Abstract
Objectives
Intracranial pressure (ICP) monitoring is recommended for severe traumatic brain injuries (TBI) but some data suggests it may not improve outcomes. The objective was to investigate the effect of ICP monitoring among TBI.
Methods
This retrospective observational cohort study (1/1/2015–6/1/2020) included severe TBI patients. Outcomes [discharge destination, length of stay (LOS)] were compared by ICP monitoring and were stratified by GCS (3 vs. 4–8), α < 0.05.
Results
Of the123 patients who met inclusion criteria, 47% received ICP monitoring. There were baseline differences in the two groups characteristics, ICP monitored patients were younger (p = 0.02), had a subarachnoid hemorrhage less often (p = 0.04), and a subdural hematoma more often (p = 0.04) than those without ICP monitors. ICP monitored patients had a significantly longer median LOS (12 vs. 3, p < 0.01) than patients without monitoring. There was a trend towards more ICP monitored patients discharged home (40% vs. 23%, p = 0.06). Among patients with GCS = 3, ICP monitored patients had a longer LOS (p < 0.01) with no significant differences in discharge destinations. For those with a GCS of 4–8, ICP monitoring was associated with a longer LOS (p = 0.01), but fewer were discharged to a skilled nursing facility or long-term care (p = 0.01).
Conclusions
For TBI patients, ICP monitoring was associated with an increased LOS, with no significant differences in discharge destinations when compared to those without ICP monitoring. However, among only those with a GCS of 4–8, ICP monitoring was associated with a decreased proportion of patients discharged to a skilled nursing facility or long-term acute care .
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Severe traumatic brain injury (TBI) management focuses on preventing secondary insults [1]. The Brain Trauma Foundation severe TBI guideline recommends treatment guided by monitoring modalities including intracranial pressure (ICP) monitors [2]. They state that Level 2B evidence shows ICP monitoring may reduce mortality rates [2]. The Brian Injury Guideline, recommends that severe TBIs, categorized as Brain Injury Guideline 3, receive repeat imaging, a neurosurgeon consultation, and are admitted to the hospital, but have no ICP monitoring recommendations [3].
There is conflicting evidence on ICP monitoring efficacy for improving morbidity and mortality [4,5,6,7,8,9,10,11]. Differing results may be attributable to subsequent treatments used due to ICP monitoring results [2]. ICP monitoring is recommended for patients with a Glasgow Coma Scale (GCS) ≤ 8 and an abnormal head computed tomography (CT) [2]. It is possible that patients with GCS = 3 may be skewing the mortality rate of ICP monitoring; one study of ICP monitored patients with GCS = 3 reported a mortality rate of 49%, another of ICP monitored patients with GCS 3–8 reported a mortality rate of 24% [9, 12]. Although many studies examined the effect of ICP placement, there is little evidence on the role of GCS. The study purpose was to 1) compare the effect of ICP monitoring among TBI patients on outcomes providing additional evidence on its efficacy, and 2) to further stratify results by GCS. The hypothesis was that there would be no differences in outcomes by ICP monitoring overall, nor for those with a GCS = 3, but ICP placement would improve outcomes for those with a GCS of 4–8.
Methods
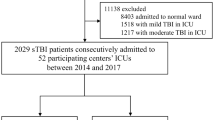
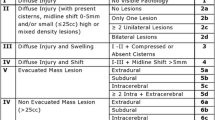
This was a retrospective observational cohort study comparing severe TBI patients who received ICP monitoring to those who did not at a Level II trauma center. Severe TBI was defined as having an admission GCS ≤ 8 and Brain Injury Guidelines 3 classification per imaging characteristics [subdural hematoma (SDH) > 8 mm, epidural hematoma (EDH) > 8 mm, intra-parenchymal hematoma (IPH) > 8 mm and multiple locations, scattered subarachnoid hemorrhage (SAH), and intraventricular hemorrhage (IVH)] [3]. Included patients were enrolled consecutively over a 5.5-year period starting on 01/01/2015 and ending on 06/01/2020. Additional selection criteria were as follows. Blunt and penetrating injuries were included, burn patients were excluded. Patients could have suffered an isolated TBI or poly-trauma. There were no exclusions applied based on age. The Western Investigational Review Board approved of this study with a waiver of consent. Data were collected from the trauma registry and electronic medical records. ICP monitors were placed at the trauma surgeon’s discretion.
