Abstract
Background
In the acute distress respiratory syndrome (ARDS), specific lung regions can be exposed to excessive strain due to heterogeneous disease, gravity-dependent lung collapse and injurious mechanical ventilation. Computed tomography (CT) is the gold standard for regional strain assessment. An alternative tool could be the electrical impedance tomography (EIT). We aimed to determine whether EIT-based methods can predict the dynamic relative regional strain (DRRS) between two levels of end-expiratory pressure (PEEP) in gravity-non-dependent and dependent lung regions.
Methods
Fourteen ARDS patients underwent CT and EIT acquisitions (at end-inspiratory and end-expiratory) at two levels of PEEP: a low-PEEP based on ARDS-net strategy and a high-PEEP titrated according to EIT. Three EIT-based methods for DRRS were compared to relative CT-based strain: (1) the change of the ratio between EIT ventilation and end-expiratory lung impedance in arbitrary units ([ΔZAU low-PEEP/EELIAU low-PEEP]/[ΔZAU high-PEEP/EELIAU high-PEEP]), (2) the change of ΔZ/EELI ratio calibrated to mL ([ΔZml low-PEEP/EELIml low-PEEP]/[ΔZml high-PEEP/EELIml high-PEEP]) using CT data, and (3) the relative change of ∆ZAU (∆ZAU low-PEEP/∆ZAU high-PEEP). We performed linear regressions analysis and calculated bias and limits of agreement to assess the performance of DRRS by EIT in comparison with CT.
Results
The DRRS assessed by (ΔZml low-PEEP/EELIml low-PEEP)/(ΔZml high-PEEP/EELIml high-PEEP) and ∆ZAU low-PEEP/∆ZAU high-PEEP showed good relationship and agreement with the CT method (R2 of 0.9050 and 0.8679, respectively, in non-dependent region; R2 of 0.8373 and 0.6588, respectively, in dependent region; biases ranging from − 0.11 to 0.51 and limits of agreement ranging from − 0.73 to 1.16 for both methods and lung regions). Conversely, DRRS based on EELIAU ([ΔZAU low-PEEP/EELIAU low-PEEP]/[ΔZAU high-PEEP/EELIAU high-PEEP]) exhibited a weak negative relationship and poor agreement with the CT method for both non-dependent and dependent regions (R2 ~ 0.3; bias of 3.11 and 2.08, and limits of agreement of − 2.13 to 8.34 and from − 1.49 to 5.64, respectively).
Conclusion
Changes in DRRS during a PEEP trial in ARDS patients could be monitored using EIT, based on changes in ΔZmL/EELIml and ∆ZAU. The relative change ∆ZAU offers the advantage of not requiring CT data for calibration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Dynamic lung strain refers to the deformation of the pulmonary parenchyma during tidal ventilation (VT) relative to the end-expiratory lung volume (EELV) [1, 2]. Specific lung regions can be exposed to excessive strain due to heterogeneous disease, gravity-dependent lung collapse, and injurious mechanical ventilation. This excessive regional strain correlates with worsening local inflammation in acute respiratory distress syndrome (ARDS) [2,3,4].
The gold-standard method to assess regional strain is computed tomography (CT). However, this is a time-consuming procedure that exposes the patient to X-ray radiation [5]. As an alternative, electrical impedance tomography (EIT), a bedside radiation-free method, has been proposed for assessing regional strain [6]. In a proof-of-concept study, our group demonstrated a strong association between changes in strain measured by CT and changes in electrical impedance (ΔZ) at two levels of positive end-expiratory pressure (PEEP) [7].
A novel method of EIT-based strain was proposed by Gogniat et al. [6] calculating the relative change in lung strain at two levels of PEEP by dividing ΔZ by end-expiratory lung impedance (EELI), a surrogate of EELV. This approach is compelling as it shares similarities with the classical CT-based strain method. However, caution is warranted in utilizing EELI in arbitrary units (A.U., the standard EIT unit), which may provide inaccurate measurements of strain due to “arbitrariness” of the absolute value at the end of expiration, such as the possibility of values close to zero or even negative (producing a non-physiological strain). In addition, a validation study comparing the change of regional strain measured by CT and EIT is lacking.
