Abstract
In 2016, the Bloomberg Philanthropies Data for Health initiative assisted the Philippine Statistical Authority in implementing Iris, an automated coding software program that enables medical death certificates to be coded according to international standards. Iris was implemented to improve the quality, timeliness, and consistency of coded data as part of broader activities to strengthen the country’s civil registration and vital statistics system. This study was conducted as part of the routine implementation of Iris to ensure that automatically coded cause of death data was of sufficient quality to be released and disseminated as national mortality statistics. Data from medical death certificates coded with Iris between 2017 and 2019 were analysed and evaluated for apparent errors and inconsistencies, and trends were examined for plausibility. Cause-specific mortality distributions were calculated for each of the 3 years and compared for consistency, and annual numeric and percentage changes were calculated and compared for all age groups. The typology, reasons, and proportions of records that could not be coded (Iris ‘rejects’) were also studied. Overall, the study found that the Philippine Statistical Authority successfully operates Iris. The cause-specific mortality fractions for the 20 leading causes of death showed reassuring stability after the introduction of Iris, and the type and proportion of rejects were similar to international experience. Broadly, this study demonstrates how an automated coding system can improve the accuracy and timeliness of cause of death data—providing critical country experiences to help build the evidence base on the topic.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Reliable mortality statistics (on both fact and cause of death) are crucial for public health, medical research, evaluating interventions, and setting health priorities [1]. The underlying cause of death, which is the disease or injury that initiated the train of events leading to death, is the most important aspect of the medical death certificate [2]. To standardise mortality data and make them globally comparable, the International Statistical Classification of Diseases and Related Health Problems (ICD) was developed and adopted by all World Health Organization (WHO) Member States [3]. The ICD contains rules on how cause of death data should be coded. Consequently, mortality coders must be trained in the ICD and systematically apply its coding rules.
In the Philippines, like in most countries, the source of cause of death data is the medical death certificate, and around 90% of registered deaths have such a certificate [4]. In 2016, the Philippines Ministry of Health joined the Bloomberg Philanthropies Data for Health (D4H) Initiative to improve the quality of cause of death data, with the aim of strengthening informed decisions regarding policy and health programs. As a partner of this Initiative, D4H has assisted the Philippine Statistics Authority (PSA) in implementing Iris, an automated coding software program that enables medical death certificates to be coded according to ICD standards. Before the introduction of automated coding, 30 coders in the Vital Statistics Unit at PSA manually coded approximately 580,000 death certificates each year, routinely taking 2–3 years to produce mortality statistics for the country. Manual coding is associated with a high workload for coders and can result in untimely, erroneous, and inconsistent coded data [5, 6].
Automated cause of death coding software: Iris
Automated systems for the classification and retrieval of cause of death information reported on medical death certificates began in the 1960s with ACME, introduced by the National Center for Health Statistics [7]. A more recent development is Iris, a software for the automated coding of multiple causes of death and for the selection of the underlying cause of death. The Iris system, managed by the German Federal Institute of Drugs and Medical Devices, is free to download and provides a consistent application of ICD coding rules—improving national consistency and international comparability. The software is governed and maintained by a user group including the countries who use Iris. All mortality coding rules included in the software are based on decisions of the WHO Mortality Reference Group. While Iris has been implemented in 25 countries, the Philippines was the first country in Asia to implement it for routine coding, with India introducing the software in 2018 as a coding aid, and Taiwan introducing Iris in 2019 for routine coding [8].
Iris can be used in any language, provided the included dictionary is translated and populated with local diagnostic expressions. All entries on the death certificate are assigned an ICD code and the selection of the underlying cause of death is guided by a set of overarching principles developed by WHO and outlined in Volume 2 of the 10th edition of the ICD (ICD-10) [9]. Prior to the release of ICD-11, the ICD-10 classification and coding rules for selection of an underlying cause of death were reviewed regularly by the WHO Mortality Reference Group with updates implemented annually. These ICD updates were also implemented into Iris on annual basis, ensuring cause of death coding practices within Iris were up to date. Version 6.0 of Iris is currently undergoing updates to align with ICD-11, with regular updates from the Mortality Reference Group planned to continue as with ICD-10.
Although selection of the underlying cause of death and corresponding ICD code is mostly done automatically by Iris, there will always be a certain number of medical death certificates that cannot be coded automatically and hence, will be rejected by Iris. This can be due to spelling mistakes or other simple errors on certificates, which can be corrected and then re-entered into Iris [10].
