Abstract
Background
Patients on maintenance hemodialysis (MHD) have been disproportionately affected by COVID-19. Identifying factors associated with disease severity and viral clearance times can inform better clinical management for this high-risk group.
Methods
We retrospectively analyzed clinical and hematological data from 85 COVID-19 positive MHD patients. Disease severity was classified as non-severe (mild/moderate) or severe (severe/critical). Logistic regression was used to evaluate factors associated with disease severity. The time to viral clearance was assessed and correlated with clinical variables.
Results
Cardiovascular disease (OR=11.19, 95% CI 2.35–53.38), neutrophilia (OR=1.24, 95% CI 1.01–1.53), and elevated inflammatory markers (procalcitonin and white blood cell count) were independent predictors of severe COVID-19. A prognostic model incorporating these factors showed good discrimination for severity risk (AUC=0.835). The median time to viral clearance was 19 days. Delayed clearance was associated with higher levels of C-reactive protein, troponin, and N-terminal pro-B-type natriuretic peptide.
Conclusions
We identified key prognostic factors for COVID-19 severity and characterized the time to viral clearance in MHD patients. These findings can aid in risk stratification and optimize management for this vulnerable population. Further research through multicenter collaborative studies is warranted to validate these results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In recent years, Coronavirus Disease 2019 (COVID-19) has become a significant global public health event, posing unprecedented challenges to health systems worldwide [1]. The severity of COVID-19 is influenced by several factors, such as age, gender, and underlying diseases [2, 3]. In the early stages of the COVID-19 pandemic, cases of infection were reported among patients with chronic kidney disease and those undergoing dialysis, who often had higher incidence rates and mortality rates [4,5,6]. However, for patients with uremia on maintenance hemodialysis (MHD), the risks associated with COVID-19 are even more pronounced [7, 8].
Maintenance Hemodialysis (MHD) serves as a prevalent therapeutic approach for uremia, necessitating patients to undertake dialysis treatments thrice weekly, each lasting four hours, to compensate for the compromised renal function. Given the existence of chronic diseases, dialysis patients experience immunodeficiency and frequently exhibit an array of complications including hypertension, anemia, and disorders of bone mineral metabolism [9]. In comparison to the general population, the mortality rate in MHD patients exhibits an increment between 5.1 and 6.8 folds [10], Data from the United States Renal Data System (USRDS) corroborates that the five-year survival rate post initiation of dialysis in MHD patients stands at a mere 49% [11], while research conducted in our country reveals a slightly higher survival rate of 59% over the same period [12]. Numerous studies have shown that the primary causes of mortality in maintenance hemodialysis (MHD) patients include cardiovascular disease (CVD), infections, cerebrovascular incidents, gastrointestinal bleeding, malnutrition, and sudden death [13]. These complications significantly increase the susceptibility of dialysis patients to COVID-19 and can exacerbate the severity of the disease, underscoring the critical need for continuous and comprehensive care in managing MHD patients, especially during the COVID-19 pandemic [14]. Furthermore, the health status of MHD patients might be impacted by several factors such as dialysis duration, frequency, and adequacy, all of which could potentially exert substantial influence on the severity of COVID-19 [15].
Studies on COVID-19 risk factors in maintenance hemodialysis (MHD) patients are limited. A retrospective multicenter cross-sectional study reported significantly higher mortality rates in MHD patients compared to the general population post-COVID-19 infection1. Factors such as age, gender, BMI, blood pressure, and pulmonary function may influence COVID-19 severity and duration in these patients23. Recent findings indicate that the time from COVID-19 diagnosis to viral clearance is an independent risk factor for disease severity, with longer clearance times correlating with more severe disease. Additionally, a higher number of complications is associated with extended viral clearance times24. These insights suggest that MHD patients with COVID-19 are at increased risk of severe disease, with viral clearance time serving as a potential severity marker.
Studies on the risk factors of COVID-19 in patients with maintenance hemodialysis (MHD) are limited. A retrospective multicenter cross-sectional study found that the mortality rate of MHD patients was significantly higher than that of the general population after COVID-19 infection [16]. In addition, studies have shown that factors such as age, gender, body mass index, blood pressure, and pulmonary function in MHD patients may influence the severity and duration of COVID-19 [17, 18]. However, the understanding of COVID-19 risk factors in MHD patients is still limited, and further studies are needed to investigate the disease risk and prognosis of MHD patients during the COVID-19 pandemic.
A recent study found that the time from COVID-19 diagnosis to viral clearance was also an independent risk factor for disease severity in maintenance hemodialysis patients [19]. This means that the longer the time to viral clearance, the more severe the disease is likely to be. The study also found that the number of complications a patient had was associated with a longer time to viral clearance [17]. These findings suggest that maintenance hemodialysis patients who develop COVID-19 are at increased risk of severe disease, and that the time to viral clearance may be a useful marker of disease severity.
