Abstract
Background
In major trauma patients, hypocalcemia is associated with increased mortality. Despite the absence of strong evidence on causality, early calcium supplementation has been recommended. This study investigates whether calcium supplementation during trauma resuscitation provides a survival benefit.
Methods
We conducted a retrospective analysis using data from the TraumaRegister DGU® (2015–2019), applying propensity score matching to balance demographics, injury severity, and management between major trauma patients with and without calcium supplementation. 6 h mortality, 24 h mortality, and in-hospital mortality were considered as primary outcome parameters.
Results
Within a cohort of 28,323 directly admitted adult major trauma patients at a European trauma center, 1593 (5.6%) received calcium supplementation. Using multivariable logistic regression to generate propensity scores, two comparable groups of 1447 patients could be matched. No significant difference in early mortality (6 h and 24 h) was observed, while in-hospital mortality appeared higher in those with calcium supplementation (28.3% vs. 24.5%, P = 0.020), although this was not significant when adjusted for predicted mortality (P = 0.244).
Conclusion
In this matched cohort, no evidence was found for or against a survival benefit from calcium supplementation during trauma resuscitation. Further research should focus on understanding the dynamics and kinetics of ionized calcium levels in major trauma patients and identify if specific conditions or subgroups could benefit from calcium supplementation.
Similar content being viewed by others
Background
In major trauma patients, disturbances in ionized calcium levels (iCa2 +) will be caused by the injury itself, physiological derangements, subsequent resuscitation strategies, and transfusion of blood products [1, 2].
Hypocalcemia resulting from the transfusion of citrate-containing blood products is well known [3,4,5]. Citrate chelates with the unbound ionized fraction of calcium, which can be worsened by profound shock in which organ failure leads to a reduced hepatic clearance of citrate. Especially during massive transfusion, with large volumes and at high rates, iCa2 + levels drop rapidly. However, even with the transfusion of a small number of blood products, a significant decrease in iCa2+ levels has been observed [5]. Moreover, other fluid resuscitation strategies also contribute to low calcium levels due to fluid-induced hemodilution or binding to colloids [6]. Hypocalcemia, resulting from resuscitation and transfusion, worsens platelet- dependent hemostasis disturbances [6, 7]. This will contribute to trauma-induced coagulopathy, leading to increased blood loss, the need for transfusion, and eventually death [8].
Even upon arrival at the emergency department (ED), before extensive resuscitation and transfusion, calcium disturbances are common with hypocalcemia identified in 13% to 74% of patients [2]. An independent association with increased mortality, coagulopathy, and blood transfusion requirements has also been demonstrated [2, 9, 10]. As a result, it has been suggested that hypocalcemia should be added to the well-known lethal triad of trauma-related death, consisting of hypothermia, acidosis, and coagulopathy [11].
To date, however, only a correlation has been demonstrated, and no causation has been proven [10]. Moreover, in a cohort analysis of more than 30,000 major trauma patients, we recently demonstrated that the relationship between iCa2 + levels and outcome appeared to be parabolic. Hypercalcemia upon arrival at the ED was also associated with an increased incidence of coagulopathy, transfusion requirements, and mortality. Compared to hypocalcemia, patients with hypercalcemia upon arrival at the ED had the highest mortality rates [2]. Similarly, MacKay et al. identified any hypercalcemia during the first 24 h after injury, in trauma patients requiring high-volume transfusion, to be associated with increased mortality [12].
High-quality evidence on calcium supplementation during trauma resuscitation is lacking [13]. The latest version of the European guidelines on major bleeding and coagulopathy following trauma, recommends monitoring of iCa2 +, and avoiding levels < 0.9 mmol/L. However, these recommendations are based on low-quality evidence [14]. Moreover, the extent to which these guidelines on calcium management are part of daily clinical practice remains unknown. Nevertheless, despite limited evidence, aggressive correction of iCa2 + levels has been advocated in recent literature [15,16,17].
