Abstract
Background
Type A aortic dissection (TAAD) with coronary involvement is rare but potentially fatal. Proper myocardial protection during surgery is essential.
Case presentation
Here, we describe a 52-year-old woman who presented with sudden chest pain. CT angiography revealed TAAD with right coronary artery involvement. During surgery, the proximal intima of the right coronary artery was found to be completely severed and everted. Conventional myocardial perfusion methods were inadequate. A patented perfusion tip for coronary artery orifice perfusion was used, resulting in favourable surgical outcomes. The patient was discharged without complications.
Conclusions
This case emphasizes the need for careful preoperative assessment of coronary involvement in TAAD patients. The myocardial protection method used here is very helpful and can be applied effectively in similar cases encountered by surgeons.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In patients afflicted with type A aortic dissection (TAAD), coronary artery involvement is rare yet potentially life-threatening due to the risk of myocardial infarction [1,2,3]. Severe coronary ostia involvement impedes coronary perfusion after cross-clamping, and prolonged ischaemic time before myocardial perfusion may result in severe and irreversible myocardial infarction. Thus, ensuring timely and adequate myocardial protection during surgery is important. We present a case of TAAD complicated by right coronary involvement featuring proximal intima sleeve-like severance and eversion, but significant myocardial ischaemia was absent. Conventional myocardial perfusion methods were inadequate for myocardial protection. Utilizing our patented perfusion tip design, we successfully administered cardioplegia via the right coronary artery orifice, leading to successful myocardial protection and subsequent discharge of the patient from the hospital.
Case report
A 52-year-old woman with hypertension was referred to the emergency department with sudden onset of chest pain. The patient reported no prior history of coronary artery disease. Her blood pressure was 160/96 mmHg, and her heart rate was 90 bpm. Clinical examination revealed normal serum levels of myocardial enzymes and cardiac troponin. There were no signs of myocardial infarction on electrocardiography and no apparent wall motion abnormalities on transthoracic echocardiography. Subsequent CT angiography confirmed the diagnosis of TAAD, which prompted preparation for emergency surgery.
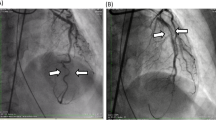
Aortic CT angiography revealed significant enlargement of the false lumen compared to the true lumen, resulting in profound compression of the true lumen. On the cross-sectional CT images, the right coronary artery was clearly identified as originating from the false lumen. Both transverse and curved planar reformation of coronary artery CT images revealed an intraluminal filling defect in the proximal segment of the right coronary artery adjacent to the ostium (Fig. 1).
On April 23, 2023, emergency surgery with midline sternotomy was performed. Cardiopulmonary bypass was established through right axillary artery cannulation combined with right atrium cannulation. Moderate hypothermia and antegrade cerebral perfusion were employed. When the ascending aorta was clamped and the aorta was incised to access the aortic root, an unusual occurrence was observed. There was no thrombus present in the coronary artery. The intima of the right coronary artery exhibited sleeve-like severance, with complete eversion resulting in the inner surface facing outwards and the outer surface facing inwards. This configuration formed a structure resembling a sleeve coupling that was attached to the dissected intima of the aortic root (Fig. 2). Cardioplegia was administered during the procedure by directly cannulating our patented coronary ostial cannula tip into right coronary ostium, which was intimal-free with the adventitial layer remaining intact (Fig. 3). The subsequent steps of the procedure followed previously reported techniques [4]. After achieving cardiac arrest, a saphenous vein graft was anastomosed end-to-side to the distal right coronary artery. Following completion of the anastomosis, graft perfusion was performed to ensure adequate cardiac protection. Subsequently, we conducted the Bentall procedure to address aortic root lesions by implanting a 23 mm St. Jude mechanical valved conduit. Then, the left coronary ostium with button-like aortic tissue was excised from the aorta, which was then reimplanted in the corresponding site in the valved conduit. To ensure long-term coronary patency of right coronary artery, an additional segment of saphenous vein was utilized. It was anastomosed end-to-end with the right coronary ostium, with the other end anastomosed to the ascending valved graft. After the core temperature reached 26 °C, under circulatory arrest and unilateral antegrade cerebral perfusion, a stented elephant trunk was implanted into the descending aorta. A four-branched vascular graft was then sutured to connect the distal ascending aortic graft with the proximal end of the stented elephant trunk. Finally, the proximal end of the saphenous graft was anastomosed to the ligated perfusion branch of the four-branched graft, completing the main surgical procedure.
