Abstract
Background
Mycoplasma pneumoniae pneumonia (MPP) is responsible for 20 to 40% of all cases of pneumonia acquired by children and shows an increasing incidence year by year. The aim of this study was to investigate the expression of miR-34a in children with MPP and its diagnostic value, and further explore the relationship between miR-34a and the rehabilitation effect of children with MPP.
Methods
The expression level of miR-34a was detected by RT-qPCR, and the clinical value of miR-34a was analyzed by ROC analysis. In addition, the levels of IL-6, IL-18 and TNF-α in serum of children with MPP were detected by ELISA kit, and the correlation with miR-34a was analyzed.
Results
Elevated levels of miR-34a were observed in the serum of children with MPP, and significantly higher expression levels were observed in children with severe symptoms and poor rehabilitation. The study suggested that miR-34a has potential as a diagnostic marker for MPP in children, helping to distinguish between mild and severe cases and predicting rehabilitation from MPP in children. In addition, miR-34a expression was positively correlated with IL-6, IL-8, and TNF-α levels.
Conclusions
miR-34a is closely related to MPP in children and miR-34a may be used as a clinical biomarker for MPP in children.
Similar content being viewed by others
Introduction
Mycoplasma pneumoniae pneumonia (MPP), a prevalent respiratory illness among children, is responsible for 20 to 40% of all cases of pneumonia acquired by children and shows an increasing incidence year by year [1]. The incidence of Mycoplasma pneumoniae (M. pneumoniae) infection among children has seen an early surge in various areas of China since June 2023. Notably, a sharp rise in the number of M. pneumoniae infection cases was observed in September, accompanied by more severe clinical presentations [2]. Children infected with M. pneumoniae may present with a range of clinical symptoms, which include a persistent cough, an elevated body temperature, a scratchy throat, a husky voice, a tension headache, muscle aches, shivering, and a sense of widespread unease [3]. Despite advancements in unraveling the underlying causes and the physiological mechanisms of pneumonia, the infection remains a significant contributor to both illness and death. Consequently, there is a pressing need for better diagnostic instruments [4].
MicroRNAs (miRNAs) serve as potent regulatory elements within the genome, demonstrated by their capacity to orchestrate complex cellular processes by engaging with a diverse array of gene targets [5]. miRNAs are instrumental in both the detection and prediction of cancer [6], functioning as biomarkers for an assortment of illnesses [7, 8]. Within the scope of lung diseases, miRNAs have emerged as crucial controllers of immune and inflammatory reactions [9]. Previously, numerous investigations have documented the involvement of miRNAs in cases of M. pneumoniae [10], Coronavirus disease 2019 (COVID-19) [11], and pulmonary fibrosis [12].
In recent times, the utility of miR-34a in various diseases has been the subject of numerous investigations, such as miR-34a plays an important role by regulating the tumor immune microenvironment [13]. miR-34a is engaged in a variety of processes related to both normal nervous system development and pathological conditions [14]. miR-34a promotes the transformation of renal fibroblasts into myofibroblasts [15]. Additionally, research has revealed that the expression of miR-34a is increased in individuals suffering from pneumonia [16]. However, the clinical use of miR-34a in in children with MPP has not been clarified.
The purpose of this study was to investigate the abnormal expression of miR-34a in children with MPP and its diagnostic value, and further explore the relationship between miR-34a and the rehabilitation effect of children with MPP.
Methods and materials
Research object
A sample of 120 children with MMP, ranging in age from 3 to 12 years, was chosen for this study from June 2021 to December 2023 in Affiliated Haimen Hospital of Xinglin College, Nantong University, with 65 boys and 55 girls, and the mean age of the children was 7.27 ± 2.38. Patients were categorized into a severe group (n = 65) if they exhibited the following criteria: (1) Detection of positive serum MP-IgM antibodies, persistently high fever lasting over 7 days, and severe cough with shortness of breath, wheezing, chest pain, decreased oxygen saturation, blood in sputum or haemoptysis or the presence of pulmonary or extrapulmonary complications. (2) Those displaying a systemic inflammatory response accompanied by large patchy shadows occupying one or more lung lobes on imaging examination. All other children were classified as having a mild condition (n = 55). Simultaneously, a control group consisting of 50 healthy children was recruited. This group comprised 27 boys and 23 girls, with an average age of 7.26 ± 2.36, spanning the age range of 3 to 12 years. The distribution of genders and the age distribution between the two groups were nearly identical (p > 0.05). The study protocol was meticulously reviewed and approved by the Institutional Review Board of Affiliated Haimen Hospital of Xinglin College, Nantong University. Prior to enrollment, informed consent was obtained from the parents or legal guardians of the participating children.
