Abstract
Background
Preventing severe arthrogenic muscle inhibition (AMI) after knee injury is critical for better prognosis. The novel Sonnery-Cottet classification of AMI enables the evaluation of AMI severity but requires validation. This study aimed to investigate the electromyography (EMG) patterns of leg muscles in the examination position from the classification during isometric contraction to confirm its validity. We hypothesised that the AMI pattern, which is characterised by quadriceps inhibition and hamstring hypercontraction, would be detectable in the supine position during isometric contraction.
Methods
Patients with meniscal or knee ligament injuries were enrolled between August 2023 and May 2024. Surface EMG was assessed during submaximal voluntary isometric contractions (sMVIC) at 0° extension in the supine position for the vastus medialis (VM) and vastus lateralis (VL) muscles and at 20° flexion in the prone position for the semitendinosus (ST) and biceps femoris (BF) muscles. Reference values for normalisation were obtained from the EMG activity during the gait of the uninjured leg. The Kruskal–Wallis test was used to compare the activation patterns of the muscle groups within the same leg, and the post-hoc tests were conducted using the Mann–Whitney U test and Bonferroni correction.
Results
Electromyographic data of 40 patients with knee injuries were analyzed. During sMVIC, the extensor and flexor muscles of the injured leg showed distinct behaviours (P < 0.001), whereas the uninjured side did not (P = 0.144). In the injured leg, the VM differed significantly from the ST (P = 0.018), and the VL differed significantly from the ST and BF (P = 0.001 and P = 0.026, respectively). However, there were no statistically significant differences within the extensor muscle groups (VM and VL, P = 0.487) or flexor muscle groups (ST and BF, P = 0.377).
Conclusion
AMI was detectable in the examination position suggested by the Sonnery-Cottet classification. The flexor and extensor muscles of the injured leg exhibited distinct activation behaviours, with inhibition predominantly occurring in the quadriceps muscles, whereas the hamstrings showed excitation.
Similar content being viewed by others
Background
Arthrogenic muscle inhibition (AMI) is an innate protective reflex triggered by joint injury that protects the damaged knees by restricting joint motion [1, 2]. When the knee joint is injured, changes such as effusion and pain, alter articular sensory receptors, leading to inhibitory signals at the spinal cord level. This modulation affects the group 1 non-reciprocal (1B) inhibitory pathway, flexion reflex, and gamma loop (spinal and supraspinal pathways), thereby altering spinal reflex excitability [3,4,5,6]. As a result, decreased activation of the vastus medialis (VM) muscle and increased hamstring flexor reflex result in an asymmetric activation pattern of the leg muscles. This often results in the loss of terminal extension without mechanical intraarticular pathology, leading to flexion contracture, which hinders recovery [7]. Therefore, properly addressing AMI is critical to achieve better clinical outcomes.
Several studies have investigated the pathophysiology, contributing factors, and nature of AMI [1, 4,5,6, 8]. However, the lack of consensus on a grading system for evaluating AMI severity has hindered its comprehensive understanding. Recently, Sonnery-Cottet et al. introduced a novel classification system that facilitated quantitative evaluation, paving the way for further studies [9] (Table 1). This classification system is theoretically based on pathophysiology and assesses grades through physical examination findings, including the inspection of VM contraction during isometric extension in the supine position, the presence of extension deficits, and the response to short-term physiotherapy. Although this system is simple and feasible for daily practice, its validation and theoretical foundations are necessary for comprehensive advancements in this field. Specifically, because the classification examines patients in the supine position, it is essential to investigate whether this position is appropriate for assessing the degree of AMI, and whether the amount of muscle inhibition is accurately reflected in this position.
Among several methods for evaluating muscle activity, surface electromyography (EMG) is a valuable and non-invasive tool for assessing electrical muscle activity [10, 11]. Schilaty et al. assessed EMG in patients who underwent ACL reconstruction and found that the motor unit characteristics were altered [13]. Dos Anjos et al. have used EMG to assess the outcome of rehabilitation treatment in patients with AMI, as it provides real-time feedback on muscle function [14]. Its versatility makes it ideal for assessing AMI in various positions and motions both clinical and study settings [12].
Therefore, this study aimed to investigate the EMG patterns of leg muscles in the examination position from the Sonnery-Cottet classification during isometric contraction to confirm its validity. Activation failure patterns of the quadriceps and hamstring muscles were compared. We hypothesised that the AMI pattern, which is characterised by quadriceps inhibition and hamstring hypercontraction, would be detectable in the supine position during isometric contraction.
