Abstract
Background
To evaluate the impact of implementation of 2019 European respiratory distress syndrome (RDS) guidelines on the incidence of bronchopulmonary dysplasia (BPD).
Method
We retrospectively collected the clinical data of very preterm infants (VPIs) born before 32 gestational weeks from January 1st 2018 to December 31st 2021. VPIs were divided into group A and group B according to their birth date which was before or at/after January 1st 2020, when the 2019 European RDS guidelines were introduced. BPD is considered as primary outcome. We statistically analyzed all the data, and we compared the general characteristics, ventilation support, medication, nutrition and the outcomes between the two groups.
Results
A total of 593 VPIs were enrolled, including 380 cases in group A and 213 cases in group B. There were no statistic differences regarding to gender ratio, gestational age, birth weight and delivery mode between the two groups. Compared with group A, group B showed higher rate of antenatal corticosteroid therapy (75.1% vs. 65.5%). The improvement of ventilation management in these latter patients included lower rate of invasive ventilation (40.4% vs. 50.0%), higher rate of volume guarantee (69.8% vs. 15.3%), higher positive end expiratory pressure (PEEP) [6 (5, 6) vs. 5 (5, 5) cmH2O] and higher rate of synchronized nasal intermittent positive pressure ventilation (sNIPPV) (36.2% vs. 5.6%). Compared with group A, group B received higher initial dose of pulmonary surfactant [200 (160, 200) vs. 170 (130, 200) mg/Kg], shorter antibiotic exposure time [13 (7, 23) vs. 17 (9, 33) days], more breast milk (86.4% vs. 70.3%) and earlier medication for hemodynamically significant patent ductus arteriosus (hsPDA) treatment [3 (3, 4) vs. 8 (4, 11) days] (p < 0.05). As the primary outcome, the incidence of BPD was significantly decreased (16.9% vs. 24.2%) (p < 0.05), along with lower extrauterine growth retardation (EUGR) rate (39.0% vs. 59.7%), while there were no statistic differences regarding to other secondary outcomes, including mortality, intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), retinopathy of preterm (ROP) and necrotizing enterocolitis (NEC). However, in the subgroups of infants less than 28 gestational weeks or infants less than 1,000 g, the incidence of BPD was not significantly decreased (p > 0.05).
Conclusions
After implementation of 2019 European RDS guidelines, the overall incidence of BPD was significantly decreased in VPIs. Continuous quality improvement is still needed in order to decrease the incidence of BPD in smaller infants who are less than 28 gestational weeks or less than 1,000 g.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Following the improvement of antenatal-perinatal medicine, maternal and child healthcare, neonatal resuscitation skills and integrated preterm management, the survival rate of preterm infants has significantly increased in the last 30 years worldwide [1,2,3]. Unfortunately, some of the very preterm infants (VPIs) who are delivered before 32 gestational weeks may develop different kinds of on-going problems, including bronchopulmonary dysplasia (BPD), the most common and severe respiratory complication of VPIs [4], which is notably associated with poor neurodevelopmental outcomes [5]. According to data from Chinese Neonatal Network (CHNN), the overall incidence of BPD in Chinese VPIs is about 29.2% [6]. However, in extremely preterm infants (EPIs) less than 28 gestational weeks the incidence of BPD could be significantly higher [7].
European consensus guidelines on management of respiratory distress syndrome (RDS) were published in 2007 for the first time and have been updated every 3 years for several times [8]. They were translated into Chinese and published in national medical journal, to provide theoretical and practical guidance for Chinese neonatologists to manage preterm infants at early stage postnatally. However, due to uneven economic conditions and medical resources, there is wide variation of preterm care practices and subsequent neonatal outcomes in different regions in China [9].
As one of the participants of CHNN [10], we have been improving our institutional management of VPIs within the quality improvement structure of the national network based on our own fundamental conditions. In accordance with 2019 updated version of European RDS guidelines [11] and domestic literature recommendations, we modified and initiated our protocol of VPIs management since January 2020, including ventilation support, medication, nutrition, treatment of patent ductus arteriosus (PDA) and so on. This study is aiming to analyze the impact of the modified practices on the incidence of BPD and other neonatal outcomes.
Patients and methods
Study design and objects
Inclusion criteria: All of the infants born less than 32 gestational weeks admitted to the Department of Neonatology in Shanghai Children’s Hospital from January 1st 2018 to December 31st 2021 were screened for this retrospective single-center cohort study.
