Abstract
Background
Type A acute aortic dissection (TAAAD) is a deadly condition that demands immediate surgery, because it involves a critically. The mortality and morbidity associated with it are significant, and it is vital that the patient’s conditions and treatment strategies are fully understood to ensure the appropriate management of TAAAD. This study aims to ascertain whether hemiarch repair (HAR) versus extended arch repair (EAR) with or without descending aortic intervention results in better perioperative and late outcomes for patients with TAAAD.
Methods
Four leading centers of cardiac surgery from two European countries have joined forces to create a groundbreaking multicenter observational registry (AoArch). This study was approved by the institutional review board (IRB 202201173). We conducted a retrospective review (NCT 0591263) of our prospectively maintained database for patients who underwent operative repair of DeBakey type I or type II dissection from January 1, 2005 to March 2024 (NCT 05927090). We will analyze how patient co-morbidities, referral conditions, and surgical strategies involving hemi-arch repair (HAR) and extended arch repair (EAR) impact early and late adverse events. We have developed a procedure urgency algorithm based on the severity of preoperative hemodynamic conditions and malperfusion due to TAAAD, and we will use it to assess the primary clinical outcomes: in-hospital mortality, late mortality, and reoperations on the aorta. We will define secondary outcomes as permanent neurologic deficit, the need for new dialysis, respiratory failure, a composite of major adverse events (myocardial infarction, cerebrovascular accidents, the need for dialysis, or the need for tracheostomy), and a composite of major adverse pulmonary events (intubation over 48 h, pneumonia, reintubation, tracheostomy), and reoperation due to bleeding.
Discussion
This multicenter registry will definitively determine the prognostic significance of critical preoperative conditions and the efficacy of extended arch interventions and hemiarch repair in reducing the risk of early adverse events after surgery for TAAAD. This registry will provide insights into the long-term durability of different strategies of surgical repair for TAAAD.
Similar content being viewed by others
Introduction
Type A Acute Aortic Dissection (TAAAD) is a surgical emergency. However, with recent advances in management, TAAAD mortality rates have been significantly reduced for most patients, currently ranging from 15 to 25% [1,2,3,4,5]. To achieve optimal surgical outcomes, it is crucial to balance the risks of surgery during the perioperative period. However, there is still uncertainty regarding the preferable surgical option, whether conservative or more extensive. [6,7,8] TAAAD repair involves removing the primary intimal tear, restoring proper blood flow to the true lumen, and reducing pressure in the false lumen through hemiarch repair under circulatory arrest. Effectively closing off the false lumen (FL) flow can lead to improved late remodeling. [9, 10] Adverse remodeling, which has been linked to a nearly 20% risk of increased mortality at five years, can be caused by distal new entry tears. [11,12,13] Performing extended arch repair (EAR) in TAAAD is increasingly popular due to their ability to promote late remodeling and reduce the risk of distal new entry tears. This is supported by the improving outcomes of EAR procedures [14,15,16,17,18]. However, concerns of equipoise between perioperative safety and more conservative techniques should not limit the common use of advanced techniques to optimize long-term outcomes of TAAAD. [19, 20] Hybrid EAR with a frozen elephant trunk (FET) has become a popular and promising option for patients in need of aortic arch repair. [17, 21, 22] Single-center studies have indicated long-term benefits of this approach without increasing perioperative risks. The evidence supports the use of hybrid EAR as a diverse and effective alternative to traditional arch replacements. [14,15,16,17,18] However, while technology has advanced, there are still concerns regarding the technical complexity, duration of cardiopulmonary bypass (CPB), and circulatory arrest. Furthermore, there is evidence of wide variability in outcomes from center to center, and a recent meta-analysis suggested that EAR approaches may be associated with increased perioperative mortality [13,14,15,16,17,18, 22,23,24]. It is important to acknowledge these issues and work towards finding solutions that benefit all parties involved. Aggressive intervention on the arch may not be performed without a clear understanding of the perioperative risk involved. It is currently unclear whether hemiarch repair with descending aortic access (HAR-DAA) or extended arch repair with descending aortic access (EAR-DAA) offers any advantage over partial or extended arch repair without descending aortic access (HAR/EAR-NDAA) in terms of perioperative risk factors. However, in the absence of randomized data, large multicenter registries are the best way to assess the perioperative safety of aortic arch procedures.
The Multicenter Aortic Arch Registry of Surgery for TAAAD (AoArch) will definitively evaluate the contemporary early outcomes and the durability of different surgical strategies for acute TAAAD at 18 years in a large study population. The registry will compare early outcomes and the durability of patients with TAAAD undergoing EAR versus HAR using either NDAA or DAA access.
Methods
The AoArch is a retrospective analysis of our prospectively maintained database for patients who underwent operative repair of DeBakey type I or type II dissection from January 1, 2005 to March 2024 (STAAD registry NCT 05927090). This database is updated and maintained by clinical information analysts on a regular basis (Table 1).
For this study, we will retrospectively retrieve information on patients who underwent surgical repair for TAAAD during the study timeframe. Our aim is to gather further relevant details for future clinical investigation on this argument. We will use a Microsoft Access datasheet (Redmond, Washington, USA) to collect data on executive patients with TAAAD, with baseline, operative, and outcome variables pre-specified. Prior to commencing the study, we will request permission to conduct the investigation from the relevant institutional or national review boards in accordance with the legislation in force in the country or region in which the study is to be carried out.
For this study, we will retrospectively retrieve information on patients who underwent surgical repair for TAAAD during the study period. Our aim is to gather further relevant details for future clinical investigation on this subject. We will collect data on consecutive patients with TAAAD into a Microsoft Access datasheet (Redmond, Washington, USA) with pre-specified baseline, operative, and outcome variables. We will request permission to conduct this study from institutional or national review boards according to local legislation.
Ethical approval from the Institutional Review Board (IRB) and multicenter data sharing agreements were secured for pooled analysis (IRB No. 202201173; Juliet, 12, 2022; ClinicalTrials.gov ID: NCT05912634 AoArch study). Individual patient consent was waived due to the retrospective nature of the study.
AoArch study patient entry criteria
Characterization of patient populations
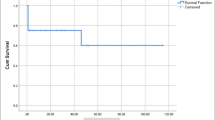
The trial will include patients who underwent surgery for TAAAD, both with circulatory arrest to facilitate either a HAR or EAR repair and without circulatory arrest. The definition of HAR was the replacement of the ascending aorta with an open distal anastomosis under systemic circulatory arrest. The EAR-DAA replacement is a definitive arch repair that can be accomplished through a frozen or conventional elephant trunk in conjunction with endovascular aortic treatment. EAR-NDAA is defined as a repair that is more extensive than HAR but does not involve reinforcing the descending thoracic aorta with a stented segment. The choice of intervention was based on surgeon priority, which varied from center to center. The distribution of patients by surgical repair strategy is shown Fig. 1.
The database contains information on the participation of women and minorities in clinical studies. This is important for scientific, ethical, and social reasons, as well as for the generalizability of study results. AorticArch registry is dedicated to achieving scientific results while ensuring balanced recruitment of patients regardless of gender or ethnicity. The study has recruited at least 30% women and 25% minorities.
Inclusion criteria
-
TAAAD or intramural hematoma involving the ascending aorta;
-
Patients aged > 18 years:
-
Symptoms started within 7 days from surgery;
-
Primary surgical repair of acute TAAAD;
-
Any other major cardiac surgical procedure concomitant with surgery for TAAAD.
Exclusion criteria
-
Patients aged < 18 years;
-
Initiation of symptoms > 7 days from surgery;
-
Former procedure for TAAAD;
-
Coinciding endocarditis;
-
TAAAD secondary to blunt or penetrating chest trauma.
Trial design and endpoints
The trial design schematic is reported in Fig. 1.
Primary
The primary end point will be operative mortality (OM) defined as 30-day and in-hospital mortality, late mortality and reoperation.
Secondary
The trial will evaluate several secondary endpoints. This endpoint provides essential clinical information to the primary physiological endpoint, allowing us to assess the overall benefit of treatment. The following secondary endpoints have been defined for the trial.