Therefore, we aimed to determine whether EIT-based methods, including the recent ΔZ/EELI approach in A.U., can predict changes in dynamic regional strain between two levels of PEEP measured by CT in gravity-non-dependent and dependent lung regions in ARDS patients.
Methods
This study involved mechanically ventilated patients with ARDS under deep sedation and neuromuscular blockade on volume-controlled ventilation (VCV) with VT of 6 ml/kg of predicted body weight. The study was approved by the Ethics Committee of Hospital Clínico Universidad de Chile (N.027/2016). Dynamic strain was assessed in gravity-non-dependent and dependent lung regions using whole-lung low radiation CT [7] and EIT (Enlight 1800, Timpel Medical, Brazil) simultaneously. These regions-of-interest were selected due to physiological relevance [8] and simple clinical applicability. Part of the CT and EIT data used in this study were obtained from a previous investigation [7]. Data collection was performed through end-expiration and end-inspiration breath-holds at two PEEP levels, applied in a random order according to the ARDS-net strategy (low-PEEP) [9] and to the EIT (high-PEEP). The latter was defined as the PEEP associated with the lowest combination of collapse and overdistension during a decremental PEEP trial after a recruitment maneuver [7, 10]. The end-inspiration holds were performed by configuring a continuous positive airway pressure (CPAP) level similar to the plateau pressure, while end-expiratory holds utilized CPAP at the same PEEP total level. The reference frames for the EIT image reconstruction were based on the PEEP level defined by the ICU team before the performed PEEP titration.
The CT strain (StrainCT) was calculated as the ratio between VT and EELV. The relative change in StrainCT between low-PEEP and high-PEEP, termed dynamic relative regional strain (DRRS), was defined as (StrainCT low-PEEP/StrainCT high-PEEP) for each region-of-interest. The EIT-based strain was assessed according to the following methods:
-
(1)
The relative change of ΔZ/EELI ratio in A.U. between the lowest and the highest value of PEEP ([ΔZAU low-PEEP/EELIAU low-PEEP]/[ΔZAU high-PEEP/EELIAU high-PEEP]).
-
(2)
The relative change of ΔZ/EELI ratio in mL between the lowest and the highest value of PEEP ([ΔZml low-PEEP/EELIml low-PEEP]/[ΔZml high-PEEP/EELIml high-PEEP]). For this calculation, we converted the regional EELI in mililiters (EELIml) at low-PEEP using corresponding EELV measured by CT. The ΔZml was computed multiplying the ΔZAU by the ratio of VT/ΔZAU at low-PEEP. Finally, the EELIml at high-PEEP was estimated from the sum of EELImL at low-PEEP and ΔEELIml calculated multiplying the ΔEELIAU by the ratio of VT/ΔZAU at low-PEEP [11].
-
(3)
the relative change of ∆ZAU between the lowest and the highest value of PEEP (∆ZAU low-PEEP /∆ZAU high-PEEP) [7].
The summary of the protocol is shown in Fig. 1A. We performed linear regressions analysis and calculated bias and limits of agreement to assess the performance of DRRS by EIT in comparison with CT.