The exclusion criteria were: (1) early death within 14 days after birth, because these patients could not be diagnosed with BPD based on the definition, (2) withdrawing medical support or discharge against medical advice (DAMA) within 14 days after birth, (3) admission after 14 days after birth, (4) complex congenital heart disease, chromosomal abnormality or gene mutation which may impact long-term outcomes, (5) repeated admission after discharge.
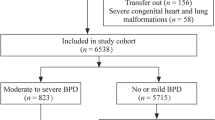
Enrolled infants were divided into group A and group B according to their birth date, which was before or at/after January 1st 2020 when the 2019 European RDS guidelines were introduced, respectively. Data including maternal history, gestational age (GA), birth weight (BW), postnatal management, main inspection results and outcomes were collected (Fig. 1).
The institutional management protocol of VPIs was modified and initiated since January 1st 2020. The main changes were based on European consensus guidelines on management of RDS which were published in 2019, including improvement of ventilation management, administration of pulmonary surfactant (PS), nutrition, medication for infection, sedation and PDA management. All the data were statistically analyzed, and the general characteristics, ventilation support, medication, nutrition and the outcomes between the two groups were compared.
Ethics
This study was reviewed and approved by ethic committee of Shanghai Children’s Hospital in accordance with the Declaration of Helsinki (approval number: 2021R013-E01). All the parents of enrolled patients read and signed the informed consent at admission that their children’s clinical data other than their personal information might be used for clinical statistical analysis for publication.
Primary outcome
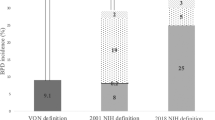
BPD was considered as the primary outcome for this cohort. Due to lack of universal diagnostic criteria, different studies may use different definitions and classifications to diagnose BPD. It is reported that different standards of diagnosis for BPD could impact the statistical result [12,13,14]. Based on our clinical practices and understanding to BPD, we adopted the 2018 revised BPD definition proposed by the National Institute of Child Health and Human Development (NICHD) in this retrospective cohort study [15] (supplementary material 1).
Secondary outcomes
The secondary outcomes included death, intraventricular hemorrhage (IVH) (grade ≥ 3), periventricular leukomalacia (PVL), retinopathy of prematurity (ROP) (stage ≥ 3 or any need for intervention), necrotizing enterocolitis (NEC) (stage ≥ 2) and extrauterine growth restriction (EUGR).
IVH was defined as equal to or greater than grade 3 according to Papile criteria [16]. PVL was defined as presence of periventricular cysts either identified by cranial ultrasound or magnetic resonance imaging (MRI). ROP was defined as equal to or greater than stage 3 or any need for intervention according to International Classification of Retinopathy of Prematurity [17]. NEC was defined as equal to or greater than stage 2 according to modified Bell’s staging criteria [18]. EUGR was defined as the Z score of body weight at the time of discharge decreased > 1.0 compared to which at the time of birth.
Other definitions
Admission hypothermia was defined as axillary temperature < 36.0 Celsius degree at admission. Prolonged premature rupture of membrane (PPROM) was defined as membrane rupture ≥ 18 h before delivery. Intensive resuscitation was defined as any demand of positive pressure ventilation, intubation, chest compression or epinephrine during birth resuscitation. High fraction of inspired oxygen (FiO2) demand was defined as FiO2 demand > 0.6 more than 6 h continuously at any time. Early onset sepsis was defined as clinically diagnosed or pathogen proven sepsis within 3 days after birth. Late onset sepsis was defined as clinically diagnosed or pathogen proven sepsis which occurred after 3 days after birth. Long-term sedation was defined as continuous sedation demand of fentanyl or midazolam for over 3 consecutive days. The definition of hemodynamically significant PDA (hsPDA) referred to literature published by Shepherd [19] (supplementary material 2).
Statistical analysis
Categorical variables were presented by percentages. All continuous variables received test for distribution. Continuous variables with normal distribution were expressed as mean ± standard deviation (SD). Continuous variables with non-normal distribution were described as median (Q1, Q3). χ2 test was performed for numeration data and independent-samples t test or Mann-Whitney U test was performed for measurement data. All the statistical analyses were performed using SPSS Statistics 27.0 (IBM, US). p < 0.05 was considered to indicate a statistically significant difference.