-
Functional Status and Neurocognition.
-
NYHA Classification.
-
Myocardial infarction (fourth universal definition).
-
Respiratory failure.
-
Need for new dialysis.
-
Spinal cord injury (SCI; paraplegia, paraparesis).
-
Neurocognitive results.
-
Permanent neurologic deficit (PND; stroke).
-
Transient neurologic deficit (transient ischemic attack, confusion, delirium, agitation).
-
-
Composite of Major Adverse Events (MAE; OM, myocardial infarction, cerebrovascular accidents, need for dialysis, or need for tracheostomy).
-
Composite of Major Adverse Pulmonary Events (MAPE; intubation > 48 h, pneumonia, reintubation, tracheostomy).
-
Safety
-
Incidence of serious adverse events.
-
-
Peri-operative Measures
-
The operative time for each procedure of TAAAD, CPB, and cross-clamp time must be recorded.
-
Blood loss and transfusion.
-
-
Quality of Life and Economic Measures
-
Change in quality of life (QOL).
-
Minnesota Living with Heart Failure (MLHF) score.
-
SF-12.
-
EuroQoL.
-
Dasi.
-
Definition of the clinical and operative variables and their criteria
Suggested course of treatment for TAAAD
We propose that the treatment plan for TAAAD be divided into three categories based on the initial surgical considerations in TAAAD. These categories take into account increasing severity of hemodynamic instability, cerebral malperfusion and the intrinsic characteristics of the aortic dissection based on the TEM Classification [25,26,27,28,29,30] Table 2.
It is important to be aware of the potential complications associated with TAAAD including myocardial infarction, acute aortic regurgitation, cardiac tamponade, aortic rupture, and end-organ malperfusion. These complications can have a significant impact on morbidity and mortality. Given the potential for such events to be acutely life-threatening, it is advisable to consider immediate surgical intervention to reverse any ongoing physiological compromise and mitigate the risk of fatal outcomes. It is estimated that the mortality rate of unoperated acute type A aortic dissection is 1% per hour [31]. Furthermore, it has been observed that the time intervals between symptom onset, diagnosis, and surgery have a significant effect on the outcome, with the highest mortality rate occurring in those undergoing surgery 8 to 12 h after diagnosis [32]. It is recommended that patients presenting with clinical indicators of severe physiologic compromise (shock, neurologic deficits, malperfusion, myocardial ischemia) be considered for repair as a potential option for survival, given the immediacy of the situation.
It is worth noting that patients presenting with type A acute aortic dissection who are hemodynamically stable may have an unpredictable course, given the difficulty in predicting the eventual rupture. Although there are indications that night-time surgery may be associated with an increased risk of mortality, as evidenced by studies that have reported a higher mortality rate during nighttime surgery [33, 34] other studies have indicated that there is no diurnal difference in outcomes [35, 36]. Furthermore, all studies have shown no difference in outcomes between weekend and night-time surgery, suggesting that there may be no inherent disadvantage to performing night-time surgery, at least with respect to mortality. It is recommended to consider the surgeon and center experience and resource availability in order to achieve the best possible outcome. Despite the potential for a slight delay in surgery, transfer from a low- to a high-volume hospital (one that performs 7 aortic root, ascending aorta, or transverse arch aortic dissections repairs per year) [27] as part of a regionalized approach to care can result in significantly improved outcomes [27].
In patients with cerebral malperfusion, there is some evidence to suggest that surgical treatment may be more effective than medical management, although this remains a topic of debate. In patients with acute type A aortic dissection and acute stroke, the mortality rates of surgical versus medical management are 25–27% versus 76% respectively [29, 37]. It is noteworthy that Estrera et al. demonstrated that patients with acute type A aortic dissection who had presented with stroke had a low operative mortality rate of 7% and showed no deterioration in their neurologic status following the operation [30]. While their investigation and others have underscored the importance of timely aortic repair in stroke patients, with a cutoff of 5 to 10 h, Chiu et al. [38] found that there was no association between postoperative neurologic improvement and time from onset of neurologic symptoms to surgery. IRAD data indicates that while mean times to surgery of 12.3 and 13.8 h were experienced by patients who experienced a cerebrovascular accident or coma, respectively, 84% and 79% were successfully resolved [39]. It is, however, important to note that in a recent report of 11 patients with acute type A aortic dissection and complete occlusion of an internal carotid artery, all patients died from cerebral edema and herniation, regardless of treatment strategy, [40] which raises questions about whether surgical intervention is beneficial in this subset of patients.
Individual surgeon’s skills
The surgeon has completed at least 20 elective or urgent TAAAD repairs, including ascending aorta/aortic arch, in the past year.
Preoperative antithrombotic medications administered
Any of the following antithrombotic medications must not be consumed within two days before the surgical procedure: aspirin, clopidogrel, ticagrelor, prasugrel, ticlopidine, low-molecular weight heparin, unfractionated heparin, fondaparinux, direct oral anticoagulants and/or warfarin.
Laboratory benchmarks assessment, both baseline and postoperative
The following benchmarks will be monitored: baseline levels of hemoglobin, creatinine, platelets, arterial lactate, cardiac enzymes, and C-reactive protein, as well as postoperative minimum peak tresholds of hemoglobin and platelets, and postoperative peak thresholds of creatinine and arterial lactate.
Attention to genetic disorders
It is possible for genetic syndromes to lead to aortopathies and TAAAD. The purpose of this registry is to collect data on any specific genetic syndrome associated with TAAAD.
Arterial hypertension
A systolic arterial pressure of greater than 150 mmHg and a diastolic arterial pressure of greater than 80 mmHg, or the use of anti-hypertensive drugs, are indicative of a systemic arterial pressure greater than 150/80 mmHg.
Diabetes
The presence of hyperglycemia, which necessitates the administration of insulin or oral pharmaceuticals.
Neurologic dysfunction
Any new neurological deficit, whether transient or permanent, focal or global, identified by a standard neurological examination (performed by a neurologist or other qualified physician and documented by appropriate diagnostic tests and consultation notes). The investigating physician distinguishes between transient ischaemic attack (TIA) and stroke, TIA being fully reversible within 24 h without evidence of infarction and stroke lasting more than 24 h or less than 24 h with evidence of infarction. To document the presence and severity of neurological deficits, the Modified Rankin Scale and the NIH Stroke Scale must be administered at the time of the event (within 72 h following the event) and 90 days following the event.
Subcategories must be assigned to each neurological event as:
-
A transient ischaemic attack (TIA) refers to an acute event that is completely reversed within 24 h and does not show imaging evidence of infarction.
-
Ischemic or Hemorrhagic Stroke, also known as Cerebrovascular Accident, is considered to be an event lasting more than 24 h or less than 24 h and accompanied by infarction on imaging. If an ischemic stroke undergoes hemorrhagic conversion, it should still be classified as ischemic.
-
Toxic Metabolic Encephalopathy refers to a disturbance of brain function resulting from abnormal systemic metabolism or exogenous agents that alters awareness and/or consciousness, in which there is a non-focal neurological examination and a negative brain scan.
Previously suffered a transient ischemic attack
This definition applies to any preoperative focal or global neurological syndrome caused by ischemia or hemorrhage that resolves within 24 h. It encompasses a neurological event that occurs at any time before the patient is admitted for treatment of TAAD, but not one that is directly related to the acute phase of TAAD.
Previously suffered a stroke
This refers to any preoperative focal or global neurological syndrome caused by ischemia or hemorrhage that does not resolve within 24 h is a qualifying event. It refers to a neurological event occurring any time before hospitalization for TAAAD, but not to a neurological event related to acute TAAAD.
Neurocognition
Neurocognition will be the focus to assess cognitive performance using a battery of tests. These tests include the Hopkins Verbal Learning Test, Trailmaking Tests A and B, MCG Complex Figures, Boston Naming Test, Digit Span, and Digit Symbol Substitution Test Clinical site personnel, trained by experienced neuropsychologists identified at each site of recruiting, will administer neurocognitive testing. Neurologists at each center of enrollment will perform all neurocognitive test scoring.
