Abstract
Background
To evaluate the prevalence of dry eye disease (DED) and its associated risk factors in a sample of the Argentine population.
Methods
A prospective cross-sectional population-based study was conducted in Argentina during April 2022 through an anonymous electronic survey that included participants aged 12 years old or older. The prevalence of symptomatic DED was evaluated using the Women's Health Study (WHS) dry eye questionnaire. In addition, a list of conditions possibly related to dry eye were evaluated in the questionnaire to assess the prevalence of potential risk factors. A multivariate logistic regression analysis was performed.
Results
10,812 subjects (mean age 44.1 ± 13.9, range 12–94 years old) answered the survey. Overall prevalence of DED was 42.1%. DED prevalence in women was 45.1% (3848 out of 8525) and in men was 30.8% (704 out of 2287). Risk factors were female sex (OR 2.78; p < 0.001), age > 60 years (OR 2.92), rheumatologic disease (OR 2.80, CI 1.62–3.13), use of digital screens for more than 6 h per day (OR 2.62; CI 1.43–2.80), glaucoma topical treatment (OR 2.05; CI 1.20–3.01), dysthyroidism (2.03; CI 1.48–2.51), and sleeping less than 7 h per day (OR 1.92; CI 1.30–2.51).
Conclusion
DED was found to be a prevalent condition among Argentine participants, the main risk factors were determined by sex, age, and especially those related to lifestyle in South America.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Dry eye disease (DED) is one of the most common disorders of the tear film and ocular surface. Also, is a growing multifactorial global health problem, the etiology and pathophysiology are still poorly understood [1]. The prevalence is often underestimated because of varying presentation symptoms. Studies have demonstrated that advancing age and female sex are significantly associated with increased risk of DED [2,3,4,5,6]. Epidemiological studies can be considered of significant importance because of the description that they provide regarding distribution of a disease, the identification of factors that influence that distribution, the measurement of the impact and the morbidity of a disease in defined populations [6].
Global prevalence of DED was reported to be 5–50% [6]. There have been many population studies about the prevalence and risk factors of DED [1,2,3,4,5, 7,8,9,10,11,12,13,14,15]. However, none of them were focused on South America [6] with the exception of two studies [10, 11] performed in Brazil. It is important to improve the understanding of DED, in order to know whether the differences in prevalence rates among studies might be attributed to ethnicity, geographic, climatic, environmental variations or lifestyle as mentioned in the TFOS DEWS II [6]. The Epidemiology Report refers to the paucity of data, especially in populations under 40 years of age [6]. Argentina is a country with a low population density. It experiences diverse climatological conditions, predominantly a warm climate, but also tropical characteristics in the north and subpolar regions in the southeast. The ethnic characteristics of the Argentine population are the result of the interaction of the aboriginal population with Iberian-European colonists to which, over the years, European and Asian immigration, mostly Italian and Spanish, was added.
The COVID 19 pandemic produced a change in the world, mainly modifying the lifestyle by increasing the hours of screen use for most activities, with direct and indirect consequences on the ocular surface [12]. The “TFOS lifestyle: Impact of societal challenges on the ocular surface report¨, mentions that long-term changes in remote or flexible work and study practices will persist beyond the pandemic [13]. Most of the studies focus on women [9] but it is interesting to analyze whether post-pandemic COVID 19 changes affect men differently, since the risk factors for dry eye are different [14], as well as what happens in younger populations.
The aims of this study were to assess the prevalence of DED and identify potential risk factors by sex and age for this ocular surface disorder in a sample of the Argentine population.
2 Materials and methods
2.1 Study design and ethics
A cross-section population study was designed to evaluate DED symptoms and risk factors in Argentina. The study was carried out in accordance with the Declaration of Helsinki and the Ethical Review Board of “Hospital El Cruce” approved the study protocol. Considering this was a nationwide study, it was also evaluated and approved by the Ministry of Health of Buenos Aires province and the Argentinian Ocular Surface Society. The study follows the personal data law protection of Argentina (number 25326) and “Digital Informed consent” was obtained before having access to the questionnaire.
