Abstract
Background
The center of pressure (COP) excursion parameters are recognized as risk factors for the etiology and development of patellofemoral pain (PFP). The purpose of the present study measures the effect of pain exacerbation on COP excursion, and the correlation between pain intensity and COP excursion in women with PFP during single leg squat (SLS).
Methods
Sixty patients with PFP participated in this cross-sectional study. The outcome measures were included pain intensity and COP excursion which evaluated in pre and post pain exacerbation during SLS. The COP parameters were evaluated during single leg squat in 60° of knee flexion. A paired t-test and MANOVA was used to compare pain intensity and COP excursion between the two conditions, respectively. Furthermore, A Pearson’s correlation matrix was used to examine the relationship between pain intensity with COP excursion.
Results
Statistical analysis showed that pain intensity (t = − 16.655, p < 0.001) and COP excursion (Wilks’ Lambda = 0.225, p < 0.001) with medium effect size increased after PFJ loading. In addition, an excellent positive correlation was observed between increased in pain intensity and COP excursion (P < 0.001, r > 0.80).
Conclusion
After PFJ loading, women with PFP presented increases in the pain intensity, COP excursions, and sway velocity. In addition, there was an association between the increase in pain intensity and COP excursions. Clinicians aiming to improve postural control of patients with PFP could use kinesio taping as a short-term intervention and balance training to improvements in postural control at medium and long-term. Furthermore, emphasizing psychological factors to reducing kinesiophobia can be useful to restoring proper movement pattern, reducing pain and improving symptoms.
Similar content being viewed by others
Background
Patellofemoral pain (PFP) defined as pain in the retropatellar or peripatellar region [1, 2]. This orthopedic condition is aggravated by the patellofemoral joint (PFJ) loading [3, 4]. The prevalence of PFP in the general population and professional athletes has been reported as 22.7% and 35.7%, respectively [5]. It has been shown PFP is more common in females aged 18 to 35 years with an estimated prevalence being 13% [6, 7]. Researchers speculate there are many biomechanical and anatomical alignment factors that may lead to the increased incidence of PFP in females compared with males. These factors include increased Q-angle, increased dynamic knee valgus, reduced lower extremity muscle strength, increased hip internal rotation, hip adduction moment, and knee abduction moment, and decreased knee flexion angle [8]. Despite the high prevalence, the PFP etiology is unknown [6]. However, growing body of research suggests psychological factors (e.g. kinesiophobia) have play a more important role in self-reported pain, function, and disability and have greater influence on movement impairments in women with PFP [9, 10]. Importantly, change behavior due to kinesiophobia in patients with PFP may change kinematics and lead to detrimental effects at the PFJ [9, 10].
Postural control involves a complex integration of visual, vestibular and somatosensory systems based on reflex actions occurring to postural stability [11, 12]. The center of pressure (COP) path assessment is the most common technique for balance assessment, which represents the average absolute pressure exerted by the body on the ground [11]. The changes of COP parameters are recognized as risk factors for the etiology and development of PFP [11, 13]. More specialized, alterations in COP parameters can impact on force transmission through the lower limb kinetic chain and lead to lower extremity overuse injuries, including PFP [13]. In this line, Thijes et al. (2007) reported the COP shifted more slowly from the lateral to the medial side during foot rollover; this could cause less shock absorption in the foot [14]. Consequently, a greater part of the ground reaction forces is transferred to the more proximal joints that could result in an overloading of the PFJ, which would lead to PFP [14]. Mostly, balance restore is neglected in the PFP rehabilitation protocols and conflicting findings to interventions effectiveness in improve postural control have been reported [11, 15]. It is believed that pain, proprioceptive defects, central control, and abnormal muscle activities are the main mechanisms in the poor balance of PFP patients [11]. In painful conditions, sensory impulses may be impairing in the central and peripheral levels of the central nervous system (CNS) and subsequently disruption of movement control and balance [3, 11].