Fasting venous blood was collected after hospitalization. The samples were allowed to clot spontaneously at room temperature for a duration of 30 min. Subsequently, the samples underwent centrifugation at a speed of 3,000 rpm for a 10-minute interval to separate the serum. The detection of clinical indicators was completed in the clinical laboratory of Affiliated Haimen Hospital of Xinglin College, Nantong University, presented in Tables 1 and 2.
Inclusion and exclusion criteria
Inclusion criteria: (1) Participants diagnosed with MPP [17] and exhibiting a serum MP antibody titer of ≥ 1:160. (2) Patients who were undergoing standard therapy and demonstrated satisfactory adherence to treatment. (3) Individuals whose clinical records were comprehensive.
Exclusion criteria: (1) Subjects with congenital heart defects, underdeveloped lungs, or immunodeficiency. (2) Participants suffering from recurring upper respiratory tract infections, tracheomalacia, tuberculosis, bronchial asthma, or other related pulmonary conditions. (3) Those displaying severe liver or renal impairment or the presence of malignancies. (4) Subjects who have recently used immunosuppressive or anticoagulant medications within the past three months. (5) Participants with abnormal cognitive development or significant injuries. (6) Those with additional acute or chronic infections from pathogens.
Follow-up
The children were monitored for a duration of 6 months via telephonic conversations, home visits, or scheduled clinic appointments. Detailed documentation of their health status was maintained throughout this period. Subsequently, these children were categorized into two groups: good rehabilitation group and poor rehabilitation group. The classification was based on the resolution of symptoms and the results of chest X-ray assessments. In the category of good rehabilitation group, the children experienced a significant reduction or complete disappearance of clinical symptoms and signs. Body temperature was normal, cough and asthma symptoms were significantly relieved. Their imaging examination returned to normal or showed substantial improvement with most focus areas resolved, and their serological markers normalized. Conversely, the poor rehabilitation group exhibited only minor improvements in symptoms or showed signs of worsening, whose cough and pulmonary symptoms have worsened, whose lung lesions are absorbing, no significant improvement in lung function or worsening on chest X-ray, or children needs to be transferred to a higher level of care.
RT-qPCR
According to the instructions, Trizol reagent (Invitrogen, USA) was used to extract total RNA from serum. The quantity of the extracted RNA was determined using a NanoDrop 1000 spectrophotometer based on UV-visible light absorption (Chenlian Biotechnology, China). Reverse transcription PCR was performed by the TaqMan MicroRNA Reverse Transcription kit (Biosystems, USA). RT-qPCR was performed using SYBR® Green (Promega, USA). The sequences of the primers utilized in the current study are as follows:
U6 forward: 5’-GCTTCGGCAGCACATATACTAAAAT-3’.
U6 reverse: 5’-CGCTTCACGAATTTGCGTGTCAT-3’.
miR-34a forward: 5’-ACACTCCAGCTGGGTGGCAGTGTCTTAGCTGGT-3’.
miR-34a reverse: 5’-CTCAACTGGTGTCGTGGA-3’.
ELISA
The levels of interleukin-6 (IL-6), interleukin-18 (IL-18), and tumor necrosis factor-alpha (TNF-α) in the serum were determined by enzyme-linked immunosorbent assay (ELISA) kits (Nanjing Jiancheng Bioengineering Institute, China), following the producer’s protocol. In summary, the wells for the blank, standards, and samples were set up. Following a series of washing steps, 100 µl of enzyme-labeled secondary antibody was added to each well and allowed to incubate at a temperature of 37 ℃ for a duration of 60 min. Subsequently, another round of washing was conducted, after which a chromogenic agent was added to each well. The mixture was incubated at room temperature for an additional 20 min, concluded by the addition of a termination solution. The absorbance reading at 450 nm for each well was determined.