Results
General characteristics
A total of 593 VPIs were enrolled in this retrospective cohort study, including 380 cases in group A and 213 cases in group B. There was no statistic difference regarding to gender ratio, gestational age, birth weight, conception and delivery mode, and Apgar score at the 5th minute between the two groups (p > 0.05), while group B showed significantly higher rate of gestational diabetes mellitus (GDM) (17.3% vs. 11.6%), antenatal corticosteroid administration (75.1% vs. 65.5%) and magnesium sulfate therapy (68.1% vs. 50.8%), with lower rate of admission hypothermia (16.0% vs. 35.5%) (p < 0.05) (Table 1).
Risk factors of BPD
The overall incidence of BPD for the whole cohort was 21.6% (128/593). The risk factors of BPD included birth weight less than 1,000 g, gestational age less than 28 weeks, male gender, fetal growth restriction (FGR), intensive resuscitation, invasive mechanical ventilation (IMV), high FiO2 demand, hypercarbia, sepsis, surfactant demand, long-term sedation, feeding intolerance, hsPDA and EUGR, while Cesarean section seemed to be a protective factor for BPD (Table 2).
Postnatal management
Based on 2019 European consensus of BPD management guidelines, several changes were achieved in clinical practices for VPIs in group B compared with group A (Table 3). For respiratory support, IMV (40.4% vs. 50.0%), high flow nasal cannula (HFNC) (26.5% vs. 43.4%) and nasal high frequency oscillatory ventilation (nHFOV) (3.7% vs. 9.4%) were used less, volume guarantee (VG) (69.8% vs. 15.3%) and synchronized nasal intermittent positive pressure ventilation (sNIPPV) (36.0% vs. 5.3%) were used more with higher initial positive end expiratory pressure (PEEP) [6 (5, 6) vs. 5 (5, 6) cmH2O] or continuous positive airway pressure (CPAP) [6 (5, 6) vs. 5 (5, 5) cmH2O]. The overall rate of PS administration was similar, but the initial dose was higher in group B [200 (160, 200) vs. 170 (130, 200) mg/Kg], with a lower rate of long-term sedation (9.9% vs. 18.4%) and shorter antibiotics exposure time [13 (7, 23) vs. 17 (9, 33) days]. For nutrition management, group B showed higher rate of early initiation of enteral feeding, breast milk, donor milk and fortifier usage. For PDA management, the overall rate of medication or ligation for hsPDA was the same, but group B was treated earlier with more ibuprofen.
Outcomes
The incidence of BPD was significantly lower in group B, compared with group A (16.9% vs. 24.2%) (p < 0.05). However, there was no statistical difference regarding to severity of BPD between the two groups.
As for secondary outcomes, less infants in group B developed EUGR, while there was no statistical difference in mortality, incidence of IVH, PVL, ROP and NEC between the two groups (Table 4).
Subgroups comparison
After dividing patients into subgroups based on gestational weeks or birth weight, there was no significant difference of BPD in extremely preterm infants (EPIs) (GA < 28 weeks) or extremely low birth weight infants (ELBW) (BW < 1,000 g) (Table 5).
Discussion
BPD is a major complication which impacts the long-term outcomes of VPIs. One of the most important tasks for neonatologists to manage VPIs is aiming to reduce the incidence of BPD and subsequent neurodevelopment disorders. For this purpose, we adopted 2019 European consensus of RDS management guidelines and improved our clinical practices since January 2020, including optimized respiratory support and medication use, improved nutrition management and timely intervention for hsPDA. As a result, the overall incidence of BPD in VPIs was decreased significantly (16.9% vs. 24.2%).
It is well known that smaller gestation age and lower birth weight are high risk factors of BPD. In a previous study, it was reported that oxygen during resuscitation, surfactant demand, NIPPV, IMV, HFOV, PDA and nosocomial sepsis were also associated with BPD in preterm infants born at or less than 32 weeks of gestation [20]. In addition, higher FiO2 demand and maximum mean airway pressure (MAP) were reported as risks of BPD in EPIs [21]. In our cohort, we also found that BPD is significantly associated with FGR, long-term sedation, feeding intolerance and EUGR. FGR is considered as a pattern of fetal programming which could impact the long-term outcomes [22]. It is reported that FGR could increase the incidence of BPD with hypothesis of mechanistic link between fetal programming and vascular architecture and mechanics [23]. Antenatal corticosteroid exposure is considered to decrease mortality rate in EPIs, but the rate of BPD in survivors did not differ [24]. In our cohort, we also found that BPD was not associated with antenatal corticosteroid exposure. However, it is obvious that the rate of antenatal corticosteroid treatment in our preterm population had been increasing over recent years (75.1% vs. 65.5%), although it is still lower than the number reported in high-income countries which is usually over 90%.