2.2 Population and parameters
The study was carried out during April 2022 through an anonymous volunteer electronic questionnaire, developed in Google Forms platform. During the same month, the questionnaire link was distributed and shared in different ways, and people over 12 years old were included. For that purpose, a study group was created. At least one ophthalmologist was designated for each province and was included in this study group. Instructions were given via WhatsApp message, for all participating ophthalmologists. We included 23 provinces and Buenos Aires City. The survey could be accessed through a link where each ophthalmologist shared on social networks such as Facebook, Instagram, Whatsapp groups, mailing, radio and television as well as a QR code was available for patients to scan during appointments. The group encouraged the general population to participate explaining the objective of the work and also with an information campaign for teaching about ocular surface diseases.
Since the primary purpose of the study was to analyze the prevalence of symptomatic DED, questions were based on the Women's Health Study (WHS) dry eye questionnaire [16]. This short questionnaire with 3 questions has been validated and used in a prevalence study in Brazil [10, 11]. This dry eye questionnaire is the most widely used in population-based studies [6, 9,10,11, 15, 16]. It includes 2 questions about DED symptoms: “How often do your eyes feel dry?” and “How often do your eyes feel irritated?” with answer options: 0 never, 1 sometimes, 2 often, or 3 constantly. A third question is about a previous clinical diagnosis of DED: “Have you ever been diagnosed as having dry eye syndrome?” and the possible answers were yes or no. The “Dry eye” condition was defined by the presence of severe dry eye symptoms (both dryness and irritation indicated as constantly or often) detected by the questionnaire, or an affirmative answer about previous diagnosis of DED by an ophthalmologist or a general practitioner. As mentioned, this questionnaire was previously used in other population studies and was reported to provide a high specificity for dry eye.
In addition, demographic data and a list of conditions possibly related to DED were evaluated. The participants answered YES/NO to the following questions: (a) Lifestyle: sleep < 7hs/day, use of digital screens > 6hs/day, smoking; (b) History of diseases (thyroid disease, diabetes, rheumatic disease): (c) Medications: radio or chemotherapy, antiallergic drugs, isotretinoin, antidepressants and/or oral contraceptive; (d) ophthalmic conditions: history of ocular surgery, glaucoma topical treatment, contact lens wear. The entire form is available as supplementary data (Online Resource 1) in Spanish version.
2.3 Statistics
A descriptive statistical evaluation was performed with all of the obtained data. Subsequently, the results were analyzed by applying a univariate regression design, considering the Odds ratio (OR) and 95% confidence interval (CI). All risk factors that were associated with a P-value lower than 0.10 were selected to finally develop a logistic regression of the data, in the context of a multivariate study, in order to determine the relevance of the potential risk factors in the population studied, considering the DED criteria as the main outcome factor.
This multivariate analysis was performed for the entire population, and a second sub-analysis was also performed for the group of women and men, independently. P-values of less than 0.05 were considered statistically significant differences. A statistical analysis was performed with the XLMiner Analysis ToolPak software (Frontline Systems Inc.). Data is registered at “R.O.M.A.T. creator center” and is available upon request to the corresponding author.
3 Results
3.1 Population characteristics and prevalence of dry eye by sex and age
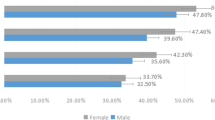
A total of 10,812 participants were included in the study, 8525 women (78.8%) and 2287 men (21.2%), with a mean age of 44.1 ± 13.9 years (range 12–94). Table 1 summarizes the demographics, showing the evaluated characteristics (first column) for the total studied population (second column), for the subgroups of dry eye, previous dry eye diagnosis and severe dry eye symptoms (third, fourth and fifth columns respectively). The percentages were calculated to know the partial prevalence within each of these subgroups (calculated based on the total value presented in the second row). The overall prevalence of DED was 42.1% (4552 out of 10.812), the majority being women (3848 were women and 704 were men; OR 2.78; CI 95% 1.7–2.1; p < 0.001) as is presented in Table 2. In the subgroup by sex analysis, women showed a DED prevalence of 45.1% (3848 out of 8525) and DED prevalence in the men's group was 30.8% (704 out of 2287). The percentage of people with DED in relation to the total number of participants according to age and sex is presented in Fig. 1.