Statistical analyses
Values are presented as the mean ± standard deviation (SD) and analyzed via an independent t-test, one-way ANOVA. Statistical analyses were conducted using GraphPad Prism version 9.0 and SPSS 26.0. ROC curve was used to evaluate the diagnostic potential of miR-34a in children with MPP and the predictive value of rehabilitation. Chi-square test was used to analyze the correlation between miR-34a and clinical indicators. Logistic regression analysis was used to evaluate the risk factors of poor rehabilitation in MPP children. A p-value of less than 0.05 was deemed statistically significant.
Result
The baseline characteristics manifestation
There was no significant difference in age, gender, and lymphocyte level between the control group, mild MPP group and severe MPP group. Compared with the control group, the WBC level of the mild group was increased, there was also a significant difference between the mild and severe groups. At the same time, the levels of neutrophils, C-reactive protein (CRP), lactate dehydrogenase (LDH), procalcitonin (PCT), D-dimer (D-D) and erythrocyte sedimentation rate (ESR) were increased successively in control group, mild group, and severe group. In addition, there were differences in the use of glucocorticoid drugs and the combination of penicillin antibiotics, as well as length of hospitalization between mild and severe MPP children (Table 1). The levels of WBC, neutrophils, CRP, LDH, PCT, D-D and ESR were increased in the poor rehabilitation group compared with the good rehabilitation group (Table 2).
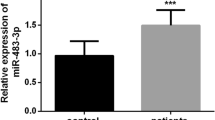
Differentially miR-34a expressed in MPP children
The serum levels of miR-34a were significantly increased in children suffering from MPP, with levels being highest in the severe MPP group compared to the mild MPP group (Fig. 1A and B). Furthermore, a higher level of miR-34a was observed in the poor rehabilitation in contrast to the good rehabilitation children (Fig. 2).
Differential expression of miR-34a in children with MPP. (A) The Expression of miR-34a in control group (n = 50), mild group (n = 55), and severely group (n = 65). (B) The Expression of miR-34a in patients with good (n = 84) and poor (n = 36) rehabilitation. ***p<0.001 vs. Control or Good rehabilitation; ###p<0.001 vs. Mild group
Diagnostic value of miR-34a
The Receiver Operating Characteristic (ROC) analysis revealed that the AUC for miR-34a in identifying MPP in children was 0.873, with a sensitivity of 77.5% and a specificity of 86.0% (Fig. 2A). Furthermore, miR-34a was capable of differentiating between children experiencing mild MPP versus severe MPP, yielding an area under the curve (AUC) of 0.788, a sensitivity of 72.3%, and a specificity of 80.0% (Fig. 2B). Additionally, miR-34a exhibited potential in forecasting the rehabilitative status of children with MPP, achieving an AUC of 0.821, a sensitivity of 75.0%, and a specificity of 80.9% (Fig. 2C).
Risk factors for poor rehabilitation in children with MPP
The patients were divided into two groups based on the mean value of each indicator in the patients with poor rehabilitation, respectively. Chi-square test was used to analyze the correlation between the expression of miR-34a and clinical indicators of children with poor rehabilitation, and the results showed that the expression of miR-34a was significantly correlated with the levels of CRP, LDH, PCT, D-D and ESR of patients (Table 3). Then, miR-34a and factors significantly correlated with miR-34a were included in logistic regression analysis, and the results showed that miR-34a and LDH were risk factors for poor rehabilitation effect in MPP children (Table 4).
Levels of IL-6, IL-18 and TNF-α
The MPP children exhibited a heightened serum IL-6 level when contrasted with the control group. Moreover, the severe group demonstrated a marked increase in IL-6 levels compared with the mild group (Fig. 3A). This trend was also observed for the serum levels of IL-18 and TNF-α (Fig. 3B and C). Additionally, the serum concentrations of IL-6, IL-18, and TNF-α were substantially elevated in children with poor rehabilitation compared to those with good rehabilitation (Fig. 3D and F).
