016), and gestational hypertension (OR: 4.262; 95% CI: 1.058–17.167; P = 0.041) were the independent risk factors for a fetal weight of < 3400 g (Table 5). A prediction model was constructed, and ROC curves were plotted [Fig. 3; AUC = 0.616 (0.572–0.659), sensitivity = 78.24%, and specificity = 40.59%]. Figure 4 shows the calibration curves. The Hosmer-Lemeshow test results (χ²=5.024, P = 0.541) indicated no significant difference between actual observations and predictions.
Discussion
This study comprised 510 pregnant women, and the median vitamin D value among participants was 14.7 ng/mL (well below the normal range), implying that low vitamin D levels are an independent risk factor for short gestational length and low fetal weight. Women with vitamin D levels below 14.7 ng/mL had a 1.61 times higher risk of delivering a small-for-gestational-age or low-birth-weight fetus. Lower mid-pregnancy 25(OH)D levels were linked to higher incidences of low fetal weight and small-for-gestational-age births. Ruth Morley conducted an observational study involving 374 pregnant women and found similar results [10]. Additionally, low BMD T-scores and comorbid PIH increased the risk of short gestational length and low fetal weight, while anemia showed a protective association against short gestational length. Therefore, mid-pregnancy 25(OH)D levels have predictive value for gestational length and neonatal weight, emphasizing the importance of vitamin D supplementation during pregnancy.
Vitamin D metabolism and molecular regulation during pregnancy
Vitamin D is crucial during pregnancy, with 1,25(OH)2D levels significantly increasing, doubling in the first trimester and continuing to rise throughout pregnancy, then declining after delivery. Vitamin D is converted in the liver to 25(OH)D, the main circulating form, and then to the active hormone 1,25(OH)2D primarily in the kidneys, as well as in the placenta and maternal immune cells [10]. The enzyme CYP27B1, which converts 25(OH)D to 1,25(OH)2D, is expressed in the placenta [11, 12]. Vitamin D receptors (VDR) are present in trophoblast cells and decidua [13], allowing placental cells to respond to locally synthesized 1,25(OH)2D. VDR binding to 1,25(OH)2D regulates genes involved in calcium and phosphorus metabolism, immune function, cell proliferation, and differentiation, emphasizing vitamin D’s importance in placental physiology.
Vitamin D binding protein (VDBP) is the main carrier for vitamin D and its metabolites, maintaining vitamin D homeostasis and acting as an immunomodulator for healthy pregnancies. VDBP levels increase during pregnancy [14], likely influenced by hormones like progesterone [15], peaking at 40–50% higher in late pregnancy, which can decrease free 25(OH)D levels and affect vitamin D availability [16]. This highlights the importance of adequate vitamin D intake during pregnancy.
Genetic polymorphisms in vitamin D metabolizing enzymes and VDBP can affect enzyme activity, influencing the production and degradation of 25(OH)D and 1,25(OH)2D, leading to individual differences in vitamin D status. For example, mothers with the rs12512631 “C” allele have lower 25(OH)D levels in maternal and cord blood, associated with decreased infant birthweight [17]. Polymorphisms in VDBP also impact vitamin D status and the effectiveness of supplementation, increasing the risk of vitamin D-dependent diseases and explaining varying responses among individuals [18].
Association of 25(OH)D levels in pregnant women with neonatal weight and gestational length
The fetus is entirely dependent on maternal vitamin D stores. 25(OH)D is transferred from mother to fetus across the placenta in early pregnancy, with levels in cord blood at birth approximately 50-80% of maternal serum values [19]. A study of 7098 mother-child pairs showed that low maternal 25(OH)D concentrations are associated with fetal growth restriction and increased preterm birth risk [20], consistent with our findings. Vitamin D is crucial for fetal growth, particularly bone growth and mineralization. Major bone mineralization occurs in late pregnancy [21], and fetal weight gain during this period mainly results from fat mass accumulation and bone density, both regulated by vitamin D.
Low vitamin D levels increase the risk of short gestational length due to its role in immune response regulation and inflammatory processes. An Irish study found that vitamin D status is associated with uteroplacental dysfunction, with 25(OH)D > 75 nmol/L having a protective effect [22]. Higher vitamin D levels are linked to more live births and fewer miscarriages [23]. Vitamin D’s anti-inflammatory properties suggest that deficiency could lead to placental inflammatory lesions [24, 25], affecting blood supply and fetal growth, potentially inducing short gestational length [26]. Vitamin D also helps protect the fetus from maternal immune attacks, and deficiency could lead to immune imbalances, increasing the risk of short gestational length [27, 28]. Additionally, vitamin D is vital for muscle function, including myometrium stability [29,30,31,32,33,34], and deficiency might disrupt uterine muscle balance [35,36,37,38], increasing the risk of short gestational length.