In Table 2 it is possible to observe that age is a risk factor for DED in women from 25 years old and over, with significant impact mainly after the age of 60 (OR 2.55), meanwhile in the men's group, age is not a risk factor for DED.
3.2 Dry eye risk factors
In the population studied the frequency of risk factors (Table 2) was as follows: in relation to lifestyle, 1872 (17.3%) reported sleeping less than 7 h, being exposed to screens for more than 6 h a day, 2524 (23.3%), and 552 (5.1%) people answered that they were smokers. History disease/condition: 484 rheumatological disease (4.4%) thyroid disease 1008 (9.3%), diabetes 182 (1.6%). Elective treatment oral contraceptives 623 (5.7%) antiallergic 543 (5%) antidepressant 411 (3.8%) radio or chemotherapy 124 (1.1%) isotretinoin 60 (0.5%). Ocular history/condition: artificial tears 3197 (29.5%) ocular surgery 677 (6.2%) contact lens wear 509 (4.7%) glaucoma topical treatment 150 (1.3%).
In the DED group (4552 cases) the potential risk factors were present in Table 2. The association with the number of participants, OR, 95% CI, and their statistical significance were presented. The results were analyzed for the total population, in each parameter, and also discriminated by sex. In Table 2, the percentage of each risk factor in relation to the total population of 10,812 participants has also been calculated and shown. Likewise, to visualize the representation of the number of people who have a risk factor and DED, the percentage of each risk factor in the groups with DED, in relation to the total number of people who have that characteristic (with and without DED), has also been calculated and presented.
Figure 2 presents the eight risk factors for dry eye whose odds ratios were statistically significant for women and six risk factors that were statistically significant for men. In women's group, the significant risk factors were rheumatologic disease (OR 2.74), use of digital screens for more than 6 h per day (OR 2.71), the use glaucoma topical treatment (OR 2.12), thyroid disease (OR 1.98), sleeping less than 7 h/day (OR 1.89), antidepressant treatment (OR 1.86), contact lens use (OR 1.39), and previous ocular surgery (OR 1.25). In contrast, for men´s group, the significant risk factors were sleeping less than 7 h/day (OR 2.03), rheumatologic disease (OR 1.82), antidepressant treatment (OR 1.78), glaucoma topical treatment (OR 1.58), use of digital screens for more than 6 h per day (OR 1.47) and, thyroid disease (OR 1.12).
The possibly modifiable risk factors as digital screen use, hours of sleep and contact lens use, distributed by age, are shown in Fig. 3. The survey also addressed the use of artificial tears. Positive answer was found in 40% (Table 2) of the general population (4.327/10.812). The distribution according to decade of life, of people with DED that use lubricants, is also shown in Fig. 3. Considering the DED Group 70.2% were under ocular lubricants regimen (3197/4552) while in ̈No DED Group, 18% (1130/6260). Figure 3 shows all of the participants that answered about using lubricants, with the discrimination of the number of people who use lubricants regarding whether to have DED or not.
4 Discussion
This is the first population-based study of DED prevalence and risk factors carried out in a sample of the Argentine population, with a large number of participants. The association found between age, female sex, together with lifestyle-related aspects such as the use of digital screens, the use of contact lenses or sleep disorders, provide us with information to understand why we observe more frequent dry eye problems in young people [9, 11, 13, 17, 18].