In order to decrease the incidence of BPD, we modified our protocol of management of VIPs in accordance with 2019 European RDS guidelines. Protective ventilation strategy is essential to protect fragile lungs of VPIs from pulmonary volutrauma and barotrauma. It has been proven that prophylactic nasal CPAP in very preterm infants can reduce the incidence of BPD compared to mechanical ventilation [25]. NIPPV could reduce incidence of extubation failure and need for reintubation, although it has no effect on BPD or mortality [26]. In addition, synchronization is very important to use NIPPV. If neonates need mechanical ventilation, volume targeted ventilation mode could reduce the rate of death or BPD, pneumothoraces, hypocarbia, severe neurological outcomes and duration of ventilation, compared with pressure limited ventilation mode [27]. Elective HFOV could slightly reduce the risk of BPD compared with conventional ventilation, but the evidence is weak due to inconsistency in the different studies [28]. Therefore, based on above evidence and combined with 2019 European RDS guidelines, we optimized our ventilation strategy in VPIs. The overall rate of IMV was decreased (40.4% vs. 50%). Most infants who needed mechanical ventilation were put on VG mode (69.8% vs. 15.3%) with a higher initial PEEP [6 (5, 6) vs. 5 (5, 6) cm H2O]. For non-invasive ventilation mode, sNIPPV was used more (36% vs. 5.3%), while HFNC (26.5% vs. 43.4%) and nHFOV (3.7% vs. 9.4%) were used less. New evidence for better ventilation strategies continuously emerges overtime. Zhu et al. [29] reported that both nHFOV and NIPPV could lower the risk of reintubation compared with CPAP, while they did not find any difference in BPD within those 3 groups. The latest Cochrane Database systemic review pointed out that early NIPPV may reduce the risk of respiratory failure, the need for intubation and the rate of BPD in preterm infants with a gestational age of 28 to 32 weeks [30]. It reminds us that we should continuously optimize our ventilation strategies based on current evidence in order to improve the pulmonary outcomes of VPIs.
Rational medication for VPIs is also important. It has been around 30 years since exogenous PS was introduced to Chinese neonatologists, which saved many lives of preterm infants who might die of RDS. Based on the Cochrane review published in 2015 [31], 2019 European RDS guidelines recommended that porcine sourced PS with an initial dose of 200 mg/kg is better for RDS rescue therapy. Hence, we increased the initial dosage of PS administration in VPIs [200 (160, 200) vs. 170 (130, 200) mg/Kg]. A recent retrospective study found that switching initial dose of PS from 100 mg/kg to 200 mg/kg was associated with a marked reduction of BPD [32]. Empiric antibiotic therapy is considered as a risk factor of BPD in VLBW infants [33]. Therefore, we improved our antibiotics stewardship and significantly decreased the antibiotic exposure time of VPIs [13 (7, 23) vs. 17 (9, 33) days]. Routine use of sedation in VPIs on mechanical ventilation is not recommended [11]. Thereupon, we decreased the use of long-term sedation of fentanyl or midazolam in VPIs (9.9% vs. 18.4%). In respect of other medications, there was no significant difference in the use of caffeine, postnatal steroid and diuretics between the two groups.
Nutrition is another crucial part of management of VPIs. Breast milk is always considered as the best food source for neonates. A systematic review indicated that use of exclusive mother’s own milk feedings was associated with a significant reduction in the risk of BPD in very preterm infants [34]. Another systematic review suggested that donor milk was also effective to protect against BPD [35]. In 2016, our hospital established the first charitable donor milk bank in Shanghai. Due to the benefit from the support of donor milk bank, we are able to provide appropriate enteral nutrition to VPIs in the early stage of life. The improvement of nutrition management of VPIs in our clinical practice included higher rate of breast milk feeding (86.4% vs. 71.6%), donor milk feeding (92.5% vs. 84.5%), human milk fortifier (86.4% vs. 72.9%) and early enteral feeding within 24 h postnatally (83.6% vs. 71.6%). Above measures resulted in a significant reduction of EUGR (39.0% vs. 59.7%).