Maternal vitamin D levels are positively correlated with neonatal birth weight. Vitamin D regulates calcium and phosphorus metabolism, crucial for fetal growth and development. Vitamin D deficiency can lead to calcium metabolism disorders [39], affecting bone development. Adequate vitamin D and calcium intake are necessary for bone homeostasis and multiple prenatal physiological processes [9, 29, 40, 41]. Although the fetus may initiate a series of compensatory mechanisms to meet its mineral requirements for rapid growth, they could lead to fetal intrauterine growth restriction and low birth weight in the long term [42]. An Iranian study also linked maternal calcium intake with birth weight gain [43,44,45]. Vitamin D is also involved in regulating endocrine systems, including insulin secretion and blood pressure control [14].Deficiency has been linked with gestational diabetes and preeclampsia [46, 47], which could indirectly lead to preterm labor or fetal growth restrictions, resulting in low neonatal weight.
In summary, vitamin D sufficiency is crucial for a normal pregnancy. Deficiency can affect placental health, fetal nutrition, and physiological homeostasis, increasing the risk of short gestational length and low neonatal weight. Ensuring adequate vitamin D intake and maintaining appropriate serum levels during pregnancy are imperative for maternal and fetal health.
Predictive value of mid-pregnancy 25(OH)D levels for neonatal weight and gestational length
To evaluate the predictive value of 25(OH)D levels for gestational length at delivery and neonatal birth weight, ROC curve analysis indicated that 25(OH)D has predictive value for both outcomes (AUC > 0.6, P < 0.05). Although the AUC values of 0.618 (0.575–0.661) and 0.616 (0.572–0.659) are not ideal, the high sensitivity of the model (78.24% and 77.73%) shows its potential value in clinical applications. This indicates that the model effectively detects cases with actual issues. It assists in identifying high-risk pregnant women early, leading to timely interventions and improved pregnancy outcomes. Key variables in the model, such as vitamin D ≤ 14.7 ng/mL, low bone mineral density T-value, and gestational hypertension, significantly influenced gestational length and neonatal weight. The independent risk contributions of these variables (e.g., OR of 1.610 for vitamin D ≤ 14.7 ng/mL) were crucial, supporting the critical role of vitamin D in pregnancy health. By improving these variables (e.g., vitamin D supplementation, managing gestational hypertension), clinicians may be able to help improve pregnancy outcomes.
Existing research also supports this conclusion. For example, two meta-analyses by Qin LL and Aghajafari demonstrated that low vitamin D levels were significantly associated with low fetal weight and shorter gestation periods [48, 49]. Further, it is emphasized that delivery before 39 weeks is associated with a higher risk of poor neonatal outcomes [50, 51]. The model in this study highlights the high risk of delivery before 38 weeks, particularly for pregnant women with vitamin D levels below 14.7 ng/mL. This underscores the importance of maintaining adequate vitamin D levels during pregnancy in clinical practice.
Although current models are not precise enough for a final diagnosis. Its high sensitivity and the established correlation between vitamin D and pregnancy outcomes suggest that it could be used as a screening tool in clinical practice. It is recommended that the model be used in conjunction with other clinical assessments and tests This will lead to comprehensive diagnosis and improved management and prevention of adverse pregnancy outcomes.
Association of BMD, PIH and anemia with neonatal weight and gestational length
In this study, women with PIH exhibited a higher incidence of low fetal weight and small for gestational age at delivery. This finding is consistent with previous international studies [52]. This could be due to reduced blood perfusion to the uteroplacenta caused by vasoconstriction in hypertensive pregnant women, leading to intrauterine growth restriction, short gestational length, and consequently, low neonatal weight [53].
We also found that BMD is an independent risk factor for a short gestational length (weeks) and low fetal weight. However, there is limited literature on this topic, necessitating additional research to further verify the relationship of BMD with gestational length and fetal weight.