This study aims to investigate the effects of calcium supplementation during trauma resuscitation on early and overall mortality. We hypothesized that calcium supplementation, administered during trauma reception and resuscitation, would have a beneficial effect on mortality.
Methods
Data source
The TraumaRegister DGU® of the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) is a multicenter database of pseudonymized and standardized documentation of severely injured patients. The inclusion criteria are ED admission to hospital, with life signs on arrival, and subsequent intensive care unit (ICU) management, or reaching hospital with vital signs but dying before ICU admission. The participating hospitals are primarily located in Germany (90%), but an increasing number of hospitals from other countries contribute data as well. The full dataset is obligatory for all supra-regional trauma centers, only hospitals certified as a regional or local trauma center within the TraumaNetzwerk DGU® are allowed to complete a basic dataset. The latter does not include iCa2 + levels. Laboratory values on admission, including iCa2 + , are defined as the first documented values at time of first blood collection upon arrival at the ED.
A detailed description of the dataset is provided in Supplement 1.
The present study is in line with the publication guidelines of the TraumaRegister DGU® and is registered under the TR-DGU project ID 2023-022. Because of the retrospective study design, no approval by the ethical committee was needed.
Study population
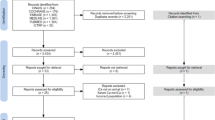
iCa2 + levels have been part of the full dataset since the ‘version V2015’ of the TraumaRegister DGU®. For this analysis, the study cohort was selected from this ‘version V2015’, which includes injured patients between 2015 and 2019. It was decided to use the identical population that was used in our previous study on this topic [2]. Moreover, during this time period, prehospital blood transfusion, and possibly accompanying calcium administration, was not routine practice. In the years after, there was an increasing number of services that implemented prehospital transfusion, which could not be registered in the TR-DGU [18]. The selection of the study sample is shown in Fig. 1.
The study cohort included adults (≥ 16 years old) with major traumatic injuries (Abbreviated Injury Scale [AIS] ≥ 3), who were directly admitted from the accident scene to a European trauma center. Patients who were transferred to another hospital within 48 h were excluded due to missing outcome data. Patients with only basic dataset registration or with missing/invalid data for transfusion, coagulation, or iCa2 + levels were also excluded.
Calcium supplementation was defined as the administration of a calcium supplement, in any formulation and dose, during the initial trauma reception and resuscitation. This includes the time between the patient's admission to the ED and subsequent admission to the ICU. The exact timing, formulation, and dose of the calcium supplement couldn’t be retrieved from the registry.
Statistical analysis
Demographics and characteristics
Relevant patient demographics, clinical characteristics, and outcome parameters were extracted from the registry and compared between patients who did and did not received calcium supplementation during trauma resuscitation.
Continuous variables were recorded as means with standard deviation (SD) if approximal normally distributed and as medians with interquartile range (IQR) otherwise. Categorical variables were presented as numbers with percentages. Differences were assessed by Student’s t test/Mann–Whitney U-test for continuous and Chi-squared test for categorical variables. A P value ≤ 0.05 was considered statistically significant. However, in large cohort analyses small differences could become statistically significant, even without any clinical significance. Therefore, P values do not necessarily reflect clinical relevance.
Multivariable logistic regression and propensity score matching
In this observational study, Propensity Score Matching (PSM) with matched pairs was chosen as the statistical method to pair treated and control subjects based on their propensity scores, which represent the probability of receiving treatment given observed covariates. This approach aims to balance the distribution of covariates between the groups, reducing selection bias and allowing for a more accurate estimation of the treatment effect [19].