Methods
This study was approved by the Institutional Review Board of the medical centre of current study. The patient data were collected and assessed anonymously by the first author.
Participants
We prospectively recruited patients with meniscal or knee ligament injuries between August 2023 and May 2024. The inclusion criteria of the present study were as follows: knee ligament or meniscal injury, consent to participate in the study, ability to participate in kinematic analysis, and absence of fractures. Exclusion criteria were trauma requiring immediate surgical treatment, history of injury on the contralateral side, presence of moderate osteoarthritis (K–L grade ≥ 2), and artefacts on EMG data due to inadequate electrode contact.
EMG measurement
Electrical muscle activity was recorded by a single examiner in the gait analysis laboratory of the medical centre where the study was conducted. The four target muscles were the VM and vastus lateralis (VL) for the quadriceps, the semitendinosus (ST) and the biceps femoris (BF) for the medial and lateral hamstring. According to the Surface ElectroMyoGrapy for the Non-Invasive Assessment of Muscles (SENIAM) guidelines [15], the skin areas were shaved and cleansed with alcohol. For the VM, the electrodes were placed at 4/5 of the distance between the anterior superior iliac spine (ASIS) and the joint space anterior to the medial collateral ligament, parallel to the muscle fibre direction. For the VL, electrodes were placed at 2/3 of the distance between the ASIS and the lateral patella. For the ST and BF, electrodes were placed at half the distance between the ischial tuberosity and the medial and lateral epicondyles of the tibia, respectively [15, 16]. Wireless bipolar surface EMG sensors with an inter-electrode distance of 20 mm (LE230, Biometrics Ltd, UK) were used to measure the muscle activities on the bellies of four target muscles. The EMG electrodes were small (22 mm × 28 mm), disc-shaped, and silver/silver chloride electrodes designed for single or multiple applications to the same patient. The reference electrodes were placed on the tibial tuberosity of dominant knee. Real time EMG recordings were obtained using a portable EMG system (DataLITE PIONEER, Biometrics Ltd, UK). Surface EMG data were recorded at 1000 Hz (band-width 10-450 Hz, signal amplification 1000), and all data were stored anonymously on a designated storage device for analysis. Obtained EMG data were analysed using DataLITE Analysis software (PC version 11.02).
Experimental procedure
Electromyographic measurements were performed in two modes: repeated submaximal voluntary isometric contraction (sMVIC) and single free gait. Instead of using a standardised position for MVIC, which may cause discomfort to the patients, activities of the leg muscles during isometric contraction were measured at joint angles of 0° extension in the supine position (for VM and VL) and 20° flexion in the prone position (for ST and BF), according to the examining position used in the Sonnery-Cottet classification [9]. Patients were then asked to perform isometric contractions as hard as possible. The EMG activity of leg muscles varies, depending on the intensity of contraction and knee angle [17]. Thus, the isometric contractions were regarded as submaximal contractions.
First, VM and VL muscle activities during sMVIC were measured (Fig. 1A). The examiner placed a hand beneath the knee joint, providing a slight counterforce to enhance sensory feedback as the participants extended their knees. The participants were instructed to exert maximal effort, maintain force, and then relax quickly. This procedure was performed on both the injured and uninjured sides. Before recording, the patients were guided through three practice sMVICs to ensure familiarity with isometric contractions. The sMVICs were performed twice for 3 s each, with a 5-s rest period between repetitions. In the same manner, ST and BF activities were measured during sMVIC. While the patient was lying prone on the bed, the examiner resisted the ankle to provide a counterforce to the flexion contraction, keeping it stationary. The EMG activity during the mid-contraction of 1 of 3 s was assessed. To measure the EMG values during gait, the participants rested for 10 min after the sMVIC recordings. Following the rest period, the participants walked barefoot along a 12-m runway [18]. The EMG activity of uninjured leg during five gait cycles (entire stride, including both the swing and stance phases) was collected. These measurements were obtained at the midsection of the runway to represent average walking speed (Fig. 1C) [19].
