Abstract
Background
It is controversial whether pulmonary function testing should be performed routinely in cardiac surgery patients. The aim of our study was to focus on patients who have congestive heart failure, caused by left ventricular dysfunction or left-sided heart valve disease, and study the prognostic value of performing preoperative pulmonary function testing on their postoperative outcomes.
Methods
This is a retrospective propensity score matched study that included 366 patients with congestive heart failure who underwent cardiac surgery and had preoperative pulmonary function test. The patients were divided into two groups: Group 1 who had a normal or mild reduction in pulmonary function tests and group 2 who had moderate to severe reduction in pulmonary function tests. The postoperative outcomes, including pulmonary complications, were compared between the two groups.
Results
Pulmonary function tests were normal or mildly reduced in 190 patients (group 1) and moderately to severely reduced in 176 patients (group 2). Propensity matching identified 111 matched pairs in each group with balanced preoperative and operative characteristics. Compared to group 1, Group 2 had longer duration of mechanical ventilation [12 (7.5–16) vs. 9 (6.5–13) hours, p < 0.001], higher postoperative Creatinine [111 (90–142) vs. 105 (81–128) µmol/dl, p = 0.02] and higher hospital mortality (6.31% vs. 0%, p = 0.02).
Conclusion
Routine Pulmonary Function Testing should be performed in patients with Left ventricular dysfunction and/or congestive heart failure undergoing cardiac surgery since moderate to severe reduction in those patients was associated with longer duration of mechanical ventilation and higher hospital mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Lung dysfunction after cardiac surgery remains an important cause of postoperative morbidity despite continuing improvement in cardiopulmonary bypass techniques and postoperative intensive care management. There is a significant co-existence of cardiac and pulmonary disease. Moreover, most of the patients who are candidates for cardiac surgery have pre-existing pulmonary pathology. The important correlation of lung function and cardiac surgical outcomes is emphasized by the prognostic value of chronic lung disease assessment in the Society of Thoracic Surgeons (STS) and EuroSCORE II operative mortality estimation tools [1]. This led some centres to perform pulmonary function testing (PFT) routinely before any elective cardiac surgery procedure based on the evidence that spirometry evidence of obstructive ventilatory pattern may predict the duration of mechanical ventilation and intensive care unit (ICU) stay following elective cardiac surgery [2]. Additionally, different levels of chronic obstructive pulmonary disease (COPD) severity may impact the prediction of postoperative morbidity and prolonged lengths of ICU and hospital stay in patients undergoing coronary artery bypass grafting (CABG) [3].
However, pulmonary congestion secondary to heart failure or left-sided heart valve disease is known to cause both obstructive and restrictive abnormalities in PFT, which obviously could influence the preoperative spirometry results of cardiac surgical patients. It is debatable whether abnormal PFT results in those patients represent a real risk of postoperative pulmonary complications or they are just a reflection of the left-sided heart congestion. This led some centres to adopt the selective performance of preoperative spirometry at the discretion of the individual physician or departmental standards based on patient history of respiratory symptoms or smoking habits. Some authors did not even include PFT in their proposed model for predicting patients who require prolonged ventilation post cardiac surgery [4], that included parsonnet score, ejection fraction (EF), age, and emergency re-operation for bleeding or cardiac arrest.
Very few studies have looked at the interaction between left-sided heart valve dysfunction or ventricular dysfunction and the results of lung spirometry and suggested that lung function parameters may provide prognostic information in patients with heart failure and may help to guide treatment decisions [5].
Hence, our study aimed to focus on this subgroup of cardiac surgery patients with congestive heart failure caused by left ventricular dysfunction or left-sided heart valve disease and study the prognostic value of performing preoperative PFT on their postoperative outcomes.
Methods
Study design and data collection
The study is a retrospective propensity score matched study that was conducted at a tertiary Cardiac centre. It included adult patients above or equal to 18 years who underwent any cardiac surgery with cardiopulmonary bypass, had congestive heart failure, as defined by European Society of Cardiology (ESC): heart failure with reduced (HFrEF), mildly reduced (HFmrEF) and preserved ejection fraction (HFpEF) (based on transthoracic echocardiography), and had preoperative PFT during the time period from May 2015 to December 2019. Patients who did not have preoperative PFT were excluded from the study. All PFTs were performed in the hospital core lab and was interpreted by two experienced specialists.
Data were collected on patients’ demographics, preoperative PFT parameters, operative data and postoperative data and complications from electronic medical records. Echocardiographic parameters were obtained from the echocardiographic laboratory databases.
