Abstract
Background
Extracorporeal membrane oxygenation (ECMO) is applied in patients with respiratory or cardiopulmonary failure, but bleeding is a frequent complication contributing to the high mortality rates in this patient collective. A major factor predisposing patients to bleeding events is an acquired von Willebrand syndrome (aVWS). So far, specific treatment options for this phenomenon are lacking. In hereditary von Willebrand disease (VWD), treatment with recombinant or plasma-derived von Willebrand factor (rVWF or pVWF) is common practice. Closure time measured by the Platelet Function Analyser-200 (PFA-200) is an established assay to detect defects in primary hemostasis and the method is useful to monitor the effect of hemostatic therapy. The aim of this study was to assess the effect of recombinant (rVWF) vs. plasma-derived von Willebrand factor (pVWF) on closure times measured by PFA in blood obtained from ECMO patients with aVWS.
Methods
Blood was sampled from thirteen patients receiving extracorporeal membrane oxygenation and three patients with hereditary VWD. Diagnosis of aVWS was made by conventional coagulation parameters and by multimeric structure analysis. PFA analysis of blood spiked with rVWF or pVWF was performed.
Results
Thirteen patients receiving ECMO were recruited. Ten patients survived and three patients suffered major bleeding complications. PFA closure times in ECMO patients with aVWS spiked with rVWF were significantly shorter at all concentrations than with pVWF (e.g., rVWF vs. pVWF: 1 U/ml: 150.4 ± 21.7 s vs. 263.8 ± 11.7 s; 4 U/ml: 97.8 ± 9.8 s vs. 195.8 ± 15.4 s, p<0.001). PFA closure times were also significantly shorter in three patients with hereditary VWD treated with rVWF compared to pVWF (e.g., 1 U/ml rVWF vs. pVWF: 73.7±1.33 s vs. 231.3±43.4 s, p<0.01)
Conclusion
In summary, this study shows that rVWF compared to pVWF more effectively reduced PFA closures times in blood samples of ECMO patients with aVWS. Higher doses of VWF are needed to normalize PFA closure time in blood samples of patients with ECMO-induced aVWS compared to hereditary VWD. These data support the use of PFA-200 to monitor hemostatic effects in a future clinical trial involving ECMO patients with aVWS.
Similar content being viewed by others
Background
Extracorporeal membrane oxygenation (ECMO) is being increasingly used in patients with respiratory or cardiopulmonary failure [1]. Although many patients benefit from ECMO, mortality in patients receiving this treatment is high, ranging between 40-60 % depending on the cannulation strategy and underlying condition [2, 3]. Apart from the primary disease, bleeding is a leading cause of morbidity and mortality in ECMO patients. The so-called ECMO-induced coagulopathy is responsible for these bleeding events and has a complex pathogenesis [4, 5]. Exposure of blood components to high shear stress and large extracorporeal surfaces in the ECMO circuit affects multiple components of the coagulation system. For example, patients are predisposed to bleeding by the resulting ECMO-induced thrombocytopenia [6], platelet dysfunction [7], hyperfibrinolysis [8] and acquired von Willebrand syndrome (aVWS) [9, 10]. In particular, the aVWS is characterized by a loss of high molecular weight von Willebrand factor (VWF) multimers, which is most likely caused by shear stress in the ECMO circuit and possibly enhanced cleavage by a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13) [11]. Acquired VWS needs to be differentiated from the hereditary forms of von Willebrand disease (VWD) as it usually ceases after weaning from ECMO [9], whereas the hereditary forms are chronic diseases. Furthermore, there are established treatment options for the hereditary forms of VWD, for example, recombinant and plasma-derived VWF (rVWF and pVWF) [12, 13], but data for the treatment of aVWS in ECMO patients is insufficient.
Since VWF is essential for primary hemostasis, aVWS can be sensitively detected by the Platelet Function Analyzer PFA-200. Its advantages include simplicity, ease of execution and high sensitivity compared to measurement of bleeding time [14, 15].
The aim of this study was to assess the effect of recombinant vs. plasma-derived von Willebrand factor on closure times measured by PFA in blood obtained from ECMO patients with aVWS.