While not altering the classifications or their rules, the implementation of automated coding software can affect the assignment of underlying cause of death codes. In Australia, the change from manual to automated coding in 1997 significantly affected the consistency of mortality statistics, particularly for deaths due to senile/presenile dementia and pneumonia [11]. Minor deviations in major causes of death were also reported in Ireland [12], the Netherlands [6], and Scotland [13] after the introduction of Iris.
Implementing Iris in the Philippines
In September 2016, D4H together with the Australian Bureau of Statistics (ABS), who also use Iris, visited the Vital Statistics Unit in the Philippines to co-develop a roadmap towards Iris implementation and to verify the critical pre-conditions for Iris, basic ICD knowledge and information technology (IT) infrastructure, were in place. Even though multiple languages are used in the Philippines, medical documentation, including certification of cause of death, is done in English. Therefore, the Iris English dictionary used by the Office of National Statistics in the United Kingdom was adopted for use in the Philippines. Common diagnoses and diagnostic expressions used by physicians were included in the dictionary. Iris language standardisation tables were also customised to map various diagnostic expressions to the Iris dictionary.
A clear understanding of registration and data collection processes was established through the development of business process maps. Process mapping supports a better understanding of complex systems and enables adaptation of interventions to the local context [14]. Based on these maps, several key changes were implemented to the civil registration and vital statistics (CRVS) system, most significantly, that PSA’s Regional Offices became responsible for entering all the information on medical death certificates directly into the central CRVS database—the Decentralized Vital Statistics System (DVSS)—enabling centralized coding.
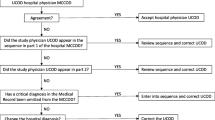
Some internal processes in the Vital Statistics Unit were also clarified and changed, and coders were trained in WHO ICD-10 rules for selecting the underlying cause of death, including how to use the mortality decision tables. Mortality decision tables are a set of tables originally developed by the National Centre for Health Statistics, United States of America, to help coders easily understand causal relationships and apply mortality coding rules. Together with the IT team, the Iris process was mapped, and changes made to the DVSS to enable the database to store the data in a different format, compatible with Iris. A PSA programmer wrote an interface program to allow the import of data into Iris from DVSS (see Fig. 1). The existing DVSS program, with the help of interface program, transfers medical death certificate data into Iris and the coded data are fetched from the Iris’s Microsoft access certificate database.
Once these pre-conditions were in place and updated IT processes were operational, a full pre-testing of Iris and its work processes, including those of the interface program, was completed in April 2017 by D4H, with several issues resolved to reduce the number of Iris rejects (38% in the first batch processing round). After the pre-test, a formal 5-day training on Iris was conducted for PSA coders in June 2017 by D4H, covering (1) the Iris module; (2) the DVSS—Iris interface program module; (3) the administrative module; and, (4) the ICD module. Following training, participants were able to:
-
Understand the different operations of Iris.
-
Use Iris in both text (user enters diagnostic text into Iris) and code (user enters ICD codes) entry modes.
-
Use the DVSS—Iris interface program to transfer medical death certificate data into Iris.
-
Attend successfully to the different types of Iris rejects.
As part of ongoing monitoring, evaluation, and learning activities, medical death certificate data that were coded with Iris between 2017 and 2019 were analysed and evaluated by PSA with the support of technical experts from D4H. Assessments focused on the 20 leading causes of death, which are responsible for approximately 88% of all deaths in the Philippines, and followed three main approaches:
-
1.
Dual coding A sample (N = 207,508) of medical death certificates were both manually coded and coded with Iris from January to May 2017 In order to assess the level of agreement between manually coded certificates and those coded by Iris. The comparability ratio (CR) between the two coding sources was calculated. The CR is defined as the number of deaths coded manually for a particular ICD code, divided by the number of deaths coded by Iris to the same ICD code [11]. The closer this ratio is to 1.0, the higher the level of agreement between the two coding sources. It should be noted that, while the CR compares the number of deaths assigned to the same ICD-10 code, it does not imply that the same individual was assigned the same code.
-
2.
Reviewing Iris rejects for obvious errors and inconsistencies Common errors include the assignment of non-standardised ICD-10 codes, or codes that are incompatible with the age and/or sex of the deceased (for example, assigning ovarian cancer to a biological male). Codes were examined for consistency and plausibility by comparing them with data from previous years.
-
3.