Whether, when or how to treat a PDA is still a tricky question to neonatologists. In general, hsPDA is considered to be a risk factor in the development of BPD [36]. Previous studies indicate that delaying pharmacologic PDA treatment for 2 ~ 3 days after birth does not increase the incidence of BPD, but delaying treatment after 1 week may be associated with an increase of BPD [37]. With regard to medication for PDA, a systematic review in 2018 pointed out that oral ibuprofen had same rate of PDA closure compared with intravenous indomethacin, along with a significant reduction of risk of NEC [38]. Paracetamol was reported as effective as ibuprofen for PDA closure but the evidence was not strong [39]. Therefore, we aimed to identify hsPDA and start intervention earlier in VPIs. The initiation time of medication for hsPDA was significant earlier in group B, compared with group A [3 (3, 4) vs. 8 (4, 11) days]. We also used more ibuprofen rather than paracetamol. Only 2 infants who failed with pharmacological PDA closure and suffered from persistent hemodynamic impact received ligation surgery in group B.
After we improved our clinical practice on ventilation management, medication, nutrition and PDA treatment based on 2019 European RDS management guidelines, the overall incidence of BPD in VPIs significantly decreased (16.9% vs. 24.2%), along with a lower incidence of EUGR (39% vs. 59.7%). There was no statistic significant difference in other outcomes, such as death, IVH, PVL, ROP and NEC. However, the severity of BPD did not differ. Meanwhile, around half of the smaller preterm infants who were less than 1,000 g or less than 28 gestational weeks still developed BPD despite of all the above quality improvement measures. It reminds us that continuous quality improvement is still needed to reduce the incidence of BPD in smaller preterm infants.
There are some limitations in this study. Firstly, as a children’s hospital without maternal settings, all the patients in our department are out-born. Improvement of antenatal care or resuscitation in the delivery room is outside of our jurisdiction. Secondly, BPD is a multifactorial disease, but some external environmental impacts are not discussed in this study, such as the influence of COVID which seriously impacted the overall birth rate and human resource in medical facilities. Lastly, as a single-center retrospective study, the number of extremely small infants was small, along with a portion of early death or withdrawing treatment cases, which may cause bias of the statistical analysis.
Conclusions
After implementation of 2019 European RDS guidelines, the overall incidence of BPD was significantly decreased in VPIs. Continuous quality improvement is still needed in order to decrease the incidence of BPD in smaller infants < 28 weeks or < 1,000 g.
Data availability
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
References
Cao G, Liu J, Liu M, Global. Reginal, and National Incidence and Mortality of neonatal Preterm Birth, 1990–2019. JAMA Pediatr. 2022;176(8):787–96. https://doi.org/10.1001/jamapediatrics.2022.1622.
Serra G, Miceli V, Albano S, et al. Perinatal and newborn care in a two years retrospective study in a first level peripheral hospital in Sicily (Italy). Ital J Pediatr. 2019;45(1):152. https://doi.org/10.1186/s13052-019-0751-6.
Serra G, Giuffre M, Piro E, et al. The social role of pediatrics in the past and present times. Ital J Pediatr. 2021;47(1):239. https://doi.org/10.1186/s13052-021-01190-6.
Tracy MK, Berkelhamer SK. Bronchopulmonary Dysplasia and Pulmonary outcomes of Prematurity. Pediatr Ann. 2019;48(4):e148–53. https://doi.org/10.3928/19382359-20190325-03.
Gallini F, Coppola M, De Rose DU, et al. Neurodevelopmental outcomes in very preterm infants: the role of severity of Bronchopulmonary Dysplasia. Early Hum Dev. 2021;152:105275. https://doi.org/10.1016/j.earlyhumdev.2020.105275.
Cao Y, Jiang S, Sun J, et al. Assessment of neonatal Intensive Care Unit practices, Morbidity, and Mortality among very Preterm infants in China. JAMA Netw Open. 2021;4(8):e2118904. https://doi.org/10.1001/jamanetworkopen.2021.18904.