The results of this study may help to identify the population of maintenance hemodialysis patients who are most susceptible to the effects of COVID-19 and provide guidance to clinicians to help improve these patients' survival. The aim of this study (1) is to investigate the risk factors associated with the severity of COVID-19 in patients on maintenance hemodialysis for uremia, (2) as well as the risk factors affecting the time to viral clearance of patients. Through in-depth study of these issues, we hope to provide more accurate guidance for the clinical management of these patients to reduce the adverse effects of COVID-19 infection on their health.
2 Research materials and methods
2.1 Data collection
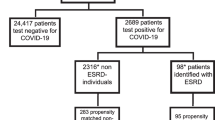
This study was a retrospective study of patients with maintenance hemodialysis who were diagnosed with COVID-19 at the Renal Center of the Kidney and Nephrology Department of the study Hospital in Shanghai from April 1, 2022 to May 30, 2022. All patients had positive results on the first nasopharyngeal swab nucleic acid test for COVID-19 (Ct value < 40), Laboratory measurements, including complete blood counts, inflammatory markers, and other biochemical parameters, were performed at the hospital’s central laboratory. Blood samples were collected within 24 h of hospital admission and subsequently on days 7 and 14 post-admission to monitor disease progression and response to treatment. And diagnosis of COVID-19 was confirmed by RT-PCR tests on nasopharyngeal swabs. Viral clearance was assessed by two consecutive RT-PCR tests, with each test separated by a 24-h interval. The viral clearance cycle for patients infected with the Omicron variant of the COVID-19 virus was the period from admission to the hospital to the period of two consecutive nucleic acid tests with Ct values > 35 [20, 21]. The study was approved by the Ethics Committee of the Ruijin Hospital-Shanghai Jiao Tong University School of Medicine and all subjects provided informed consent. The severity of COVID-19 in patients was assessed based on the clinical presentation, laboratory test results, and imaging test results of the cases. The following are the general criteria for assessing the severity of COVID-19 [22]:
Mild cases: Patients have mild symptoms such as low-grade fever and cough, with no signs of pneumonia.
Moderate cases: Patients exhibit fever, respiratory symptoms, and radiographic evidence of pneumonia.
Severe cases: Patients meet any of the following criteria: respiratory rate ≥ 30 breaths/min; resting oxygen saturation ≤ 93%; ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) ≤ 300 mmHg; or pulmonary infiltrates > 50% progression within 24–48 h per imaging.
Critical cases: Patients have respiratory failure requiring mechanical ventilation, shock, other organ failure requiring intensive care unit monitoring, or pneumonia with multiple organ dysfunction syndrome.
Inclusion criteria: The study on risk factors for disease severity and time to viral clearance in COVID-19 patients on maintenance hemodialysis (MHD): (1) Laboratory-confirmed diagnosis of COVID-19; (2) Receiving MHD treatment; (3) Age 18 years or older; (4) Complete medical records available, including laboratory test results and treatment process documentation.
Exclusion criteria: (1) Not receiving MHD treatment; (2) No laboratory-confirmed diagnosis of COVID-19; (3) Age under 18 years; (4) Incomplete or missing key information in medical records, such as lack of laboratory test results or treatment process documentation; (5) Concurrent serious infections that could interfere with results (e.g., severe bacterial or fungal infections); (6) Pregnant or lactating women, as these special populations may have unique responses to COVID-19 progression and treatment; (7) Other major comorbidities, such as end-stage malignancies or severe cardiopulmonary insufficiency, that could impact study outcomes.
2.2 Data collection
-
(1)
Basic information: age, sex, primary disease, age on dialysis (in months), diabetes mellitus, hypertension, pulmonary infection, and history of cardiovascular disease, cardiovascular disease was defined as the presence of one or more of the following: history of myocardial infarction, angina pectoris, heart failure, or documented poor left ventricular ejection fraction (< 40%), as confirmed by medical diagnostic records.
-
(2)
Clinical information: Hematology-White blood cell count (WBC), Hemoglobin (HB), Neutrophils (N), Neutrophils (N) Lymphocytes (L), Platelet count (PLT), Fibrinogen (Fg), d-dimer (D-D); Inflammatory markers-C-reactive protein (CRP), Procalcitonin (PCT); Renal function-Blood Urea Nitrogen (BUN) mmol/L, Creatinine mmol/L (Cr), Glomerular Filtration Rate (GFR), Uric acid (UA); Electrolyte and Acid–Base Balance- Potassium mmol/L (K), Potassium mmol/L (Potassium, K) Bicarbonate mmol/L (Bicarbonate, HCO3), Calcium mmol/L (Calcium, Ca), Phosphorus mmol/L (Phosphate, PO4); Nutrition and Liver function (Nutrition and Liver function)-Albumin g/L (Alb); Cardiac function- Myoglobin (Mb), Troponin (Tn), Brain Natriuretic Peptide (BNP).