Surface EMG examination. A Wireless surface EMG electrodes are attached to the belly of four target muscles. EMG during sMVIC for VM and VL muscles were measured at joint 0° extension in the supine position. B Likewise, EMG during sMVIC for ST and BF muscles were measured at 20° flexion in the prone position. C EMG activity during 5 gait cycle at the midsection of the 12-meter runway were collected to obtain the reference value for normalization. VM, vastus medialis; VL, vastus lateralis, ST, semitendinosus; BF, biceps femoris
Data processing
The obtained EMG data were analyzed using DataLITE Analysis PC software version 11.02 (Biometrics Ltd, UK). Raw EMG data from the sMVIC and gait trials were corrected for resting bias, converted to microvolts, and bandpass filtered at 10–450 Hz. The Root Mean Square (RMS) value was used to quantify the electric signal [16, 20]. The RMS value of the EMG was automatically calculated using a 100 ms moving-average window by the software. The EMG data during sMVIC were normalised to the reference value of EMG activity during the five strides of healthy leg muscles, referred to as the dynamic mean normalisation method [12]. Many authors have favoured the method because it has been reported to reduce inter-subject variability [21,22,23,24]. Moreover, the muscle activity of injured side during sMVIC (%) was normalised to the EMG amplitude of the uninjured side to compare the activation level of the four muscle groups.
The intraclass correlation coefficient was assessed to evaluate the validity of the measurement method. The raw EMG data of ten patients were randomly selected, processed, and assessed by two authors. The strength of agreement was interpreted as follows: 0.91, almost perfect agreement; 0.71–0.90, good agreement; 0.61–0.70, acceptable agreement; 0.51–0.60, poor agreement; and P < 0.50, unacceptable agreement. The intraobserver reliability and interobserver agreement were 0.996 (95% confidence interval [CI] 0.995–0.997; P < 0.001) and 0.912 (95% CI 0.873–0.941; P < 0.001) respectively, which were interpreted as almost perfect agreement.
Statistical analysis
An adequate sample size was estimated by power analysis using G*Power version 3.1.9.7 program (Universitat Kiel, Germany). Normalised mean EMG activities of VM, VL, ST, and BF during sMVIC were measured as 127.1, 160.0, 239.6, and 124.3%, respectively, from a pilot study of 10 patients. The effect size calculated from this sample was 0.38. Assuming a 95% significance level and 80% power, the required sample size was calculated to be 80 muscles, corresponding to 20 participants. The statistical analysis were performed using SPSS Statistics for Windows, version 25. Electromyography data are widely dispersed among individuals [12, 25, 26]. Therefore, the Kolmogorov–Smirnov test was conducted to assess the normality of the EMG data distribution. As normality was not satisfied, the Mann–Whitney U test was used to compare the differences between the injured and uninjured sides. To investigate the different inhibition patterns among muscles within the same leg, the EMG data were analysed using a Kruskal–Wallis test, followed by pairwise Mann–Whitney U tests with Bonferroni correction for intergroup comparisons. Statistical significance was set at P < 0.05.
Results
Participants
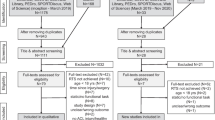
Among 71 patients who were diagnosed with ligament and meniscal injury, 7 patients were excluded from the study due to the history of contralateral knee injury and 11 patients were excluded due to the presence of moderate osteoarthritis (K–L grade ≥ 2). Among the 53 patients who underwent EMG, 13 with poor EMG data due to noise were excluded. Finally, 40 patients were included in the study (Fig. 2).
The included patients comprised 26 male and 14 female patients with a median age of 36.5 year (IQR 24.8–61.5). There were 22 knee ligament and 18 isolated meniscal injuries. The mean body mass index was 25.4 ± 3.5 kg/m2. The median time from injury to EMG examination was 2 days (IQR 2–4), and detailed patient characteristics are shown in Table 2.
Comparison of muscle activities during sMVIC
During the sMVIC, the dynamic mean normalisation method did not produce significant differences between the activities on the injured and uninjured sides in each muscle group. However, although there were no significant variations between the dynamic mean normalised activities of the muscles on the uninjured side (P = 0.144), the relative activities of the four muscles were altered after the injury (P < 0.001) (Table 3).
As the sMVIC of the injured leg muscles showed statistical significance in the Kruskal–Wallis test (P < 0.001), the post-hoc Mann–Whitney U test was conducted to compare the difference in activation level between the muscle groups. Significance values were adjusted using Bonferroni correction for multiple comparisons (Fig. 3A). This reveals a heterogeneous activation pattern between the extensor and flexor muscle groups. The VM showed significant differences compared to the ST (P = 0.018). Similarly, the VL muscle showed significant differences from the ST and BF muscles (P = 0.001 and P = 0.026, respectively). In contrast, there were no statistically significant differences within the extensor (VM and VL, P = 0.487) or flexor muscle groups (ST and BF, P = 0.377).