The pulmonary functions test results were classified into obstructive or restrictive patterns and then classified in severity according to the American Thoracic Society (ATS) grading system [6, 7]. The patients were divided into two groups: Group 1 who had a normal or mild reduction in PFT and Group 2 who had moderate to severe reduction in PFT. The postoperative outcomes, including pulmonary complications, were compared between the two groups.
The Institutional Review Board approved the data collection of this study, and they waived the need for patients’ consent because of the retrospective nature of the study.
Statistical analysis
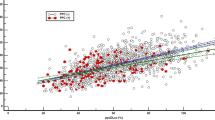
Patients’ characteristics were reported using means and medians for continuous variables and proportions for categorical variables. A p- value of less than 0.05 was considered statistically significant. Propensity score matching was performed using 1:1 nearest neighbour match with a calibre of 0.06 and no replacement for factors. Propensity score distribution was presented in Fig. 1 and the absolute bias difference of 20% of covariates between groups indicated a satisfactory match. Shapiro-Wilk normality test was performed, and non-normally distributed continuous variables were presented as median (Q1-Q3). Continuous variables were compared using Wilcoxon test for the unmatched groups and Wilcoxon matched-pairs signed-rank test for the matched groups. Categorical variables were presented as numbers and percentages and compared with the Chi-square or Fisher exact test for the unmatched groups and Mcnemar or Friedman tests for the matched groups. We reported the P-value and the standardized mean difference for the baseline data pre and post-match. Statistical analysis was performed using Stata 16.1 (Stata Corp- College Station- TX- USA).
Standardized bias across covariates before and after matching. TV: tricuspid valve, MVR: mitral valve replacement, AF: atrial fibrillation, CKD: chronic kidney disease, LVESD: left ventricular end systolic dimension, COPD: chronic obstructive pulmonary disease, MV: mitral valve, AVR: aortic valve replacement, LVEDD: left ventricular end diastolic dimension, DM: diabetes mellitus, BMI: body mass index, TIA: transient ischemic attack, PVD: peripheral vascular disease, CAD: coronary artery disease, CABG: coronary artery bypass grafting
Results
Three hundred and sixty-six patients were included in the study. PFT were normal or mildly reduced in 190 patients (group 1) and moderately to severely reduced in 176 patients (group 2). All patients with pulmonary dysfunction in our study showed a restrictive pattern. Group 1 included more males and more patients who underwent CABG while Group 2 included more patients with preoperative stroke and more patients who underwent combined procedures, mitral valve procedures, tricuspid valve repair and MAZE procedure (Table 1). Propensity matching identified 111 matched pairs in each group with balanced preoperative and operative characteristics (Table 2).
Compared to Group 1, Group 2 had longer duration of mechanical ventilation [12 (7.5–16) vs. 9 (6.5–13) hours, p < 0.001], higher postoperative Creatinine [111 (90–142) vs. 105 (81–128) µmol/dl, p = 0.02] and higher hospital mortality (6.31% vs. 0%, p = 0.02). The rest of post-operative data and complications are illustrated in Table 3.
Discussion
Several studies showed a reduction in forced expiratory volume in the first second (FEV1) and forced vital capacity (FVC) in heart failure patients [8,9,10,11]. Factors responsible for the restrictive pattern are increased lung stiffness, respiratory muscle fatigue, cardiac enlargement and constriction of under perfused alveoli leading to reduced lung compliance in a low cardiac output state. Elsobkey and Gomaa [12] showed that both valvular and ischemic patients had lower than normal PFT results pre-operatively with a predominant restrictive pattern. The authors also noticed that patients with rheumatic heart disease had lower values compared to patients with ischemic heart disease and this was explained by the fact that patients with rheumatic heart disease are more prone to develop pulmonary congestion in which the lung compliance is reduced and the resistance to airflow is increased with resultant decreased gas exchange and pulmonary function. This finding had also been confirmed in patients with mitral valve disease by Saxena et al. [8]. Importantly, restrictive or obstructive lung impairment can be identified that is solely due to cardiac decompensation in the absence of any intrinsic lung disease [13].
The question is whether these reduced spirometry readings in surgical patients represent a real risk for postoperative respiratory complications or it is just a reflection of the heart failure status that would improve postoperatively after fixing the surgical problem. This association between PFT values and postoperative outcomes in this specific group of patients with impaired LV function has not been studied before. In order to answer this problem, we included in this study only coronary patients with left ventricular dysfunction and patients with severe left-sided valvular problems causing congestive heart failure. Despite the small percentage of patients with a history of asthma or COPD in our cohort, we demonstrated that the group of patients with moderate to severe impairment of pulmonary function test has a significantly longer duration of intubation and higher hospital mortality. Of note, even patient with history obstructive lung disease demonstrated predominantly a restrictive pattern indicating the predominance of heart failure symptoms and cardiac decompensation on presentation.