Methods
Patient recruitment and blood sampling
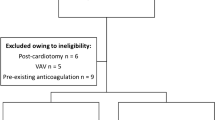
Patients receiving veno-arterial (VA) or veno-venous (VV) ECMO were recruited from the medical intensive care units of the University Hospital in Freiburg, Germany, from October until December 2021. One blood sample per patient was obtained within an interval 12-60 hours (h) after initiation of ECMO. As defined by the study protocol, the following exclusion criteria applied: hemoglobin (Hb) level <8 g/dl, platelet count < 100 G/l, hematological malignancies. All study participants were older than 18 years. Using an arterial line, blood was sampled slowly into tubes containing buffered 3.8% tri-sodium-citrate (Sarstedt, Germany)
Clinical and laboratory parameters from ECMO patients were gathered from the electronic patient data management system closest to the time point of blood sampling.
Major bleeding was defined as previously described [16]. Patients were counted as survivors if they were discharged from the intensive care unit.
As part of a limited case series, patients with hereditary VWD were also recruited by our local outpatient clinic. Blood was taken slowly into by antecubital vein puncture at one time point. Patients had not taken any medication in the past 14 days.
The buffered citrated whole blood was left untreated (“blank” or “untreated” sample), or supplemented with increasing concentrations (final concentration 0.5-4 U/ml) of recombinant (Vonicog alfa, Takeda Pharmaceutical, Japan) or plasma-derived VWF (Haemate ®, CSL Behring, Germany) (“spiked” whole blood). The assays were then carried out in these “untreated or spiked” samples.
ECMO management
Nomenclature used in this paper is based on recommendations by the Extracorporeal Life Support Organization [17, 18]. Patients receiving ECMO were managed as previously described [7, 19, 20]. In brief, ECMO placement was indicated by an experienced ECMO physician. ECMO was placed by percutaneous cannulation. The configuration for VA ECMO was ‘V21-23f - A15-17f‘ (femoral venous drainage to femoral arterial return; venous cannula diameters were 21-23 French (Fr), arterial cannula diameters were 15-17 Fr). The configuration for VV ECMO was ‘(dl27-31) Vj-V’ (dual-lumen jugular venous drainage to venous return; diameters ranging between 27-31 Fr).
If required, ECMO patients received red blood cell transfusions to maintain hemoglobin levels above 8 g/dl. Patients without signs of bleeding or thrombosis (including the ECMO circuit) were anticoagulated with unfractionated heparin aiming for an activated partial thromboplastin time (APTT) of 40-50 s. If patients showed signs of bleeding or thrombosis, individual targets for the APTT and platelet counts were decided.
The systems used for ECMO included the Maquet Cardiohelp System with an HLS Set Advanced (Maquet Cardiopulmonary GmbH, Rastatt, Germany), the Stöckert® centrifugal pump (LivaNova PLC, London, United Kingdom) and the CentrimagTM system (Abbott Cardiovascular, Chicago, USA).
Analysis of von Willebrand factor parameters
VWF activity was quantified in the central laboratory of the University Hospital in Freiburg using the INNOVANCE® VWF Ac (Siemens Healthineers, Germany) on a Sysmex CS5100 analyzer.
In addition, analysis of VWF antigen, VWF collagen binding capacity (VWF:CB) and VWF multimeric analysis were performed as previously described [21].
Platelet Function Analyzer (PFA)
The PFA-200 (Siemens Healthineers, Germany) assay was carried out following the manufacturer’s instructions. Col/ADP cartridges (containing collagen and Adenosine diphosphate (ADP)) were used because they are insensitive to aspirin and nonsteroidal anti-inflammatory drugs (NSAID). If closure time was longer than exactly quantifiable, the longest time quantified by the instrument was used for further analysis. ‘Normalization’ after spiking of blood with rVWF or pVWF designates a closure time <121 s, which is the upper reference limit provided by the manufacturer.
Many PFA studies used the PFA-100. Therefore, it has to be mentioned that PFA-100 and PFA-200 use the same fundamental mechanics and deliver equivalent results [22].