Maternal anemia is often seen as a risk factor for adverse pregnancy outcomes. However, we found a positive correlation between maternal anemia and gestational length. This might be due to uncontrolled confounding variables. For instance, pregnant women in the study region may have lower preterm birth rates and higher anemia incidence due to specific lifestyle, dietary habits, or healthcare systems. Anemic pregnant women might also receive more aggressive nutritional interventions and support, such as increased intake of iron-rich foods and supplements, improving their overall nutritional status and reducing short gestational length risk. Additionally, stricter medical monitoring and timely intervention might help maintain a normal gestational length. Iron is involved in the regulation of immune function and inflammatory responses in the body [54]. We speculate that moderate iron deficiency might reduce excessive inflammatory responses, indirectly lowering short gestational length risk through specific mechanisms. However, this phenomenon requires further scientific research and is not intended to promote anemia in pregnant women. Current knowledge still regards prenatal anemia as a significant health issue that should be actively prevented and addressed.
Limitations and future directions
This study has several limitations. First, the sample was drawn exclusively from pregnant women receiving prenatal care at the Tumen Maternal and Child Health Hospital in Yanbian Prefecture, which limits the generalizability of the conclusions due to regional and individual variations. Second, as a retrospective analysis relying on clinical records and follow-up outcomes, there was no control over the study process, potentially introducing biases. Third, the small sample size limited the number of pregnant women with normal vitamin D levels and hindered categorization according to guideline definitions, potentially compromising reliability. The small PIH cohort also led to wider confidence intervals in model predictions, indicating a higher degree of uncertainty and the need for validation with larger datasets. Additionally, due to the lack of external validation, it cannot be confirmed whether the model will maintain its predictive accuracy on new data. Future research should include independent datasets collected from multiple sources to evaluate the model’s external validity.
Future studies must address these issues by expanding sample sizes, conducting prospective trials, and ensuring broader population representation to enhance validity and applicability. Future studies should also focus on different periods of pre-conception and pregnancy to correct vitamin D deficiencies or maintain optimal levels. Despite these limitations, understanding the importance of vitamin D during pregnancy has significantly advanced over the past few decades.
Conclusions
This study highlights the significant role of mid-pregnancy vitamin D levels in determining neonatal birth weight and gestational age of delivery. The findings indicate that vitamin D insufficiency, with median levels of 14.7 ng/mL, constitutes an independent risk factor for shorter gestational periods and lower fetal weight. These results underscore the necessity and importance of routine monitoring and supplementation of vitamin D during pregnancy to optimize maternal and fetal health.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- PIH:
-
Pregnancy-Induced Hypertension
- GDM:
-
Gestational Diabetes Mellitus
- BMD:
-
Bone Mineral Density
- BMI:
-
Body Mass Index
- LBW:
-
Low Birth Weight
- DM:
-
Diabetes Mellitus
- HTN:
-
Hypertension
- AUC:
-
Area Under the Receiver Operating Characteristic Curve
- VDR:
-
Vitamin D Receptor
- VDBP:
-
Vitamin D Binding Protein
References
Saraf R, et al. Global summary of maternal and newborn vitamin D status - a systematic review. Matern Child Nutr. 2016;12(4):647–68.
Ali AM, et al. Effect of vitamin D3 supplementation in pregnancy on risk of pre-eclampsia - randomized controlled trial. Clin Nutr. 2019;38(2):557–63.
McDonnell SL, et al. Maternal 25(OH)D concentrations ≥ 40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PLoS ONE. 2017;12(7):e0180483.
Hossain N, et al. Obstetric and neonatal outcomes of maternal vitamin D supplementation: results of an open-label, randomized controlled trial of antenatal vitamin D supplementation in Pakistani women. J Clin Endocrinol Metab. 2014;99(7):2448–55.
Yu H, Fu J, Feng Y. Utility of umbilical cord blood 25-hydroxyvitamin D levels for predicting bronchopulmonary dysplasia in preterm infants with very low and extremely low birth weight. Front Pediatr. 2022;10:956952.
Patterson JK, et al. Building a predictive model of low birth weight in low- and middle-income countries: a prospective cohort study. BMC Pregnancy Childbirth. 2023;23(1):600.
Mizuno S, et al. Establishment of the early prediction models of low-birth-weight reveals influential genetic and environmental factors: a prospective cohort study. BMC Pregnancy Childbirth. 2023;23(1):628.
Bujang MA, et al. Sample size guidelines for logistic regression from Observational studies with large Population: emphasis on the Accuracy between statistics and parameters based on Real Life Clinical Data. Malays J Med Sci. 2018;25(4):122–30.