For the calculation of the propensity score, a multivariable logistic regression model was used with calcium administration as a dependent variable. From the about 150 variables in the registry, potential predictors were selected a priori to the analysis, based on previous literature and expert consensus [2, 20]. Variables were considered relevant when available early during trauma management and related to patient demographics (age > 70 years), injury characteristics (AIS ≥ 3 head/thorax/abdomen/extremities, Injury Severity Score [ISS], polytrauma), prehospital and early interventions (intubation, catecholamine administration, pleural decompression), suspected active bleeding and/or shock (acidosis: base excess [BE] < −6, anemia: Hb < 8 g/dL, shock index [SI] ≥ 1, volume replacement, transfusion, tranexamic acid [TXA]), and measured hypocalcemia (iCa2 + < 1.10 mmol/L). Despite ISS and AIS are only calculated post-hoc, they reflect injury severity on arrival and include injuries that most of the time will be obvious after initial clinical examination and early diagnostics. Patients with missing data for any variable were excluded from the propensity score calculation.
Based on this multivariable model, the probability to receive calcium (propensity score) was derived and expressed as rounded percentages. Next, pairs from both groups with identical propensity scores were matched one-to-one at random (1:1 exact matching without replacement). After matching, the adequacy of the propensity score model was assessed by measuring the comparability between the groups using the standardized difference. A difference < 0.1 was considered as a sign of balance [19, 21].
SPSS® Statistics software (IBM Corp. Version 27. Armonk, NY, USA) was used for all statistical analyses.
Outcomes
The following primary outcome parameters were considered: 6 h mortality, 24 h mortality, and in-hospital mortality. In-hospital mortality was measured as an absolute number, and subsequently, a standardized mortality ratio (SMR) was also calculated. The SMR compares the measured mortality to the expected mortality. This allowed us to evaluate whether differences in in-hospital mortality between the two matched groups were related to calcium supplementation or rather to differences in expected mortality. For this mortality prediction, the Revised Injury Severity Classification, version II (RISC II) was used. The RISC has been developed and used for outcome adjustment in the TraumaRegister DGU® since 2003; it was updated in 2014 to a second version (RISC II) and has been repeatedly validated since its introduction [22, 23].
Other secondary outcome parameters were measured: ICU admission, length-of stay (LOS) in ICU, multiple-organ-failure (MOF) and sepsis, iCa2 + and INR on arrival in ICU, in-hospital LOS, and cause of death.
Results
Study cohort selection
In the TraumaRegister DGU® 175,729 patients were registered within the ‘version V2015’ dataset (2015–2019). Of these, 30,183 adult major trauma patients who were directly admitted to a European trauma center and from whom the full dataset was available were considered (Fig. 1).
A total of 18,389 patients were excluded because of missing/invalid iCa2 + values. To detect potential selection bias, some relevant comparative data was analyzed between this group and the study cohort. This group had a median age of 55 years, but with lower injury severity (ISS 17) and mortality (13%, RISC II 12.4%) compared to the study cohort.
A total of 1860 (62%) patients for whom no data on calcium supplementation was available were excluded. This left a cohort of 28,323 patients.
Demographics and characteristics were retrieved and compared between all patients with (n = 1593, 5.6%) and without calcium supplementation (n = 26,730). These results are shown in Table 1. Compared to those who did not receive calcium supplementation, those who received calcium supplementation were more severely injured (median ISS 33 [IQR 22–43] vs. 20 [IQR 14–29], P < 0.001), with a higher incidence of thoracic, abdominal and extremity injuries. They received more prehospital interventions (intubation, catecholamines, decompression, and volume resuscitation; P < 0.001). On arrival at the ED, they were more shocked (SI ≥ 1, 43.1% vs. 14.4%, P < 0.001), acidotic (BE −6.6 (SD 6,8] vs. −1.9 [SD 4.5], P < 0.001), and coagulopathic (INR 1.46 [SD 0.85] vs. 1.18 [SD 0.51]; P < 0.001). iCa2 + levels were significantly different between the two groups (1.14 [SD 0.12] vs. 1.17 [SD 0.08] mmol/L, P < 0.001), although both were within the normal range. The incidence of hypocalcemia was higher in the group which received calcium supplementation (23.4% versus 12.0%, P < 0.001) During in-hospital management, higher total volumes were administered to the calcium supplementation group (3000 ml [IQR 15000–5000] vs. 500 ml [IQR 500–1500], P < 0.001), including a higher incidence of transfusion (74% vs. 10%, P < 0.001) and more units if transfused (5 [IQR 3–9] vs. 3 [IQR 2–5] units of pRBC, 4 [IQR 0–8] vs. 0 [IQR 0–4] units of FFP; P < 0.001).