The general prevalence of DED found in this population of 10,812 participants from all Provinces of Argentina was 42.1%. There is not enough information about prevalence of DED in South America yet, except for the Castro study in Brazil [10] which showed a prevalence of 12.8% with dry eye; previous diagnosis was reported by 10.2% and presence of severe symptoms in 4.9%. In the present study, the previous diagnosis of dry eye was found in 27.7% and the presence of severe symptoms in 14.4%. In both studies, the same methodology was used to analyze DED and risk factors to unify and improve the regional information. Disparities in results can occur despite the proximity between the two countries, Argentina is the southernmost country in the continent, and there are different ethnic groups and different geographical and weather conditions. This study was done after the COVID 19 pandemic and may be one of the reasons for the higher prevalence of DED in Argentina due to direct and indirect changes in people's lifestyles. Also, our results of DED prevalence are higher compared to Europe too, ranging from 10 to 22%, and those in the United States, ranging from 7 to 15% [3].
A symptoms evaluation might be an important variable in the DED pathway [17]. In fact, DED prevalence rates based on the report of symptoms have been widely used [6, 9,10,11]. In the present study we evaluated separately dry eye diagnosis (previously diagnosed by an ophthalmologist) and severe symptoms. Analyzing subjective parameters, such as symptoms is a challenge [19]. Although the Ocular Surface Disease Index (OSDI) test is a widely validated tool, in our work, the possibility of using the WHS questionnaire, which was previously used in other population studies [9, 10, 16], and was reported to provide a high specificity for dry eye, allowed us to simultaneously reach all of the provinces of Argentina, through the use of digital technology, in a short period (30 days), with the same criteria used in a population-based study carried out in Brazil [10].
The statistical analysis carried out allows us to highlight the significant risk factors that were identified, mainly the female sex and age over 60 years. It is noteworthy that when comparing age groups, between men and women, the female sex continues to be a significant risk factor from 25 years old on as shown in Table 2. The prevalence of DED increased with age in both sexes, but age is not a risk factor in the men's group. There was a threefold increase in men from the age of 19 and then gradually increased in the following years, not in a significant way. On the other hand, the most significant increase was made in women after 60 years of age. There is a relevant difference in participation rates between the female and male, but while analyzing each group separately, women presented more DED than men. Out of 10 women, 4.5 presented DED, while 3 out of 10 male participants. It is interesting to focus on men, since it is less significant than women, it is still an important group to analyze as well as evaluate different risk factors (42% women DED and 30% Men DED).
Likewise, given that technological advances are changing lifestyles globally, it is also known that the digital environment can trigger, worsen or impact on ocular surface diseases [20]. Our study evaluated DED frequency and potential risk factors from the age of 12, and there are already reports that show an increase in prevalence in groups of younger people [9, 11, 21]. In the Netherlands study [9], a very large population of 79,866 participants was evaluated, showing that a relatively high prevalence of symptomatic dry eye in adults aged 20–30 was associated with contact lens wear which appeared to be a strong risk factor in the younger age categories. It could also be related to the increased use of screens, but in their review, did not have information regarding the use of such screens. A study was carried out on Brazilian undergraduate students [11] with an average age of 23 ± 5.2 years where an increase in prevalence was also observed with respect to those over 40 years and that female sex, contact lens wear, digital use for more than 6 h per day, less than 6 h of sleep per night, and certain medications were found relevant as risk factors for DED.
In Argentina, we have some evidence that the digital environment and the use of screens have directly influenced ocular surface problems. The context was developed during the COVID-19 pandemic [22]. The current study showed a higher prevalence of the symptoms or diagnosis of dry eye and the number of hours of screen use, greater than 6 h a day, according to what has been published, it would seem to have a potential proportional correlation [22, 23]. Likewise, there is still disagreement on the maximum time recommended for exposure to digital screens in order to avoid potential harm. This is a relevant issue, once the digital environment continues to grow in the context of screen use. Its relevance is revealed in the latest TFOS Lifestyle Workshop [13]. Authors such as Kamøy, Magno discussed about the vicious circle [24, 25] that is generated with the use of screens by decreasing the blink rate and/or increasing incomplete blinks, which generates instability of the tear film, the increase in evaporation and hyperosmolarity. With the increase in inflammation mediators, which promotes film instability and perpetuates the vicious circle. Regarding the epidemiology of eye strain, according to the TFOS Lifestyle Workshop, it is 70.7% with great variability and this is explained according to the criteria used for diagnosis, the equipment used, the task or ergonomic conditions, among others [13].