2.3 Statistical analysis
Categorical data were described using rates or composition ratios, with differences between groups compared using chi-square tests or Fisher’s exact probability tests. For normally distributed measurement data, mean ± standard deviation (x̅ ± s) was used for descriptions, with t-tests or analysis of variance used for between-group comparisons. For non-normally distributed measurement data, medians and interquartile ranges were used for descriptions, and rank sum tests were used for statistical analyses. All statistical analyses were performed using R Statistics software version 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
3 Results
3.1 General characteristics
A total of 85 hospitalized COVID-19 positive MHD patients were included, comprising 50 males and 35 females. The minimum age was 33 years and maximum age was 92 years, with a mean age of 65.26 and standard deviation of 12.53. There were 28 (32.9%) mild cases, 44 (51.7%) moderate cases, 8 (9%) severe cases, and 5 (5%) critical cases. During hospitalization, the minimum time to viral clearance for COVID-19 positive MHD patients was 7 days, the maximum was 49 days, and the median was 19 days. At the end of the study period, 8 patients remained positive.
3.2 MHD and COVID-19 severity
COVID-19 severity was classified as mild, moderate, severe, or critical. Risk factors influencing COVID-19 severity were explored. Among them, underlying CVD, WBC, neutrophil count, and PCT differed significantly between groups stratified by COVID-19 severity, as shown in Table S1.
COVID-19 severity was further classified into non-severe (combining mild and moderate) and severe (combining severe and critical) groups. Risk factors influencing COVID-19 severity were explored. Results showed that underlying CVD, WBC, neutrophils (N), and PCT differed significantly between the non-severe and severe COVID-19 groups, as shown in Table 1. These factors appear to be associated with worse COVID-19 outcomes in maintenance hemodialysis patients based on this data. Additionally, the time to viral clearance differed between the groups, with the severe group (24.86 ± 11.54 days) exhibiting longer time to clearance compared to the non-severe group (19.47 ± 5.22 days).
3.3 Multivariable logistic regression analysis of risk factors for COVID-19 severity in MHD patients
Variables with p < 0.10 in univariate analysis were included in the multivariate logistic regression analysis, as shown in Table S2. History of cardiovascular disease (CVD) [OR = 10.21, 95% CI (2.72–38.30)], neutrophil count (N) [OR = 1.24, 95% CI (1.01–1.53)], and white blood cell count (WBC) [OR = 1.26, 95% CI (1.01–1.57)] were significant risk factors for severe COVID-19. After adjusting for age and other factors, patients with CVD had a 11.19-fold higher risk of developing severe COVID-19 compared to those without CVD [OR = 11.19, 95% CI (2.51–61.30)]. Then the regression forest plot for the multifactorial logistic regression analysis of MHD and COVID-19 severity is shown in Fig. 1.
3.4 Nomogram for predicting COVID-19 severity in MHD patients
A nomogram prediction model shown in Fig. 2 was constructed based on the regression coefficients of the 6 risk factors identified from univariate and multivariate logistic regression analyses. The nomogram score scale ranges from 0 to 100 points, with each risk factor represented by a vertical line corresponding to its points value on the score scale. The total sum of points for the 6 predictive factors is the total score for a patient, which is then mapped to the probability of severe COVID-19 on the “Total points” scale. Higher total scores indicate higher risks of severe COVID-19. The nomogram total scores are mainly distributed between 290 to 350 points, corresponding to 0% to 90% probability of severe COVID-19. The red dot in the figure shows the profile of a mild COVID-19 case, a female patient with CVD and the following values: WBC 4.06, N 6.95 mmol/L, troponin 28 μg/L, PCT 24.2 ng/mL. This patient's total nomogram score is 334 points, corresponding to a 51.9% probability of severe COVID-19.
3.5 Performance of the prediction model
As shown in Figure S1, the Brier score for overall evaluation of the nomogram prediction model was 0.096, falling between 0 and 0.25 and closer to 0. This indicates that the prediction model has good overall performance in predicting the risk of severe COVID-19 in MHD patients. The ROC curve for the nomogram prediction model. The area under the curve (AUC) was 0.835 (95% CI 0.707 to 0.931), greater than 0.80, indicating that the prediction model has good discrimination ability. Our results show the calibration plot and ROC curve suggest satisfactory predictive performance of the nomogram model.