Recently, a systematic review and meta-analysis with quantitative synthesis of 53 studies reported that very low to moderate certainty evidence indicated that patients with PFP have worse anterior- posterior and overall stability indexes during single-leg stance (SMD = 0.71, 95% CI: 1.29, 0.14; SMD = 0.63, 95%CI: 0.94, 0.32) [15]. Greater COP displacements during dynamic tasks are signs of poor postural control that can higher risk for developing subsequent injuries [15]. Nevertheless, the results of COP analysis show conflicting evidence of COP excursion in PFP patients [16]. For example, Saad et al. (2015) demonstrated females with PFP had higher COP excursion during stair negotiation compared to healthy individuals [17]. In contrast, Silva et al. (2016) reported females with PFP had lower COP excursion during stair climbing [16]. It seems the conflicting evidence was due to the fact that the patients did not have their worst pain when at the time of data collection [16]. Therefore, studies which aimed on pain intensity controlling during data collection is necessary to understand this conflicts. In this regard, previous studies reported the PFJ loading protocol is useful for pain exacerbation in females with PFP and there is a positive correlation between PFJ loading and pain intensity [6, 18]. Furthermore, a meta-analysis indicates that pain intensity in patients with PFP were increased during walking, running, squatting and stair ambulation [19]. Since previous studies showed the PFJ loading exacerbation of the pain and symptoms of females with PFP [18]; It seems different intensity of pain in females with PFP demonstrate different strategies during biomechanical analyzes and clinical evaluations [18]. Thus, the PFJ loading is important factor in physiological or biomechanical strategies when the presence of pain [18, 20].
There is little information about the effect of pain on the balance of patients with PFP has not been investigated. Now the question is whether pain intensity can affect COP excursion. Meanwhile, the studies reported that there is conflicting evidence regarding the relationship between pain and balance [11]. Thus, understanding the effect of pain intensity can provide new insights to management and treatment of PFP [21]. Therefore, the purpose of the current study was 1) the immediate effect of pain exacerbation on COP excursion 2), and the relationship between pain intensity with COP excursion in women with PFP during single leg squat (SLS). We hypothesized that (1) the PFJ loading would significantly increase pain intensity and COP excursion (2) there would be significantly positive correlations between pain intensity with COP excursion.
Method
Participants
The statistical population of the current study were females with PFP (age: 38.90 ± 3.33 years, weight: 59.13 ± 3.9 kg, height: 169.53 ± 4.6 cm). We recruited patients who visited in the orthopedic clinics of Hamedan province from January to April 2023. First, an orthopedic clinician and a physiotherapist (with 15 years of experience) screened the patients through non-invasive tests (stair descent /Clark test). If the PFP symptoms were positive and there were eligibility criteria, the patient was invited to the movement analysis and rehabilitation laboratory.
Inclusion criteria included: pain intensity of 3 out of 10 visual analog scale (VAS), pain exacerbation during weight bearing activities, normal alignment of upper and lower limbs, age range of 18–45 years, unilateral symptoms (PFP in right knee), and suffering from PFP for more than 6 weeks. Exclusion criteria included: history of physical therapy, participation in professional and recreational sports, history of surgery, upper and lower limb malalignment, vestibular and vision disorders, injury and pain in other joints (except PFJ). Ethical approval of the present study was obtained from the Ethics Committee in Biomedical Research of Bu-Ali sina University with the code IR.BASU.REC.1402.012. Before data collection, patients signed an informed consent form. Also, we followed the Helsinki Declaration of 2008.
Sample size
We used the free software G*Power version 3.1.9.2 to sample size planning. Using the reference of a related study that evaluated the effect of PFJ loading on pain intensity, and vertical loading rate, the type I error rate was 0.05, the type II error was 0.20 and the estimated correlation coefficient (r) = 0.5 was planned [6]. The output of the software reported at least 26 subjects [6]. However, we enrolled 60 subjects to increase statistical power.