Ethics
This study was carried out in accordance with the declaration of Helsinki. All patients or their legal guardians provided informed consent. The study protocol for the recruitment of ECMO patients was approved by the Ethics Committee of the University Hospital in Freiburg, Germany.
Statistics
Variables are presented as mean ± standard error of the mean (SEM) or as median (interquartile range) as indicated in the figure or table legend. One-way ANOVA followed by Tukey’s post-hoc analysis was performed to compare three or more unpaired variables. A p-value ≤0.05 was considered statistically significant. Analysis was performed using GraphPad Prism V.9.4.1 (GraphPad Software, San Diego, California, USA).
Results
Thirteen patients receiving ECMO were recruited for this study (Table 1). Four patients were female, nine patients were male. Eleven patients were on VV ECMO, two patients were on VA ECMO. The underlying condition for the VV ECMO patients was ARDS, most commonly due to Coronavirus disease 2019 (COVID-19). One patient received VA ECMO for COVID-19 associated perimyocarditis and the other patient for COVID-19 associated pulmonary embolism.
Ten patients were discharged from intensive care and were counted as survivors. One patient died due to severe intracranial bleeding on ECMO. The other two patients died because of the severity of their underlying diseases. Major bleeding was observed in three patients and minor bleeding was documented in three patients. Two patients suffered from intracranial bleeding. Transfusions were required in two patients the day before blood sampling (red blood cells), but throughout their time on ECMO nearly all patients required transfusions. None of the patients required platelet transfusions the day before blood sampling.
Acquired VWS in ECMO patients was confirmed by pathological VWF activity to antigen ratios and markedly reduced or missing high molecular weight von Willebrand factor (HMW VWF) multimers (Table 2). All patients had prolonged PFA closure times and all but one patient had PFA closure times beyond the upper test limit. Platelet counts were > 100 G/l (as was required by the study protocol).
We used the PFA-200 as an in-vitro model of primary hemostasis to estimate the effect of different VWF concentrates in the context of ECMO-induced aVWS. In citrated whole blood samples from ECMO patients which were “spiked” with either recombinant or plasmatic von Willebrand factor (VWF), recombinant and plasmatic VWF led to a dose dependent reduction of the PFA COL/ADP closure time (Fig. 1). Closure times were significantly lower if blood was spiked with rVWF vs. pVWF, which was the case for all concentrations (e.g., closure time (s), rVWF vs. pVWF: 1 U/ml: 150.4 ± 21.7 s vs. 263.8 ± 11.7 s; 4 U/ml: 97.8 ± 9.8 s vs. 195.8 ± 15.4 s, p<0.001). In summary, rVWF was significantly more effective in correcting a pathologic PFA closure time in blood samples from patients with ECMO-induced aVWS than pVWF.
Effects of treatment with recombinant or plasma-derived VWF (rVWF vs. pVWF) on PFA COL/ADP closure time of samples from thirteen patients with ECMO-induced aVWS. The closure time was analyzed in-vitro on buffered citrate whole blood from ECMO patients spiked with rVWF or pVWF using the PFA-200 analyzer. If the time until hemostasis was longer than exactly quantifiable by the instrument, the highest value presented by the instrument was chosen for analysis. Data are presented as mean ± SEM. Data were analyzed by unpaired ANOVA. ns – not significant, ***p<0.001
Figure 2 shows the PFA closure curves of samples from patients with aVWS. We also observed a reduction of the flow rate over time in untreated samples which can be interpreted as partial occlusion of the PFA capillary. There is a more pronounced reduction in the flow rate after addition of VWF, which does not always lead to PFA closure as it can be seen in Fig. 2 for the pVWF concentrations 1 U/ml and 2 IU/ml.