3.6 Clinical utility of the prediction model
As shown in the decision curve analysis (DCA) plot in Figure S2, the x-axis of the DCA curve represents the threshold probability and the y-axis represents the net clinical benefit (NCB). NCB is calculated by subtracting the treatment harm (TH) from the treatment benefit (TB), where TB is the net benefit gained from treatment and TH is the net risk from treatment. In the DCA curve, the net clinical benefit of the model is plotted as a line across a range of threshold probabilities. Typically, the x-axis of a DCA plot ranges from 0 to 1, and the y-axis ranges from the minimum to maximum NCB. The DCA analysis in this study showed that comparing the DCA curves of different models, the full nomogram model with all variables had the highest net clinical benefit, indicating this model has superior clinical utility.
3.7 Analysis of factors affecting time to COVID-19 clearance
During hospitalization, the time to viral clearance for the 85 COVID-19 positive MHD patients ranged from 7 to 49 days, with a median of 19 days. At the end of the study period, 8 patients remained positive. The density distribution of time to clearance in MHD patients is shown in Fig. 3. Based on the median, the study population was divided into a rapid clearance group (< 19 days) and delayed clearance group (≥ 19 days). There were 32 (41.5%) patients in the delayed clearance group and 45 (58.5%) in the rapid clearance group.
3.8 Analysis of factors affecting rapid vs delayed viral clearance (median 19 days)
Differences in CRP, BNP, and troponin levels between the rapid and delayed clearance groups were statistically significant (p < 0.05), while differences in age, gender and other factors were not significant between the two groups (p > 0.05), as shown in Table 2. Additionally, there was no significant difference in COVID-19 severity between the two groups (p > 0.05).
3.9 Analysis of factors affecting rapid vs delayed clearance (14 days)
Therefore, 14 days was set as the cutoff [23], dividing the study population into a rapid clearance group (< 14 days) and delayed clearance group (≥ 14 days). There were 64 (41.5%) patients in the delayed clearance group and 13 (58.5%) in the rapid clearance group as shown in Table S3.
3.10 Correlation analysis of time to clearance
Time to viral clearance was correlated with phosphorus (r = − 0.273, p = 0.049), hemoglobin (r = − 0.277, p = 0.046), blood urea nitrogen (r = − 0.294, p = 0.034), white blood cell count (r = 0.304, p = 0.028), uric acid (r = − 0.334, p = 0.015), neutrophils (r = 0.375, p = 0.006), C-reactive protein (r = 0.435, p < 0.01), GFR (r = 0.479, p < 0.01), troponin (r = 0.519, p < 0.01), and procalcitonin (r = 0.648, p < 0.01). All correlations were statistically significant as shown in Supplementary figure S3.
3.11 Prediction model for time to clearance
A regression model was constructed with time to clearance (Time) as the dependent variable and other influencing factors as independent variables to predict time to viral clearance. Prior to regression, multicollinearity was assessed using variance inflation factors (VIFs) by removing variables with VIF > 10. The final regression model was developed through stepwise regression to identify variables entering the model. Results are shown in Table 3. After adjustment, neutrophils (N), uric acid, myoglobin, troponin, PCT and fibrinogen (Fg) showed statistically significant associations with time to clearance. Uric acid, myoglobin and troponin had very small beta coefficients, while N had a beta coefficient of − 3.81 [− 7.60, − 0.08], PCT is 1.91 [1.21, 2.72], and Fg is 3.02 [0.60, 5.44].
To develop an appropriate model for predicting time to viral clearance in patients, a random forest model was constructed. The entire dataset was split into 80% training set and 20% test set using an 8:2 ratio. The model was trained using the 80% training data, and then evaluated for accuracy on the 20% test set. As shown in Supplementary Figure S4, the random forest model demonstrated better predictive accuracy (r = 0.5, p = 0.05) compared to a general linear model (r = 0.27, p = 0.31). The improved performance of the random forest model highlights the potential of machine learning approaches for forecasting COVID-19 viral clearance time versus traditional regression techniques.
4 Discussion
Since the outbreak of the novel coronavirus disease (COVID-19) pandemic in late 2019, healthcare systems worldwide have faced enormous challenges. The rapid transmission of COVID-19 pneumonia has imposed unprecedented strains on public health and clinical medicine [24, 25]. In this pandemic, patients with end-stage kidney disease on maintenance hemodialysis (MHD) represent a particularly high-risk population of concern. The aim of this study was to analyze differences in COVID-19 severity (non-severe vs severe) in MHD patients during clinical treatment. We found that MHD patients with underlying comorbidities were at higher risk of developing severe COVID-19. We hope to provide robust theoretical basis for the prevention, diagnosis, and treatment of COVID-19 positive MHD patients, in order to reduce the infection risk and mortality of this vulnerable group and promote their recovery.