Holick MF, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Ganguly A, et al. Vitamin D, the placenta and early pregnancy: effects on trophoblast function. J Endocrinol. 2018;236(2):R93–103.
Zehnder D, et al. The ontogeny of 25-hydroxyvitamin D(3) 1alpha-hydroxylase expression in human placenta and decidua. Am J Pathol. 2002;161(1):105–14.
Tamblyn JA, et al. Dysregulation of maternal and placental vitamin D metabolism in preeclampsia. Placenta. 2017;50:70–7.
Evans KN, et al. Vitamin D and placental-decidual function. J Soc Gynecol Investig. 2004;11(5):263–71.
Bouillon R, et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr Rev. 2019;40(4):1109–51.
Zhang JY, et al. Impact of pregnancy on vitamin D status: a longitudinal study. Br J Nutr. 2014;112(7):1081–7.
Karras SN, et al. Deconvoluting the Biological roles of vitamin D-Binding protein during pregnancy: a both clinical and theoretical challenge. Front Endocrinol (Lausanne). 2018;9:259.
Chun SK, et al. Effects of maternal genetic polymorphisms in vitamin D-binding protein and serum 25-hydroxyvitamin D concentration on infant birth weight. Nutrition. 2017;35:36–42.
Moon RJ, et al. Response to Antenatal Cholecalciferol supplementation is Associated with Common vitamin D-Related genetic variants. J Clin Endocrinol Metab. 2017;102(8):2941–9.
Ortigosa GS, et al. [Sociodemographic factors related to plasma concentrations of 25-OH vitamin D and PTH in cord blood]. Rev Esp Salud Publica. 2015;89(1):75–83.
Miliku K, et al. Maternal vitamin D concentrations during pregnancy, fetal growth patterns, and risks of adverse birth outcomes. Am J Clin Nutr. 2016;103(6):1514–22.
Ryan BA, Kovacs CS. Calciotropic and phosphotropic hormones in fetal and neonatal bone development. Semin Fetal Neonatal Med. 2020;25(1):101062.
Kiely ME, et al. Vitamin D status is associated with uteroplacental dysfunction indicated by pre-eclampsia and small-for-gestational-age birth in a large prospective pregnancy cohort in Ireland with low vitamin D status. Am J Clin Nutr. 2016;104(2):354–61.
Mumford SL, et al. Association of preconception serum 25-hydroxyvitamin D concentrations with livebirth and pregnancy loss: a prospective cohort study. Lancet Diabetes Endocrinol. 2018;6(9):725–32.
Chen YH, et al. Gestational vitamin D deficiency causes placental insufficiency and fetal intrauterine growth restriction partially through inducing placental inflammation. J Steroid Biochem Mol Biol. 2020;203:105733.
Bhutia SK. Vitamin D in autophagy signaling for health and diseases: insights on potential mechanisms and future perspectives. J Nutr Biochem. 2022;99:108841.
Wilson RL, et al. Reduced Dietary Calcium and Vitamin D Results in Preterm Birth and altered placental morphogenesis in mice during pregnancy. Reprod Sci. 2020;27(6):1330–9.
Sykes L et al. The Th1:th2 dichotomy of pregnancy and preterm labour. Mediators Inflamm, 2012. 2012: p. 967629.
Zahran AM, Zharan KM, Hetta HF. Significant correlation between regulatory T cells and vitamin D status in term and preterm labor. J Reprod Immunol. 2018;129:15–22.
Mendes MM, Botelho PB, Ribeiro H. Vitamin D and musculoskeletal health: outstanding aspects to be considered in the light of current evidence. Endocr Connect, 2022. 11(10).
Cermisoni GC et al. Vitamin D and endometrium: a systematic review of a neglected area of Research. Int J Mol Sci, 2018. 19(8).
Agoncillo M, Yu J, Gunton JE. The role of vitamin D in skeletal muscle repair and regeneration in animal models and humans: a systematic review. Nutrients, 2023. 15(20).
Vienonen A, et al. Expression of nuclear receptors and cofactors in human endometrium and myometrium. J Soc Gynecol Investig. 2004;11(2):104–12.
Grzesiak M et al. Vitamin D(3) metabolic enzymes in the Porcine Uterus: expression, localization and autoregulation by 1,25(OH)(2)D(3) in Vitro. Int J Mol Sci, 2022. 23(7).