Evaluation of the PFA-200 COL/ADP closure curves. The flow rate in µl/min is monitored until either complete closure occurs, the measurement exceeds 300 s or the sample volume runs out (which can happen in samples with a low hematocrit). In samples from ECMO-induced aVWS a sudden incline in flow can occur, as seen in the present example for the whole blood sample without VWF after approx. 270 s
After the unexpected finding that the dose of rVWF concentrate required to normalize the PFA closure time in aVWS was much higher than described for hereditary VWD [23], we assessed the effectiveness of rVWF vs. pVWF in a small group of patients with hereditary VWD (n=3). Two of these patients had VWD type 1 (one of them with Vicenza type VWD characterized by low VWF due to short VWF half-life) and one patient had type 2A VWD (formerly described as 2C Miami). VWD parameters (VWF activity and VWF antigen) were severely impaired (Table 3). We found that both, rVWF and pVWF, were able to normalize PFA closure times in spiked blood samples of patients with hereditary VWD, but rVWF was more effective in correcting the pathologic PFA closure time at lower dosages (e.g., 0.5 & 1 U/ ml) compared to pVWF (e.g., closure time (s) 1 U/ml rVWF vs. pVWF: 73.7±1.33 vs. 231.3±43.4, p<0.01, Fig. 3). The PFA closure time could be normalized in all samples from patients with hereditary VWD with the lowest rVWF dose tested (0.5 U/ml). However, for aVWS, higher dosages of rVWF were required to normalize PFA closure times: for example, in 10/13 (77 %) cases PFA closure times could be normalized with highest concentration of rVWF tested, but PFA closure time also improved from baseline in the remaining 3 patients that did not achieve normal PFA closure time. Therefore, we could confirm that the dose required to normalize the PFA closure is higher in ECMO-induced aVWS compared to VWD.
Effects of treatment with recombinant or plasma-derived VWF on PFA COL/ADP closure time of samples from patients with VWD. The closure time was analyzed in-vitro on buffered citrate whole blood from three VWD patients spiked with rVWF or pVWF using the PFA-200 analyzer. If the time until hemostasis was longer than exactly quantifiable by the instrument, the highest value presented by the instrument was chosen for analysis. Data are presented as mean ± SEM. Data were analyzed using unpaired ANOVA. *p<0.05, **p<0.01, ***p<0.001
Regarding the PFA closure curves, we frequently observed a sudden incline in the flow rate (Fig. 2, with no VWF) in aVWS patients which may correspond to instability in the primary thrombus. We did not observe this phenomenon when assessing samples from hereditary VWD patients.
Discussion
Bleeding is a leading cause of morbidity and mortality in ECMO patients [5, 9]. Acquired von Willebrand syndrome (aVWS) contributes to the bleeding tendency observed in patients on ECMO support [4, 24]. In the current study, we recruited thirteen ECMO patients with ECMO-induced aVWS. Presence of aVWS was confirmed by VWF multimeric structure analysis. Major bleeding was observed in three patients, two of them suffered from intracranial hemorrhage. Although bleeding is frequent in ECMO it has yet to be determined how to manage aVWS-related bleeding in ECMO patients [5]. After discontinuation of ECMO, HMW VWF multimers are restored within 6 hours [9]. However, if ECMO cannot be discontinued, Desmopressin (DDAVP) is an option in some patients, however, Desmopressin resistance during ECMO due to exhausted endothelial storage sites can occur. This phenomenon has recently been described in COVID-19 patients on ECMO support [25]. Especially in this context, therapy with VWF concentrates has to be considered. In this study, we compared the potential of different VWF concentrates in an in-vitro model.
PFA closure time is an established assay to detect defects in primary hemostasis [26, 27] and the method is useful to monitor the effect of hemostatic therapy for example with DDAVP [28, 29, 30]. After whole blood samples from patients with ECMO-induced aVWS had been spiked with increasing concentrations of rVWF or pVWF, we observed a dose dependent reduction of the PFA closure time. As there are differences in the HMW VWF multimer content of different plasma-derived VWF concentrates, the concentrate which had the highest HMW multimer content in a comparison of 12 concentrates was used [31]. Nevertheless, rVWF was significantly better than pVWF in normalizing the PFA closure time of whole blood samples from patients with aVWS. It is known that rVWF and pVWF differ in their multimer composition [32]. The rVWF contains ultra-large (UL) VWF multimers because it has not been in contact with ADAMTS13. Our findings are in line with a recently published comparison of rVWF and pVWF in ECMO patients that showed a better effect of rVWF on ristocetin-induced platelet aggregation (RIPA) [33].