Functional status
-
New York Heart Association (NYHA) Classification
Functional status is determined using the NYHA classification scale. Full guidelines for the NYHA classification can be found in supplementary material. Table 3.
-
Angina Class
Angina class is assigned according to the Canadian Cardiovascular Society Classification (CCSC) [41].
-
Myocardial Infarction
Myocardial infarction (MI) is diagnosed when there is clinical sign of myocardial necrosis consistent with myocardial ischaemia. [42] The diagnosis can be made if any one of the following criteria is met:
-
MI
-
Evidence of an increase and/or decrease in cardiac biomarkers (ideally troponin) with at least one value above the 99th percentile of the upper limit of reference (URL), together with evidence of myocardial ischaemia with at least one of the following:
-
ECG changes indicating new ischemia, such as new ST-T changes or new left bundle branch block (LBBB).
-
Ischemia signs.
-
pathological Q waves have developed in the ECG.
-
Imaging findings of new loss of viable myocardium or new regional wall motion abnormalities.
-
-
Peri-TAAAD repair MI
For patients undergoing TAAAD repair with normal baseline troponin values, elevations of cardiac biomarkers above the 99th percentile URL indicate peri-procedural myocardial necrosis. Conventionally, biomarker elevations greater than 5 times the 99th percentile upper reference limit (URL), in addition to new Q waves or new LBBB, new graft or native coronary artery occlusion documented by angiography, or imaging findings of new loss of viable myocardium, have been considered to diagnose TAAAD-related MI.
-
Peri-Percutaneous Intervention (PCI) MI.
This condition is observed in patients who have undergone percutaneous coronary intervention (PCI) and have developed iatrogenic TAAAD. For patients who have undergone previous PCI with normal baseline troponin values, elevations of cardiac biomarkers above the 99th percentile URL indicate peri-procedural myocardial necrosis. Elevations in biomarkers > 3 × 99th percentile URL have been conventionally interpreted as defining PCI-related MI. A subset associated with documented stent thrombosis is recognized.
-
Sudden unexplained cardiac mortality associated with cardiac arrest, often with symptoms consistent with myocardial ischaemia, and associated with suspected new ST elevation or new LBBB and/or evidence of fresh thrombus by coronary angiography and/or autopsy, where death precedes the collection of blood samples or the expected appearance of cardiac biomarkers in the blood, is classified as mortality due to MI.
Physiologic measures
-
Echocardiography assessment are as follows:
-
Quantification of aortic regurgitation.
-
Quantifying aortic valve area.
-
Left ventricle (LV) size and function including, left ventricle ejection fraction (LVEF), left ventricle end diastolic dimension (LVEDD), left end systolic dimension (LVESD), left end diastolic volume indexed (LVEDVI), left end systolic volume indexed (LVESVI).
-
In patients with connective tissue disease (CTD) who are experiencing TAAAD, it is essential to consider the LA dimension, which encompasses Barlow disease of the mitral valve.
-
In patients with CTD who are experiencing TAAAD, it is necessary to consider the right ventricle (RV) size and function.
-
Assessing regional wall motion for left ventricular function and viability.
Renal events
The classification of renal function will be based on the estimated glomerular filtration rate (eGFR), which will be calculated using both the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [43] and the European Kidney Function Consortium (EKFC) equation [44]. The severity of renal failure will be classified into different stages, as listed in Table 4.
Two types of kidney related events will be recognised:
-
Renal Dysfunction.
Abnormal kidney function is defined as a rise in serum creatinine (Cr) of more than 100% from baseline, and a Cr level greater than 2.0.
-
Renal Failure.
New requirement for hemodialysis related to renal dysfunction. This definition excludes aquapheresis for volume removal alone.
Extracardiac arteriopathy
The following are examples of conditions which may be present: lower limb claudication, critical limb ischemia, carotid occlusion or greater than 50% stenosis, enhanced risk of amputation due to occurred arterial disease, previous or planned intervention on the abdominal aorta or on the extremities or carotid arteries.
Pulmonary disease
The use of bronchodilators and/or steroids for the treatment of lung diseases [45].
Pulmonary hypertension
The systolic pulmonary artery pressure in patients coming towards the operating room is categorized as follows: <31 mmHg, 31–55 mmHg, and > 55 mmHg. [45].
Limited mobility
This condition is defined as severe impairment of mobility due to musculoskeletal or neurological dysfunction [45].
Moderate-to-severe frailty
The patient requires assistance due to moderate-to-severe physical and cognitive impairment (score > 5 on the Rockwood Clinical Frailty Scale) [46].
Patient in a critical preoperative state
In the preoperative setting, the following conditions should be idenitifed and recorded separately: ventricular tachycardia or ventricular fibrillation or aborted sudden death, preoperative cardiac massage, preoperative ventilation before the anesthetic room, preoperative inotropes, and preoperative acute renal failure (anuria or oliguria < 10 ml/hr) [45].
Patient’s neurological condition prior to the procedure
The following conditions will be reported as separate variables: unconsciousness prior to sedation, hemiplegia/hemiparesis, paraplegia/paraparesis, dysarthria/aphasia, vision loss, confusion, and intubation/sedation at hospital admittance.
Malperfusion
Table 5 offer suggestions for the management of malperfusion, and the clinical evidence presented therein pertains to malperfusion syndrome [47,48,49,50].
Malperfusion is defined as acute organ ischemia resulting from aortic tributary vessel hypoperfusion. This severe condition is typically identified through the examination of clinical signs and symptoms [51, 52]. In this context, myocardial malperfusion is defined as any alterations in ST levels observed in an electrocardiogram, in addition to an increase in cardiac enzymes. Cerebral malperfusion, on the other hand, is identified by the occurrence of acute preoperative stroke. For the purposes of this document, spinal malperfusion will be deemed to be acute paraplegia or paraparesis. Mesenteric malperfusion will be defined as sudden, mild to severe abdominal pain joined or not by nausea and vomiting, which may or may not be joined by rectal bleeding or bloody diarrhea. Renal malperfusion will be identified as anuria or oliguria. Peripheral malperfusion will be identified as a lack of pulse, joined by sensory or motor shortfalls in any limb. Figure 2 presents a decision tree that will be used to distribute patients into the different study groups.
Preoperative computed tomography discoveries
Preoperative computed tomography scans will be evaluated to assess the extent of aortic dissection/intramural hematoma in different aortic subdivisions and their ramifications. Dissection of aortic tributary vessel will be identified as any intimal flap at the artery provenance causing any degree of stenosis. This also applies to aortic tributary vessel perfused through the false lumen. We will collect data on the maximal diameter of the aortic root, ascending aorta, aortic arch, descending aorta, and abdominal aorta.
Intramural hematoma
The diagnosis of aortic intramural hematoma, defined as a hematoma confined to the media of the aorta without intimal flap formation, is made when no concomitant intimal flap is in situ at preoperative imaging. When an intramural hematoma is associated with an intimal flap in another segment of the aorta, the condition is classified as a quite aortic dissection.
Arterial and venous cannulation plants
This designation pertains to the primary cannulation sites. Any alteration to the designated cannulation site prior to the initiation of cardioplegia will be duly noted.
Intraoperative discoveries
A comprehensive data collection will be conducted on the intraoperative findings of the pericardium, ascending aorta, and aortic arch, in order to gain a deeper understanding of the nature of the dissection. In addition, an in-depth description will be provided regarding the extent of the dissection at the level of the Valsalva sinuses and the morphology of the aortic valve.
Surgical repair
Information pertaining to the specific type of aortic root/ascending aorta and aortic arch surgical repair will be gathered, along with dateline on any concomitant major cardiac surgery proceedings Additionally, details regarding the level of aortic anastomosis will be duly identified and recorded. In particular, data on the suture techniques employed for aortic anastomosis (i.e., the use and number of layers of Teflon or pericardial patch to reinforce the anastomosis and the aortic wall) and the use of biological glue to the dissected tissues will be retrieved. In the context of anastomosis suture techniques, a double layer reinforcement patch technique refers to a suture with two patches: one outside the aorta and the other between the dissected tissues or from inside the aorta. Similarly, a triple layer reinforcement patch technique involves a suture with three patches: one outside the aorta, one within the dissected tissues and one from inside the aorta.