Instrumentation
A plantar pressure platform (ZEBRIS GmbH, Isny, Germany; ICC = 0.91) made in Germany was used to record the COP excursion [22]. The Zebris plantar pressure has a platform with dimensions of 54 × 34 cm and 2560 active sensors with high sensitivity [23]. This platform records the pressure in the range of 1–120 N/cm2 with a sampling rate of 50 Hz [22]. In addition, Zebris FDM software was used to process and export the data (Fig. 1). The COP parameters including: minor axis (COP displacement in mediolateral direction) and major axis (COP displacement in anteroposterior direction), and sway velocity (Fig. 2).
The horizontal purple line is the connecting line of the three COPs (Center of pressure). The ellipse around includes 95% of the COPs. The middle cross is the center of pressure of the whole body. Minor axis (total traveling distance of COP displacement in mediolateral direction) and major axis (total traveling distance of COP displacement in anteroposterior direction)
Experimental protocol
First, we performed randomization through Random Allocation Software. According to the study of Briani et al. (2018), a random order of four block was planned [6]. Thus, block 1 and 2 were considered for the first and second days of pre- pain exacerbation condition. Also, block 3 and 4 were considered for the first and second days of post- pain exacerbation condition. Consequently, conditions or days were randomized. Of note, we assessed pain and COP excursion in pre and post pain exacerbation.
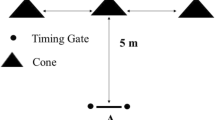
In pre- pain exacerbation condition (without PFJ loading), patients were asked to indicate pain intensity (resting time) as real-time on a 10-cm VAS. Then, patients were asked to perform the SLS three times. In post- pain exacerbation condition (with PFJ loading), the PFJ loading protocol was applied to pain exacerbation. The PFJ loading protocol consisted of a staircase with seven steps (each step being 18 cm high), which participants performed 15 repetitions of stair negotiation with an external load of 35% of the subject’s body mass (carried in a backpack) [6]. Afterward, the pain intensity of the patients was evaluated on a 10-cm VAS and patients were asked immediately to perform the SLS three times. Of note, data collection was done in symptomatic limb (i.e. right limb). Importantly, PFJ loading protocol does not cause neuromuscular fatigue [18]. However, to be sure, we evaluated patients’ fatigue after the PFJ loading protocol using the Borg scale.
Task and procedure
The COP displacement in anterior-posterior direction, medial-lateral direction, and sway velocity was recorded during SLS. The SLS is a common clinical assessment that trial balance and musculoskeletal disorders of the lower limbs [24]. Before data recording, information was provided to the patients to familiarize with the test. The patients were taught to stand upright on the platform and place hands on the chest to remove the effect of hands on balance control (they stood on the right foot/limb painful). Of note, in the test limb the hip and knee were in extended position, whilst the contralateral limb from back was flexed to 90° [25]. The head was placed in a neutral position to prevent the vestibular disturbance. The ankles and feet were set in a neutral position.
The SLS were perform up to 60° of knee flexion. We used a flexible electro-goniometer to record the knee joint angle during SLS and made feedback to the patient when the knee reaches the target angle. Before starting the data collection, the patients were familiar with the test and practiced the trial 3 times. A 2-minute rest was considered between each trial to minimize fatigue. The International Society for Posture and Gait Research recommends that evaluation of postural control parameters between 25 and 40 s are reliable [26]. Overall, each patient performed SLS test in 3 separate trials and the rest period between each trial was 2 min. The duration of the SLS test in each trial was 30 s, and at this time the COP excursion data was collection. In record of COP excursion, the examiner was blind. Finally, the average of 3 trials was used for COP excursion analysis.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) (IBM; Armonk, NY, USA) version 21 was used for statistical analysis. Normal distribution of data and homogeneity of variances were checked with Shapirowilk and Levene tests, respectively. A paired t-test (two-tailed) was used to compare pain intensity between pre and post pain exacerbation. In addition, multivariate analysis of variance (MANOVA) to compared the results COP excursion between the two conditions. A Pearson correlation matrix was used to examine the relationship between pain intensity with COP excursion. Of note, the score change from pre- pain exacerbation condition to post- pain exacerbation condition (i.e., pre- pain exacerbation condition – post- pain exacerbation condition = score change) was used to the correlation calculation [6]. Therefore, positive values and negative values are indicating higher values in pre- pain exacerbation condition and post- pain exacerbation condition, respectively [6]. The correlation rates were interpreted in four categories as poor (r = 0.00 to 0.25), fair (r = 0.25 to 0.50), moderate to good (r = 0.50 to 0.75), or excellent (r = 0.75 to 1) [27]. The effect size was interpreted as small (d < 0.20), medium (d = 0.21–0.79), and large (d > 0.80) [28]. A significance level of P < 0.05 was considered.