Comparison of activation level among leg muscles. A The EMG activity of injured leg during sMVIC (%) was normalised by dynamic mean method. Mann–Whitney’s U test was conducted to compare the difference in activation pattern between the muscle groups. Significance values was adjusted by the Bonferroni correction for multiple comparisons. *Indicates statistical significance (P value < .05). The activities of the extensor muscles were significantly lower than the flexor muscles after injury. B The EMG activity of injured leg during sMVIC (%) was normalised with regard to the EMG amplitude of the uninjured side during sMVIC. The quadriceps muscles exhibited inhibition, whereas the hamstring muscles showed hypercontractility. EMG, electromyography; sMVIC, submaximal voluntary isometric contraction; VM, vastus medialis; VL, vastus lateralis; ST, semitendinosus; BF, biceps femoris
The EMG activity of the injured leg during sMVIC normalised to EMG amplitude of the uninjured side revealed that the amount of activation failure was larger in the extensor muscle groups (83.9 ± 36.4% for VM and 93.7 ± 42.9% for VL, respectively) than in the flexor group (109.6 ± 44.7 for ST and 112.1 ± 57.7 for BF); however, there was no statistical significance (P = 0.051) (Fig. 3B).
Discussion
The main finding of this study was that surface EMG revealed distinct behaviours in the quadriceps and hamstring muscles of the injured leg. Consistent with previous studies [13, 19, 27,28,29], we observed that the quadriceps muscles (VM and VL) of the injured leg were inhibited in patients with AMI, whereas the hamstring muscles (ST and BF) were excited. Importantly, these differences in muscle activity were observed in the examined position of the Sonnery-Cottet classification [4], which primarily assessed AMI based on VM contractility and extension deficits caused by hamstring contracture while the patient was lying supine. This study supports the validity of the classification system which is practical for daily use. Another clinically important finding of this study was that AMI was observed in patient with acute knee injuries with various disease entities other than ACL injuries. Most studies on AMI have primarily focused on patients with ACL injuries [30,31,32,33,34]. In contrast, this study included a wider range of disease entities than ACL injury. Among the 40 participants in this study diagnosed with acute knee injuries, only 10 were diagnosed with ACL rupture. Nevertheless, the EMG findings of this study showed AMI patterns similar to those of other studies of AMI patterns after ACL injury alone. Although this might introduce heterogeneity into the study groups, it enhances the comprehensive understanding of AMI. However, it remains unclear whether AMI occurs acutely or persists chronically. Future studies with a larger number of participants would enable the comparison of AMI patterns among disease entities.
Several tools have been used to evaluate the muscle activity. Functional magnetic resonance imaging can be used to measure multilayered metabolic muscle activity. However, it can only show changes after an activity and not in real-time [11]. Ultrasonography is another option that can provide quantitative changes in muscle cross-sectional areas during real-time activity. However, Moodie et al. [10] reported that the validity of ultrasonography during intensive contraction is questionable and concluded that EMG is a reliable measure of muscle activity over a wide range of contraction intensities. Therefore, surface EMG is preferred for analysing muscle activity during voluntary motion [35,36,37,38,39], and AMI after knee injury or surgery. Kim et al. found decreased quadriceps neuromuscular activity in patients who underwent anterior cruciate ligament (ACL) reconstruction compared to healthy individuals [40]. McPherson et al. reported decreased thigh muscle activation and altered muscle stiffness using elastography 12 months after an ACL injury [41]. The common finding in previous studies is that the quadriceps muscles are inhibited, whereas the hamstring muscles show excitability [2]. In this study, the differences between muscle groups during sMVIC were assessed, revealing that the quadriceps and hamstring muscles of the injured leg have different activation patterns, which is consistent with the results of previous studies. These results suggest that a combination of strengthening the quadriceps while performing hamstring fatigue exercises is important to resolve hamstring hypercontractility, which can lead to knee extension deficits if left untreated [2, 30].