The results demonstrated statistically significant differences in cardiovascular disease (CVD), white blood cell count (WBC), neutrophils (N), and procalcitonin (PCT) across COVID-19 severity groups. Firstly, CVD as a prevalent comorbidity had a substantial impact among COVID-19 positive MHD patients, potentially exacerbating systemic inflammation and cardiopulmonary dysfunction, thereby worsening COVID-19 pneumonia [2]. The cardiovascular status of patients plays a crucial role in the course and prognosis of COVID-19 pneumonia. Moreover, studies indicate MHD patients may have a CVD mortality risk up to 40% [26]. In an age- and sex-matched study, MHD patients had over tenfold higher CVD mortality versus the general population [27]. Hence, elucidating CVD risk factors in MHD patients could better inform clinical decision-making. Secondly, WBC was associated with COVID-19 severity, as elevated WBC may reflect exuberant immune responses to viral infection, which can precipitate cytokine storm, pulmonary damage, and systemic inflammation, consequently deteriorating the disease [28]. Studies demonstrate WBC can serve as an indicator of COVID-19 severity [29]. One study found increased WBC in hospitalized COVID-19 patients was linked to higher mortality risk [30]. WBC elevation in COVID-19 has also related to severe complications like inflammation, lung injury, and multiorgan damage [31, 32]. However, the mechanisms underlying WBC and COVID-19 severity remain to be thoroughly investigated. Some studies propose it may involve SARS-CoV-2 effects on immunity, as viral entry via ACE2 receptors can elicit cytokine storm and immune dysregulation, prompting inflammation and immune cell aggregation/activation, thereby influencing WBC [28]. Further research into the mechanisms is imperative. Nevertheless, timely WBC monitoring could facilitate assessment of disease progression and treatment response in patients.
Utilizing these variables, we developed a logistic regression model that achieved an area under the curve (AUC) of 0.835, demonstrating strong predictive accuracy. One study analyzing demographic and clinical data from 538 confirmed COVID-19 cases using logistic modeling, ROC curves, and Bayesian discriminant functions predicted disease severity to assist early diagnosis and patient stratification [33, 34]. This demonstrates the feasibility of model-assisted clinical decision-making for early diagnosis and patient stratification, while another study collected hematology and other clinical data from over 12,000 COVID-19 patients across 16 Hubei hospitals, exploring whether blood indexes could predict mortality risk [33]. However, predictions of COVID-19 severity in MHD patients remain scarce. Therefore, our prediction model results could aid clinicians in more precise risk evaluation and personalized treatment planning. Moreover, nomograms are often utilized to forecast cancer prognosis and have recently been widely applied in predicting terminal events across various fields and diseases [35, 36], demonstrating favorable predictive performance and clinical utility. Moving forward, it is essential to continue investigating risk factors for severe COVID-19 in MHD patients while proactively developing and integrating predictive models, including those powered by machine learning (ML) and artificial intelligence (AI) technologies. These advanced tools can enhance the accuracy and applicability of clinical predictions for various conditions, including chronic diseases and infectious diseases, providing more intuitive and rational information for junior doctors, patients, and health administrators in their decision-making processes [37, 38]. By leveraging model-based information supported by AI and ML, clinicians can enable individualized treatment plans and actively implement appropriate interventions, thereby prolonging patient survival and improving the quality of life for MHD patients.
Regarding SARS-CoV-2 infectivity, studies report the highest transmission risk occurs in the first week of infection, while generally, infectivity starts around 48 h before symptom onset [39]. Under normal circumstances, COVID-19 recovery takes 7–10 days. Many experiences symptom improvement by day 5 yet remain infectious. Research finds viral clearance time correlates with disease severity. One study observing 94 SARS-CoV-2 infected cases discovered mild patients had average viral clearance of 11 days, while severe patients averaged 20 days [26]. Another study indicated nasal irrigation could accelerate viral elimination, shortening time to clearance [40], but whether this applies to MHD patients requires further investigation. Notably, self-testing kits have some false negative rates, thus negative results cannot completely preclude infectious risk. Convalescent patients exhibit substantial declines in antibody levels and neutralizing antibodies within 2–3 months post-infection, indicating that previous exposure may not confer long-term immunity. Furthermore, significant correlations were found between time to viral clearance and several parameters. Specifically, cardiovascular-related parameters such as troponin and procalcitonin showed strong correlations. In contrast, parameters like white blood cells, neutrophils, and C-reactive protein are more indicative of inflammatory/infectious processes. These findings generate hypotheses about the interconnected mechanisms linking viral persistence, inflammation, kidney dysfunction, and cardiovascular injury in patients, which merit further mechanistic investigation.