Cardiopulmonary bypass setpoints
Information pertaining to the timeframe myocardial ischemia, cardiopulmonary bypass, hypothermic circulatory arrest, and retrograde or antegrade cerebral perfusion will be gathered. In instances where multiple perioperative periods of perfusion or organ ischemia have occurred, the total timeframe of these periods will be recorded. Additionally, the lowest temperature attained during hypothermic circulatory arrest will be documented.
Outcomes and their criteria for definition
Operative mortality
Defined as 30-day and in-hospital mortality. The occurrence of death from any cause during the index hospitalization, which is defined as the period of time during which the patient received surgical treatment for TAAAD.
Acute heart failure
A condition characterized by a sudden decline in cardiac function, resulting in the need for inotropic support for more than 24 h and/or the utilization of a mechanical circulatory support device.
Safety
-
Re-operation.
All re-operations and re-operation-related procedures associated with each distinct TAAAD approach will be duly recorded and the incidence of re-operation will be subjected to rigorous analysis.
-
Adverse Events.
An adverse event (AE) is any unwanted clinical occurrence in a study participant, irrespective of whether it is associated with the study intervention or not. Pre-existing conditions are not considered adverse events unless there is a change in their nature, severity, or degree.
The incidence of serious adverse effects over the course of the trial will be compared between the two treatment groups. Specialists in charge of clinical control at each center will adjudicate all serious and protocol-defined AE. The safety endpoints will be recorded as the frequency of each adverse event, the rate of adverse events per patient/year and the time to each event. Additionally, the number of patients experiencing each type of serious adverse event will be recorded. Safety data will be collected during patient follow-up and the incidence of each event type will be calculated with 95% confidence intervals.
-
Serious Adverse Event.
According to Food and Drug Administration (FDA) guidelines, a serious adverse event is any experience that results in death, is life-threatening, results in significant or prolonged disability, requires or prolongs hospitalisation, results in a congenital anomaly/birth defect, or, in the opinion of the investigators, represents other significant risks or potentially serious injury to subjects or others. Major medical events that are not fatal, life-threatening, or requiring hospitalisation may be considered serious adverse events if, in the reasonable medical judgment of a clinician, they may endanger the patient and may require medical or surgical intervention to prevent one of the outcomes listed in this definition. Examples of medical events that may require medical or surgical treatment are: bronchospasm requiring intensive care in an emergency department or at home, blood dyscrasias, or seizures that do not require inpatient hospitalisation.
-
Unexpected Major Adverse Events.
An unexpected major adverse event refers to a serious adverse event that is not defined in the protocol or documented in the patient consent form. Unscheduled notification is mandatory for unexpected serious adverse events. During hospitalization and follow-up, the study will document any adverse events. The investigator will evaluate the relationship between the adverse event and the procedure performed. Causality is defined in Table 6.
-
Specific Adverse Events Definition.
-
Myocardial Infarction.
Myocardial infarction (MI) is diagnosed when there is clinical sign of myocardial necrosis consistent with myocardial ischaemia [42].
-
Stroke.
A condition characterized by an acute episode of a focal or global neurologic deficit that presents at least one of the following: change in the level of consciousness, hemiplegia, hemiparesis, numbness, or sensory loss on one side of the body, dysphasia or aphasia, hemianopia, or other neurologic signs or symptoms consistent with a stroke. The duration of the deficit is at least 24 h. In the case of a focal deficit that results in death, the deficit must be documented by neuroimaging to be consistent with a new brain hemorrhage or infarct. Amaurosis fugax, or other neurological signs or symptoms consistent with stroke, must be present for a duration of at least 24 h. If this is not available, neuroimaging must demonstrate the presence of a new brain hemorrhage or infarct. Finally, if the neurological deficit results in death, it is classified as a stroke. Stroke will be classified as ischemic, hemorrhagic, or a combination of both.
-
Global Brain Ischemia.
The patient has been diagnosed with diffuse hypoxic damage, as evidenced by brain imaging and electroencephalography.
-
Paraplegia/Paraparesis.
This means that there is debility and/or sensory disturbances on both sides of the body below the level of the affected area of the spinal cord.
-
Acute Kidney Damage.
We’ll define it based on changes in serum creatinine levels after surgery. We’ll also use the Kidney Disease: Improving Global Outcomes (KDIGO) criteria [43] (Table 4) to grade its severity. Since TAAD patients often stay in the hospital for a while, we’ll evaluate changes in serum creatinine levels during the entire index hospitalization. We know that acute kidney injury can also be diagnosed based on urine output. However, since we’ll be working with data from past events, this method isn’t going to work. We’ll leave it out of the study, then. Dialysis is temporary if it stops when a person is discharged from the hospital where they had surgery for acute TAAD. It’s permanent if it continues after they’re discharged.
-
Mesenteric ischemia.
The clinical syndrome of mesenteric ischemia presents with abdominal pain, which may be associated with nausea and vomiting, and with rectal bleeding or bloody diarrhea [53]. The diagnosis of this condition can be established at the imaging, endoscopic and/or surgical levels.
-
Mechanical Circulatory Support.
Mechanical circulatory support (MCS) is defined as the use of intra-aortic balloon pump (IABP) and/or venoarterial extracorporeal membrane oxygenation (VA-ECMO) for the treatment of postoperative acute heart failure. The duration of treatment for these patients will be documented in order to assess the effectiveness of the aforementioned therapies.
-
Cardiac Arrhythmias.
Any recorded arrhythmia that causes clinical impairment (e.g. haemodynamic impairment, oliguria, pre-syncope or syncope), necessitates hospitalisation or a physician visit, or occurs during hospitalisation. Cardiac arrhythmias are classified into two categories:
-
Persistent ventricular arrhythmia necessitating defibrillation or cardioversion.
-
Persistent supraventricular arrhythmia necessitating drug treatment or cardioversion.
-
Respiratory Insufficiency.
Respiratory function impairment that requires re-intubation, tracheostomy, or the inability to discontinue ventilatory support within 48 h after surgery. This does not include intubation for re-operation or temporary intubation for diagnostic or treatment purposes.
-
Hepatic Dysfunction.
If any two of the following liver test results (total bilirubin, aspartate aminotransferase/AST and alanine aminotranferease/ALT) are three times higher than the upper limit of normal for the hospital, or if liver dysfunction is the main cause of death.
-
Procedures for vascular complications.
The present study will examine procedures for vascular complications, including any vascular and endovascular intervention for ischemic and bleeding complicating event. The aggravating contingency in question will encompass neurologic complicating event, mesenteric ischemia, upper and lower limb ischemia, as well as bleeding from the aorta and its ramifications.
-
Bleeding.
A bleeding incident is characterised by any of the following.
-
Death due to hemorrhage can occur when more than 10 units of red blood cells are transfused within the first 24 h following surgery.
-
Re-operation may be necessary in cases of hemorrhage or tamponade.
Note
A hemorrhagic stroke is classified as a neurological event rather than a distinct bleeding event.
-
Blood loss and transfusions.
A data collection initiative is underway to ascertain the number of transfused units of red blood cells. The E-CABG bleeding classification has been proposed as a simple classification of perioperative bleeding, with evidence suggesting its comparability to the Universal Definition of Perioperative Bleeding in the prediction of early mortality [54, 55]. This study will adopt a simplified version of the E-CABG perioperative classification [54,55,56]. According to this classification, severe bleeding is defined as the requirement for the transfusion of more than 4 units of red blood cells during and after surgery, in addition to the need for a reoperation due to excessively heavy intrathoracic bleeding, as detailed in Table 7.
-
Reoperation for Bleeding.
A reoperation for bleeding is defined as the reopening of the chest for the purpose of controlling excessive bleeding. This definition encompasses any reoperation for bleeding in patients in whom the sternum was left open. Conversely, a reoperation for bleeding does not include instances of hemodynamic instability without excessive bleeding, as well as pericardial/pleural puncture or chest drain insertion for retained blood syndrome.