However, a major difficulty in interpreting the EMG data is the wide dispersion of values between individuals and experimental conditions [42,43,44]. Since performing a true MVIC is often compromised and unreliable in patients due to discomfort or pain [12, 45, 46], patients performed submaximal isometric contraction in the specific position with respect to a previous study. The examination position (submaximal isometric extension in the fully extended knee position and submaximal isometric flexion in the 20° flexion knee position) was feasible and repeatable in all patients who participated in the present study [9]. Another difficulty in the interpretation of EMG lies in the various normalisation methods. In this study, the EMG during sMVIC was normalised using the dynamic mean method, referenced by the EMG activity during the five strides of the uninjured leg [12]. Among the common EMG normalisation techniques, such as MVIC, dynamic peak EMG activity, or dynamic mean EMG activity, a level recorded during a task, such as walking, is preferred, as it has been reported to reduce intersubject variability [21,22,23,24]. This normalisation method showed that the activation of extensor and flexor muscles exhibited distinct behaviours. Additionally, the EMG activity of the injured leg during sMVIC, normalised to the EMG amplitude of the uninjured side, showed that the extensor muscle groups were inhibited, whereas the flexor muscle groups were excited. The two normalisation methods used in this study yielded similar results. Nevertheless, the interpretation of functional differences in EMG requires caution when comparing different populations.
The insightful AMI classification proposed by Sonnery-Cottet et al. appears easy and feasible, suggesting that it was designed with profound consideration and extensive clinical experience [9]. The intraclass correlation coefficient of the classification also showed good reliability [4]. The present study investigated the electrical muscle activity in the examined position in the classification and found that the AMI pattern was detectable, which showed distinct patterns among muscle groups. This study supports the basic concept of AMI classification based on VM contraction and extension deficits. However, this classification system has several limitations. A major concern is that subcategories a and b are determined by the outcome of physiotherapy, which can vary significantly depending on the practitioner's treatment quality and duration. In addition, classifying patients based on therapeutic outcomes is time-consuming. Furthermore, a person performing physical therapy also acts as an examiner, which may introduce bias. Therefore, the definition of the subcategories should be revised to assess the status quo before any intervention. This approach enables the classification system to evaluate the effects of treatments more accurately. Given that AMI is complex and multifactorial, further studies analysing the contributing factors, differences among diagnostic groups, and complications would enrich our comprehensive understanding of this condition and improve the validity and versatility of the classification system.
Limitations
This study has several limitations. First, surface EMG has inherent limitations. The soft tissue between the electrode and the target muscle may introduce signal interference. Additionally, ultrasonography was not used to identify the muscle bellies in this study. In general, surface EMG may be influenced by the crosstalk between adjacent muscles and may not accurately capture deep muscle activity. Second, a subgroup analysis was not conducted because only a small number of participants were recruited. For the same reason, risk factor analysis or analysis of the relationship between the AMI classification and EMG findings was not performed. As this was a pilot cross-sectional study, sub-analysis was beyond the scope of the current study. Third, this study was conducted only at specific positions without comparison with other positions. The changes in muscle activity may differ in other positions. Fourth, a comparison with healthy volunteers was not performed. Previous studies have reported bilateral AMI after unilateral knee injuries [29, 44, 47]. Thus, comparison with a healthy control group is considered necessary in future studies. Finally, 13 patients were excluded during the screening due to poor surface EMG data quality, which may have introduced a potential bias.
Conclusions
Arthrogenic muscle inhibition was detectable in the examination position suggested by the Sonnery-Cottet classification. The flexor and extensor muscles of the injured leg exhibited distinct activation behaviours, with inhibition predominantly occurring in the quadriceps muscles, whereas the hamstrings showed excitation.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EMG:
-
Electromyography
- sMVIC:
-
Submaximal voluntary isometric contraction
- CI:
-
Confidence interval
- VM:
-
Vastus medialis
- VL:
-
Vastus lateralis
- ST:
-
Semitendinosus
- BF:
-
Biceps femoris
- RMS:
-
Root mean square
- BMI:
-
Body mass index
- EMG:
-
Electromyography
- ACL:
-
Anterior cruciate ligament
- PCL:
-
Posterior cruciate ligament
- PLC:
-
Posterolateral corner
- MCL:
-
Medial collateral ligament
- LCL:
-
Lateral collateral ligament
- MPFL:
-
Medial patellofemoral ligament
- LM:
-
Lateral meniscus
- MM:
-
Medial meniscus
References
Rice DA, McNair PJ, Lewis GN, Dalbeth N. Quadriceps arthrogenic muscle inhibition: the effects of experimental knee joint effusion on motor cortex excitability. Arthritis Res Ther. 2014;16(6):502. https://doi.org/10.1186/s13075-014-0502-4.
Delaloye JR, Murar J, Sánchez MG, Saithna A, Ouanezar H, Thaunat M, et al. How to rapidly abolish knee extension deficit after injury or surgery: a practice-changing video pearl from the scientific anterior cruciate ligament network international (SANTI) study group. Arthrosc Tech. 2018;7(6):e601–5. https://doi.org/10.1016/j.eats.2018.02.006.
Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40(3):250–66. https://doi.org/10.1016/j.semarthrit.2009.10.001.
Sonnery-Cottet B, Hopper GP, Gousopoulos L, Pioger C, Vieira TD, Thaunat M, et al. Incidence of and risk factors for arthrogenic muscle inhibition in acute anterior cruciate ligament injuries: a cross-sectional study and analysis of associated factors from the SANTI Study Group. Am J Sports Med. 2024;52(1):60–8. https://doi.org/10.1177/03635465231209987.
Palmieri-Smith RM, Kreinbrink J, Ashton-Miller JA, Wojtys EM. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med. 2007;35(8):1269–75. https://doi.org/10.1177/0363546506296417.
Reeves ND, Maffulli N. A case highlighting the influence of knee joint effusion on muscle inhibition and size. Nat Clin Pract Rheumatol. 2008;4(3):153–8. https://doi.org/10.1038/ncprheum0709.
Thomas AC, Wojtys EM, Brandon C, Palmieri-Smith RM. Muscle atrophy contributes to quadriceps weakness after anterior cruciate ligament reconstruction. J Sci Med Sport. 2016;19(1):7–11. https://doi.org/10.1016/j.jsams.2014.12.009.
Lim SH, Hong BY, Oh JH, Lee JI. Effects of joint effusion on quadriceps muscles in patients with knee osteoarthritis. Phys Ther Sport. 2016;17:14–8. https://doi.org/10.1016/j.ptsp.2015.09.001.
Sonnery-Cottet B, Hopper GP, Gousopoulos L, Vieira TD, Thaunat M, Fayard J-M, et al. Arthrogenic muscle inhibition following knee injury or surgery: pathophysiology, classification, and treatment. Video J Sports Med. 2022;2(3):26350254221086296. https://doi.org/10.1177/26350254221086295.
Moodie KF, O’Leary SP, Tucker KJ, McPhail SM, Peolsson A. The relationship of ultrasound measurements of muscle deformation with torque and electromyography during isometric contractions of the cervical extensor muscles. J Manip Physiol Ther. 2020;43(4):284–93. https://doi.org/10.1016/j.jmpt.2018.11.033.
Cagnie B, Elliott JM, O’Leary S, D’Hooge R, Dickx N, Danneels LA. Muscle functional MRI as an imaging tool to evaluate muscle activity. J Orthop Sports Phys Ther. 2011;41(11):896–903. https://doi.org/10.2519/jospt.2011.3586.
Commandeur D, Klimstra M, Brodie R, Hundza S. A comparison of bioelectric and biomechanical EMG normalization techniques in healthy older and young adults during walking gait. J Funct Morphol Kinesiol. 2024;9(2):90. https://doi.org/10.3390/jfmk9020090.
Schilaty ND, McPherson AL, Nagai T, Bates NA. Arthrogenic muscle inhibition manifests in thigh musculature motor unit characteristics after anterior cruciate ligament injury. Eur J Sport Sci. 2023;23(5):840–50. https://doi.org/10.1080/17461391.2022.2056520.
Dos Anjos T, Gabriel F, Vieira TD, Hopper GP, Sonnery-Cottet B. Neuromotor treatment of arthrogenic muscle inhibition after knee injury or surgery. Sports Health. 2024;16(3):383–9. https://doi.org/10.1177/19417381231169285.
Merletti R, Hermens H. Introduction to the special issue on the SENIAM European Concerted Action. J Electromyogr Kinesiol. 2000;10(5):283–6. https://doi.org/10.1016/s1050-6411(00)00019-5.
López-de-Celis C, Sánchez-Alfonso N, Rodríguez-Sanz J, Romaní-Sánchez S, Labata-Lezaun N, Canet-Vintró M, et al. Quadriceps and gluteus medius activity during stable and unstable loading exercises in athletes. A cross-sectional study. J Orthop Res. 2024;42(2):317–25. https://doi.org/10.1002/jor.25680.
Hirose N, Tsuruike M. Differences in the electromyographic activity of the hamstring, gluteus maximus, and erector spinae muscles in a variety of kinetic changes. J Strength Cond Res. 2018;32(12):3357–63. https://doi.org/10.1519/jsc.0000000000002747.
Kim HY, An YS, Oh SH, Lee HC. Clinical feasibility of a markerless gait analysis system. Clin Orthop Surg. 2024;16(3):506–16. https://doi.org/10.4055/cios23065.