Results
Table 1 shows the demographic data of the patients. No statistically significant difference was observed in demographic characteristics (age: 38.90 ± 3.33 years, height: 169.53 ± 4.6 cm, mass: 59.13 ± 3.9 kg, BMI: 20.66 ± 1.53 kg/m2, pain duration: 11.52 ± 3.14 months, kujala score: 49.81 ± 8.70 points); So the data distribution is normal (p > 0.05). Paired t-test show pain intensity is significantly higher in post- pain exacerbation condition (7.0 ± 1.0 cm) compared to pre- pain exacerbation condition (4.33 ± 1.0 cm) (Fig. 3) with a large effect size (t 59 = − 16.655, P < 0.001, d = − 1.27). The MANOVA analysis showed a significant difference in the COP parameters between pre and post pain exacerbation (Wilks’ Lambda = 0.225, p < 0.001). The compared between pre and post pain exacerbation showed a significant difference with a medium effect size in the COP anterior - posterior displacement (F 1, 118= 133.099, P < 0.001, η2 = 0.530), medial - lateral displacement (F 1, 118= 80.279, P < 0.001, η2 = 0.405), and sway velocity (F 1, 118= 391.700, P < 0.001, η2 = 0.768) (Table 2).
Table 3 shows in the anterior - posterior parameter, an increased COP excursion was shown in post- pain exacerbation condition (36.51 ± 9.99 mm) compared to pre- pain exacerbation condition (19.51 ± 5.50 mm). In the medial - lateral parameter, an increased COP excursion was shown in post- pain exacerbation condition (39.26 ± 9.38 mm) compared to pre- pain exacerbation condition (26.93 ± 5.04 mm). In the sway velocity parameter, an increased sway velocity was shown in post- pain exacerbation condition (28.03 ± 5.57 mm) compared to pre- pain exacerbation condition (12.68 ± 2.24 mm) (Fig. 4).
Pearson correlation matrix showed excellent positive correlation between the increase in pain intensity with COP excursion in anterior-posterior direction (P < 0.001, r = 0.823) (Fig. 5), medial - lateral direction (P < 0.001, r = 0.839) (Fig. 6), and sway velocity (P < 0.001, r = 0.810) (Fig. 7) from pre- pain exacerbation condition to post- pain exacerbation condition.
Discussion
The present study evaluated the immediate effect of PFJ loading on (1) pain intensity and COP excursion (2) the relationship between pain intensity with COP excursion in women with PFP. In the present study, results showed that pain exacerbation negatively influences postural control after PFJ loading. In addition, a positive correlation was observed between increased pain intensity with COP excursion. In general, by reasoning on previous studies, we believe that the increase in pain intensity through neuromuscular system defects increases the COP excursion. As a result, both of our hypotheses are supported. Our results agreement made with previous studies with a similar purpose. For example, Briani et al. (2018) found a positive correlation between pain levels with loading rate during stair negotiation [6].