Levels of IL-6, IL-8 and TNF-α. (A-C) The levels of IL-6, IL-8 and TNF-α in control group (n = 50), mild group (n = 55), and severely group (n = 65). (D-F) The levels of IL-6, IL-8 and TNF-α in patients with good (n = 84) and poor (n = 36) rehabilitation. ***p<0.001 vs. Control or Good rehabilitation; ###p<0.001 vs. Mild group
Correlation between miR-34a and IL-6, IL-18 and TNF-α
The relationship between miR-34a and IL-6, IL-18, and TNF-α in serum of patients with severe MPP was investigated using Pearson correlation analysis. The findings revealed a positive association between the expression of miR-34a and the serum levels of IL-6 (Fig. 4A), as well as the levels of IL-18 and TNF-α (Fig. 4B and C).
Discussion
MPP infection may result in cardiovascular or renal inflammation, posing a significant risk to the well-being and survival of pediatric patients. Delayed intervention can lead to organ damage and potentially fatal outcomes [18]. Alterations in the expression levels of microRNAs are intricately linked to the onset of MPP, such as the expression levels of miR-29c and miR-146a may serve as diagnostic biomarkers for identifying MPP [19]. The upregulated expression of miR-222-3p modulates the inflammatory response in monocytes, which contributes to the pathogenesis of MPP in children [20]. Reduced expression of miR-1323 is observed in MPP, which in turn upregulates IL-6 expression and promotes the inflammatory response [21].
In this study, miR-34a was upregulated in children with MPP, and was higher expressed in children with severe MPP and children with poor rehabilitation, this also confirmed previous research(15). Another novel finding we have demonstrated was that miR-34a may predict the occurrence of MPP and distinguish between mild and severe MPP children, and that miR-34a may predict the rehabilitative effect of children with MPP. This provided a new clinical application value for miR-34a. The levels of WBC, neutrophils, CRP, LDH, PCT, D-D and ESR were increased in children with MPP, the findings indicated the potential presence of substantial injury and intense inflammation in children with MPP. Additionally, MP-IgM served as a sensitive biomarker for M. pneumoniae infection in pediatric patient [22]. MP-IgM appears after MP infection and antibody titres increase with disease progression [23] Therefore, MP-IgM positivity was used as one of the indicators for children with severe MPP. This study also analyzed that the expression of miR-34a was significantly correlated with the clinical indicators of MPP children and was a risk factor for poor rehabilitation in MPP children, indicating that miR-34a was closely related to the onset of MPP in children. Therefore, clarifying the expression of miR-34a in children with MPP and exploring its clinical role in children with MPP may be of great significance for the treatment of MPP in children. This provided additional evidence for the use of miRNAs in the clinical management of children with MPP as well as representing a significant advance in clinical application.
The study found that IL-6 levels are elevated in children with MPP and can be a predictor of MPP [24]. Another study also reported that IL-6 and TNF-α are significantly elevated in lobular pneumonia induced by Mycoplasma pneumoniae in children and may play an important role in the pathogenesis of MPP [25]. The levels of IL-18 expression were notably elevated in children suffering from pneumonia [26]. Concentrations of IL-18 in serum were significantly higher in individuals diagnosed with tuberculosis, extra-pulmonary tuberculosis, pneumonia, and lung cancer, in comparison to the control group [27]. In addition, it has been found that miR-34a overexpression can promote the activity of TNF-α, IL-6 and IL-18 in neonates with lung injury [28].
To investigate the correlation between miR-34a and the cytokines IL-6, IL-18, and TNF-α in children with MPP, we measured the expression levels of IL-6, IL-18, and TNF-α in the serum of children suffering from MPP. It indicated that the serum concentrations of these cytokines were elevated in MPP patients, with higher levels observed in those exhibiting a poor rehabilitation. Additionally, miR-34a expression was found to be positively associated with the serum levels of IL-6, IL-18, and TNF-α, aligning with previous research findings [28]. The data suggested that the onset of MPP triggers a systemic inflammatory response, with the expression level of miR-34a being closely linked to the inflammatory status. It is plausible that miR-34a plays a role in the pathogenesis of MPP in children by interacting with inflammatory mediators.