To address the challenges posed by the reconstruction of the right coronary ostium and to mitigate the risk of haemorrhage and difficulties in achieving haemostasis, we opted to perform right coronary artery bypass grafting (CABG) prior to releasing the cross-clamp. Following the processes of rewarming and deairing, successful cardiac resuscitation was accomplished.
Postoperative examination revealed that the patient had resumed regular activities. Subsequent CT angiography demonstrated a patent saphenous venous graft with satisfactory revascularization of the thoracic aorta (Video 2). This patient had an uneventful recovery and was ultimately discharged from the hospital without any complications related to myocardial infarction.
Discussion
Previous studies reported a 10.6% incidence of coronary involvement, with 3.9% of patients clinically diagnosed with acute myocardial infarction (AMI) [2, 3]. In patients with TAAD complicated by AMI, the most common pathological change is compression of the coronary ostium, often leading to myocardial infarction. This case is unique due to the complete severance and eversion of the proximal coronary artery intima, and the right coronary artery was entirely supplied by the false lumen as a result. Typically, the complete severance and reversal of the intima in the proximal coronary artery is rare. Patients with severe coronary involvement may die before receiving proper medical attention. However, these distinctive anatomical characteristics contribute to patient survival until successful surgery can be performed.
TAAD patients with coronary involvement have a high mortality rate and require aggressive coronary revascularization [2]. Various classifications, such as the Neri classification [5], have been proposed to guide treatment options. In this case, we suggest that CABG is the optimal choice for coronary revascularization. However, the coronary perfusion strategy for intraoperative myocardial protection is the main challenge in achieving favourable surgical outcomes. Timely myocardial perfusion is crucial for preventing prolonged ischaemia. CABG cannot provide timely myocardial perfusion after aortic cross-clamping, and conventional myocardial perfusion methods may be inadequate. Conventional antegrade coronary perfusion was unable to deliver cardioplegia effectively, making retrograde perfusion a viable alternative. However, retrograde perfusion still presents the issue of inadequate myocardial protection for the right ventricle. In this case, where the coronary ostia had intact adventitia but severed intima, we achieved good results by using our patented perfusion tip for direct coronary ostium perfusion, ensuring timely and effective myocardial protection.
Conclusion
Based on our experience, surgeons should be vigilant when CT images present similar findings. Our coronary perfusion method, which has been effectively applied and proven feasible, can serve as a valuable alternative measure in such patients.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- TAAD:
-
Type A Aortic Dissection
- CABG:
-
Coronary Artery Bypass Grafting
- AMI:
-
Acute Myocardial Infarction
References
Kreibich M, Bavaria JE, Branchetti E, et al. Management of patients with coronary artery Malperfusion secondary to type A aortic dissection. Ann Thorac Surg. 2019;107(4):1174–80.
Uchida K, Karube N, Minami T, et al. Treatment of coronary malperfusion in type a acute aortic dissection. Gen Thorac Cardiovasc Surg. 2018;66(11):621–5.
Imoto K, Uchida K, Karube N, et al. Risk analysis and improvement of strategies in patients who have acute type a aortic dissection with coronary artery dissection. Eur J Cardiothorac Surg. 2013;44(3):419–25.
Sun LZ, Qi RD, Chang Q, et al. Surgery for acute type a dissection using total arch replacement combined with stented elephant trunk implantation: experience with 107 patients. J Thorac Cardiovasc Surg. 2009;138(6):1358–62.
Neri E, Toscano T, Papalia U, et al. Proximal aortic dissection with coronary malperfusion: presentation, management, and outcome. J Thorac Cardiovasc Surg. 2001;121(3):552–60.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Ling-chen Huang and Zeng-bin Feng contributed equally to this work and share the first authorship. Ling-chen Huang wrote the main manuscript text and Ling-chen Huang and Zeng-bin Feng prepared Figs. 1, 2 and 3. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Video 1. Surgical examination of the right coronary ostium, while using our patented designed cannula tip to administer cardioplegia.
Supplementary Material 2: Video 2. Postoperative CT examination revealed that the saphenous vein graft was patency.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, Lc., Feng, Zb. & Guo, Hw. Uncommon presentation of acute type A aortic dissection: sleeve-severed and everted proximal right coronary artery intima without myocardial ischaemia. J Cardiothorac Surg 19, 538 (2024). https://doi.org/10.1186/s13019-024-03040-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-03040-y