Siffle C, Kistler KD, Lewis JFM, et al. Global incidence of bronchopulmonary dysplasia among extremely preterm infants: a systematic literature review. J Matern Fetal Neonatal Med. 2021;34(11):1721–31. https://doi.org/10.1080/14767058.2019.1646240.
Sweet D, Bevilacqua G, Carnielli V. at al. European consensus guidelines on the management of neonatal respiratory distress syndrome. J Perinat Med. 2007, 35(3):175 – 86. https://doi.org/10.1515/JPM.2007.048
Bai R, Jiang S, Guo J, et al. Variation of neonatal outcomes and Care practices for Preterm infants < 34 weeks’ Gestation in different regions of China: a Cohort Study. Front Pediatr. 2021;9:760646. https://doi.org/10.3389/fped.2021.760646.
Hei M, Li X, Shi Y, et al. Chinese neonatal network: a national protocol for collaborative research and quality improvement in neonatal care. BMJ Open. 2022;12(5):e051175. https://doi.org/10.1136/bmjopen-2021-051175.
Sweet DG, Carnielli V, Hallman M, et al. European Consensus guidelines on the management of respiratory distress syndrome – 2019 update. Neonatology. 2019;115(4):432–50. https://doi.org/10.1159/000499361.
Gomez Pomar E, Concina VA, Samide A, et al. Bronchopulmonary dysplasia: comparison between the two most used diagnostic criteria. Front Pediatr. 2018;6:397. https://doi.org/10.3389/fped.2018.00397.
Sun L, Zhang H, Bao Y, et al. Long-term outcomes of Bronchopulmonary Dysplasia under two different diagnostic criteria: a retrospective cohort study at a Chinese Tertiary Center. Front Pediatr. 2021;9:648972. https://doi.org/10.3389/fped.2021.648972.
Wang X, Lu YK, Wu YY, et al. Comparison of two novel diagnostic criteria for bronchopulmonary dysplasia in predicting adverse outcomes of preterm infants: a retrospective cohort study. BMC Pulm Med. 2023;23(1):308. https://doi.org/10.1186/s12890-023-02590-6.
Higgins RD, Jobe AH, Koso-Thomas M, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8. https://doi.org/10.1016/j.jpeds.2018.01.043.
Papile LA, Burstein J, Burstein R, et al. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529–34. https://doi.org/10.1016/s0022-3476(78)80282-0.
International Committee for the Classification of Retinopathy of Prematurity. The International classification of retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123(7):991–9. https://doi.org/10.1001/archopht.123.7.991.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33(1):179–201. https://doi.org/10.1016/s0031-3955(16)34975-6.
Shepherd JL, Noori S. What is a hemodynamically significant PDA in preterm infants? Congenit Heart Dis. 2019;14(1):21–6. https://doi.org/10.1111/chd.12727.
Sucasas Alonso A, Pértega Diaz S, Sáez Soto R, et al. Epidemiology and risk factors for bronchopulmonary dysplasia in preterm infants born at or less than 32 weeks of gestation. Pediatr (Engl Ed). 2022;96(3):242–51. https://doi.org/10.1016/j.anpede.2021.03.006.
Geetha O, Rajadurai VS, Anand AJ, et al. New BPD-prevalence and risk factors for bronchopulmonary dysplasia/mortality in extremely low gestational age infants ≤ 28 weeks. J Perinatol. 2021;41(8):1943–50. https://doi.org/10.1038/s41372-021-01095-6.
Piro E, Serra G, Schierz I, et al. Fetal growth restriction: a growth pattern with fetal, neonatal and long-term consequences. EuroMediterranean Biomedical J. 2019;14(9):038–44. https://doi.org/10.3269/1970-5492.2019.14.09.
Sehgal A, Gwini SM, Menahem S, et al. Preterm growth restriction and bronchopulmonary dysplasia: the vascular hypothesis and related physiology. J Physiol. 2019;597(4):1209–20. https://doi.org/10.1113/JP276040.
Travers CP, Carlo WA, McDonald SA, et al. Mortality and pulmonary outcomes of extremely preterm infants exposed to antenatal corticosteroids. Am J Obstet Gynecol. 2018;218(1):130e. 1-130.e13.
Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2016;6CD001243. https://doi.org/10.1002/14651858.CD001243.pub3.