There is presently limited literature on viral clearance times in COVID-19 positive MHD patients, however dialysis patients still require active treatment and isolation precautions post-SARS-CoV-2 infection to prevent transmission. Levels of CRP, BNP, and troponin differed between groups. CRP is a non-specific inflammatory marker that can rise in acute inflammation, infection, and trauma [41, 42]. BNP is a cardiovascular biomarker that elevates in conditions like heart failure [43]. However, BNP levels are influenced by various factors beyond cardiac function, particularly in patients with chronic kidney disease (CKD). In CKD patients, BNP levels can be elevated due to decreased renal clearance, fluid overload, and other non-cardiac factors, complicating its interpretation as a pure marker of cardiac function. While these parameters may be utilized for diagnosis, monitoring, and assessing disease status, they lack diagnostic specificity. Moreover, few studies compare rapid versus delayed clearance groups for COVID-19. Re-analyzing groups by a 14-day cutoff revealed a significant GFR difference between rapid and delayed clearers, while CRP, BNP, and troponin no longer differed. However, research indicates SARS-CoV-2 can precipitate acute kidney injury, potentially by directly infecting renal cells, eliciting inflammation, and damaging tissues [44]. Viral infection may also incite systemic inflammatory response syndrome and circulatory dysfunction, hampering kidney perfusion and GFR. Nevertheless, the GFR discrepancy between rapid and delayed clearers may relate to the extent of renal damage from COVID-19, but more studies are imperative to verify this hypothesis.
5 Study limitations
While this study had some meaningful findings, there were also certain limitations. (1) As a retrospective study, causal relationships cannot be established. (2) The relatively small sample size may have introduced bias or instability in the results. (3) All participants were from a single hospital; thus, the generalizability of findings may be restricted. (4) This study only analyzed COVID-19 positive cases among patients with uremia, therefore conclusions are confined to this population and manifestations may differ in other groups. (5) Although we considered some potential risk factors, there may be other important variables influencing COVID-19 presentation and severity in dialysis patients that were overlooked. Hence, further research is imperative to validate our results and explore additional risk factors. Despite these limitations, our study still provides valuable insights and can offer useful clinical guidance for COVID-19 positive dialysis patients. Moving forward, larger multi-center prospective studies are warranted to consolidate our findings and gain deeper understanding of COVID-19 in this vulnerable population.
6 Conclusion
In this study, we assessed clinical and hematological profiles from 85 COVID-19 positive hemodialysis patients to identify risk factors for severe disease outcomes. We found that cardiovascular disease, elevated white blood cell and neutrophil counts, and increased procalcitonin levels are significant predictors of severity. A predictive model incorporating these markers showed robust efficacy in forecasting severe COVID-19 risks. Additionally, prolonged viral presence correlated with elevated inflammatory markers such as C-reactive protein, interleukin-6, and neutrophils. These results underscore the importance of using these prognostic factors for risk stratification and tailored treatment in this vulnerable group. Further multicenter studies are needed to validate and refine these findings, reinforcing the case for personalized medicine approaches to optimize outcomes for dialysis-dependent patients with COVID-19.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due. The datasets generated during and/or analyzed during the current study are not publicly available due to hospital policy restrictions. Any unauthorized disclosure or transfer of data to non-hospital regions is subject to penalties. but data may be made available from the corresponding author upon reasonable request.
References
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–12.
Sykes RA, Neves KB, Alves-Lopes R, Caputo I, Fallon K, Jamieson NB, et al. Vascular mechanisms of post-COVID-19 conditions: rho-kinase is a novel target for therapy. Eur Heart J Cardiovasc Pharmacother. 2023. https://doi.org/10.1093/ehjcvp/pvad025.
Feng Z-Y, Ren X-W, Duren ZN, et al. Human Genetic Variants Associated with COVID-19 Severity are Enriched in Immune and Epithelium Regulatory Networks. Phenomics. 2022;2:389–403.
Kant S, Menez SP, Hanouneh M, Fine DM, Crews DC, Brennan DC, et al. The COVID-19 nephrology compendium: AKI, CKD, ESKD and transplantation. BMC Nephrol. 2020;21:449.
Ng JH, Hirsch JS, Hazzan A, Wanchoo R, Shah HH, Malieckal DA, et al. Outcomes among patients hospitalized with COVID-19 and acute kidney injury. Am J Kidney Dis. 2021;77:204-215.e1.