-
Major Infection.
A new episode of clinical infection with pain, fever, drainage and/or leukocytosis in the setting of antimicrobial treatment (non-prophylactic). There should be a positive culture from the infected site or organ, unless there is strong clinical evidence that treatment is required despite negative cultures. The following are the general categories of infection:
-
Localized Infection.
The infection is limited to a specific organ or region, such as mediastinitis, and there is no evidence of systemic involvement (as defined by sepsis). This is determined through standard clinical methods and may be associated with evidence of bacterial, viral, fungal, or protozoal infection, or may require empirical treatment.
-
Infection of the prosthesis or Endocarditis.
The following clinical signs, symptoms, and laboratory tests are compatible with endocarditis: fever of 38. 0 °C or higher, positive blood cultures, new regurgitant murmurs or heart failure, the presence of embolic phenomena (such as focal neurologic impairment, glomerulonephritis, renal and splenic infarcts, and septic pulmonary infarcts), and peripheral cutaneous or mucocutaneous lesions (such as petechiae, conjunctival or splinter hemorrhages, Janeway lesions, Osler’s nodes, and Roth spots). If echocardiography reveals a new intra-cardiac vegetation, along with or without other signs and symptoms, this should be considered sufficient evidence to support the diagnosis of endocarditis. Transesophageal echocardiography (TEE) is the preferred diagnostic modality for prosthetic valve endocarditis.
-
Sepsis.
There is sign of systemic involvement by infection as evidenced by positive blood cultures and/or hypotension.
-
Deep sternal wound infection/mediastinitis.
The term “deep sternal wound infection” is defined as an infection that has been proven to involve deep sternal wound tissues and/or the mediastinum.
-
Venous Thromboembolic Event.
Clinical and laboratory evidence of a venous thromboembolic event, such as deep vein thrombosis or pulmonary embolism, can be detected using standard tests.
-
Arterial Non-Central Nervous System Systemic Thromboembolism.
Confirmation of an acute systemic arterial perfusion deficit in any non-cerebrovascular organ system due to thromboembolism can be made by one or more of the following:
-
Standard clinical and laboratory testing o Operative findings.
-
Autopsy findings.
This definition excludes neurological events.
-
Pericardial Fluid Trapping.
Pericardial effusion is the collection of fluid or thrombus in the pericardial space requiring surgical intervention or percutaneous catheter drainage. This event can be further classified into two categories: those with clinical signs of tamponade (such as increased central venous pressure and decreased cardiac output) and those without signs of tamponade.
-
Other.
An occurrence that results in a clinically significant alteration in the patient’s state of health, or any event that is life-threatening, results in death, leads to permanent disability, necessitates hospitalisation or prolongs an existing hospital course.
Hospitalization
-
Index Hospitalization.
We will measure the length of stay for the index hospitalization and break it down by days stayed in the ICU. Additionally, we will record the discharge location.
-
Readmission.
Readmission ratios will be computed for the first 30 days after the procedure and for the duration of follow-up. All hospitalizations will be categorized, including any adverse event involving the prior surgical repair of TAAAD, as well as cardiovascular and heart failure readmissions. To classify a readmission as heart failure related, at least two of the following signs and conditions of acute decompensated heart failure must be observed:
-
Dyspnea felt related to HF.
-
Administration of vasodilators, intravenous diuretics or inotropes.
-
Pulmonary capillary wedge pressure (PCWP) or left ventricular end-diastolic pressure.
(LVEDP) > 18 mmHg.
-
On physical examination, rales may indicate the presence of malperfusion syndrome, pulmonary edema or pulmonary vascular congestion as seen on X-ray.
-
CT scan control of the procedure performed.
The investigator will classify all readmissions, which will then be adjudicated by the cardiologist in charge of hospitalization.
Quality of life
The study will assess improvement in quality of life (QOL) from baseline using the disease-specific Minnesota Living with Heart Failure (MLHF) score, the disease-specific Duke Activity Status Index (DASI), the Short Form-12 general health status index and the EuroQol 5-D measures of health state preference from an individual and societal perspective. The Minnesota Living with Heart Failure Questionnaire is a tool that measures the physical, psychological, and social effects of heart failure and its treatment on patients. The DASI questionnaire provides cardiovascular stress across four spheres of adult activity that are linked with oxygen uptake: walking, personal care, household tasks, and sexual function and leisure. The SF-12 examines 8 dimensions of quality of life, including physical activity, social activity, role/physical, body pain, general mental health, role/emotional, vitality, and general health perception. The SF-12 and EuroQoL 5-D are both instruments used to measure health-related quality of life. The EuroQoL 5-D is a standardized questionnaire that provides a simple descriptive profile consisting of 5 dimensions. The EuroQoL 5-D is a standardized questionnaire that provides a simple descriptive profile consisting of 5 dimensions. The instrument assesses five domains: anxiety/depression, pain/discomfort, usual activities, self-care, and mobility. Additionally, it includes a self-assessment of health status.
Late outcomes
Outcomes at the conclusion of the study will be evaluated. Patients who have been lost to follow-up will be identified. Any subsequent surgical or endovascular procedures on the aorta will be documented, including the urgency, indications, and aortic segment treated.
Assessments for statistical analysis
One of the primary research objectives of this registry is to investigate the impact of EAR compared to more limited aortic resection on early and late outcomes. Given the expected low frequency of this surgical approach, we conducted a sample size analysis to determine the extent of distal aortic repair. Notwithstanding the aforementioned constraints, including the failure to consider the combined impact of competing risk factors or the repeat operation factor, the Lau et al. [6] study reported that an extensive approach, including the EAR, was a predictor of late reoperation (odds ratio, 3.03 [95% confidence interval, 1.29–7.2]; P = 0.01). If we use this odds ratio, we’ll need about 100 patients in each study group to reject the null hypothesis (alpha 0.05, power 0.80).
One effective strategy for inducing downstream aortic remodeling and reducing the need for distal reinterventions is to choose the HAR-DAA or EAR-DAA surgical option. Vallabhajosyula and colleagues reported that stent graft placement at the time of the index TAAAD repair was associated with improved false lumen thrombosis of the stented segment (82% vs. 39%; P < 0.01). However, freedom from open reintervention was not significantly different between the stented and non-stented groups (98% vs. 90%; P = 0.1). However, endovascular late reintervention was significantly higher in the non-stented group (18% vs. 3%, P < 0.01) [55]. Preventza and colleagues [13] reported that the need for reintervention was also not significantly different. However, in a matched comparison, 5-year survival was better in the stented group (49.9% vs. 41.6%, P < 0.015). In a selected group of patients who received an antegrade stent graft, Roselli and colleagues [56] observed that thrombosis of the FL in the stented segment was 92%, 5-year freedom from reintervention was only 72%, and survival was 80%0.31 Shrestha and colleagues [17] consistently utilized FET in EAR for TAAAD. Despite this approach, 12% of operative survivors still required downstream aortic reinterventions.
In order to calculate the requisite sample size for a non-inferiority trial, it was appointed that the freedom rate from distal aortic reoperation would be 95%. Additionally, it was posited that a difference in the reoperation rate as great as 10% in favour of EAR would be permissible. A non-inferiority margin of 0.1, with a power of 0.90 and a one-sided confidence interval of 97.5%, would allow the less extensive repair to be non-inferior. The required sample size would therefore be 100 patients per group. It is hired that approximately 20% of patients have undergone total arch repair in this collaborative registry. Therefore, a study population of 1300 patients would be sufficient to study the impact of EAR in preventing late aortic reoperation in patients with acute TAAD. It is anticipated that the participating hospitals will provide a sample size of at least 1900 patients (i.e., a mean of > 20 procedures for acute TAAAD each year), which would prevent a type II error.