Unlike most pVWF concentrates, rVWF does not contain factor VIII which can be very high in COVID-19 patients [34, 35]. Critically ill patients with COVID-19 require ECMO relatively often if an acute respiratory distress syndrome develops [36]. It has recently been shown that pVWF concentrates were able to enhance VWF activity in ECMO-induced aVWS patients [37]. The mean VWF ristocetin cofactor activity to antigen ratio increased after treatment but was not normalized. Control of bleeding within 24 hours was achieved in 4/10 patients. In-vivo data regarding the use of rVWF in ECMO aVWS are still missing. Therefore, more in-vivo studies regarding treatment of ECMO-induced aVWS are elementary.
It is difficult to monitor the treatment of the so-called ‘type 2 aVWS’ (as most often observed in ECMO-induced aVWS) since these patients already have very high VWF levels [34, 35]. Unlike for patients with hereditary VWD there is no well-defined target range for substitution in bleeding situations. Our data indicate that the PFA closure time may be useful in monitoring the effect of VWF concentrates in situations of already elevated VWF levels.
One PFA study showed a dose-dependent reduction of PFA closure time in patients with hereditary VWD by spiking buffered citrated whole blood with recombinant von Willebrand factor (rVWF) [23]. In their study with 12 patients suffering from hereditary VWD, Pekrul et al. observed a normalization of PFA closure time in all blood samples after spiking in 1 U/ml rVWF which was not sufficient in many samples from patients with aVWS in our study. To investigate if in aVWS higher doses of VWF may be needed to normalize PFA closure times we investigated the effect of rVWF and pVWF on PFA closure time in spiked blood samples from patients with VWD. We observed a dose dependent reduction in PFA closure time for pVWF and rVWF. In line with the literature, a concentration of 0.5 U/ml rVWF was sufficient to normalize PFA closure time in the context of hereditary VWD [23]. When we looked at the PFA closure curves (Fig. 2) a sudden incline in the flow rate could be observed in some samples from aVWS patients but not from VWD patients. This could be interpreted as a sign for instability in the primary thrombus occluding the PFA capillary. There were some important differences between samples from aVWS and VWD. The samples from aVWS patients had higher baseline VWF antigen levels, lower platelet counts (although all had a platelet count > 100.000/µl) and a lower hematocrit. Both the patients’ VWF and the added VWF can competitively bind to collagen inside the PFA capillary. A competing effect of abundant VWF from the patient might theoretically reduce the effect of spiked VWF. However, we found no correlation between VWF antigen level and PFA closure time. Low platelet count and low hematocrit might also lead to prolonged PFA closure time. However, no significant correlation between PFA closure time and platelet count or hematocrit was observed. The severity of platelet dysfunction [7, 9] might also affect the PFA closure time but was not assessed in the current study. In conclusion, our model predicts a worse response to VWF substitution in ECMO-induced aVWS than in VWD as it has been described for other forms of aVWS [38].
Our study has some limitations. First, it has yet to be shown that the results of our in-vitro study hold true for the in-vivo situation. Most of the patients were on ECMO due to COVID-19. Therefore, the results might not be generalizable to ECMO patients in general. Although in the small subset of non-COVID patients on ECMO the results were consistent. There are factors other than VWF that affect PFA closure time. We consider platelet count, hematocrit and platelet dysfunction to be the most relevant in the current study. But also drugs [39], ABO blood group and time of blood collection [40] are known confounders of PFA closure time. To avoid interference by aspirin and NSAID, Col/ADP cartridges were used. One blood sample per patient was obtained within a 12-60 hours interval after ECMO initiation and not at exactly the same time point which due to the variation in time on ECMO may have had an effect on the severity of the underlying aVWS and therefore could have influenced PFA results.