The primary outcome was discharge destination, which was categorized as: in-hospital mortality, home, rehabilitation, or skilled nursing facility/long-term acute care. Secondary outcomes included hospital length of stay (LOS), intensive care unit length of stay (intensive care unit LOS), total ventilator days, and pneumonia. Outcomes were collected from the trauma registry. Fisher’s exact test and Chi-squared test were used to compare categorical or dichotomous data, which were summarized as proportion (count). Kruskal Wallis or Student’s t-tests were used to compare continuous variables based on the distribution of the data. Continuous variables were summarized as median with interquartile range, when non-parametric, and means with standard deviation, when parametric. In a post-hoc analysis of these outcomes, the average power was 85%. Because of the effect of GCS on mortality in previous studies, a stratified analysis was conducted based on the GCS (3 vs. 4–8). A significance level of α < 0.05 and Statistical Analysis System v9.4 (Cary, North Carolina) were used for all analyses.
Results
A total of 123 patients met the selection criteria. Of those 47% received ICP monitoring and 53% did not. Overall, the median age was 43 and 34% were female, Table 1. Regarding the patient’s demographics, those with ICP monitoring were significantly younger (p = 0.02) than those without ICP monitoring. Other demographics were similar between groups; there were no differences in gender (p = 0.96), race (p = 0.20), or ethnicity (p > 0.99). The severity of patients’ injuries measured through the GCS (p = 0.48) and Injury Severity Scale (ISS) (p = 0.91) were also comparable by ICP monitoring.
There were observed differences in the hemorrhage type by ICP monitoring. There was a lower proportion of ICP monitored patients with a SAH (50% vs 66%, p = 0.04), and a higher proportion with a SDH (74% vs. 54%, p = 0.04), when compared to those without ICP monitoring, Table 2. Other types of bleeds were similar. There was no difference in the proportion of skull fractures (p = 0.14). There was a significantly higher proportion of ICP monitored patients who had a craniotomy (48% vs. 12%, p < 0.0001), craniectomy (38%, vs 3%, p < 0.0001), tracheostomy (40% vs. 15%, p = 0.004), or gastrointestinal tube placed (40% vs. 17%, p = 0.01) when compared to those without ICP monitoring. Of the ICP monitored patients, 56% needed an external ventricular drain, 22% needed a bolt, and 5% needed a different type of drain.
There was a trend towards having a significantly higher proportion of ICP monitored patients discharged home (40% vs 23%, p = 0.06) when compared to patients without ICP monitoring, Table 3. Other discharge destinations, including mortality, were comparable. A higher proportion of ICP monitored patients had pneumonia (28% vs. 3%, p = 0.0002) than patients without ICP monitoring. There were no deaths among patients with pneumonia, in fact patients with pneumonia who had ICP monitoring were more often discharged home than those without ICP monitoring (26% vs. 9%, p = 0.01). ICP monitored patients had a significantly longer intensive care unit LOS (11 vs 3, p = 0.0001), total ventilator days (6 vs 2, p < 0.0001), and LOS (12 vs 3, p < 0.0001) than patients without ICP monitoring.
In a stratified analysis of only patients with a GCS = 3, ICP monitoring was still associated with a significantly higher rate of pneumonia (p = 0.01), a significantly longer intensive care unit LOS (p = 0.002), ventilator days (p = 0.0002), and LOS (p = 0.001) when compared to patients without ICP monitoring, Table 4. Among patients with a GCS of 4–8, ICP monitoring was still associated with a significantly higher rate of pneumonia (p = 0.03), and longer LOS (p = 0.01); but intensive care unit LOS (p = 0.08) and ventilator days (p = 0.07) were only trending towards being significantly longer when compared to those without ICP monitoring. There was a significantly lower proportion of patients with a GCS of 4–8 and ICP monitoring who were discharged to a skilled nursing facility or long-term acute care when compared to those without ICP monitoring (p = 0.01) and there was also a trend towards a higher proportion of ICP monitored patients being discharged home (p = 0.09) than patients without ICP monitoring.
Discussion
Based on this observational study, TBI patients with ICP monitoring may have an extended intensive care unit LOS, LOS, ventilator days and a higher rate of pneumonia. Discharge destinations were generally improved with ICP monitoring but this association was dependent on GCS. For patients with a GCS of 4–8 there was a significantly lower proportion of ICP monitored patients discharged to a skilled nursing facility or long-term acute care and a trend towards a higher proportion of ICP monitored patients discharged home when compared to those without ICP monitoring. Whereas for those with a GCS = 3, there were no significant associations with the discharge destination.