Molina-Mora JA, González A, Jiménez-Morgan S, et al. Clinical Profiles at the Time of Diagnosis of SARS-CoV-2 Infection in Costa Rica During the Pre-vaccination Period Using a Machine Learning Approach. Phenomics.2022;2:312–322.
Chung EYM, Palmer SC, Natale P, Krishnan A, Cooper TE, Saglimbene VM, et al. Incidence and outcomes of COVID-19 in people with CKD: a systematic review and meta-analysis. Am J Kidney Dis. 2021;78:804–15.
Hsu CM, Weiner DE, Aweh G, Miskulin DC, Manley HJ, Stewart C, et al. COVID-19 among US dialysis patients: risk factors and outcomes from a national dialysis provider. Am J Kidney Dis. 2021;77:748-756.e1.
Chester AC, Schreiner GE. Maintenance hemodialysis. JAMA. 1981;245:2026.
Ohnishi T, Kimachi M, Fukuma S, Akizawa T, Fukuhara S. Postdialysis hypokalemia and all-cause mortality in patients undergoing maintenance hemodialysis. Clin J Am Soc Nephrol. 2019;14:873–81.
Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, Bragg-Gresham J, et al. US renal data system 2014 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2015;66:Svii, S1-305.
Sun Y, Wang Y, Yu W, Zhuo Y, Yuan Q, Wu X. Association of dose and frequency on the survival of patients on maintenance of hemodialysis in China: a Kaplan-Meier and Cox-proportional hazard model analysis. Med Sci Monit. 2018;24:5329–37.
Yu S-B, Yuan H-H, Salerno S, Gou S-J, Chen W-W, Yang H-L, et al. Risk factors for mortality at beginning of maintenance hemodialysis. Chin Med J. 2020;133:868–70.
Pethő ÁG, Kevei P, Juha M, Kóczy Á, Ledó N, Tislér A, et al. The impact of COVID-19 infection before the vaccination era on the hospitalized patients requiring hemodialysis: a single-center retrospective cohort. Ren Fail. 2023;45:2251593.
Sim JJ, Huang C-W, Selevan DC, Chung J, Rutkowski MP, Zhou H. COVID-19 and survival in maintenance dialysis. Kidney Med. 2021;3:132–5.
Selvaskandan H, Hull KL, Adenwalla S, Ahmed S, Cusu M-C, Graham-Brown M, et al. Risk factors associated with COVID-19 severity among patients on maintenance haemodialysis: a retrospective multicentre cross-sectional study in the UK. BMJ Open. 2022;12: e054869.
Canoglu K, Caliskan T, Sinmez E. Risk factors for prolonged nucleic acid conversion time in patients with COVID-19. Int J Health Sci. 2022;16:32–6.
Galán MI, Velasco M, Casas ML, Goyanes MJ, Rodríguez-Caravaca G, Losa-García JE, et al. Hospital-Wide SARS-CoV-2 seroprevalence in health care workers in a Spanish teaching hospital. Enferm Infecc Microbiol Clin. 2022;40:302–9.
Hu B, Guo H, Zhou P, Shi Z-L. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19:141–54.
Punchoo R, Bhoora S, Bangalee A. Laboratory considerations for reporting cycle threshold value in COVID-19. EJIFCC. 2022;33:80–93.
Shah VP, Farah WH, Hill JC, Hassett LC, Binnicker MJ, Yao JD, et al. Association between SARS-CoV-2 cycle threshold values and clinical outcomes in patients with COVID-19: a systematic review and meta-analysis. Open Forum Infect Dis. 2021;8: ofab453.
Saha S, Al-Rifai RH, Saha S. Diabetes prevalence and mortality in COVID-19 patients: a systematic review, meta-analysis, and meta-regression. J Diabetes Metab Disord. 2021;20:939–50.
Martin-Blondel G, Marcelin A-G, Soulié C, Kaisaridi S, Lusivika-Nzinga C, Zafilaza K, et al. Time to negative PCR conversion amongst high-risk patients with mild-to-moderate Omicron BA1 and BA2 COVID-19 treated with sotrovimab or nirmatrelvir. Clin Microbiol Infect. 2023;29:543.e5-543.e9.
Sharma A, Tiwari S, Deb MK, Marty JL. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): a global pandemic and treatment strategies. Int J Antimicrob Agents. 2020;56:106054.
Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87:281–6.
Pandit JA, Radin JM, Chiang D, Spencer EG, Pawelek JB, Diwan M, et al. The COVID-19 rebound study: a prospective cohort study to evaluate viral and symptom rebound differences in participants treated with nirmatrelvir plus ritonavir versus untreated controls. Clin Infect Dis. 2023. https://doi.org/10.1093/cid/ciad102.
de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LMJ, Ansell D, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302:1782–9.