Fernando M et al. Vitamin D-Binding protein in pregnancy and Reproductive Health. Nutrients, 2020. 12(5).
Thota C, et al. Vitamin D regulates contractile profile in human uterine myometrial cells via NF-κB pathway. Am J Obstet Gynecol. 2014;210(4):e3471–34710.
Amiri M, et al. Mode of delivery and maternal vitamin D deficiency: an optimized intelligent bayesian network algorithm analysis of a stratified randomized controlled field trial. Sci Rep. 2023;13(1):8682.
Thomsen CR, et al. Vitamin D and the risk of dystocia: a case-control study. PLoS ONE. 2020;15(10):e0240406.
Cooper C, et al. Maternal gestational vitamin D supplementation and offspring bone health (MAVIDOS): a multicentre, double-blind, randomised placebo-controlled trial. Lancet Diabetes Endocrinol. 2016;4(5):393–402.
Vanchinathan V, Lim HW. A dermatologist’s perspective on vitamin D. Mayo Clin Proc. 2012;87(4):372–80.
Hofmeyr GJ, et al. Prepregnancy and early pregnancy calcium supplementation among women at high risk of pre-eclampsia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2019;393(10169):330–9.
Fleet JC, Vitamin D-M. Regul Intestinal Calcium Absorpt Nutrients, 2022. 14(16).
Mosha D, et al. Dietary iron and calcium intakes during pregnancy are associated with lower risk of prematurity, stillbirth and neonatal mortality among women in Tanzania. Public Health Nutr. 2017;20(4):678–86.
Khoushabi F, Saraswathi G. Impact of nutritional status on birth weight of neonates in Zahedan City, Iran. Nutr Res Pract. 2010;4(4):339–44.
Gallo S, et al. Vitamin D supplementation during pregnancy: an Evidence Analysis Center Systematic Review and Meta-analysis. J Acad Nutr Diet. 2020;120(5):898–e9244.
Souza R et al. The Influence of Nutrients Intake during Pregnancy on Baby’s Birth Weight: A Systematic Review. J Trop Pediatr, 2021. 67(2).
Mahendra A, Fall C. Maternal vitamin D deficiency and GDM risk: evidence for the case of investing more attention in antenatal clinics. Proc Nutr Soc, 2021: p. 1–7.
Wang L, et al. Serum vitamin D deficiency and risk of gestational diabetes mellitus: a meta-analysis. Arch Med Sci. 2020;16(4):742–51.
Qin LL et al. Does maternal vitamin D Deficiency increase the risk of Preterm Birth: a Meta-analysis of Observational studies. Nutrients, 2016. 8(5).
Aghajafari F, et al. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. BMJ. 2013;346:f1169.
Chiossi G, et al. Timing of delivery and adverse outcomes in term singleton repeat cesarean deliveries. Obstet Gynecol. 2013;121(3):561–9.
Oshiro BT, et al. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804–11.
Lake EA, Olana FR. Low Birth Weight and its Associated factors among newborns delivered at Wolaita Sodo University Teaching and Referral Hospital, Southern Ethiopia, 2018. Int J Pediatr. 2019;2019:p4628301.
Amaral LM, et al. Pathophysiology and current clinical management of Preeclampsia. Curr Hypertens Rep. 2017;19(8):61.
Lanser L et al. Physiology and inflammation driven pathophysiology of Iron Homeostasis-mechanistic insights into Anemia of inflammation and its treatment. Nutrients, 2021. 13(11).
Acknowledgements
The authors would like to thank all the reviewers who participated in the review, as well as MJEditor (www.mjeditor.com) for providing English editing services during the preparation of this manuscript.
Funding
This study was supported by Jilin Science and Technology Agency funding (20230508067RC).
Author information
Authors and Affiliations
Contributions
QC, YQC, and RXL were involved in the study conception and design. QC participated in data acquisition, analysis, and interpretation. QC and YL wrote the manuscript. All authors have read and approved the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Second Hospital of Jilin University[(2024) Annual Review No. (156)]. This retrospective non-interventional study has applied to the Ethics Committee for a waiver of written informed consent from the patients in this study. The use of patient data was confidential and in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Q., Chu, Y., Liu, R. et al. Predictive value of Vitamin D levels in pregnant women on gestational length and neonatal weight in China: a population-based retrospective study. Reprod Biol Endocrinol 22, 102 (2024). https://doi.org/10.1186/s12958-024-01276-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-024-01276-w