Multivariable logistic regression and propensity score matching
From a multivariable logistic regression, a propensity score was generated. (Table 2) Only 262 patients (0.9%) had missing data for one of the variables and could not be included in the logistic regression model. Increasing volume administration during in-hospital resuscitation, increasing number of pRBC transfusion, transfusion of FFP, administration of catecholamines, and decreasing levels of iCa2 + appeared to be associated with a higher probability of calcium supplementation. Patients who needed massive transfusion with 10 or more units of pRBC had the highest probability of receiving calcium (OR 6.099, 95% CI 4.566–8.148; P < 0.001).
Shock index (OR 0.971), polytrauma (OR 1.074), prehospital intubation (OR 1.125), and prehospital pleural decompression (OR 0.983) could be excluded due to minimal effect. Polytrauma was defined according to the Berlin definition [24].
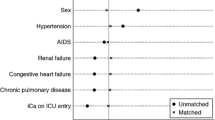
To estimate the treatment effect of calcium supplementation 1447 patients (91%) could be matched based on their identical propensity scores. After matching, these two groups were well comparable with similar demographics and injury profiles. (Table 1) The prevalence of major thoracic and abdominal trauma was higher in the group that did not receive calcium supplementation (P < 0.05). Prehospital management did not differ between the two groups, and they had comparable clinical findings on admission at the ED. Despite statistical significance, INR was almost identical between the two groups (INR 1.38 vs. 1.43, P = 0.016) and not reflecting a clinically relevant difference. There was no difference in iCa2 + level at first measurement after arrival at the ED and the proportion of patients with hypocalcemia was comparable. The volume administered in ED and the incidence of transfusion were similar in both groups. In absolute numbers, there was no relevant difference in units of blood products that were transfused, however it yielded statistical significance (pRBC n = 4, P = 0.023; FFP n = 4 vs. 3, P = 0.005).
The robustness of our model was confirmed by standardized differences < 0.1 in the matched groups, except from AIS thorax (0.111), indicating no signs of imbalance between the two groups after matching. (Fig. 2).
Outcomes
Considering the propensity score matched groups, mortality at 6 h and 24 h did not differ significantly. (Table 3) In-hospital mortality was higher in the group that received calcium supplementation (28.3% versus 24.5%, P = 0.020). However, after calculating the SMR with the RISC II, as an in-hospital mortality predictor, this difference was no longer statistically significant (P = 0.244). The expected mortality was indeed higher in the group that received calcium (27.9%) compared to the group that did not (25.9%) (P = 0.030).
There was no significant difference in the cause of death between the two groups (P = 0.600).
There was a similar admission rate to ICU, and no significant difference in the development of MOF during admission. Sepsis appeared to be more frequent in those who did not receive calcium (18.2% vs. 15.3%, P = 0.048). Nevertheless, ICU LOS did not differ between the groups. In contrast, in-hospital LOS was significantly shorter in the group which received calcium (20 [IQR 8–37] vs. 22 [IQR 9–38] days). iCa2 + levels on arrival in ICU did not differ between the groups (1.18 vs. 1.20 mmol/L, P = 0.574). The incidence of hypocalcemia was slightly higher when no calcium was supplemented (20.7% vs. 19.2%, P < 0.001). Conversely, the incidence of hypercalcemia was significantly higher in the group that received calcium (14.5% vs. 9.2%n P < 0.001). Despite the statical significance, no clinically significant difference in INR was detected at ICU admission (1.29 vs. 1.28, P = 0.037).
Discussion
Calcium supplementation is a common intervention in the management of major trauma patients and is part of the guidelines for the management of major bleeding in trauma patients [1, 14, 25, 26]. However, the evidence on this topic remains limited. To the best of our knowledge, no randomized controlled trials (RCTs) of calcium administration in major trauma patients are available, and this is the first study to evaluate the effect of calcium supplementation during trauma reception and resuscitation.