Postural control during dynamic movements is maintained through muscle strength and proprioception [29]. Previous studies reported poor balance in patients with PFP is associated with weak muscle strength and proprioception deficits [11, 30]. The motor system is responsible for activating muscles to movement. Weak muscle strength, especially when accompanied by pain can lead to make postural instability [31]. In general, balance control and pain-induced muscle inhibition have common pathways in the CNS [32]. Previous study reported that pain increases the presynaptic inhibition of muscle afferents and effects the central modulation of the muscle spindles and proprioception; finally, muscle control decreases [32]. Silva et al. (2016) believed that knee extensor muscles control COP excursion in the anterior-posterior direction [31]. Furthermore, Wu et al. (2002) found the eccentric strength of the knee extensors was associated with the COP displacement in anterior – posterior direction [33]. Meanwhile, Gribble (2004) showed that local fatigue of hip and knee extensor muscles leads to postural instability in the anterior-posterior direction [34]. Briani et al. (2020) reported a decrease in peak knee extensor moment following the pain exacerbation [35]. The quadriceps muscle inhibition can be the result of spinal reflex inhibition of the alpha motor neuron. This reflex inhibition is modulated by pre- and post-synaptic mechanisms and it is created by abnormal afferent from a painful joint [21]. Therefore, pain causes a decrease in motor impulses to the muscles; As a result, the potential of the muscle to produce force is limited [21]. Thus, the mechanism of muscle inhibition caused by pain lead to increase COP excursion in the sagittal plane.
On the other hand, increasing COP displacement in the anterior-posterior direction may be a compensatory strategy to reducing PFJ stress or pain resulting from high quadriceps activity [13]. Overall, the PFJ stress is influenced by the quadriceps muscle force and knee flexion angle [36]. Thus, decreased quadriceps activation “quadriceps avoidance” could be a compensatory strategy to reduce PFJ stress [21]. Following this, reduction in the knee extensor moment likely compensate by increasing the ankle plantar flexor moment, leading to a greater displacement of the COP in the anterior direction and increase tibialis anterior activity [13, 35]. As a result, this mechanism can facilitate the plantar flexor muscles recruitment to absorbing the vertical ground reaction force and reducing the load transfer to the knee [13]. In addition, increased activation of the ankle plantar flexors may increase hip extensor demand during SLS; thus decrease quadriceps muscle demand [13]. However, this compensatory mechanism may have negative consequences in this joints [35].
On the other hand, with the anterior displacement of the COP, a larger part of the body’s weight is transferred to the forefoot region, which leads to a higher plantar pressure in this area [37]. In this line, Thijs et al. (2015) reported that greater loading on the second and third metatarsals can transmit higher vertical forces to the knee joint, which is an important factor in identifying individuals at risk of PFP [14]. Furthermore, Rathleff et al. (2014) reported that patients with PFP showed higher loading of the forefoot, which has the potential to transfer harmful forces to the external area of the PFJ and develop PFP [38].
Carry et al. (2017) reported that patients with PFP significantly increased COP displacement in the medial - lateral direction compared to the control group during SLS [39]. The moment arm of the gluteus medius muscle is longer than other muscles of the lower limb [40]. The gluteus medius controls frontal and sagittal plane movement by minimizing medial - lateral COP acceleration [31]. The pain onset in patients with PFP can reduce ability of the gluteus medius to control adduction and internal rotation of the hip. The abductor and external rotator muscles of the hip contraction eccentrically to control adduction and internal rotation [41]. As a result, weakness and abnormal activation of the gluteus medius lead to adduction and internal rotation of the hip [42]. In this regard, Lee et al. (2012) reported PFP patients which have hip abductor weakness showed postural instability in the frontal plane. Also, Neghaban et al. (2018) showed hip muscle fatigue leads to increased COP displacement in the medial - lateral direction [43]. In this regard, a decrease in COP displacement in the medial-lateral direction were showed to using a hip stabilizer brace [40]. Therefore, it is argued the pain intensity had correlation to faulty kinematic of the lower limbs, muscle incoordination, and arthrogenic inhibition of the hip and quadriceps muscles [21]. Finally, the pain intensity can effect COP excursion in females with PFP through of the inhibition mechanisms of hip and quadriceps muscles.
Limitations
We had three limitations in this study. First, the current study is cross-sectional, so we cannot determine the cause and effect relationship. Second, our statistical population was only females; Therefore, caution should be generalizing the results to men’s population. Third, since only SLS were trialed (because of time constraints), the findings may not reliable to generalize challenging tasks. Therefore, we recommend future studies evaluation the effect of the PFJ loading on kinematic and kinetic variables during challenging tasks in both genders.