Experimental protocol and correlation between changes in lung volume by computed tomography (CT) and electrical impedance tomography (EIT) related data. A Experimental protocol of a representative case. Traces of airway pressure (upper row), impedance change in non-dependent (middle row) and dependent (lower row) lung regions during the study timeframe are shown. Two levels of PEEP were applied in random order (in this representative case, first low-PEEP and then high-PEEP, after a recruitment maneuver). At both PEEP levels, end-expiratory and end-inspiratory holds were applied to obtain positive end-expiratory pressure and end-expiratory lung impedance (EELI), and airway plateau pressure and end-inspiratory lung impedance (EILI), respectively. The impedance change (ΔZ) corresponded to the difference between EILI and EELI. CT and EIT assessments were performed at the same time. B Linear correlation between delta end-expiratory lung volume (ΔEELV) CT-measured and the change of lung volume obtained from changes in end-expiratory lung impedance (ΔEELIml)
Results
Fourteen patients (age 67 [60–76] years, 8 males) were included. Their worst PaO2:FiO2 ratio during the acute phase of ARDS was 129 [96–167] mmHg. At the study entry, the mechanical ventilation time was 8 [4–12] days and PaO2:FiO2 ratio was 235 [210–274] mmHg with FiO2 0.35 [0.30–0.36]. The median low-PEEP and high-PEEP values were 6 [5–7] cm H2O and 12 [10–14] cm H2O, respectively.
Global EELV was 1300 [1064–1706] ml at low-PEEP and 1901 [1472–2463] ml at high-PEEP. Global EELI was − 14.67 [− 28.1 to − 11.86] A.U. at low-PEEP and 10.91 [− 7.57 to 32.53] A.U. at high-PEEP. The ΔEELIml, induced by PEEP changes, demonstrated a strong association with the ΔEELV detected by CT (Fig. 1B).
We observed a negative association between DRRS by ∆ZAU/EELIAU and DRRS by StrainCT in both lung regions (Fig. 2A; R2 ~ 0.3), and a poor agreement for both non-dependent and dependent regions (bias of 3.11 and 2.08, and limits of agreement of − 2.13 to 8.34 and from − 1.49 to 5.64, respectively).
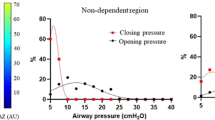
Association and agreement between CT-based DRRS and the different EIT-based methods evaluated in non-dependent and dependent lung regions. A Association between DRRS by CT and DRRS by ΔZAU/EELIAU. B Association between DRRS by CT and DRRS by ΔZml/EELIml. C Association between DRRS by CT and DRRS by ΔZAU (For A–C individual values and linear regression curves with 95% confidence bands for both regions analyzed are shown). D Agreement between CT-based DRRS and the different EIT-based methods. For this analysis, the differences between the individual value of CT-based DRRS and the respective EIT-based DRRS values are shown with mean and standard deviation for each EIT method. E Illustration of changes in EELI induced by PEEP using different references for EIT reconstruction (PEEP 5 cmH2O and PEEP 7 cmH2O). Note that modifying the reference results in arbitrary DRRS values (both in absolute levels and the differences between the PEEP steps), with an increase in reference EELI values which leads to lower DRRS
On the other hand, DRRS based on ∆Zml/EELIml and ∆ZAU showed good relationship and agreement with the reference method in both lung regions, with biases ranging from − 0.11 to 0.51 and limits of agreement ranging from − 0.73 to 1.16 (Fig. 2C–E).
Discussion
This study demonstrated that DRRS estimation between two levels of PEEP is feasible at the bedside using EIT. The DRRS based on changes in ∆Zml/EELIml accurately predicts the change in lung strain assessed by CT in different gravitational lung regions. Our data also suggests that the relative change in ∆ZAU induced by PEEP changes (∆ZAU low-PEEP/∆ZAU high-PEEP) can be used as a surrogate of DRRS.
However, the DRRS based on changes in ΔZAU/EELIAU exhibited a behavior that contradicts biophysically principles when EELIAU is negative. The negative value of EELIAU is a frequent finding; indeed, its absolute value depends on the clinical condition at the start of EIT recordings (i.e., the reference frame), and it varies significantly among subjects, and even within the same subject [12, 13]. EELIAU is also influenced by changes in intrathoracic blood volume or fluid status [14]. From a physical perspective, the absolute values of EELI are intrinsically meaningless. Its value should be exclusively derived from its linear relationship with changes in lung air content. Furthermore, any attempt to avoid negative EELIAU values, such as using a lower level of PEEP as a reference value for EIT reconstruction, will not yield meaningful DRRS value. The higher the adjustment in EELIAU, the lower the DRRS value (see Fig. 2E). Therefore, relying on EELI measurements in arbitrary units is impractical for quantifying strain independently of the EIT reference.