The aim of administering calcium is to prevent hypocalcemia, which is known to be associated with a higher incidence of coagulopathy, the need for blood transfusions, and mortality [9]. Tissue injury and accompanying physiological disturbances, combined with subsequent resuscitation involving blood transfusion, can cause a decrease in iCa2 + levels [11, 15]. Calcium is a crucial co-factor in the coagulation cascade and platelet function, and is essential for cardiac contractility and maintaining vascular tone [10, 17, 25]. The inotropic and procoagulant effect of calcium may be advantageous, by ameliorating trauma-induced coagulopathy, cardiac dysfunction, and vasoplegia [27, 28].
It is unsurprising that in this analysis, calcium was mostly administered to the most severely injured and sick trauma patients, given the expected beneficial effect. This group had more severe injuries and shock, required more extensive pre- and in-hospital interventions, had longer stays in both the ICU and hospital, had higher rates of complications, and had worse outcomes. Hemorrhage was especially evident as a cause of death.
The probability of receiving calcium supplementation increased with the administration of tranexamic acid, transfusion, and volume administration. It is well-established that higher volumes dilute iCa2 + levels and blood product transfusions exacerbate calcium decrease due to chelation with citrate. The group receiving extensive resuscitation would be expected to benefit the most from calcium supplementation.
In a matched pair analysis with identical propensity scores, two groups of severely injured trauma patients, with similar characteristics and management strategies, could be compared with calcium supplementation as the dependent variable. Awaiting RCTs, this approach permits to balance the distribution of covariates between the groups, reducing selection bias and allowing for a more accurate estimation of the treatment effect [21].
This analysis failed to demonstrate any survival benefit from calcium supplementation during trauma reception and resuscitation. It is important to note that this study is an analysis of the current practice of calcium administration, not limited to the correction of hypocalcemia. The rationale for calcium supplementation can be variable and could not be retrieved from the database. The lack of high-quality guidelines on calcium supplementation likely results in a variety of approaches to decision-making in current practice. Indications may include the correction of measured hypocalcemia, a predetermined standard operating procedure after a set number of blood products, or empirical practice [15].
Recently, concerns have been raised about empirical therapy in the trauma population, with a plea for a targeted, individualized approach based on point-of-care diagnostics [29, 30]. While our study does not provide evidence of the effectiveness of calcium supplementation in the overall major trauma population, our findings do not preclude that it might be beneficial in particular subgroups and in contrast be harmful to others.
Although exploring subgroups can be valuable, it was decided not to include subgroup analyses in this study because of methodological concerns and risks. Post-hoc subgroup analyses following negative overall results have increased risk of type 1 errors, bias, and overgeneralization. Inaccurate conclusions from small subgroup cohorts with low statistical power could undermine the reliability of the study's findings [31,32,33]. Therefore, future studies should be specifically designed to investigate the effect in specific groups of interest, such as those with hemorrhagic shock, TBI, massive transfusion, or hypocalcemia at any stage during trauma resuscitation.
It is, however, unclear whether there exists a crucial lower limit of iCa2 + below which correction is necessary. No consensus or evidence has been achieved within the recent literature [10, 14, 16]. Thrombo-elastography in healthy volunteers demonstrated that normal coagulation can be expected at iCa2% levels above 0.51–0.56 mmol/L [17, 34]. Conversely, in trauma patients, inducing early supraphysiologic calcium concentrations to improve platelet dependent hemostasis has been promoted [17].