Statistical analysis
Microsoft Access software (Microsoft Corp., Redmond, Wash.) will be used to store data. IBM SPSS Statistics version 24 (IBM Corp., Armonk, NY) will analyze the data, as will R version 3.4.2 (R Foundation for Statistical Computing) and the R packages tableone, survminer, and cmprsk. We will use the c2 test to analyze categorical variables with a frequency of five or less. For those with a frequency of five or more, we will use Fisher’s exact test. Continuous variables are assessed through the application of the Mann-Whitney test after ensuring normality. We will use propensity score matching to achieve a balance in treatment strategies for any differences at baseline. The propensity score will be estimated using a non-parsimonious multilevel mixed-effects logistic regression, taking into account the cluster effect of the participating centers. This will allow for the consideration of referral pathways, surgical techniques and perioperative care. The multilevel mixed-effects logistic regression model will include all available baseline variables. We will use the estimated propensity score for inverse propensity score weighting analysis and one-to-one propensity score matching analysis using a caliper width of 0.1 to 0.2 of the standard deviation of the estimated logit. We will accept standardised differences < 0.10 between the matched cohorts as an acceptable imbalance. We will perform logistic and Cox multivariable regression analysis to determine significant predictors of both in-hospital adverse events and long-term survival. To evaluate goodness of fit, we will employ the Akaike information criterion for logistic regression and the Akaike and Bayesian information criterion for Cox regression. To verify the proportional hazards assumption, we will conduct a test using Schoenfeld residuals. We will also examine multicollinearity by calculating the variance inflation factor (VIF) on all variables. Any VIFs ≥ 2 will be excluded from the analysis, as these data are highly correlated with other variables.
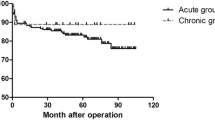
Regarding missing data, our dataset had a low rate of < 6% missing data, which we will exclude from the analysis. We will evaluate long-term survival using the Kaplan–Meier method and compare it using the log-rank test. All patients will have at least one follow-up visit. Patients will be censored at the time of their last follow-up. We will calculate the competing risk of reoperation, with death as a competing risk, using the Fine and Gray method [57].
We will evaluate interinstitutional and between-surgeons differences in terms of early outcomes using mixed-effects logistic regression. We will estimate the risk-adjusted rate of adverse binary events at each center by dividing the observed number of adverse events by the expected number of adverse events and multiplying this ratio by the average event rate of the overall series. We will calculate the expected numbers of adverse events with logistic regression. We will summarize the estimated risk-adjusted rates of adverse events as odds ratios and their 95% confidence intervals in caterpillar plots with the x-axis ordered for increasing adjusted rates.
Discussion
The past two decades have witnessed a notable improvement in surgical experience and outcomes following TAAAD repair [3, 58,59,60,61]. In the nonemergency setting, EAR procedures have gained traction, with a wide range of techniques employed. Variability in techniques has also been observed in the emergency setting [8, 55, 62,63,64,65]. The reluctance to perform EAR procedures in TAAAD is attributable to concerns regarding the technical complexity and increased perioperative risk, particularly in relation to the occurrence of stroke and the development of spinal cord ischemia. This protocol will evaluate one-quarter of patients who have undergone an EAR operation to determine whether there is an equivalent rate of perioperative mortality and a worse neurological outcome after statistical adjustment.
A number of single-center studies have indicated that there is no significant difference in perioperative mortality and neurologic complications between the FET technique [63, 66] TEVAR, [64] and other EAR techniques [65, 67, 68]. It is important to note that these studies are limited by the heterogeneity of definitions used for neurologic complications, the variability in the extent of dissection, and the relatively young age of the patient populations observed in some centers. It is crucial to emphasize that the findings of these studies may not be directly applicable to the referral center context [66, 69]. Despite the encouraging results observed at a single center, the Society of Thoracic Surgeons multicenter series examining the correlates of perioperative stroke in TAAAD repair (n = 7353) is yet to identify TARP as a significantly associated factor with stroke [70].
Limitations
The preceding two decades have seen changes in surgical technique and experience. Age-adjustment statistics partially mitigate this effect. The protocol’s definitions for the extent of root and arch surgery and neurological outcomes are standardised. However, the inherent variability in these definitions means that the registry data may not be entirely accurate. The procedures in the EAR group are heterogeneous. To perform individual comparisons based on the type of EAR technique would require a larger sample size. We will set the number of patients at 20% in the protocol, but this number could be lower. In fact, the Canadian registry [70] reported only 16% of patients who had an EAR-DA and 25% who had an EAR-NDAA [70]. Likewise, the data from the UK TAAAD registry show that the EAR-DA and EAR-NDAA techniques have lower reported rates [2].
We must acknowledge that there is still considerable heterogeneity with respect to the degree of extension of dissected aorta. It is quite challenging to confirm the extent of inner curvature resection in HAR replacements from retrospective analysis. We will therefore consider any distal more proximal open repair of the innominate artery as HAR, which may include some less aggressive ascending replacements performed in circulatory arrest. Furthermore, we must determine the number of patients for whom computed tomography (CT) scan data will be available before discharge to ensure the reliability of the post-procedure image-based analysis. CT scans may not be available for all patients, which could introduce a potential bias in our analysis among those with available postoperative images. We must consider the possibility that CT scans may not be available for all patients, introducing a potential bias into the analysis of those with available postoperative images. In order to fully understand the influence of EAR interventions on aortic remodeling, we must obtain late follow-up. This was planned as part of this study.
We will complete one of the largest multicenter studies comparing arch intervention strategies currently available. Our protocol could be an important trial on the subject, especially in relation to the lack of large, randomized studies that have reported robust results.
Conclusion
In this study, we will compare aggressive and conservative approaches for aortic arch repair in a large European cohort of patients with TAAAD. Our goal is to demonstrate that extended arch surgeries can be performed in TAAAD with similar perioperative mortality and neurological risk as less aggressive surgeries. The analysis of subgroups of patients receiving EAR-DAA or EAR-NDAA will undoubtedly pave the way towards a “time-only” treatment of extended TAAAD in the descending aorta. We will clarify the extent to which extended techniques should be approached in the context of TAAAD, given the increased risk of perioperative complications. We will demonstrate that extended repairs can improve the resolution of malperfusion, especially when performed with techniques involving interventions in the descending aorta.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CPB:
-
Cardiopulmonary bypass
- CTD:
-
Connective tissue disease
- DAA:
-
Descending aortic access
- EAR:
-
Extended arch repair
- eGFR:
-
Glomerular filtration rate
- EKFC:
-
European Kidney Function Consortium
- FET:
-
Frozen elephant trunk
- FL:
-
False lumen
- HAR:
-
Hemiarch repair
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- IABP:
-
Intra-aortic balloon pump
- IRB:
-
Institutional review board
- LBBB:
-
Left bundle branch block
- MAE:
-
Major Adverse Events
- MAPE:
-
Major Adverse Pulmonary Events
- MCS:
-
Mechanical circulatory support
- MLHF:
-
Minnesota Living with Heart Failure
- MI:
-
Myocardial infarction
- NCT:
-
Number clinical trial
- NDAA:
-
Non descending aortic access
- NYHA:
-
New York Heart Association
- OM:
-
Operative mortality
- PCI:
-
Percutaneous coronary intervention
- PND:
-
Permanent neurologic deficit
- QOL:
-
Change in quality of life
- SCI:
-
Spinal cord injury
- TAAAD:
-
Type A acute aortic dissection
- TIA:
-
Transient ischaemic attack
- URL:
-
Upper reference limit
- VA-ECMO:
-
Venoarterial extracorporeal membrane oxygenation
References
Biancari F, Juvonen T, Fiore A, et al. Current outcome after surgery for type A aortic dissection. Ann Surg. 2023 Mar;13. https://doi.org/10.1097/SLA.0000000000005840.
Benedetto U, Dimagli A, Kaura A, et al. Determinants of outcomes following surgery for type a acute aortic dissection: the UK National Adult Cardiac Surgical Audit. Eur Heart J. 2021;43(1):44–52. https://doi.org/10.1093/eurheartj/ehab586.
Evangelista A, Isselbacher EM, Bossone E, et al. Insights from the International Registry of Acute Aortic dissection: a 20-Year experience of collaborative clinical research. Circulation. 2018;137(17):1846–60. https://doi.org/10.1161/CIRCULATIONAHA.117.031264.