Lemyre B, Davis PG, De Paoli AG, et al. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (CPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. 2017;2(2):CD003212. https://doi.org/10.1002/14651858.CD003212.pub3.
Klingenberg C, Wheeler KI, McCallion N, et al. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10(10):CD003666. https://doi.org/10.1002/14651858.CD003666.pub4.
Cools F, Offringa M, Askie LM. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev. 2015;3CD000104. https://doi.org/10.1002/14651858.CD000104.pub4.
Zhu X, Qi H, Feng Z, et al. Noninvasive high-frequency Oscillatory Ventilation vs nasal continuous positive Airway pressure vs nasal intermittent positive pressure ventilation as Postextubation Support for Preterm neonates in China: a Randomized Clinical Trial. JAMA Pediatr. 2022;176(6):551–9. https://doi.org/10.1001/jamapediatrics.2022.0710.
Lemyre B, Deguise MO, Benson P, et al. Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev. 2023;7(7):CD005384. https://doi.org/10.1002/14651858.CD005384.pub3.
Singh N, Halliday HL, Stevens TP, et al. Comparison of animal-derived surfactants for the prevention and treatment of respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2015;12CD010249. https://doi.org/10.1002/14651858.CD010249.pub2.
Lanciotti L, Correani A, Pasqualini M, et al. Respiratory distress syndrome in preterm infants of less than 32 weeks: what difference does giving 100 or 200 mg/kg of exogenous surfactant make? Pediatr Pulmonol. 2022;57(9):2067–73. https://doi.org/10.1002/ppul.25979.
Cantey JB, Huffman LW, Subramanian A et al. Antibiotic Exposure and Risk for Death or Bronchopulmonary Dysplasia in Very Low Birth Weight Infants. J Pediatr. 2017;181:289–293. https://doi.org/10.1016/j.jpeds.2016.11.002.
Villamor-Martinez E, Pierro M, Cavallaro G, et al. Mother’s Own Milk and Bronchopulmonary Dysplasia: A Systematic Review and Meta-Analysis. Front Pediatr. 2019;7:224. https://doi.org/10.3389/fped.2019.00224.
Villamor-Martinez E, Pierro M, Cavallaro G, et al. Donor Human milk protects against Bronchopulmonary Dysplasia: a systematic review and Meta-analysis. Nutrients. 2018;10(2):238. https://doi.org/10.3390/nu10020238.
Willis KA, Weems MF. Hemodynamically significant patent ductus arteriosus and the development of bronchopulmonary dysplasia. Congenit Heart Dis. 2019;14(1):27–32. https://doi.org/10.1111/chd.12691.
Clyman RI. Patent ductus arteriosus, its treatments, and risks of pulmonary morbidity. Semin Perinatol. 2018;42(4):235–42. https://doi.org/10.1053/j.semperi.2018.05.006.
Ohlsson A, Walia R, Shah SS. Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev. 2018;9(9):CD003481. https://doi.org/10.1002/14651858.CD003481.pub7.
Ohlsson A, Shah PS. Paracetamol (acetaminophen) for patent ductus arteriosus in preterm or low birth weight infants. Cochrane Database Syst Rev. 2018;4(4):CD010061. https://doi.org/10.1002/14651858.CD010061.pub3.
Acknowledgements
The authors want to thank all the participants in this study. Special thanks for the NICU nurses who have made this study possible.
Funding
This study was funded by Shanghai Children’s Hospital Clinical Research Project (2020YLYM08).
Author information
Authors and Affiliations
Contributions
CY and CC contributed to the conception and design of this study. CY drafted the manuscript and revised it critically. XG, HL, YL, YL and BW contributed to acquisition, analysis and interpretation of data. All authors read the manuscript and gave the permission to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods of this study were reviewed and approved by ethics committee of Shanghai Children’s Hospital in accordance with Declaration of Helsinki and its later amendments (approval number: 2021R013-E01). All the parents of enrolled patients read and signed the informed consent.
Consent for publication
Not applicable.
Competing interests
All authors declare that there is no conflict of interest in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, C., Gong, X., Luo, H. et al. Impact of implementation of 2019 European respiratory distress syndrome guidelines on bronchopulmonary dysplasia in very preterm infants. Ital J Pediatr 50, 178 (2024). https://doi.org/10.1186/s13052-024-01752-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-024-01752-4