In summary, we showed that different VWF concentrates reduced the PFA closure time in a dose dependent manner. Interestingly rVWF was more effective than pVWF in normalizing PFA closure time. Higher doses of VWF were needed to normalize PFA closure time in ECMO aVWS compared to hereditary VWD. These data support PFA-200 to monitor hemostatic effects in a future clinical trial involving ECMO patients with aVWS. In-vivo studies will give more insights regarding the effectiveness of different therapies.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ADAMTS13:
-
A disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13
- ADP:
-
Adenosine diphosphate
- APTT:
-
Activated partial thromboplastin time
- aVWS:
-
Acquired von Willebrand syndrome
- COL:
-
Collagen
- CBA:
-
Collagen binding activity
- COVID-19:
-
Coronavirus disease 2019
- DDAVP:
-
Desmopressin
- ECMO:
-
Extracorporeal Membrane Oxygenation
- Fr:
-
French
- Hb:
-
Hemoglobin
- HMW:
-
High molecular weight
- Hb:
-
Hemoglobin
- IQR:
-
Interquartile range
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- PFA:
-
Platelet function analyzer
- pVWF:
-
Plasma-derived von Willebrand factor
- RIPA:
-
Ristocetin-induced platelet aggregation
- rVWF:
-
Recombinant von Willebrand factor
- SEM:
-
Standard error of the mean
- VA:
-
Veno-arterial
- VV:
-
Veno-venous
- VWD:
-
von Willebrand disease
- VWF:
-
von Willebrand factor
References
Karagiannidis C, Brodie D, Strassmann S, Stoelben E, Philipp A, Bein T, et al. Extracorporeal membrane oxygenation: evolving epidemiology and mortality. Intensive Care Med. 2016;42(5):889–96.
Thiagarajan RR, Barbaro RP, Rycus PT, McMullan DM, Conrad SA, Fortenberry JD, et al. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017;63(1):60–7.
Rilinger J, Krötzsch K, Bemtgen X, Jäckel M, Zotzmann V, Lang CN, et al. Long-term survival and health-related quality of life in patients with severe acute respiratory distress syndrome and veno-venous extracorporeal membrane oxygenation support. Crit Care. 2021;25(1):1–11.
Thomas J, Kostousov V, Teruya J. Bleeding and Thrombotic Complications in the Use of Extracorporeal Membrane Oxygenation. Semin Thromb Hemost. 2018;44(1):20–9.
Murphy DA, Hockings LE, Andrews RK, Aubron C, Gardiner EE, Pellegrino VA, et al. Extracorporeal membrane oxygenation-hemostatic complications. Transfus Med Rev. 2015;29(2):90–101.
Abrams D, Baldwin MR, Champion M, Agerstrand C, Eisenberger A, Bacchetta M, et al. Thrombocytopenia and extracorporeal membrane oxygenation in adults with acute respiratory failure: a cohort study. Intensive Care Med. 2016;42(5):844–52.
Siegel PM, Chalupsky J, Olivier CB, Bojti I, Pooth JS, Trummer G, et al. Early platelet dysfunction in patients receiving extracorporeal membrane oxygenation is associated with mortality. J Thromb Thrombolysis. 2022;53(3):712–21.
Karkouti K, Ho LTS. Preventing and managing catastrophic bleeding during extracorporeal circulation. Hematol (United States). 2018;2018(1):522–9.
Kalbhenn J, Schlagenhauf A, Rosenfelder S, Schmutz A, Zieger B. Acquired von Willebrand syndrome and impaired platelet function during venovenous extracorporeal membrane oxygenation: Rapid onset and fast recovery. J Hear Lung Transplant. 2018;37(8):985–91.
Schlagenhauf A, Kalbhenn J, Geisen U, Beyersdorf F, Zieger B. Acquired von Willebrand Syndrome and Platelet Function Defects during Extracorporeal Life Support (Mechanical Circulatory Support). Hamostaseologie. 2020;40(2):221–5.
Bortot M, Ashworth K, Sharifi A, Walker F, Crawford NC, Neeves KB, et al. Turbulent Flow Promotes Cleavage of VWF (von Willebrand Factor) by ADAMTS13 (A Disintegrin and Metalloproteinase With a Thrombospondin Type-1 Motif, Member 13). Arterioscler Thromb Vasc Biol. 2019;39(9):1831–42.
Peyvandi F, Mamaev A, Wang JD, Stasyshyn O, Timofeeva M, Curry N, et al. Phase 3 study of recombinant von Willebrand factor in patients with severe von Willebrand disease who are undergoing elective surgery. J Thromb Haemost. 2019;17(1):52–62.