Shanbehzadeh S, Mohseni Bandpei MA, Ehsani F. Knee muscle activity during gait in patients with anterior cruciate ligament injury: a systematic review of electromyographic studies. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1432–42. https://doi.org/10.1007/s00167-015-3925-9.
Ruspi A, Temporiti F, Adamo P, Mina F, Traverso F, Gatti R. Neuromuscular activation of quadriceps bellies during tasks performed in the same biomechanical condition in patients undergoing total knee arthroplasty. J Electromyogr Kinesiol. 2022;64: 102659. https://doi.org/10.1016/j.jelekin.2022.102659.
Soderberg GL, Knutson LM. A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther. 2000;80(5):485–98.
Burden AM, Trew M, Baltzopoulos V. Normalisation of gait EMGs: a re-examination. J Electromyogr Kinesiol. 2003;13(6):519–32. https://doi.org/10.1016/s1050-6411(03)00082-8.
Knoll Z, Kiss RM, Kocsis L. Gait adaptation in ACL deficient patients before and after anterior cruciate ligament reconstruction surgery. J Electromyogr Kinesiol. 2004;14(3):287–94. https://doi.org/10.1016/j.jelekin.2003.12.005.
Knoll Z, Kocsis L, Kiss RM. Gait patterns before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):7–14. https://doi.org/10.1007/s00167-003-0440-1.
Gallina A, Merletti R, Gazzoni M. Uneven spatial distribution of surface EMG: What does it mean? Eur J Appl Physiol. 2013;113(4):887–94. https://doi.org/10.1007/s00421-012-2498-2.
Martens J, Daly D, Deschamps K, Staes F, Fernandes RJ. Inter-individual variability and pattern recognition of surface electromyography in front crawl swimming. J Electromyogr Kinesiol. 2016;31:14–21. https://doi.org/10.1016/j.jelekin.2016.08.016.
Sato H, Nishimura Y, Tsuboi H, Minoshima Y, Sakata T, Umezu Y, Tajima F. Differences in fatigability of vastus medialis muscle between patients with limb symmetry index of <90% and ≥90% after chronic anterior cruciate ligament reconstruction. Knee. 2021;31:39–45. https://doi.org/10.1016/j.knee.2021.05.005.
Hansen C, Einarson E, Thomson A, Whiteley R, Witvrouw E. Hamstring and calf muscle activation as a function of bodyweight support during treadmill running in ACL reconstructed athletes. Gait Posture. 2017;58:154–8. https://doi.org/10.1016/j.gaitpost.2017.07.120.
McPherson AL, Schilaty ND, Anderson S, Nagai T, Bates NA. Arthrogenic muscle inhibition after anterior cruciate ligament injury: injured and uninjured limb recovery over time. Front Sports Act Living. 2023;5:1143376. https://doi.org/10.3389/fspor.2023.1143376.
Buckthorpe M, Gokeler A, Herrington L, Hughes M, Grassi A, Wadey R, et al. Optimising the early-stage rehabilitation process post-ACL reconstruction. Sports Med. 2024;54(1):49–72. https://doi.org/10.1007/s40279-023-01934-w.
Perraton L, Clark R, Crossley K, Pua YH, Whitehead T, Morris H, et al. Impaired voluntary quadriceps force control following anterior cruciate ligament reconstruction: relationship with knee function. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1424–31. https://doi.org/10.1007/s00167-015-3937-5.
Zunzarren G, Garet B, Vinciguerra B, Murgier J. Persistence of neuromuscular activation deficit in the lower limb at 3-years of follow-up after ACL reconstruction surgery. Knee. 2023;43:97–105. https://doi.org/10.1016/j.knee.2023.06.006.
Pietrosimone B, Lepley AS, Kuenze C, Harkey MS, Hart JM, Blackburn JT, Norte G. Arthrogenic muscle inhibition following anterior cruciate ligament injury. J Sport Rehabil. 2022;31(6):694–706. https://doi.org/10.1123/jsr.2021-0128.
Sonnery-Cottet B, Saithna A, Quelard B, Daggett M, Borade A, Ouanezar H, et al. Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions. Br J Sports Med. 2019;53(5):289–98. https://doi.org/10.1136/bjsports-2017-098401.
Kwok WY, So BCL, Ng SMS. Underwater surface electromyography for the evaluation of muscle activity during front crawl swimming: a systematic review. J Sports Sci Med. 2023;22(1):1–16. https://doi.org/10.52082/jssm.2023.1.