Our findings go in line with other studies that support the routine use of PFT in cardiac surgery patients. In a prospective cohort study [14], Risom EC and colleagues showed that performing spirometry on all comers for cardiac surgery irrespective of smoking or COPD history, preoperative spirometry reclassified 18% of the patients. A reduced FEV1 independently doubled the risk of death. They concluded that the inclusion of preoperative spirometry in routine screening of cardiac surgical patients may improve risk prediction and identify high-risk patients. Alam et al. [15]. observed that predicted FVC% and predicted FEV1% were most strongly associated with poor postoperative outcomes including postoperative respiratory failure, atelectasis and pulmonary infection but not with postoperative mortality.
On the other hand, a small study by Spivak et al. [16]. and another one by Bando et al. [17], found that PFT should not be used as exclusion criteria for CABG and that postoperative cardiac function and occurrence of complications are more significant than preoperative PFT in determining the duration of ventilation after cardiac surgery and that routine spirometry is unnecessary for most adult cardiac patients. In our study, all patients had congestive heart failure and hence were expected to have similar outcomes. However, PFT results helped to differentiate those who had longer duration of mechanical ventilation and higher hospital mortality. Manganas et al. [18] found that patients with severe COPD can undergo CABG without increased mortality risk when compared with patients with normal PFT or with mild to moderate COPD. However, they have an increased risk of pulmonary infections, a tendency towards atrial fibrillation and slightly increased length of hospital stay. Whether to add PFT and different classifications of COPD to the STS risk model for predicting outcomes after cardiothoracic surgery was studied by Ivanov et al. [19] and it came with only little utility.
Clinical implications
Our findings in this study support the rationale of routine performance of PFT in all patients with congestive heart failure undergoing cardiac surgery regardless of their history of respiratory disease symptoms. Although this may not necessarily exclude those patients from candidacy for cardiac surgery but rather help planning for proper timing of surgery for such patients for better resource utilization. Additionally, it could identify those patients who might require preoperative medical optimization.
Limitations
This is a retrospective study with all possible biases that it could introduce. However, we performed propensity matching analysis to control for the differences in preoperative characteristics. Additionally, the study is limited by the single-center design, which should be considered before the generalization of the results.
Conclusion
Routine Pulmonary Function Testing should be performed in patients with Left ventricular dysfunction and/or congestive heart failure undergoing cardiac surgery since moderate to severe reduction in those patients was associated with longer duration of mechanical ventilation and higher hospital mortality. Routine utilization of PFT in those patients may be justified for risk stratification, planning of proper timing of surgery and preoperative medical optimization.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the institutional patients’ confidentiality policy but are available from the corresponding author on reasonable request.
References
Reddi BA, Johnston SD, Bart S, Chan JC, Finnis M. Abnormal pulmonary function tests are associated with prolonged ventilation and risk of complications following elective cardiac surgery. Anaesth Intensive Care. 2019;47(6):510–5. https://doi.org/10.1177/0310057X19877188.
Ried M, Unger P, Puehler T, Haneya A, Schmid C, Diez C. Mild-to-moderate COPD as a risk factor for increased 30-day mortality in cardiac surgery. Thorac Cardiovasc Surg. 2010;58(7):387–91. https://doi.org/10.1055/s-0030-1249830.
Najafi M, Sheikhvatan M, Mortazavi SH. Do preoperative pulmonary function indices predict morbidity after coronary artery bypass surgery? Ann Card Anaesth. 2015 Jul-Sep;18(3):293–8. https://doi.org/10.4103/0971-9784.159796.
Dunning J, Au J, Kalkat M, Levine A. A validated rule for predicting patients who require prolonged ventilation post cardiac surgery. Eur J Cardiothorac Surg. 2003;24(2):270–6. https://doi.org/10.1016/s1010-7940(03)00269-0.
Magnussen H, Canepa M, Zambito PE, Brusasco V, Meinertz T, Rosenkranz S. What can we learn from pulmonary function testing in heart failure? Eur J Heart Fail. 2017;19(10):1222–9. https://doi.org/10.1002/ejhf.946.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–68. https://doi.org/10.1183/09031936.05.00035205.
American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med. 1995;152(3):1107–36. https://doi.org/10.1164/ajrccm.152.3.7663792.
Saxena P, Luthra S, Dhaliwal RS, Rana SS, Behera D. Early changes in pulmonary functions after mitral valve replacement. Ann Thorac Med. 2007;2(3):111–7. https://doi.org/10.4103/1817-1737.33699.