Sharma R, Flood VH. Advances in the diagnosis and treatment of Von Willebrand disease. Blood. 2017;130(22):2386–91.
Posan E, McBane RD, Grill DE, Motsko CL, Nichols WL. Comparison of PFA-100 testing and bleeding time for detecting platelet hypofunction and von Willebrand disease in clinical practice. Thromb Haemost. 2003;90(3):483–90.
Fressinaud E, Veyradier A, Truchaud F, Martin I, Boyer-Neumann C, Trossaert M, et al. Screening for von Willebrand disease with a new analyzer using high shear stress: A study of 60 cases. Blood. 1998;91(4):1325–31.
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Conrad SA, Broman LM, Taccone FS, Lorusso R, Malfertheiner MV, Pappalardo F, et al. The extracorporeal life support organization Maastricht treaty for nomenclature in extracorporeal life support a position paper of the extracorporeal life support organization. Am J Respir Crit Care Med. 2018;198(4):447–51.
Broman LM, Taccone FS, Lorusso R, Malfertheiner MV, Pappalardo F, DI Nardo M, et al. The ELSO Maastricht Treaty for ECLS Nomenclature: Abbreviations for cannulation configuration in extracorporeal life support - A position paper of the Extracorporeal Life Support Organization. Crit Care. 2019;23(1):1–9.
Siegel PM, Orlean L, Bojti I, Kaier K, Witsch T, Esser JS, et al. Monocyte Dysfunction Detected by the Designed Ankyrin Repeat Protein F7 Predicts Mortality in Patients Receiving Veno-Arterial Extracorporeal Membrane Oxygenation. Front Cardiovasc Med. 2021;8(July):1–12.
Staudacher DL, Gold W, Biever PM, Bode C, Wengenmayer T. Early fluid resuscitation and volume therapy in venoarterial extracorporeal membrane oxygenation. J Crit Care. 2017;37:130–5.
Heilmann C, Geisen U, Beyersdorf F, Nakamura L, Benk C, Trummer G, et al. Acquired von Willebrand syndrome in patients with extracorporeal life support (ECLS). Intensive Care Med. 2012;38(1):62–8.
Favaloro EJ, Mohammed S, Vong R, Chapman K, Kershaw G, Just S, et al. Harmonizing platelet function analyzer testing and reporting in a large laboratory network. Int J Lab Hematol. 2022;44(5):934–44.
Pekrul I, Kragh T, Turecek PL, Novack AR, Ott HW, Spannagl M. Sensitive and specific assessment of recombinant von Willebrand factor in platelet function analyzer. Platelets. 2019;30(2):264–70.
Panholzer B, Bajorat T, Haneya A, Kowalski D, Juhl D, Rocke A, et al. Acquired von Willebrand syndrome in ECMO patients: A 3-year cohort study. Blood Cells Mol Dis. 2021;87:102526. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33338698.
Kalbhenn J, Glonnegger H, Büchsel M, Priebe H, Zieger B. Acquired von Willebrand Syndrome and Desmopressin Resistance During Venovenous Extracorporeal Membrane Oxygenation in Patients With COVID-19: A Prospective Observational Study. Crit Care Med. 2022;50(8):1246–55.
Favaloro EJ, Pasalic L, Lippi G. Towards 50 years of platelet function analyser ( PFA ) testing. 2022. p. 1–10.
Kundu SK, Heilmann EJ, Sio R, Garcia C, Davidson RM, Ostgaard RA. Description of an in vitro platelet function analyzer - PFA-100®. Semin Thromb Hemost. 1995;21(SUPPL. 2):106–12.
Favaloro EJ, Kershaw G, Bukuya M, Hertzberg M, Koutts J. Laboratory diagnosis of von Willebrand disorder (vWD) and monitoring of DDAVP therapy: Efficacy of the PFA-100® and vWF:CBA as combined diagnostic strategies. Haemophilia. 2001;7(2):180–9.
Cattaneo M, Federici AB, Lecchi A, Agati B, Lombardi R, Stabile F, et al. Evaluation of the PFA-100 system in the diagnosis and therapeutic monitoring of patients with von Willebrand disease. Thromb Haemost. 1999;82(1):35–9.