Calculating cause-specific mortality fractions (CSMFs) CSMFs were calculated for each of the 3 years and compared for consistency, and annual numeric and percentage changes were calculated and compared for all age and sex groups. The age pattern of CSMFs provide valuable information about the distribution of causes of deaths in a population. They help to identify leading causes of death, which is important for public health planning, resource allocation, and policy development. CSMFs are used to estimate the burden of disease in a population, and changes in mortality patterns over time.
The quality of data coded by Iris was also assessed by looking at the number and pattern of Iris rejects. When information entered into Iris is not sufficient to identify a code for the underlying cause of death, the record is rejected, and manual intervention is needed. Most records are rejected because of minor errors that can easily be solved and corrected by a trained coder, before being re-entered into Iris. There are two major types of rejects:
-
1.
‘Code’ rejects. This is when a specific code is not available in the dictionary for a diagnosis written on the medical death certificate. This may be due to different local expressions of diagnoses for which the dictionary and the standardisation tables cannot match a specific ICD code. Records that contain typos are also counted as code rejects, as no corresponding ICD codes exist for such entries.
-
2.
‘ACME maybe’. Iris uses mortality decision tables to understand causal relationships and to apply mortality coding rules. An ACME maybe reject means that the decision tables recognise some causal relationships as unsure or undecided, requiring an expert coder (Nosologist) to review the record for further processing.
At PSA, Iris is run on individual desktop computers, and therefore it is not easy to study the typology pattern of Iris rejects for all batches of medical death certificates processed through the software. However, in 2018 it was possible to study several batch-processing lots to identify common types of rejects. The typology, reasons, and proportions of Iris rejects were studied for this sample of certificates (N = 590,709).
Assessing the quality of automated coding
Over 1.79 million deaths were coded using Iris during the 3 years analysed. In 2017, when Iris was first implemented, the PSA coding team dual-coded medical death certificates for a period of 5 months between January and May. During this time, 207,508 certificates were coded with Iris, and 215,693 were coded manually. This was considered to be a robust sample for analysis, representing approximately 40% of deaths registered that year. Analysis of the 3-digit underlying cause of death codes between Iris and manually coded medical death certificates revealed a 76% match between the two coding sources. This is considered a high-level match.
Time series analysis completed for the 20 leading causes of death (2014–2017) and analysis of the CR for medical death certificates that were dual-coded in 2017 showed that despite some changes, trends remained relatively stable (see Table 1). The largest change was seen with the rise in deaths from ‘X95—homicide, gun type unspecified’ (CR = 0.57, 95% CI 0.56–0.58). The PSA coding team previously had a business rule that all gun deaths were coded to handgun homicides (‘X93’), regardless of if the type of gun was specified or not. As gun type is generally not reported on the medical death certificate, the coding of ‘X95’ in Iris, as opposed to ‘X93’ (handgun death) via manual coding, was considered more accurate, and the increase in deaths coded to ‘X95’ assessed as plausible.
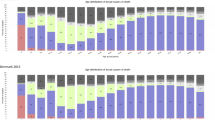
Table 2 shows the total number of deaths each year and the percentage change between the two periods (2017–2018 and 2018–2019) for the 20 leading causes of death coded by Iris. Population growth was reflected in the growing number of deaths each year, which amounted to 2% between 2017 and 2018 and 5% between 2018 and 2019. In a country such as the Philippines, one would expect that noncommunicable diseases would dominate the cause of death distribution. This was the case for each year where they consistently accounted for more than half of all deaths, while communicable diseases were less than 15%. Transport accidents and assaults, both external causes, each accounted for under 2% of all deaths. Changes in the 2018–2019 period were not significantly different from previous years’ data, except for the decrease in assaults, which declined by 16% between 2017 and 2018 and by 11% between 2018 and 2019.
The cause-specific mortality fractions (CSMFs) for the five leading causes of death showed reassuring stability over the 3 years analysed (see Fig. 2).
Given the decentralised nature of the Philippine CRVS system, Iris is installed on multiple computers, and access to centralised coding logs is limited. Further, once rejects are reviewed by coders, they are subsequently amended and re-entered into Iris and the final code is assigned—thus deleting the error log. Based on available information from 2018, the number of rejects was initially around 50% in the Philippines. Most of the rejects identified fell into the ‘code’ category. For example, it was found that many physicians used the term ‘community-acquired pneumonia high-risk’ when completing medical death certificates, however this diagnosis is not a standard term available in the ICD or in the Iris dictionary.