Kee K, Naughton MT. Heart failure and the lung. Circ J. 2010;74(12):2507–16. https://doi.org/10.1253/circj.cj-10-0869.
Agostoni P, Bussotti M, Cattadori G, Margutti E, Contini M, Muratori M, Marenzi G, Fiorentini C. Gas diffusion and alveolar-capillary unit in chronic heart failure. Eur Heart J. 2006;27(21):2538–43. https://doi.org/10.1093/eurheartj/ehl302.
Magee MJ, Herbert MA, Roper KL, Holper E, Dewey TM, Snelus T, Mack MJ. Pulmonary function tests overestimate chronic pulmonary disease in patients with severe aortic stenosis. Ann Thorac Surg. 2013;96(4):1329–35. https://doi.org/10.1016/j.athoracsur.2013.04.123.
El-Sobkey SB, Gomaa M. Assessment of pulmonary function tests in cardiac patients. J Saudi Heart Assoc. 2011;23(2):81–6. https://doi.org/10.1016/j.jsha.2011.01.003.
Contini M, Conte E, Agostoni P. Lung function evaluation in heart failure: possible pitfalls. Breathe (Sheff). 2020;16(1):190316. https://doi.org/10.1183/20734735.0316-2019.
Risom EC, Buggeskov KB, Mogensen UB, Sundskard M, Mortensen J, Ravn HB. Preoperative pulmonary function in all comers for cardiac surgery predicts mortality†. Interact Cardiovasc Thorac Surg. 2019;29(2):244–51. https://doi.org/10.1093/icvts/ivz049.
Alam M, Shehzad MI, Hussain S, Paras I, Kanwal M, Mushtaq A. Spirometry Assessment and correlation with postoperative pulmonary complications in cardiac surgery patients. Cureus. 2020;12(10):e11105. https://doi.org/10.7759/cureus.11105.
Spivack SD, Shinozaki T, Albertini JJ, Deane R. Preoperative prediction of postoperative respiratory outcome. Coronary artery bypass grafting. Chest. 1996;109(5):1222–30. https://doi.org/10.1378/chest.109.5.1222.
Bando K, Sun K, Binford RS, Sharp TG. Determinants of longer duration of endotracheal intubation after adult cardiac operations. Ann Thorac Surg. 1997;63(4):1026–33. https://doi.org/10.1016/s0003-4975(96)01279-9.
Manganas H, Lacasse Y, Bourgeois S, Perron J, Dagenais F, Maltais F. Postoperative outcome after coronary artery bypass grafting in chronic obstructive pulmonary disease. Can Respir J 2007 Jan-Feb;14(1):19–24. https://doi.org/10.1155/2007/378963
Ivanov A, Yossef J, Tailon J, Worku BM, Gulkarov I, Tortolani AJ, Sacchi TJ, Briggs WM, Brener SJ, Weingarten JA, Heitner JF. Do pulmonary function tests improve risk stratification before cardiothoracic surgery? J Thorac Cardiovasc Surg. 2016;151(4):1183–e93. https://doi.org/10.1016/j.jtcvs.2015.10.102.
Acknowledgements
We acknowlege the conclusion is similar to what we wanted to conclude.
Funding
This study was funded by the College of Medicine Research Centre, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
TBA contributed to study design and inception, data review, results review and writing the manuscript. AMA contributed to clinical data collectionAAA contributed to statistical analysis and reporting the results KDA contributed to study design and inception, data review and results reviewAE contributed to study design and inception, data review and results reviewHA contributed to study design and inception, data review and results reviewFA contributed to clinical data collectionBB contributed to study design and inception, data review and results reviewThe manuscript was reviewed and approved by all the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by King Saud University Medical City Institutional Review Board (No. E-16-2008) and was conducted in accordance with Good Clinical Practice. Written informed consent was waived by the ethics committee.
Ethics and integrity statement
This study was funded by the College of Medicine Research Centre, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia. There has been no duplicate publication or submission of this manuscript elsewhere. All authors have read and approved the manuscript. Subject to acceptance, authors will transfer copyright to the Publisher. There is no ethical problem or conflict of interest to be declared for any of the co-authors. The Institutional Review Board approved the data collection of this study, and they waived the need for patients’ consent because of the retrospective nature of the study.
Consent for publication
Non-applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Albacker, T.B., Alhothali, A.M., Arafat, A.A. et al. Should routine pulmonary function tests be performed in patients with left ventricular dysfunction and/or congestive heart failure undergoing cardiac surgery?. J Cardiothorac Surg 19, 499 (2024). https://doi.org/10.1186/s13019-024-02978-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02978-3