In the current investigation, our focus was limited to the clinical investigation of miR-34a. It is the abnormally high expression of miR-34a in children with MPP that makes miR-34a a possible clinical marker to be applied in the treatment of patients, and the potential alleviation of disease progression by inhibiting miR-34a. Of course this may require further clinical trials to confirm. Based on this study, miR-34a may be used in conjunction with conventional treatments. However, the sample size included in this study was not large enough, and more experimental data may be needed at a later stage to prove these conclusions. In addition, this study did not delve into the complex mechanisms that influence MPP in children. Moving forward, we plan to concentrate our efforts on cellular experiments to investigate the downstream pathways mediated by miR-34a and to elucidate the mechanism of affecting MPP in children.
Conclusion
Elevated levels of miR-34a have been observed in the serum of children suffering from MPP, with significantly higher expression levels observed in those experiencing severe symptoms and those who exhibit a poor rehabilitation. The study suggested that miR-34a has the potential to serve as a diagnostic marker for MPP in children, aiding in the differentiation between mild and severe cases, as well as in forecasting the rehabilitation of the disease in children. Therefore, miR-34a may be used as a clinical biomarker for MPP in children.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Zhu Y, Luo Y, Li L, Jiang X, Du Y, Wang J, et al. Immune response plays a role in Mycoplasma pneumoniae pneumonia. Front Immunol. 2023;14:1189647.
Yan C, Xue GH, Zhao HQ, Feng YL, Cui JH, Yuan J. Current status of Mycoplasma pneumoniae infection in China. World J Pediatrics: WJP. 2024;20(1):1–4.
Kumar S. Mycoplasma pneumoniae: a significant but underrated pathogen in paediatric community-acquired lower respiratory tract infections. Indian J Med Res. 2018;147(1):23–31.
Mandell LA. Community-acquired pneumonia: an overview. Postgrad Med. 2015;127(6):607–15.
Diener C, Keller A, Meese E. Emerging concepts of miRNA therapeutics: from cells to clinic. Trends Genet. 2022;38(6):613–26.
Jay C, Nemunaitis J, Chen P, Fulgham P, Tong AW. miRNA profiling for diagnosis and prognosis of human cancer. DNA Cell Biol. 2007;26(5):293–300.
Tryphena KP, Singh G, Jain N, Famta P, Srivastava S, Singh SB, et al. Integration of miRNA’s theranostic potential with nanotechnology: promises and challenges for Parkinson’s disease therapeutics. Mech Ageing Dev. 2023;211:111800.
Huang CW, Tsai KN, Chen YS, Chang RY. Differential miRNA expression profiling reveals correlation of miR125b-5p with persistent infection of Japanese Encephalitis Virus. Int J Mol Sci. 2021;22(8).
Foster PS, Plank M, Collison A, Tay HL, Kaiko GE, Li J, et al. The emerging role of microRNAs in regulating immune and inflammatory responses in the lung. Immunol Rev. 2013;253(1):198–215.
Jia Z, Sun Q, Zheng Y, Xu J, Wang Y. The immunogenic involvement of miRNA-492 in mycoplasma pneumoniae infection in pediatric patients. Jornal De Pediatria. 2023;99(2):187–92.
Arghiani N, Nissan T, Matin MM. Role of microRNAs in COVID-19 with implications for therapeutics. Volume 144. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie; 2021. p. 112247.
Zhou J, Chen Y, He M, Li X, Wang R. Role of circular RNAs in Pulmonary Fibrosis. Int J Mol Sci. 2022;23(18).
Yin M, Zhang Z, Wang Y. Anti-tumor effects of miR-34a by regulating immune cells in the tumor microenvironment. Cancer Med. 2023;12(10):11602–10.
Chua CEL, Tang BL. miR-34a in Neurophysiology and Neuropathology. J Mol Neuroscience: MN. 2019;67(2):235–46.
Saito S, Ohno SI, Harada Y, Kanno Y, Kuroda M. MiR-34a induces myofibroblast differentiation from renal fibroblasts. Clin Exp Nephrol. 2023;27(5):411–8.