Like this study, previous studies found ICP monitoring did not impact mortality [10, 11, 13]. Others observed lower mortality rates with ICP monitoring [5, 6]. Some studies have found a higher mortality with ICP monitoring [8, 9, 14]. Lane et al. found that after controlling for ISS and mechanism, ICP monitoring was associated with improved survival [4]. In this study there were no differences in the initial ISS, GCS, or mortality.
In contrast to this study, Tang et al. found a significantly lower proportion of ICP monitored patients discharged home [9]. While there was an association between patients with a GCS of 4–8 and improved discharge destinations with ICP monitoring, there were no differences observed among patients with GCS = 3. Lane et al. reported that the head abbreviated injury scale score was significantly associated with in-hospital mortality, where patients with the worst scores were more likely to die in-hospital [4]. In a study of pediatric patients who had an ICP placed, GCS = 3 also significantly increased in-hospital mortality [15].
ICP monitoring was associated with a significantly longer LOS, intensive care unit LOS, and ventilator days in this study, which could be due to the Brain Trauma Foundation recommendations on further treatment based on ICP results [2]. Additional studies have observed longer stays and ventilator days with ICP monitoring [5, 7, 8, 11, 14]. While Haddad et al. saw no difference in LOS [13]. In this study, patients with GCS = 3 experienced significantly longer intensive care unit LOS, ventilator days, and LOS with ICP monitoring; whereas for those with a GCS of 4–8 there was no significant difference in the intensive care unit LOS or ventilator days, but a significantly longer LOS with ICP monitoring.
Two other studies also observed that patients with an ICP monitor were more likely to have pneumonia [11, 13]. One possible explanation for this could be the increased ventilator days, or increased use of invasive treatments among ICP monitored patients. Among the patients with pneumonia, there were no deaths.
There were notable differences between the groups. ICP monitored patients were younger, which has been previously reported [5, 8, 11, 14]. Like other studies, the majority of ICP monitored patients had neurosurgical interventions, likely due to recommendations that ICP monitoring be used to guide treatment [2, 5, 8, 14]. Other studies reported no difference in the hemorrhage type by ICP monitoring but in this study ICP monitored patients had significantly more SDHs and less SAHs [6, 9, 16].
Limitations
This was a single-center retrospective study with a small sample size that limited the ability to conduct propensity matching or adjusted modeling and may not be generalizable. Factors related to the ICP monitor (indication, drainage volumes, etc.) were not collected. The procedure date/times were not collected so we could not determine if procedures occurred after ICP placement. There was no long-term follow-up. There was not a protocol followed by all treating physicians guiding ICP monitoring, therefore these results may not be generalizable to centers utilizing an existing protocol. Implementation of a protocol guiding ICP monitoring may result in different outcomes than seen in this study.
Conclusions
This study observed that for TBI patients ICP monitoring may be associated with a higher rate of pneumonia, an increased intensive care unit LOS, ventilator days, and LOS, with no difference in the discharge destinations, including the mortality rate, when compared to those without ICP monitoring at a Level II trauma center without a protocol guiding ICP monitoring. While ICP monitoring may not improve outcomes across all patients, select patients may have improved discharge destinations, despite longer LOS. Among those with a GCS of 4–8, ICP monitoring was associated with a significant decrease in the proportion of patients discharged to a skilled nursing facility or long-term acute care when compared to those without an ICP monitor.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available, as they were compiled from our own patient records, but data and coding methodology are available from the corresponding author on reasonable request.
Abbreviations
- TBI:
-
Severe traumatic brain injury
- ICP:
-
Intracranial pressure
- GCS:
-
Glasgow Coma Scale
- CT:
-
Computed tomography
- SDH:
-
Subdural hematoma
- EDH:
-
Epidural hematoma
- IPH:
-
Intra-parenchymal hematoma
- SAH:
-
Subarachnoid hemorrhage
- IVH:
-
Intraventricular hemorrhage
- LOS:
-
Hospital length of stay, intensive care unit
- ISS:
-
Injury Severity Scale
References
Vella MA, Crandall ML, Patel MB. Acute Management of Traumatic Brain Injury. Surg Clin North Am. 2017;95(5):1015–30.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GWJ, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, Fourth edition. Neurosurgery. 2017;80:6–15.
Joseph B, Friese RS, Sadoun M, Aziz H, Kulvatunyou N, Pandit V, et al. The BIG (brain injury guidelines) project: defining the management of traumatic brain injury by acute care surgeons. J Trauma Acute Care Surg. 2014;76(4):965–9.