Regarding sleep, there was a high percentage of participants with dry eye criteria, who reported sleeping less than 7 h per day, which is in agreement to recent studies that evaluate this issue [26,27,28]. In the Netherlands study, 44.9% of participants who reported highly symptomatic dry eye (constant or frequent) had poor sleep quality [9, 28]. Sleep is an important factor for well-being and health in general. These disorders are associated with other comorbidities and DED in a multifactorial level [28]. Indeed, there are reports about tear film alteration and sleep deprivation and others claiming that the dry eye could be the cause of poor sleep quality as a bidirectional mechanism [27].
Among the most frequent comorbidities, we found rheumatic disease with a high odds ratio, no specific questioning was posed about type of disease or medication in use. However, it is relevant to point out that 71% of the participants in this study, who had a rheumatic disease, also had DED. Another systemic condition evaluated was thyroid disease, where 50% of those who developed thyroid disease also had DED. Published information shows that hormonal dysfunction may play a role in the DED [13, 27]. Data from a regional study, carried out in Entre Ríos, where there is a high prevalence of thyroid disease showed that those patients with dry eye problems are related to this disease (523 from 1752 cases; 29.8%) [29]. It is interesting to highlight that rheumatic and thyroid disease are also highly prevalent in females.
There is growing evidence that certain medications can be a risk factor for DED, mostly due to the decrease of the lacrimal gland secretion, such as anxiolytics, antidepressants and others [15, 30,31,32,33]. Antidepressants turned out to be a prominent risk factor in our study, even though there are contradictory publications. Some studies consider that selective serotonin reuptake inhibitors alter the production of the tear film [32], and other studies show that the beneficial effect on depression outweighs the risk of suffering from dry eye due to secondary cholinergic effects [9]. Finally, within the ophthalmological history, the use of antiglaucoma agents doubled the risk of dry eye symptoms in agreement with previous evidence [33]. Contact lens wear was also a significant risk factor in this population, as it induces the reduction in the breakup time of the tear film, thinning of the lipid layer and an increase in the rate of tear evaporation [34, 35]. In our study, we could observe that the age group most affected with DED associated with contact lens wear was 20 to 29 years old, similar to the results found in the Netherlands [9]. The history of ophthalmic surgery was shown to be a risk factor in this population and greater in women, but no statistically significant relationship was found in men. Previous data of a descriptive study carried out in Argentina [36] on ocular surface discomfort after ocular surgeries, revealed that cataract surgery was the most relevant procedure, beyond what is already known on refractive corneal procedures [37, 38].
An interesting find was that 40% of the participants use ocular lubricants (4327/10812), only 29.5% had a medical diagnosis of dry eye. Within the DED group, 70.2% used tears and 18% of the population without DED according to study criteria. Because of that, it will be important to consider for future similar studies that self-medication with artificial tears can potentially affect DED manifestation, masking symptoms.
Our study also has several potential limitations. First, the use of self-reporting of symptoms and a previous dry eye diagnosis, no clinical evaluation. DED diagnosis remains a challenge due to the lack of gold-standard methods and poor correlations among the most used tests [39]. It may bring bias in our analyses and final estimates. However, we have used a validated methodology to acquire information which help us to improve our knowledge of DED, in a part of the world where we had no local data until now. Second, we could not select the population to do a proper population-based design, since subjects were voluntarily included. We understand that our sample may have some bias, since in addition to the general population, people who attended clinics and hospitals and learned about the survey may have participated. Likewise, we can infer that those who have participated were interested in the subject because they either have some dry eye symptoms or have heard about this disease from family members or friends who have the condition. This makes us remark that our study potentially has a participation bias that we have not been able to mitigate. Conducting a population-based prevalence study is complex and we consider it very important to carry out an adequate population-based sampling scheme. At the time of designing our research protocol we did not find background information to be able to do it otherwise, so we decided to conduct this study in an open way, and to acquire a sample of our population for starting to obtain regional data. With the data from the present study, we plan different study designs for the future to mitigate the limitations raised.