The outperformance of the relative changes in ∆Zml/EELIml for assessing DRRS was expected because this approach intrinsically cancelled the influence of absolute values of EELI (A.U.), retaining only its relative changes to a reference condition. A strong correlation between ∆EELV and ∆EELI during a PEEP trial is a fundamental requirement for employing this approach [11, 15]. To achieve this, we avoided changes in patient positioning between PEEP steps and also any bolus of intravenous infusions. The current study used for first time CT data to perform the correlations between ∆EELV and ∆EELIml at global and regional level. Our findings reinforce the close association between CT and EIT for EELV-related data, validating its use for calculating DRRS. The major limitation of this approach is the requirement of a baseline CT data for calibration.
An alternative is using the relative changes in ∆ZAU as a surrogate of DRRS. The ability of ∆Z to capture the change of strain in response to increase in PEEP was also suggested in the Gogniat et al. [6] study. Despite similar VT at PEEP 15 and ZEEP in the pigs (333 ± 71 ml and 334 ± 74, respectively, p = non-significant), ∆ZAU significantly increased between PEEP 15 and ZEEP (from 0.35 ± 0.90 to 0.46 ± 0.14 A.U., p < 0.05). Therefore, ∆ZAU in lung parenchyma exhibits a behavior similar to that observed in other biological tissues in response to mechanical deformation [16]. However, it is essential to acknowledge two important points: (1) regional ΔZAU may be influenced by the regional redistribution of ventilation induced by higher PEEP levels, and (2) the ΔZAU ratio at low-PEEP/high-PEEP is not a direct measurement of strain, as traditionally established by the ratio VT/EELV.
Our findings must be interpreted with caution due to some limitations: (1) being a clinical study of limited size; (2) only two levels of PEEP were evaluated and (3) the selection of regions-of-interest was based on the gravity gradient, not accounting for individualized lung injury distribution.
In conclusion, changes in DRRS during a PEEP trial in ARDS patients could be monitored using EIT, based on changes in ΔZmL/EELIml and ∆ZAU. While the ∆Z method may be slightly less precise compared to the standard ΔZmL/EELIml method, it offers the advantage of not requiring any CT data for calibration. Further research is needed to explore the clinical significance of the ΔZAU low-PEEP/ΔZAU high-PEEP method in lung protection, as well as its comparison with other VILI determinants like transpulmonary pressure.
Availability of data and materials
The datasets and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- VT :
-
Tidal ventilation
- EELV:
-
End-expiratory lung volume
- CT:
-
Computed tomography
- EIT:
-
Electrical impedance tomography
- ΔZ :
-
Tidal change in electrical impedance
- PEEP:
-
Positive end-expiratory pressure
- EELI:
-
End-expiratory lung impedance
- EILI:
-
End-inspiratory lung impedance
- A.U.:
-
Arbitrary units
- VCV:
-
Volume-controlled ventilation
- DRRS:
-
Dynamic relative regional strain
- SOFA score:
-
Sequential organ failure assessment score
- PaO2FiO2 ratio:
-
Ratio of arterial partial pressure of oxygen to inspired oxygen fraction
References
Protti A, Andreis DT, Monti M, Santini A, Sparacino CC, Langer T, et al. Lung stress and strain during mechanical ventilation: Any difference between statics and dynamics? Crit Care Med. 2013;41:1046–55.
Bellani G, Guerra L, Musch G, Zanella A, Patroniti N, Mauri T, et al. Lung regional metabolic activity and gas volume changes induced by tidal ventilation in patients with acute lung injury. Am J Respir Crit Care Med. 2011;183:1193–9.
Motta-Ribeiro GC, Hashimoto S, Winkler T, Baron RM, Grogg K, Paula LFSC, et al. Deterioration of regional lung strain and Inflammation during early lung injury. Am J Respir Crit Care Med. 2018;198:891–902.