Clinical applications
Our findings highlight the potential importance of pain exacerbations during painful daily activities on the imbalance and falls risk in women with PFP. Thus, this study showed that any future study for COP measurements in women with PFP should considered on the effect of pain intensity. Since impaired postural control is a risk factor for PFP and lower extremity injury, clinicians should assess and treat these outcomes in patients with PFP as part of a comprehensive rehabilitation program [15]. In this line, since pain impulses interfere with proprioception, it seems the focus of a rehabilitation program in women with PFP with increased COP excursions can include focusing on pain neuroscience education and proprioception training. Furthermore, clinicians aiming to improve postural control of patients with PFP could use kinesio taping as a short-term intervention and balance training to improvements in postural control at medium- and long-term [15]. Of note, Furthermore, emphasizing psychological factors to reduce kinesiophobia can be useful to restoring proper movement pattern, reducing pain and improve symptoms [9, 10]. A synthesis of treatment effectiveness would benefit clinicians targeting postural control measures [15].
Conclusion
After PFJ loading, women with PFP presented increases in the pain intensity, COP excursions, and sway velocity. In addition, there was an association between the increase in pain intensity and COP excursions. As a result, increasing PFJ loading during challenging activities is an important issue that must be considered in clinical evaluations of females with PFP.
Data availability
We undertake that the data will be available and sent if needed and requested by the journal and reviewers.
References
Yalfani A, Ahmadi M. Patients with patellofemoral pain exhibiting decrease vertical ground reaction force compared to healthy individuals during weight bearing tasks: a systematic reviews and meta-analysis. Iran J Public Health. 2023;52(2):254.
Yalfani A, Ahadi F, Ahmadi M, Asgarpoor A. Relationship between exacerbating patellofemoral pain and dynamic knee valgus in females with patellofemoral pain after a patellofemoral joint loading protocol: a cross-sectional. Phys Ther Sport. 2024;67:13–8.
Silva NC, de Castro Silva M, Tamburús NY, Guimarães MG, de Oliveira Nascimento MB, Felicio LR. Adding neuromuscular training to a strengthening program did not produce additional improvement in clinical or kinematic outcomes in women with patellofemoral pain: a blinded randomised controlled trial. Musculoskelet Sci Pract. 2023;63:102720.
Yalfani A, Ahmadi M. Effect of neurofeedback training on psychological features and plantar pressure distribution symmetry in patients with patellofemoral pain: a ransdomized controlled trial. J Bodyw Mov Ther. 2024;40:141–7.
Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, Rathleff MS, Smith TO, Logan P. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS ONE. 2018;13(1):e0190892.
De Oliveira Silva D, Briani R, Pazzinatto M, Ferrari D, Aragão F, De Azevedo F. Vertical ground reaction forces are associated with pain and self-reported functional status in recreational athletes with patellofemoral pain. J Appl Biomech. 2015;31(6):409–14.
Yalfani A, Ahmadi M, Asgarpoor A. The effect of kinetic factors of dynamic knee valgus on patellofemoral pain syndrome: a systematic review and meta-analysis. J Bodyw Mov Ther. 2023.
Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sport. 2010;20(5):725–30.
De Oliveira Silva D, Barton CJ, Briani RV, Taborda B, Ferreira AS, Pazzinatto MF, de Azevedo FM. Kinesiophobia, but not strength is associated with altered movement in women with patellofemoral pain. Gait Posture. 2019;68:1–5.
De Oliveira Silva D, Willy RW, Barton CJ, Christensen K, Pazzinatto MF, Azevedo FM. Pain and disability in women with patellofemoral pain relate to kinesiophobia, but not to patellofemoral joint loading variables. Scand J Med Sci Sports. 2020;30(11):2215–21.
Nunes GS, Rodrigues DZ, Hörbe L, Prates I, Tessarin BM, Serrão FV, de Noronha M. Is postural control affected in people with patellofemoral pain and should it be part of rehabilitation? A systematic review with meta-analysis. Sports Medicine-Open. 2022;8(1):144.