Nevertheless, some concerns have been raised regarding high iCa2 + levels. Our previous analysis demonstrated a parabolic relation between iCa2 + levels and outcome, with hypercalcemia on arrival being associated with the worst outcomes [2]. In this study, a significant higher incidence of hypercalcemia was observed on arrival in ICU for those who received calcium during initial trauma resuscitation. In a previous study by Mackay (2017), any incidence of hypercalcemia during trauma resuscitation was associated with increased mortality [12]. Similarly, an RCT among adults with out-of-hospital cardiac arrest revealed that the administration of calcium during cardiopulmonary resuscitation did not improve the return of spontaneous circulation, but showed a trend toward a harmful effect for which the study was stopped early [35]. The hypothesis formulated to explain these findings was cytosolic and mitochondrial calcium overload, caused by the reversal of sodium-calcium exchange during ischemia and the elevated levels following calcium supplementation. This could induce a hypercontraction of the heart, disrupt several intracellular signaling pathways, and trigger cell death mechanisms [35, 36]. One can assume that trauma patients are vulnerable to similar effects.
Finally, and perhaps most importantly, we must understand the pathophysiology of iCa2 + disturbances to evaluate whether we can really expect an effect on outcome. The dynamics of iCa2 + are poorly understood in the context of trauma or severe illness. The important question remains if iCa2 + disturbances are indeed the cause of adverse outcomes or only correlated with them. If one assumes that low iCa2 + indeed contributes to coagulopathy and mortality, a beneficial effect of calcium supplementation would be expected. In contrast, if disturbances in iCa2 + levels are only an expression of the severity of illness, the administration of calcium is unlikely to change the outcome as long as the underlying pathophysiological derangements are not adequately managed [2].
To date, no causation has been demonstrated despite many years of ongoing debate. Apart from research in the trauma population, there have also been several studies in the ICU population [36]. These studies showed associations between iCa2 + derangements and poor prognosis in sepsis, acute pancreatitis, COVID-19, and hemorrhagic stroke. A comparable parabolic U-shaped relationship with outcome was demonstrated, even in the absence of major bleeding or transfusion. [37, 38] Some data suggest a survival benefit from minor hypo- and/or hypercalcemia [39]. Besides, even in hypocalcemia, intracellular Ca2 + appears to be elevated in some models of severe illness [40]. Inflammation induces an imbalance between calcium uptake and release, which causes the activation of calcium‐sensing receptors with subsequent release of reactive oxygen species and inflammatory cytokines. These processes have been attributed to damage to endothelial cells and disrupted barrier functions. The subsequent systemic inflammation and vascular permeability are detrimental at the cellular level, resulting in toxicity and cell death [41]. These findings in critically ill patients raise the question of whether iCa2 + disturbances are truly related to trauma or, more likely, to trauma-induced critical illness.
A Cochrane review revealed no clear evidence that parenteral calcium supplementation impacts the outcome of critically ill patients [42]. Moreover, hypocalcemia in ICU patients often seems refractory to treatment [43]. In our analysis about 20% of patients who received calcium supplementation in ED still had low iCa2 + levels on arrival in ICU. In several animal models no hemodynamic or survival benefit of calcium supplementation was detected in critical illness, and a harmful effect was even documented [44, 45]. A single pharmacological dose of calcium was associated with increased inflammation and vascular leakage, with subsequent organ dysfunction and mortality. The calcium/calmodulin-dependent protein kinase kinase (CAMKK) signaling was identified as a key underlying mechanism [40].
It is evident that, despite calcium measurement and correction being a common practice in all areas of critical care, there is still an urgent need to gain a deeper understanding of the dynamics and kinetics of iCa2 + levels in critical illness and major trauma. Furthermore, if calcium supplementation would be studied in prospective trials, it is essential to define meaningful clinical indications and relevant outcome measures to evaluate its effectiveness [2, 43].
Limitations
We need to acknowledge several limitations of our study.
First, all retrospective database analyses have inherent limitations. Data entry errors cannot be entirely excluded, moreover, measurement and documentation techniques can differ between hospitals. However, we believe that the impact of these potential sources of bias is minimized by the large sample size.
Second, propensity score matching attempts to mimic prospective randomization by post-hoc adjustment of unbalanced baseline data to define groups with similar baseline demographics and other characteristics. However, it cannot be entirely ruled out that residual unmeasured confounders exist between the groups. Hence, a propensity score matched analysis should not substitute for a formal RCT but may be deemed a reasonable alternative until randomized trials are conducted [46].