Retamal J, Hurtado D, Villarroel N, Bruhn A, Bugedo G, Amato MBP, et al. Does regional lung strain correlate with regional inflammation in acute respiratory distress syndrome during nonprotective ventilation? An experimental porcine study. Crit Care Med. 2018;46:e591–9.
Gattinoni L, Caironi P, Pelosi P, Goodman LR. What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med. 2001;164:1701–11.
Gogniat E, Madorno M, Rodriguez PO, Dianti J, Otero PE, Krukewitt L, et al. Dynamic relative regional lung strain estimated by electrical impedance tomography in an experimental model of ARDS. Respir Care. 2022;67:906–13.
Cornejo R, Iturrieta P, Olegário TMM, Kajiyama C, Arellano D, Guiñez D, et al. Estimation of changes in cyclic lung strain by electrical impedance tomography: proof-of-concept study. Acta Anaesthesiol Scand. 2021;65:228–35.
Yoshida T, Amato MBP, Grieco DL, Chen L, Lima CAS, Roldan R, et al. Esophageal manometry and regional transpulmonary pressure in lung injury. Am J Respir Crit Care Med. 2018;197:1018–26.
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36.
Costa EL, Borges JB, Melo A, Suarez-Sipmann F, Toufen C Jr, Bohm SH, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35:1132–7.
Bikker IG, Leonhardt S, Bakker J, Gommers D. Lung volume calculated from electrical impedance tomography in ICU patients at different PEEP levels. Intensive Care Med. 2009;35:1362–7.
Ling S, Zhao Z. End-expiratory lung impedance measured with electrical impedance tomography at different days are not comparable. Crit Care Med. 2023;51:e70–2.
Heines SJH, Strauch U, van de Poll MCG, Roekaerts PMHJ, Bergmans DCJJ. Clinical implementation of electric impedance tomography in the treatment of ARDS: a single centre experience. J Clin Monit Comput. 2019;33:291–300.
Becher T, Wendler A, Eimer C, Weiler N, Frerichs I. Changes in electrical impedance tomography findings of ICU patients during rapid infusion of a fluid bolus: a prospective observational study. Am J Respir Crit Care Med. 2019;199:1572–5.
Hinz J, Hahn G, Neumann P, Sydow M, Mohrenweiser P, Hellige G, et al. End-expiratory lung impedance change enables bedside monitoring of end-expiratory lung volume change. Intensive Care Med. 2003;29:37–43.
Veil C, Muller D, Walz S, Schule J, Somers P, Tarin C, et al. Enhancing tissue impedance measurements through modeling of fluid flow during viscoelastic relaxation. IEEE Trans Biomed Eng. 2023;70:650–8.
Acknowledgements
The authors thank the nurses, respiratory therapists, medical technologists, and medical staff from Hospital Clínico Universidad de Chile for their support during the execution of the study.
Funding
Grant FONDECYT No. 1161510 and No. 1221829 awarded to Rodrigo Cornejo. The funding bodies had no role in the design of the study, or the collection, analysis, or interpretation of data or the manuscript preparation.
Author information
Authors and Affiliations
Contributions
Authorship credit was based on 1.1 RB, CM, and RC substantial contributions to conception and design. 1.2 RB, CM, ML, DG, AG, DA, MA, and RC helped in acquisition of data, performed analysis and interpretation of data, drafting the article or revising it critically for important intellectual content. 3 Final approval of the version to be published by RB, CM, ML, DG, AG, DA, MA, and RC.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board reviewed and approved the study (approval number N.027/2016, Comité Ético Científico Hospital Clínico Universidad de Chile). Informed consent was obtained from the patient’s next of kin.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brito, R., Morais, C.C.A., Lazo, M.T. et al. Dynamic relative regional lung strain estimated by computed tomography and electrical impedance tomography in ARDS patients. Crit Care 27, 457 (2023). https://doi.org/10.1186/s13054-023-04748-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04748-4