Ahmadi M, Yalfani A, Gandomi F, Rashid K. The effect of twelve-week neurofeedback training on pain, proprioception, strength and postural balance in men with patellofemoral pain syndrome: a double-blind randomized control trial. J Rehabilitation Sci Res. 2020;7(2):66–74.
Gwynne CR. Alterations in center of pressure during single-limb loading in individuals with patellofemoral pain. J Am Podiatr Med Assoc. 2020;110(2).
Thijs Y, Tiggelen D, Van, Roosen P, Clercq D, De, Witvrouw E. A prospective study on gait-related intrinsic risk factors for patellofemoral pain. Clin J Sport Med. 2007;17(6):437–45.
Batista NP, Silva DD, Mochizuki L, Norte GE, Bazett-Jones DM. Clinic-and laboratory-based measures of postural control in patellofemoral pain: a systematic review with meta-analysis and evidence gap map. Volume 3. Gait & Posture; 2024 Feb.
De Oliveira Silva D, Magalhães FH, Pazzinatto MF, Briani RV, Ferreira AS, Aragão FA, de Azevedo FM. Contribution of altered hip, knee and foot kinematics to dynamic postural impairments in females with patellofemoral pain during stair ascent. Knee. 2016;23(3):376–81.
Saad MC, Felício LR, Masullo C, de Liporaci L, Bevilaqua-Grossi RF. Analysis of the center of pressure displacement, ground reaction force and muscular activity during step exercises. J Electromyogr Kinesiol. 2011;21(5):712–8.
Briani RV, Pazzinatto MF, De Oliveira Silva D, Azevedo FM. Different pain responses to distinct levels of physical activity in women with patellofemoral pain. Brazilian J Phys Ther. 2017;21(2):138–43.
Glaviano NR, Bazett-Jones DM, Boling MC. Pain severity during functional activities in individuals with patellofemoral pain: a systematic review with meta-analysis. J Sci Med Sport. 2022;25(5):399–406.
Pazzinatto MF, de Oliveira Silva D, Barton C, Rathleff MS, Briani RV, de Azevedo FM. Female adults with patellofemoral pain are characterized by widespread hyperalgesia, which is not affected immediately by patellofemoral joint loading. Pain Med. 2016;17(10):1953–61.
Greuel H, Herrington L, Liu A, Jones RK. How does acute pain influence biomechanics and quadriceps function in individuals with patellofemoral pain? Knee. 2019;26(2):330–8.
Chaharmahali L, Gandomi F, Yalfani A, Fazaeli A. The effect of self-reported knee instability on plantar pressure and postural sways in women with knee osteoarthritis. J Orthop Surg Res. 2021;16(1):1–10.
Yalfani A, Raeisi Z. Bilateral symmetry of vertical time to stabilization in postural sway after double-leg landing in elite athletes with unilateral chronic ankle sprain. J Foot Ankle Res. 2022;15(1):1–9.
Ugalde V, Brockman C, Bailowitz Z, Pollard CD. Single Leg Squat Test and its relationship to dynamic KneeValgus and Injury Risk Screening. PM R. 2015;7(3):229–35.
Gwynne CR, Curran SA. Two-dimensional frontal plane projection angle can identify subgroups of patellofemoral pain patients who demonstrate dynamic knee valgus. Clin Biomech. 2018;58:44–8.
Scoppa F, Capra R, Gallamini M, Shiffer R. Clinical stabilometry standardization. Basic definitions - Acquisition interval - sampling frequency. Gait Posture. 2013;37(2):290–2.
Nunes GS, Barton CJ, Viadanna Serrão F. Females with patellofemoral pain have impaired impact absorption during a single-legged drop vertical jump. Gait Posture. 2019;68:346–51.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. 1988.
Rosen AB, Ko J, Brown CN. The relationship between acute pain and dynamic postural stability indices in individuals with patellar tendinopathy. Gait Posture. 2018;65:117–20.