Regarding the use of screens, we only evaluated the number of hours without considering the activity or the type of device. In addition to the sleep and DED, we only evaluated the number of hours or sleep duration, but not the quality of sleep or the use of sleeping medication. Finally, we found a significant difference between the voluntary participation of women and men which makes us wonder if there is a bias of greater participation in those who have symptoms and this could have led to false positive results. We believe the current study is a starting point in order to continue evaluating our population and confirm observed associations.
5 Conclusion
This is the first large population study performed in Argentina to evaluate DED and it is able to provide essential information regarding the epidemiological aspects. DED was found to be a prevalent condition among participants, the main risk factors were determined by sex, age, and especially those related to lifestyle. We believe this information is relevant not only for Argentina but also worldwide and could be used for future scientific comparisons.
Data availability
The dataset with all the participants' responses, through which the analysis has been carried out, is available at (Zenodo): doi: https://doi.org/10.5281/zenodo.10903549.
References
Hossain P, Siffel C, Joseph C, Meunier J, Markowitz JT, Dana R. Patient-reported burden of dry eye disease in the UK: a cross-sectional web-based survey. BMJ Open. 2021;11: e039209. https://doi.org/10.1136/bmjopen-2020-039209.
Dana R, Meunier J, Markowitz JT, Joseph C, Siffel C. Patient-reported burden of dry eye disease in the United States: results of an online cross-sectional survey. Am J Ophthalmol. 2020;216:7–17. https://doi.org/10.1016/j.ajo.2020.03.044.
Siffel C, Hennies N, Joseph C, Lascano V, Horvat P, Scheider M, et al. Burden of dry eye disease in Germany: a retrospective observational study using German claims data. Acta Ophthalmol. 2020;98:e504–12. https://doi.org/10.1111/aos.14300.
Uchino M. What we know about the epidemiology of dry eye disease in Japan. Invest Ophthalmol Vis Sci. 2018;59(14):DES1–6. https://doi.org/10.1167/iovs.17-23491.
Song P, Xia W, Wang M, Chang X, Wang J, Jin S, et al. Variations of dry eye disease prevalence by age, sex and geographic characteristics in China: a systematic review and meta-analysis. J Glob Health. 2018;8: 020503. https://doi.org/10.7189/jogh.08.020503.
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–65. https://doi.org/10.1016/j.jtos.2017.05.003.
Donthineni PR, Kammari P, Shanbhag SS, Singh V, Das AV, Basu S. Incidence, demographics, types and risk factors of dry eye disease in India: electronic medical records driven big data analytics report I. Ocul Surf. 2019;17:250–6. https://doi.org/10.1016/j.jtos.2019.02.007.
Wang MTM, Vidal-Rohr M, Muntz A, Diprose WK, Ormonde SE, Wolffsohn JS, et al. Systemic risk factors of dry eye disease subtypes: a New Zealand cross-sectional study. Ocul Surf. 2020;18:374–80. https://doi.org/10.1016/j.jtos.2020.04.003.
Vehof J, Snieder H, Jansonius N, Hammond CJ. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul Surf. 2021;19:83–93. https://doi.org/10.1016/j.jtos.2020.04.005.
Castro JS, Selegatto IB, Castro RS, Miranda ECM, de Vasconcelos JPC, de Carvalho KM, et al. Prevalence and risk factors of self-reported dry eye in Brazil using a short symptom questionnaire. Sci Rep. 2018;8:2076. https://doi.org/10.1038/s41598-018-20273-9.
Yang I, Wakamatsu T, Sacho IBI, Fazzi JH, de Aquino AC, Ayub G, et al. Prevalence and associated risk factors for dry eye disease among Brazilian undergraduate students. PLoS ONE. 2021;16: e0259399. https://doi.org/10.1371/journal.pone.0259399.