Huang S, Feng C, Zhai YZ, Zhou X, Li B, Wang LL, et al. Identification of miRNA biomarkers of pneumonia using RNA-sequencing and bioinformatics analysis. Experimental Therapeutic Med. 2017;13(4):1235–44.
Søndergaard MJ, Friis MB, Hansen DS, Jørgensen IM. Clinical manifestations in infants and children with Mycoplasma pneumoniae infection. PLoS ONE. 2018;13(4):e0195288.
Lee H, Yun KW, Lee HJ, Choi EH. Antimicrobial therapy of macrolide-resistant Mycoplasma pneumoniae pneumonia in children. Expert Rev anti-infective Therapy. 2018;16(1):23–34.
Wang J, Guo C, Yang L, Sun P, Jing X. Peripheral blood microR-146a and microR-29c expression in children with Mycoplasma pneumoniae pneumonia and its clinical value. Ital J Pediatr. 2023;49(1):119.
Chu C, Lei X, Li Y, Luo Y, Ding Y, Zhou W, et al. High expression of mir-222-3p in children with Mycoplasma pneumoniae pneumonia. Ital J Pediatr. 2019;45(1):163.
Yin L, Ma Y, Wang W, Zhu Y. The critical function of miR-1323/Il6 axis in children with Mycoplasma pneumoniae pneumonia. Jornal De Pediatria. 2021;97(5):552–8.
Ge M, Song Q, Guo Q, Zhou L, Li J, Li Z et al. Diagnostic Value of Serum ELISA of Mycoplasma Pneumoniae IgM and IgG and Passive Particle Agglutination for Mycoplasma Pneumoniae Pneumonia in Children. Clin Lab. 2021;67(1).
Sharma L, Losier A, Tolbert T, Dela Cruz CS, Marion CR. Atypical pneumonia: updates on Legionella, Chlamydophila, and Mycoplasma Pneumonia. Clin Chest Med. 2017;38(1):45–58.
Fan F, Lv J, Yang Q, Jiang F. Clinical characteristics and serum inflammatory markers of community-acquired mycoplasma pneumonia in children. Clin Respir J. 2023;17(7):607–17.
Tian F, Chen LP, Yuan G, Zhang AM, Jiang Y, Li S. Differences of TNF-α, IL-6 and Gal-3 in lobar pneumonia and bronchial pneumonia caused by mycoplasma pneumoniae. Technol Health care: Official J Eur Soc Eng Med. 2020;28(6):711–9.
Yang S, Shi J. Evaluation of serum zinc level and IL-18 mRNA expression in children with pneumonia. Cellular and molecular biology. France). 2021;67(3):168–71. (Noisy-le-Grand.
Akgun M, Saglam L, Kaynar H, Yildirim AK, Mirici A, Gorguner M, et al. Serum IL-18 levels in tuberculosis: comparison with pneumonia, lung cancer and healthy controls. Respirol (Carlton Vic). 2005;10(3):295–9.
Liu H, Liu W, Tang X, Wang T, Sun X, Lv J. IL–6/STAT3/miR–34a protects against neonatal lung injury patients. Mol Med Rep. 2017;16(4):4355–61.
Acknowledgements
Not applicable.
Funding
This study was funded by Special Funds for Scientific Research of Jiangsu Medical Association, grant number: SYH-32034-0111(2024015).
Author information
Authors and Affiliations
Contributions
M. Li and L.J. Lu made substantial contributions to the conception and design, acquisition of data or analysis and interpretation of data. M. Li were involved in drafting the manuscript and H. Xu revising it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was meticulously reviewed and approved by the Institutional Review Board of Affiliated Haimen Hospital of Xinglin College, Nantong University. Prior to enrollment, informed consent was obtained from the parents or legal guardians of the participating children.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, M., Lu, L. & Xu, H. Diagnostic value of miR-34a in Mycoplasma pneumoniae pneumonia in children and its correlation with rehabilitation effect. J Cardiothorac Surg 19, 507 (2024). https://doi.org/10.1186/s13019-024-02992-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02992-5