Improving mortality statistics
The extensive use of mortality statistics for public health programmes and research purposes requires targeted efforts and funding to improve the quality of cause of death data. In turn, this primarily depends on the quality of cause of death certification and coding [15]. While the introduction of new tools to assist in mortality coding can improve the timeliness and accuracy of cause of death data, they can also introduce new or unforeseen errors. This study was conducted as part of the routine implementation of Iris in the Philippines to ensure that automatically coded cause of death data were of sufficient quality to be released and disseminated as national mortality statistics.
While the primary purpose of this study was to understand if the underlying cause of death code attributed by Iris was accurate, rather than ascertaining the reasons why it differed from those derived during manual coding, several important observations were noted. There was a substantial decline in deaths due to assaults during 2017–2018 and 2018–2019. This should be investigated further as it is unlikely that a policy change would have caused it. It is recommended that if there is no obvious explanation for this, it may be useful to pursue this trend and investigate what type of assaults are responsible for the decrease and what age groups are affected. It could be fictitious and caused by changes in how police or coroner’s report these deaths, or an introduced error as part of automated coding with Iris.
Some of the smaller changes that occurred could be explained in part by population ageing. For instance, increases between 2018 and 2019 in ischemic heart diseases (10%), pneumonia (10%), and the category 'remainder of the nervous system’, which includes dementia and degenerative brain diseases (12%), could due to population ageing. However, it remains important to continue to monitor these trends, and frequently assess if the underlying assumptions around population dynamics and the leading causes of death hold true.
While a full assessment of the type and level of rejects was not possible as part of this study, results are similar with what has been observed in other locations. In the Netherlands, for example, Iris could code 69% of medical death certificates without any manual intervention. Of the rejected death certificates, the main reason for rejection was ‘code rejects’ (76%) [10]—similar to what was observed in the Philippines.
The year 2022 is the sixth year that cause of death data collected by the CRVS system in the Philippines have been automatically coded with Iris. Each year before dissemination, the data have undergone a thorough assessment to ensure they correctly describe the population's mortality profile and can be used for policy purposes to make further improvements. As the Philippine population is still growing rapidly, the number of deaths is also increasing annually. This together with population ageing makes it difficult to depend on raw numbers to assess changes and trends. In future assessments, it is recommended that PSA also prepares standardised death rates for the 20 leading causes of death. This would allow the separation of these two factors on observed changes in mortality for the country.
The use of Iris by PSA has helped to strengthen centralised coding practices as the software applies mortality coding rules in the same way each time medical death certificates are coded. When new diagnoses are added to the dictionary, Iris codes the diagnoses consistently. Compared to manual coding, automated coding increased the availability of mortality statistics, with data from 2017 available by January 2019—almost 1 year earlier than with manual coding. While Iris does not replace the need for skilled mortality coders entirely, it enables coders to focus on difficult cases by successfully coding the vast majority of deaths.
Experiences of the Philippines in implementing Iris offers great insight for other countries considering automated coding software. Automated coding software both considerably reduces the workload for manual coders, while improving the accuracy and timeliness of cause of death data through the systematic application of coding rules. With the introduction of ICD-11, automated coding may offer significant advantages to countries during the transition phase, including an increased ability to conduct dual coding and monitor for changes in mortality statistics. However, the change from manual to automated coding can bring about changes in the distribution of leading causes of death. It is important that both coders and end-users of national mortality statistics are aware of these potential changes when studying trends over time and routine quality assessments are carried out to detect and explain unusual or unexpected changes. Continuing to build the evidence base on Iris implementation and use by sharing country experiences, as with the example here from the Philippines, will help improve the quality of the Iris software itself, and in turn, the quality of mortality statistics worldwide.
Availability of data and materials
The data presented in this paper are publicly available on the PSA website and can be requested by filling out a form. Data are owned by the Philippine Statistics Authority, and any application for access to these data would need to be addressed and reviewed by PSA.
References
Phillips DE, AbouZahr C, Lopez AD, et al. Are well functioning civil registration and vital statistics systems associated with better health outcomes? Lancet. 2015;386(10001):1386–94. https://doi.org/10.1016/S0140-6736(15)60172-6.
World Health Organization. International statistical classification of diseases and related health problems, 11th revision (ICD-11), reference guide. Geneva: WHO; 2019. Available: https://icdcdn.who.int/icd11referenceguide/en/html/index.html#what-is-tabulated-underlying-cause-of-death.