Lulla NH, Loganathan M, Balan VGM, Swathi S. Dry eye among medical students before and during COVID-19. Indian J Ophthalmol. 2023;71:1468–71. https://doi.org/10.4103/IJO.IJO_2786_22.
Stapleton F, Abad JC, Barabino S, Burnett A, Iyer G, Lekhanont K, et al. TFOS lifestyle: impact of societal challenges on the ocular surface. Ocul Surf. 2023;28:165–99. https://doi.org/10.1016/j.jtos.2023.04.006.
Schaumberg DA, Dana R, Buring JE, Sullivan DA. Prevalence of dry eye disease among US men: estimates from the Physicians’ Health Studies. Arch Ophthalmol. 2009;127:763–8. https://doi.org/10.1001/archophthalmol.2009.103.
Koçer E, Koçer A, Özsütçü M, et al. Dry eye related to commonly used new antidepressants. J Clin Psychopharmacol. 2015;35(4):411–3. https://doi.org/10.1097/JCP.0000000000000356.
Schaumberg DA, Sullivan DA, Buring JE, et al. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136(2):318–26. https://doi.org/10.1016/s0002-9394(03)00218-6.
Farrand KF, Fridman M, Stillman IÖ, et al. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90–8. https://doi.org/10.1016/j.ajo.2017.06.033.
Osae EA, Jones L, Nichols JJ. The impact of contact lenses on meibomian gland morphology. Ocul Surf. 2022;24:148–55. https://doi.org/10.1016/j.jtos.2022.04.001.
Gulati A, Sullivan R, Buring JE, Sullivan DA, Dana R, Schaumberg DA. Validation and repeatability of a short questionnaire for dry eye syndrome. Am J Ophthalmol. 2006;142:125–31. https://doi.org/10.1016/j.ajo.2006.02.03.
Wolffsohn JS, Lingham G, Downie LE, Huntjens B, Inomata T, Jivraj S, et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023;28:213–52. https://doi.org/10.1016/j.jtos.2023.04.004.
García-Ayuso D, Di Pierdomenico J, Moya-Rodríguez E, Valiente-Soriano FJ, Galindo-Romero C, Sobrado-Calvo P. Assessment of dry eye symptoms among university students during the COVID-19 pandemic. Clin Exp Optom. 2022;105:507–13. https://doi.org/10.1080/08164622.2021.1945411.
Liviero B, Favalli M, Maccio JP, Aguirre T, Romera Verzini J, Endrek MS. Pantallas y sintomas de la superficie ocular en cuarentena por COVID-19. Oftalmol Clin Exp. 2020;13:195–206.
Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3: e000146. https://doi.org/10.1136/bmjophth-2018-000146.
Kamøy B, Magno M, Nøland ST, Moe MC, Petrovski G, Vehof J, et al. Video display terminal use and dry eye: preventive measures and future perspectives. Acta Ophthalmol. 2022;100(7):723–39. https://doi.org/10.1111/aos.15105.
Magno MS, Utheim TP, Snieder H, Hammond CJ, Vehof J. The relationship between dry eye and sleep quality. Ocul Surf. 2021;20:13–9. https://doi.org/10.1016/j.jtos.2020.12.009.
Li A, Zhang X, Guo Y, Wang J, Hao Y, Gu Y, et al. The association between dry eye and sleep disorders: the evidence and possible mechanisms. Nat Sci Sleep. 2022;14:2203–12. https://doi.org/10.2147/NSS.S378751.
Lee YB, Koh JW, Hyon JY, Wee WR, Kim JJ, Shin YJ. Sleep deprivation reduces tear secretion and impairs the tear film. Invest Ophthalmol Vis Sci. 2014;55:3525–31. https://doi.org/10.1167/iovs.14-13881.
Ayaki M, Toda I, Tachi N, Negishi K, Tsubota K. Preliminary report of improved sleep quality in patients with dry eye disease after initiation of topical therapy. Neuropsychiatr Dis Treat. 2016;12:329–37. https://doi.org/10.2147/NDT.S94648.