Zeinalzadeh A, Talebian S, Naghdi S, Salavati M, Nazary-Moghadam S, Zeynalzadeh Ghoochani B. Effects of vision and cognitive load on static postural control in subjects with and without patellofemoral pain syndrome. Physiother Theory Pract. 2018;34(4):276–85.
de Carvalho-e-Silva MC, Peixoto AP, Leão Almeida G, Oliveira Magalhães M, Renovato França FJ, Vidal Ramos LA, Comachio J, et al. Dynamic postural stability and muscle strength in patellofemoral pain: is there a correlation? Knee. 2016;23(4):616–21.
Eker Y, Kaygisiz BB. The effect of pain severity on balance, postural stability and fall risk in patients with shoulder pathologies. Arch Med Sci. 2021;17(2):390–6.
Wu G, Zhao F, Zhou X, Wei L. Improvement of isokinetic knee extensor strength and reduction of postural sway in the elderly from long-term Tai Chi exercise. Arch Phys Med Rehabil. 2002;83(10):1364–9.
Gribble PA, Hertel J. Effect of lower-extremity muscle fatigue on postural control. Arch Phys Med Rehabil. 2004;85(4):589–92.
Briani RV, Cannon J, Waiteman MC, Negrão Filho R, de F, Magalhães FH, de Azevedo FM. Influence of the exacerbation of patellofemoral pain on trunk kinematics and lower limb mechanics during stair negotiation. Gait Posture. 2021;83:83–7.
Hart HF, Patterson BE, Crossley KM, Culvenor AG, Khan MCM, King MG et al. May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions—a systematic review and meta-analysis. Br J Sports Med. 2022;521–30.
Pau M, Mandaresu S, Leban B, Nussbaum MA. Short-term effects of backpack carriage on plantar pressure and gait in schoolchildren. J Electromyogr Kinesiol. 2015;25(2):406–12.
Rathleff MS, Richter C, Brushøj C, Bencke J, Bandholm T, Hölmich P, et al. Increased medial foot loading during drop jump in subjects with patellofemoral pain. Knee surgery. Sport Traumatol Arthrosc. 2014;22(10):2301–7.
Carry PM, Gala R, Worster K, Kanai S, Miller NH, James D, Provance AJ, Carollo JJ. Postural stability and kinetic change in subjects with patellofemoral pain after a nine-week hip and core strengthening intervention. Int J Sports Phys Therapy. 2017;12(3):314.
Lee SP, Souza RB, Powers CM. The influence of hip abductor muscle performance on dynamic postural stability in females with patellofemoral pain. Gait Posture. 2012;36(3):425–9.
De Vasconcelos GS, da Silva ME, Nunes GS, Serrão FV. Relationship between kinesiophobia, isometric hip and knee torques to pelvic, hip and knee motion during the single-leg drop jump in women with patellofemoral pain: a cross-sectional study. Knee. 2023;42:264–72.
Goto S, Aminaka N, Gribble PA. Lower-extremity muscle activity, kinematics, and dynamic postural control in individuals with patellofemoral pain. J Sport Rehabil. 2018;27(6):505–12.
Negahban H, Etemadi M, Naghibi S, Emrani A, Shaterzadeh Yazdi MJ, Salehi R, et al. The effects of muscle fatigue on dynamic standing balance in people with and without patellofemoral pain syndrome. Gait Posture. 2013;37(3):336–9.
Acknowledgements
We gratefully thank patients for volunteered participation in this study.
Funding
The current study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
F.A (Manuscript writing)A.Y (Edit the Manuscript)M.A (Data analysis).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent to participate Ethical approval of the present study was obtained from the Ethics Committee in Biomedical Research of Bu-Ali Sina University with the code IR.BASU.REC.1402.012. Before data collection, patients signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yalfani, A., Ahadi, F. & Ahmadi, M. Effects of pain exacerbation on postural control in women with patellofemoral pain during single leg squat: a cross-sectional study. J Orthop Surg Res 19, 462 (2024). https://doi.org/10.1186/s13018-024-04911-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04911-9