World Health Organization. International statistical classification of diseases and related health problems, 11th revision (ICD-11), reference guide. Geneva: WHO; 2019. Available: https://icdcdn.who.int/icd11referenceguide/en/html/index.html#icd11-reference-guide.
Economic and Social Commission for Asia and the Pacific. A snapshot of progress midway through the Asian and Pacific civil registration and vital statistics decade. Bangkok: ESCAP; 2021. Available: https://www.unescap.org/kp/2021/getting-every-one-picture-snapshot-progress-midway-through-asian-and-pacific-civil.
Lu TH, Lee MC, Chou MH. Accuracy of cause-of-death coding in Taiwan: types of miscoding and effects on mortality statistics. Int J Epidemiol. 2000;29(2):336–43. https://doi.org/10.1093/ije/29.2.336.
Harteloh P, de Bruin K, Kardaun J. The reliability of cause-of-death coding in The Netherlands. Eur J Epidemiol. 2010;25:531–8. https://doi.org/10.1007/s10654-010-9445-5.
National Center for Health Statistics, US Department of Health and Human Services. About the mortality medical data system [website]. Available: https://www.cdc.gov/nchs/nvss/mmds/about_mmds.htm.
Federal Institute for Drugs and Medical Devices. Iris users [website]. Available: https://www.bfarm.de/EN/Code-systems/Collaboration-and-projects/Iris-Institute/Iris-users/_node.html;jsessionid=273D373E8982FD5CA8BAC334BF904DA0.intranet671.
World Health Organization. International statistical classification of diseases and related health problems, 10th revision. Geneva: WHO; 2016.
Harteloh P. The implementation of an automated coding system for cause-of-death statistics. Inf Health Soc Care. 2020;45(1):1–14. https://doi.org/10.1080/17538157.2018.1496092.
McKenzie K, Walker S, Tong S. Assessment of the impact of the change from manual to automated coding on mortality statistics in Australia. Health Inf Manag. 2002;30(3):1–11.
Central Statistics Office. Implementation of IRIS software for the automated coding of deaths in Ireland. Cork: Central Statistics Office, ND. Available: https://www.cso.ie/en/media/csoie/methods/birthsdeathsandmarriages/Information_Note_-_IRIS.pdf.
National Records of Scotland. The impact of the implementation of IRIS software for ICD-10 cause of death coding on mortality statistics in Scotland. Edinburgh: National Records of Scotland, ND. Available: https://www.nrscotland.gov.uk/files/statistics/vital-events/impact-of-implementation-iris-for-icd.pdf.
Antonacci G, Lennox L, Barlow J, et al. Process mapping in healthcare: a systematic review. BMC Health Serv Res. 2021;21(342):1–15. https://doi.org/10.1186/s12913-021-06254-1.
Rampatige R, Mikkelsen L, Hernandez B, et al. Systematic review of statistics on causes of deaths in hospitals: strengthening the evidence for policy-makers. Bull World Health Organ. 2014;92(11):807–16. https://doi.org/10.2471/BLT.14.137935.
Acknowledgements
Results from this study were initially presented at the Asia-Pacific Civil Registration and Research Forum, 3–4 April 2023, organised by the Economic and Social Commission for Asia and the Pacific (ESCAP). The authors wish to thank staff from the Statistics Division, ESCAP, for their assistance in preparing the manuscript for publication.
Funding
The activities described in this paper were funded by an award from Bloomberg Philanthropies to the Philippine Statistics Authority as part of the Data for Health Initiative. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
USHG, CS, and AGT-R conceived the data collection and analysis design as part of the study. AGT-R, MBV, NEP, & KJTB were responsible for data collection, cleaning, and analysis. CS coordinated activities related to data collection. USHG drafted the first version of the manuscript. RJ and NR reviewed the draft manuscript, provided comments, and coordinated finalisation of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Patient and public involvement statement
In this research, we did not directly involve patients or the public. However, we acknowledge the importance of engaging with relevant stakeholders to ensure our findings' relevance and potential impact. Throughout the research process, we sought input from experts in the field, to help shape the study design, interpretation of the results, and potential implications for the field.
Patient consent for publication
Not appliable. Ethical approval was not required for this study as the investigation was implemented as part of service improvement. Data were anonymized and irreversibly de-identified.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gamage, U.S.H., Sarmiento, C., Talan-Reolalas, A.G. et al. Automated mortality coding for improved health policy in the Philippines. Popul Health Metrics 22, 24 (2024). https://doi.org/10.1186/s12963-024-00344-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12963-024-00344-y