Torres RM, Lódolo PG. Twelve years of Ocular Surface Disease management: clinical characteristics and demographics in Entre Rios, Argentina (abstract). Invest Ophthalmol Vis Sci. 2019;60:4729.
Kawashima M. Systemic health and dry eye. Invest Ophthalmol Vis Sci. 2018;59:DES138–42. https://doi.org/10.1167/iovs.17-23765.
Yu K, Bunya V, Maguire M, Asbell P, Ying GS, Dry Eye Assessment and Management Study Research Group. Systemic conditions associated with severity of dry eye signs and symptoms in the dry eye assessment and management study. Ophthalmology. 2021;128:1384–92. https://doi.org/10.1016/j.ophtha.2021.03.030.
Rakofsky JJ, Rakofsky SI, Dunlop BW. Dry those crying eyes: the role of depression and antidepressants in dry eye disease. J Clin Psychopharmacol. 2021;41(3):295–303. https://doi.org/10.1097/JCP.0000000000001382.
Gomes JAP, Azar DT, Baudouin C, Efron N, Hirayama M, Horwath-Winter J, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511–38. https://doi.org/10.1016/j.jtos.2017.05.004.
Jones L, Efron N, Bandamwar K, Barnett M, Jacobs DS, Jalbert I, et al. TFOS lifestyle: impact of contact lenses on the ocular surface. Ocul Surf. 2023;29:175–219. https://doi.org/10.1016/j.jtos.2023.04.010.
Harbiyeli II, Bozkurt B, Erdem E, Ozcan HG, Cam B, Sertdemir Y, et al. Associations with meibomian gland loss in soft and rigid contact lens wearers. Contact Lens Anterior Eye J Br Contact Lens Assoc. 2022;45(1): 101400. https://doi.org/10.1016/j.clae.2020.12.005.
Torres R, Lódolo PG. Ocular surface after ocular surgeries (abstract). Invest Ophthalmol Vis Sci. 2020;61:388.
Naderi K, Gormley J, O’Brart D. Cataract surgery and dry eye disease: a review. Eur J Ophthalmol. 2020;30:840–55. https://doi.org/10.1177/1120672120929958.
Nair S, Kaur M, Sharma N, et al. Refractive surgery and dry eye - an update. Indian J Ophthalmol. 2023;71:1105–14. https://doi.org/10.4103/IJO.IJO_3406_22.
Alves M, Reinach PS, Paula JS, Vellasco e Cruz AA, Bachette L, Faustino J, et al. Comparison of diagnostic tests in distinct well-defined conditions related to dry eye disease. PLoS ONE. 2014;9: e97921. https://doi.org/10.1371/journal.pone.0097921.
Acknowledgements
Acknowledgment Dr. Mercedes Leguia, Chief of the Ophthalmology Service of Hospital El Cruce, who helped and collaborated so that this study could be carried out. To the Argentine Council of Ophthalmology (CAO) and the members of the board of the Ocular Surface Society of Argentina (SASO), Drs. Liliana Abuín, Alejandro Aguilar, Paula Albera, Alejandro Berra, Martín Berra, María A. Borrone, Ricardo Brunzini, Julieta Gelardi, Fernanda Girado, Francisco Lucero-Saá, Rogelio Ribes, Eugenia Sibay, Jorge L. Tredicce, and Florencia Valvecchia for their support during the management of the study. Finally, we would like to express our gratitude to our collaborating ophthalmologist, present in each province of Argentina (described in the Online Resource 2), without whom we would not have been able to have this large number of participants. They also helped us to disseminate information about dry eye disease among the general population.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by [Rodrigo M. Torres], [María Cecilia Marini] and [Belén Liviero]. The first draft of the manuscript was written by [Rodrigo M. Torres] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Marini, M.C., Liviero, B., Torres, R.M. et al. Epidemiology of dry eye disease in Argentina. Discov Public Health 21, 59 (2024). https://doi.org/10.1186/s12982-024-00185-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12982-024-00185-y