Conzelmann LO, Weigang E, Mehlhorn U, et al. Mortality in patients with acute aortic dissection type A: analysis of pre- and intraoperative risk factors from the German Registry for Acute Aortic dissection type A (GERAADA). Eur J Cardiothorac Surg. 2016;49(2):e44–52. https://doi.org/10.1093/ejcts/ezv356.
Geirsson A, Shioda K, Olsson C, et al. Differential outcomes of open and clamp-on distal anastomosis techniques in acute type a aortic dissection. J Thorac Cardiovasc Surg. 2019;157(5):1750–8. https://doi.org/10.1016/j.jtcvs.2018.09.020.
Lau C, Robinson NB, Farrington WJ, et al. A tailored strategy for repair of acute type a aortic dissection. J Thorac Cardiovasc Surg. 2022;164(6):1698–e17073. https://doi.org/10.1016/j.jtcvs.2020.12.113. Epub 2021 Jan 12.
Malaisrie SC, Szeto WY, Halas M, et al. 2021 the American Association for Thoracic Surgery expert consensus document: surgical treatment of acute type a aortic dissection. J Thorac Cardiovasc Surg. 2021;162:735–58.e2. https://doi.org/10.1016/j.jtcvs.2021.04.053.
Czerny M, Siepe M, Beyersdorf F, et al. Prediction of mortality rate in acute type a dissection: the German Registry for Acute Type A aortic dissection score. Eur J Cardiothorac Surg. 2020;58:700–6.
White A, Bozso SJ, Ouzounian M, Chu, et al. Acute type a aortic dissection and the consequences of a patent false lumen. J Thorac Cardiovasc Surg Tech. 2021;9:1–8. https://doi.org/10.1016/j.xjtc.2021.05.002.
Carrel T, Sundt TM 3rd, von Kodolitsch Y, et al. Acute aortic dissection. Lancet. 2023;401(10378):773–88. https://doi.org/10.1016/S0140-6736(22)01970-5.
Ergin MA, Phillips RA, Galla JD, et al. Significance of distal false lumen after type A dissection repair. Ann Thorac Surg. 1994;57:820–5. https://doi.org/10.1016/0003-4975(94)90182-1.
Tamura K, Chikazawa G, Hiraoka A, et al. The prognostic impact of distal anastomotic new entry after acute type I aortic dissection repair. Eur J Cardiothorac Surg. 2017;52:867–73. https://doi.org/10.1093/ejcts/ezx223.
Preventza O, Olive JK, Liao JL, et al. Acute type I aortic dissection with or without antegrade stent delivery: mid-term outcomes. J Thorac Cardiovasc Surg. 2019;158:1273–81.
Kim JB, Chung CH, Moon DH, et al. Total arch repair versus hemiarch repair in the management of acute DeBakey type I aortic dissection. Eur J Cardiothorac Surg. 2011;40(4):881–7. https://doi.org/10.1016/j.ejcts.2010.12.035.
Di Eusanio M, Berretta P, Cefarelli M, et al. Total arch replacement Versus more conservative management in type a Acute Aortic Dissection. Ann Thorac Surg. 2015;100(1):88–94. https://doi.org/10.1016/j.athoracsur.2015.02.041.
Zhang H, Lang X, Lu F, Song, et al. Acute type a dissection without intimal tear in arch: proximalor extensive repair? J Thorac Cardiovasc Surg. 2014;147(4):1251–5. https://doi.org/10.1016/j.jtcvs.2013.04.029.
Shrestha M, Haverich A, Martens A. Total aortic arch replacement with the frozen elephant trunk procedure in acute DeBakey type I aortic dissections. Eur J Cardiothorac Surg. 2017;51(suppl 1):i29–34.
Di Bartolomeo R, Murana G, Di Marco L, Pantaleo, et al. Frozen versus conventional elephant trunk technique: application in clinical practice. Eur J Cardiothorac Surg. 2017;51(Suppl 1):i20–8. https://doi.org/10.1093/ejcts/ezw335.
Nienaber CA, Rosendahl U, Yuan X. What is the strategy for strategic arch resection in acute proximal aortic dissection? J Thorac Dis. 2020;12:3418–21. https://doi.org/10.21037/jtd.2020.01.63.
Biancari F, Onorati F, Peterss S et al. Nature of Neurological Complications and Outcome After Surgery for Type A Aortic Dissection. Am J Cardiol. 2024 Mar 6:S0002-9149(24)00167-X. https://doi.org/10.1016/j.amjcard.2024.03.001
Huang F, Li X, Zhang Z, et al. Comparison of two surgical approaches for acute type a aortic dissection: hybrid debranching versus total arch replacement. J Cardiothorac Surg. 2022;17:166. https://doi.org/10.1186/s13019-022-01920-9.
Attia RQ, Cameron DE, Sundt TM III, et al. Total arch replacement in the treatment of acute type a aortic dissection. J Vis Surg. 2021;7:46. https://doi.org/10.21037/jovs-20-125.
Yan Y, Xu L, Zhang H, et al. Proximal aortic repair versus extensive aortic repair in the treatment of acute type a aortic dissection: a meta-analysis. Eur J Cardiothorac Surg. 2016;49:1392–401.
Ma L, Chai T, Yang X, et al. Outcomes of hemi- vs. total arch replacement in acute type a aortic dissection: a systematic review and meta-analysis. Front Cardiovasc Med. 2022;9:988619. https://doi.org/10.3389/fcvm.2022.988619.
Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903.
Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66:350–8.
Goldstone AB, Chiu P, Baiocchi M, et al. Interfacility Transfer of Medicare beneficiaries with Acute Type A aortic dissection and regionalization of care in the United States. Circulation. 2019;140(15):1239–50. https://doi.org/10.1161/CIRCULATIONAHA.118.038867.
Umana-Pizano JB, Nissen AP, Sandhu HK, et al. Acute typeA dissection repair by high-volume vs low-volume surgeons at a high-volume aortic center. Ann Thorac Surg. 2019;108:1330–6.
Di Eusanio M, Patel HJ, Nienaber CA et al. Patients with type A acute aortic dissection presenting with major brain injury: should we operate on them? J Thorac Cardiovasc Surg. 2013;145:S213-21.e1.
Estrera AL, Garami Z, Miller CC, et al. Acute type a aortic dissection complicated by stroke: can immediate repair be performed safely? J Thorac Cardiovasc Surg. 2006;132:1404–8.
Braverman AC. Acute aortic dissection: clinician update. Circulation. 2010;122:184–8.
Matthews CR, Madison M, Timsina LR, et al. Impact of time between diagnosis to treatment in acute type a aortic dissection. Sci Rep. 2021;11:3519.
Qiu J, Zhang L, Luo X, et al. Higher mortality in patients undergoing nighttime surgical procedures for acute type a aortic dissection. Ann Thorac Surg. 2018;106:1164–70.
Ahlsson A, Wickbom A, Geirsson A, et al. Is there a weekend effect in surgery for type A dissection? Results from the Nordic Consortium for Acute type A aortic dissection database. Ann Thorac Surg. 2019;108:770–6.
Gokalp O, Yilik L, Besir Y, et al. Overtime hours effect on emergency surgery of acute type a aortic dissection. Braz J Cardiovasc Surg. 2019;34:680–6.
Gasser S, Stastny L, Kofler M, et al. Surgery out of office hours for type A aortic dissection: does night-time and weekend surgery worsen outcome? Interact Cardiovasc Thorac Surg. 2020;31:806–12.
Sultan I, Bianco V, Patel HJ, et al. Surgery for type A aortic dissection in patients with cerebral malperfusion: results from the International Registry of Acute Aortic Dissection. J Thorac Cardiovasc Surg. 2021;161:1713–20. e1.
Chiu P, Rotto TJ, Goldstone AB, et al. Time-to-operation does not predict outcome in acute type a aortic dissection complicated by neurologic injury at presentation. J Thorac Cardiovasc Surg. 2019;158:665–72.