Franchini M, Gandini G, Manzato F, Lippi G. Evaluation of the PFA-100 system for monitoring desmopressin therapy in patients with type 1 von Willebrand’s disease. Haematologica. 2002;87(6):670.
Budde U, Metzner HJ, Müller HG. Comparative analysis and classification of von Willebrand factor/factor VIII concentrates: Impact on treatment of patients with von Willebrand disease. Semin Thromb Hemost. 2006;32(6):626–35.
Rajpurkar M, Frey MJ, Sabo C, Hollon W. Recombinant von Willebrand factor concentrate in 2A von Willebrand disease: Comparison to plasma-derived von Willebrand factor concentrate therapy. Blood Coagul Fibrinolysis. 2019;30(4):168–70.
Mazzeffi M, Henderson R, Krause E, Rabin J, Madathil R, Chow J, et al. In Vitro Comparison of Recombinant and Plasma- Derived von Willebrand Factor Concentrate for Treatment of Acquired von Willebrand Syndrome in Adult Extracorporeal Membrane Oxygenation Patients. Anesth Analg. 2022;134(2):312–21.
Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–98.
Escher R, Breakey N, Lämmle B. ADAMTS13 activity, von Willebrand factor, factor VIII and D-dimers in COVID-19 inpatients. Thromb Res. 2020;192(April):174–5.
Supady A, Combes A, Barbaro RP, Camporota L, Diaz R, Fan E, et al. Respiratory indications for ECMO: focus on COVID-19. Intensive Care Med. 2022;48(10):1326–37. Available from: https://doi.org/10.1007/s00134-022-06815-w.
Mazzeffi M, Bathula A, Tabatabai A, Menaker J, Kaczorowski D, Madathil R, et al. Von Willebrand Factor Concentrate Administration for Acquired Von Willebrand Syndrome- Related Bleeding During Adult Extracorporeal Membrane Oxygenation. J Cardiothorac Vasc Anesth. 2021;35(3):882–7.
Tiede A, Rand JH, Budde U, Ganser A, Federici AB. How I treat the acquired von Willebrand syndrome. Blood. 2011;117(25):6777–85.
Favaloro EJ. Clinical utility of the PFA-100. Semin Thromb Hemost. 2008;34(8):709–33.
Cho YU, Chi HS, Jang S, Park CJ. Reconfirmation of preanalytical variables and establishment of reference intervals of platelet function analyzer-100 closure times in Korean adults. Korean J Lab Med. 2007;27(5):318–23.
Acknowledgments
We would like to thank the staff of the medical intensive care units and the Institute for Clinical Chemistry and Laboratory Medicine of the University Hospital in Freiburg for supporting this project.
Code availability
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was supported by institutional grants from the University of Freiburg, Germany.
Author information
Authors and Affiliations
Contributions
MB: project design, data acquisition and analysis, interpretation of data, preparation of manuscript; UG: project design, interpretation of data; CB: data acquisition, analysis and interpretation of data; TW: interpretation of data; BZ: data acquisition, analysis and interpretation of data; DW: interpretation of data; PMS: project design, data acquisition and analysis, interpretation of data, preparation of manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with the declaration of Helsinki. All patients or their legal guardians provided informed consent. The study protocol for the recruitment of ECMO patients was approved by the Ethics Committee of the University Hospital in Freiburg, Germany.
Consent to publication
No identifiable patient information is provided in the manuscript or figures
Competing interests
MB and UG received travel support from CSL Behring and Takeda Pharmaceutical. BZ received research funding from Takeda, CSL Behring and Biotest. DW received honorary for talks from Abiomed, Abbott, AstraZeneca, Bayer and Novartis. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Büchsel, M., Geisen, U., Beckenkamp, C. et al. The effect of recombinant versus plasma-derived von Willebrand factor on prolonged PFA closure times in ECMO patients with acquired von Willebrand syndrome – an observational study. Thrombosis J 21, 4 (2023). https://doi.org/10.1186/s12959-022-00448-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-022-00448-1