Matsuura Y, Matsunaga N, Akuzawa H, Kojima T, Oshikawa T, Iizuka S, et al. Difference in muscle synergies of the butterfly technique with and without swimmer’s shoulder. Sci Rep. 2022;12(1):14546. https://doi.org/10.1038/s41598-022-18624-8.
Rocha de Faria JL, Laett CT, Gavilão UF, Carvalho MB, Mozella AP, De Sousa EB, Cossich VRA. Modified Pulvertaft on weave technique restores full active knee extension in patients with large chronic quadriceps tendon rupture: a case series. Arthroscopy. 2022;38(7):2268–77. https://doi.org/10.1016/j.arthro.2022.01.023.
Labanca L, Tedeschi R, Mosca M, Benedetti MG. Individuals with chronic ankle instability show abnormalities in maximal and submaximal isometric strength of the knee extensor and flexor muscles. Am J Sports Med. 2024;52(5):1328–35. https://doi.org/10.1177/03635465241232090.
Schuermans J, Danneels L, Van Tiggelen D, Palmans T, Witvrouw E. Proximal neuromuscular control protects against hamstring injuries in male soccer players: a prospective study with electromyography time-series analysis during maximal sprinting. Am J Sports Med. 2017;45(6):1315–25. https://doi.org/10.1177/0363546516687750.
Kim S, Glaviano NR, Park J. Exercise-induced fatigue affects knee proprioceptive acuity and quadriceps neuromuscular function more in patients with ACL reconstruction or meniscus surgery than in healthy individuals. Knee Surg Sports Traumatol Arthrosc. 2023;31(12):5428–37. https://doi.org/10.1007/s00167-023-07596-5.
McPherson AL, Bates NA, Haider CR, Nagai T, Hewett TE, Schilaty ND. Thigh musculature stiffness during active muscle contraction after anterior cruciate ligament injury. BMC Musculoskelet Disord. 2020;21(1):320. https://doi.org/10.1186/s12891-020-03342-x.
Zheng Y, Zheng G, Zhang H, Zhao B, Sun P. Mapping method of human arm motion based on surface electromyography signals. Sensors. 2024. https://doi.org/10.3390/s24092827.
Jorge A, Lichtenstein E, Faude O, Roth R. Muscle activity and kinematics during three hamstring strengthening exercises compared to sprinting: a cross-sectional study. Int J Sports Phys Ther. 2024;19(5):569–80. https://doi.org/10.26603/001c.116158.
Whitcomb E, Ortiz O, Toner J, Kuruganti U. The bilateral limb deficit (BLD) phenomenon during leg press: a preliminary investigation into central and peripheral factors. BMC Sports Sci Med Rehabil. 2021;13(1):89. https://doi.org/10.1186/s13102-021-00321-0.
Knauer SR, Freburger JK, Carey TS. Chronic low back pain among older adults: a population-based perspective. J Aging Health. 2010;22(8):1213–34. https://doi.org/10.1177/0898264310374111.
Cholewicki J, van Dieën J, Lee AS, Reeves NP. A comparison of a maximum exertion method and a model-based, sub-maximum exertion method for normalizing trunk EMG. J Electromyogr Kinesiol. 2011;21(5):767–73. https://doi.org/10.1016/j.jelekin.2011.05.003.
Dong S, Liu Y, Liu Z, Shen P, Sun H, Zhang P, et al. Can arthrogenic muscle inhibition exist in peroneal muscles among people with chronic ankle instability? A cross-sectional study. Sports Med Open. 2024;10(1):35. https://doi.org/10.1186/s40798-024-00710-y.
Acknowledgements
We would like to thank Han-Cheol Lee for monitoring the equipment in the motion analysis lab at our institute.
Funding
This research was supported by Eulji University in 2023.
Author information
Authors and Affiliations
Contributions
MK and MG contributed equally to this work; Data processing and analysis. JK and JHL contributed to data acquisition. HYK made substantial contributions to the conception and design of the work. HYL has drafted and managed the whole process.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received ethical approval from the Institutional Review Board of the medical centre of current study.
Consent for publication
Written consent was obtained from all participants.
Competing interests
The authors declare that they have no competing interests
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, M., Gu, M., Kim, HY. et al. Assessment of arthrogenic quadriceps muscle inhibition by physical examination in the supine position during isometric contraction is feasible as demonstrated by electromyography: a cross-sectional study. J Orthop Surg Res 19, 458 (2024). https://doi.org/10.1186/s13018-024-04949-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04949-9