Fajgenbaum DC, June CH. Cytokine storm. N Engl J Med. 2020;383:2255–73.
Costela-Ruiz VJ, Illescas-Montes R, Puerta-Puerta JM, Ruiz C, Melguizo-Rodríguez L. SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. 2020;54:62–75.
Tong X, Cheng A, Yuan X, Zhong X, Wang H, Zhou W, et al. Characteristics of peripheral white blood cells in COVID-19 patients revealed by a retrospective cohort study. BMC Infect Dis. 2021;21:1236.
Zhao K, Li R, Wu X, Zhao Y, Wang T, Zheng Z, et al. Clinical features in 52 patients with COVID-19 who have increased leukocyte count: a retrospective analysis. Eur J Clin Microbiol Infect Dis. 2020;39:2279–87.
Palladino M. Complete blood count alterations in COVID-19 patients: a narrative review. Biochem Med. 2021;31:030501.
Liu Y-M, Xie J, Chen M-M, Zhang X, Cheng X, Li H, et al. Kidney function indicators predict adverse outcomes of COVID-19. Med. 2021;2:38-48.e2.
Kocadagli O, Baygul A, Gokmen N, Incir S, Aktan C. Clinical prognosis evaluation of COVID-19 patients: an interpretable hybrid machine learning approach. Curr Res Transl Med. 2022;70:103319.
Dong Y-M, Sun J, Li Y-X, Chen Q, Liu Q-Q, Sun Z, et al. Development and validation of a nomogram for assessing survival in patients with COVID-19 pneumonia. Clin Infect Dis. 2021;72:652–60.
Hess DR. A nomogram for use of non-invasive respiratory strategies in COVID-19. Lancet Digit Health. 2021;3:e140–1.
Lu Z-H, Yang M, Pan C-H, Zheng P-Y, Zhang S-X. Multi-modal deep learning based on multi-dimensional and multi-level temporal data can enhance the prognostic prediction for multi-drug resistant pulmonary tuberculosis patients. Sci One Health. 2022;1:100004.
Zhang S-X, Wang J-C, Li Z-W, Zheng J-X, Zhou W-T, Yang G-B, et al. Impact factors of Blastocystis hominis infection in persons living with human immunodeficiency virus: a large-scale, multi-center observational study from China. Infect Dis Poverty. 2023;12:82.
Boucau J, Uddin R, Marino C, Regan J, Flynn JP, Choudhary MC, et al. Characterization of virologic rebound following nirmatrelvir-ritonavir treatment for coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2023;76:e526–9.
Long Q-X, Tang X-J, Shi Q-L, Li Q, Deng H-J, Yuan J, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26:1200–4.
Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Front Immunol. 2018. https://doi.org/10.3389/fimmu.2018.00754.
van der Meer V, Neven AK, van den Broek PJ, Assendelft WJJ. Diagnostic value of C reactive protein in infections of the lower respiratory tract: systematic review. BMJ. 2005;331:26.
Babuin L, Jaffe AS. Troponin: the biomarker of choice for the detection of cardiac injury. CMAJ. 2005;173:1191–202.
Ahmadian E, Hosseiniyan Khatibi SM, Razi Soofiyani S, Abediazar S, Shoja MM, Ardalan M, et al. Covid-19 and kidney injury: Pathophysiology and molecular mechanisms. Rev Med Virol. 2021;31: e2176.
Acknowledgements
Not applicable.
Declaration of generative AI in scientific writing
During the preparation of this work the author(s) used [OpenAI-ChatGPT tool] in order to polishing the languages. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
Funding
The study was supported by China National Science Foundation (82070740, 81870492), and National Key Research and Development Program (2016YFC1305402).
Author information
Authors and Affiliations
Contributions
WWM concept the whole manuscript and supervised the whloe process, JXZ wrote the main manuscript text and analyst the data, and XL, LLX, XH, PPQ, and DL. prepared the clinical data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance for this retrospective study was obtained from the Ethics Committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. The study adhered to the principles outlined in the Declaration of Helsinki (http://www.wma.net/en/30publications/10policies/b3/index.html). Prior to data collection, comprehensive information about the study was communicated to all subjects, and they were fully informed about the study’s content and their participation rights. Informed consent was obtained from all participants in accordance with national guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zheng, JX., Li, X., Xu, LL. et al. Assessing risk factors and time to viral clearance on maintenance hemodialysis patients with COVID-19: a retrospective study. Discov Public Health 21, 64 (2024). https://doi.org/10.1186/s12982-024-00181-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12982-024-00181-2