Lane PL, Skoretz TG, Doig G, Girotti MJ. Intracranial pressure monitoring and outcome after traumatic brain injury. JCC. 2000;43(6):442.
al Saiegh F, Philipp L, Mouchtouris N, Chalouhi N, Khanna O, Shah SO, et al. Comparison of outcomes of severe traumatic brain injury in 36,929 patients treated with or without intracranial pressure monitoring in a mature trauma system. World Neurosurg. 2020;136:e535–41 Elsevier Inc.
Alali AS, Fowler RA, Mainprize TG, Scales DC, Kiss A, de Mestral C, et al. Intracranial pressure monitoring in severe traumatic brain injury: results from the american college of surgeons trauma quality improvement program. J Neurotrauma. 2013;30:1737–46.
Talving P, Karamanos E, Teixeira PG, Skiada D, Lam L, Belzberg H, et al. Intracranial pressure monitoring in severe head injury: compliance with Brain Trauma Foundation guidelines and effect on outcomes: a prospective study. J Neurosurg. 2013;119:1248–54.
Ahl R, Sarani B, Sjolin G, Mohseni S. The Association of Intracranial Pressure Monitoring and Mortality: a propensity score-matched cohort of isolated severe blunt traumatic brain injury. J Emerg Trauma Shock. 2019;12:18–22.
Tang A, Pandit V, Fennell V, Jones T, Joseph B, O’Keeffe T, et al. Intracranial pressure monitor in patients with traumatic brain injury. J Surg Res. 2015;194:565–70 Academic Press Inc.
Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367:2471–81 Massachusetts Medical Society.
Aiolfi A, Benjamin E, Khor D, Inaba K, Lam L, Demetriades D. Brain Trauma Foundation guidelines for intracranial pressure monitoring: compliance and effect on outcome. World J Surg. 2017;41:1543–9 Springer New York LLC.
Chamoun RB, Robertson CS, Gopinath SP. Outcome in patients with blunt head trauma and a Glasgow coma scale score of 3 at presentation: clinical article. J Neurosurg. 2009;111:683–7.
Haddad S, Aldawood AS, Alferayan A, Russel NA, Tamim HM, Arabi YM. Relationship between intracranial pressure monitoring and outcomes in severe traumatic brain injury patients. Anaesth Intensive Care. 2011;39:1043–50.
Dang Q, Simon J, Catino J, Puente I, Habib F, Zucker L, et al. More fateful than fruitful? Intracranial pressure monitoring in elderly patients with traumatic brain injury is associated with worse outcomes. J Surg Res. 2015;198:482–8 Academic Press Inc.
Murphy S, Thomas NJ, Gertz SJ, Beca J, Luther JF, Bell MJ, et al. Tripartite stratification of the Glasgow coma scale in children with severe traumatic brain injury and mortality: an analysis from a multi-center comparative effectiveness study. J Neurotrauma. 2017;34:2222–9 Mary Ann Liebert Inc.
Jha RM, Elmer J, Zusman BE, Desai S, Puccio AM, Okonkwo DO, et al. Intracranial pressure trajectories: a novel approach to informing severe traumatic brain injury phenotypes. Crit Care Med. 2018;46:1792–802 Lippincott Williams and Wilkins.
Acknowledgments
We would like to acknowledge the McAllen Medical Center administration, the Trauma department, and Touro University for support of this project.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JG, AB, SJ, DBO, and CHP contributed to the concept and design of the study. XD and CHP acquired the data for the study, SJ and JCV conducted the data analysis and interpretation. CF wrote the initial manuscript draft, SJ, XD, JG, BC, CV, AB, DBO, & CHP contributed to the critical revisions of the manuscript and provided approval to submit. While the authors are affiliated with five institutions, data used in this study was solely from McAllen Medical Center. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved Western (WCG) IRB (study #1321106) with a waiver of consent.
Consent for publication
Waiver of consent was obtained via Western (WCG) IRB. All authors have read and approved of this paper for publication.
Competing interests
The authors declare that they have no competing interests. The opinions or assertions contained herein are the private views of the authors and do not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Foote, C.W., Jarvis, S., Doan, XL. et al. Correlation between intracranial pressure monitoring for severe traumatic brain injury with hospital length of stay and discharge disposition: a retrospective observational cohort study. Patient Saf Surg 16, 40 (2022). https://doi.org/10.1186/s13037-022-00350-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-022-00350-9