Berretta P, Trimarchi S, Patel HJ, et al. Malperfusion syndromes in type A aortic dissection: what we have learned from IRAD. J Vis Surg. 2018;4:65.
Fukuhara S, Norton EL, Chaudhary N, et al. Type a aortic dissection with Ce- rebral malperfusion: new insights. Ann Thorac Surg. 2020;112:501–9.
Campeau L. Grading of angina pectoris. Circulation. 1976;54:522–3.
Borger MA, Murphy AA. PM Chronic lschemic mitral regurgitation: repair, replace or rethink? Ann ThorSurg, 2006. 81: p. 1 153–1161.
Levey AS, Stevens LA, Schmid CH, et al. Coresh J; CKD-EPI (chronic kidney disease epidemiology collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Pottel H, Björk J, Courbebaisse M, et al. Development and validation of a modified full age spectrum creatinine- based equation to estimate glomerular filtration rate: a cross-sectional analysisof pooled data. Ann Intern Med. 2021;174(2):183–91.
Nashef SA, Roques F, Sharples LD EuroSCORE II. Eur J Cardiothorac Surg., Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. https://doi.org/10.1503/cmaj.050051
Geirsson A, Szeto WY, Pochettino A, et al. Significance of malperfusion syndromes prior to contemporary surgical repair for acute type a dissection: out- comes and need for additional revascularizations. Eur J Cardiothorac Surg. 2007;32:255–62.
Leshnower BG, Keeling WB, Duwayri YM, et al. The thoracic endovascular aortic repair-first strategy for acute type a dissection with mesenteric malper- fusion: initial results compared with conventional algorithms. J Thorac Cardiovasc Surg. 2019;158:1516–24.
Lawton JS, Moon MR, Liu J, et al. The profound impact of combined severe acidosis and malperfusion on operative mortality in the surgical treatment of type A aortic dissection. J Thorac Cardiovasc Surg. 2018;155:897–904.
Augoustides JG, Geirsson A, Szeto WY, et al. Observational study of mortality risk stratification by ischemic presentation in patients with acute type a aortic dissection: the Penn classification. Nat Clin Pract Cardiovasc Med. 2009;6(2):140–6. https://doi.org/10.1038/ncpcardio1417.
Zindovic I, Gudbjartsson T, Ahlsson A, Fuglsang, et al. Malperfusion in acute type a aortic dissection: an update from the nordic consortium for acute type a aortic dissection. J Thorac Cardiovasc Surg. 2019;157(4):1324–33. https://doi.org/10.1016/j.jtcvs.2018.10.134.
Tendler DA, Lamont JT. Overview of intestinal ischemia in adults. Waltham, MA: UpToDate, Post, TW, editor, UpToDate; 2020. (accessed March 19, 2021).
Biancari F, Ruggieri VG, Perrotti A, et al. European Multicenter study on coronary artery bypass grafting (E-CABG registry): study protocol for a prospective clinical registry and proposal of classification of postoperative complications. J Cardiothorac Surg. 2015;10:90.
Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg. 2014;147(5):1458–63. https://doi.org/10.1016/j.jtcvs.2013.10.070.
Bartoszko J, Wijeysundera DN, Karkouti K, et al. Transfusion avoidance in cardiac surgery study investigators. Comparison of two major perioperative bleeding scores for cardiac surgery trials: Universal Definition of Perioperative bleeding in cardiac surgery and European coronary artery bypass grafting bleeding severity grade. Anesthesiology. 2018;129(6):1092–100. https://doi.org/10.1097/ALN.0000000000002179.
Vallabhajosyula P, Szeto WY, Pulsipher A, et al. Antegrade thoracic stent grafting during repair of acute Debakey type I dissection promotes distal aortic remodeling and reduces late open distalreoperation rate. J Thorac Cardiovasc Surg. 2014;147:942–8.
Roselli EE, Idrees JJ, Bakaeen FG, et al. Evolu- tion of simplified frozen elephanttrunk repair for acute debakey type I dissection: midterm outcomes. Ann Thorac Surg. 2018;105:749–55.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496.
Abe T, Usui A. The cannulation strategy in surgery for acute type a dissection. Gen Thorac Cardiovasc Surg. 2017;65:1–9. https://doi.org/10.1007/s11748-016-0711-7.
De Paulis R, Czerny M, Weltert L, et al. Current trends in cannulation and neuroprotection during surgery of the aortic arch in Europe. Eur J Cardiothorac Surg. 2015;47:917–23. https://doi.org/10.1093/ejcts/ezu284.
Benedetto U, Mohamed H, Vitulli P, et al. Axillary versus femoral arterial cannulation in type a acute aortic dissection: evidence from a meta-analysis of comparative studies and adjusted risk estimates. Eur J Cardiothorac Surg. 2015;48:953–9. https://doi.org/10.1093/ejcts/ezv035.
Lee TC, Kon Z, Cheema FH, et al. Contemporary management and outcomes of acute type a aortic dissection: an analysis of the STS adult cardiac surgery database. J Card Surg. 2018;33:7–18. https://doi.org/10.1111/jocs.13511.
Di Marco L, Pantaleo A, Leone A, et al. The frozen elephant trunk technique: European association for cardio-thoracic surgery position and bologna experience. Korean J Thorac CardiovascSurg. 2017;50:1–7. https://doi.org/10.5090/kjtcs.2017.50.1.1.
Kremer J, Preisner F, Dib B, et al. Aortic arch replacement with frozen elephant trunk technique - a single-center study. J Cardiothorac Surg. 2019;14:147. https://doi.org/10.1186/s13019-019-0969-9.
Pochettino A, Brinkman WT, Moeller P, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg. 2009;88:482–90. https://doi.org/10.1016/j.athoracsur.2009.04.046.
Rylski B, Milewski RK, Bavaria JE, et al. Long-term results of aggressivehemiarch replacement in 534 patients with type A aortic dissection. J Thorac Cardiovasc Surg. 2014;148:2981–5. https://doi.org/10.1016/j.jtcvs.2014.05.093.
Poon SS, Tian DH, Yan T, et al. Frozen elephant trunk does not increase incidence of paraplegia in patients with acute type a aortic dissection. J Thorac Cardiovasc Surg. 2020;159:118996. https://doi.org/10.1016/j.jtcvs.2019.03.097.
Fichadiya A, Kotha V, Gregory A, et al. What is the long-term aortic remodeling outcome after hemi-arch repair for acute type a dissection? An 11-year study. Can J Cardiol. 2017;33:S31. https://doi.org/10.1016/j.cjca.2017.07.079.
Chen SW, Chen Y, Ma WG, et al. Limited vs. extended repair for acute type I aortic dissection: long-term outcomes over a decade in Beijing Anzhen Hospital. Chin Med J (Engl). 2021;134(8):986–8. https://doi.org/10.1097/CM9.0000000000001416. Published 2021 Apr 6.
Ma WG, Chen Y, Zhang W, et al. Extended repair for acute type a aortic dissection: long-term outcomes of the frozen elephant trunk technique beyond 10 years. J Cardiovasc Surg (Torino). 2020;61(3):292–300. https://doi.org/10.23736/S0021-9509.20.11293-X.
Elbatarny M, Stevens LM, Dagenais F, et al. Hemiarch versus extended arch repair for acute type a dissection: results from a multicenter national registry. J Thorac Cardiovasc Surg. 2024;167(3):935–e9435. https://doi.org/10.1016/j.jtcvs.2023.04.012.
Acknowledgements
Not applicable
Funding
This study will be performed without external financial support.
Author information
Authors and Affiliations
Contributions
FN, TS, SSVA, AS, IA, IG, FS, AF, LG, PD, PL, NB, CS contributed to planning this registry and its related studies as well as to develop the datasheet for data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study does not contain individual patient data and ethics approval is not applicable.
Consent for publication
This manuscript does not contain individual person’s data in any form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nappi, F., Schoell, T., Singh, S.S.A. et al. Aortic arch registry of type a aortic dissection (AoArch) - rationale, design and definition criteria. J Cardiothorac Surg 19, 514 (2024). https://doi.org/10.1186/s13019-024-03002-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-03002-4