Third, it was necessary to exclude patients with no recorded iCa2 + levels, which can theoretically introduce selection bias when attempting to apply these findings to the entire trauma population. It can’t be retrieved from the registry whether these missing data were a consequence of not taking a blood gas sample on arrival or an error in the documentation process. This excluded group had a slightly lower injury severity. This is not unexpected, given that the threshold for performing a blood gas analysis on arrival is likely to be higher in less severely injured patients. When considering the demographics, clinical characteristics and initial management, we are convinced that the large sample presented is representative of the major trauma population which we aimed to study.
Fourth, no data were available on the dosage or formulation of calcium used, which implies that we were unable to include a dose–effect analysis. Also, the immediate effect of calcium supplementation on iCa2 + values could not be assessed. Furthermore, the rationale behind the administration of calcium, the precise timing of it, and the number of doses administered could not be determined. Consequently, this study can only conclude on the practice of calcium supplementation, rather than correction of hypocalcemia as such. A survey of the reasoning for calcium supplementation is warranted to get better insight into the current practice.
Conclusion
When comparing two similar groups of major trauma patients, in a propensity score matched model, no evidence for or against a survival benefit from calcium supplementation during early trauma resuscitation could be demonstrated.
It is crucial to gather more evidence on this topic before incorporating calcium supplementation into guidelines. Further research into iCa2 + dynamics is highly warranted. If iCa2 + only serves as a marker for pathophysiological derangements, then the administration of calcium may be obsolete or even harmful. However, there may be specific subgroups, or a crucial threshold, that necessitates calcium supplementation.
Availability of data and materials
The sensitive data presented in this study are available from a third party, the AUC (Academy for Trauma Surgery), which is the holder of the data of the TraumaRegister DGU®. The data protection concept of TraumaRegister DGU® includes that no raw data are available for external use. More information is available from: AUC—Akademie der Unfallchirurgie GmbH, Emil-Riedel-Straße 5, 80,538 München, Deutschland, Email: support-tr@auc-online.de.
Abbreviations
- iCa2 + :
-
Ionized calcium
- DCR:
-
Damage control resuscitation
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- ISS:
-
Injury severity score
- SI:
-
Shock index
- TXA:
-
Tranexamic acid
- AIS:
-
Abbreviated injury scale
- PTT:
-
Partial thromboplastin time
- INR:
-
International normalized ratio
- BE:
-
Base excess
- pRBC:
-
Packed red blood cells
- FFP:
-
Fresh frozen plasma
- TBI:
-
Traumatic brain injury
- MOF:
-
Multiple organ failure
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- RISC II:
-
Revised injury severity classification II
- SMR:
-
Standardized mortality ratio
- LOS:
-
Length of stay
- RCT:
-
Randomized controlled trial
References
Wray JP, Bridwell RE, Schauer SG, Shackelford SA, Bebarta VS, Wright FL, et al. The diamond of death: hypocalcemia in trauma and resuscitation. Am J Emerg Med. 2021;41:104–9.
Helsloot D, Fitzgerald M, Lefering R, Verelst S, Missant C. Trauma-induced disturbances in ionized calcium levels correlate parabolically with coagulopathy, transfusion, and mortality: a multicentre cohort analysis from the TraumaRegister DGU®. Crit Care. 2023;27:1–12.
Byerly S, Inaba K, Biswas S, Wang E, Wong MD, Shulman I, et al. Transfusion-related hypocalcemia after trauma. World J Surg. 2020;44:3743–50.
Giancarelli A, Birrer KL, Alban RF, Hobbs BP, Liu-Deryke X. Hypocalcemia in trauma patients receiving massive transfusion. J Surg Res. 2016;202:182–7.
Webster S, Todd S, Redhead J, Wright C. Ionised calcium levels in major trauma patients who received blood in the emergency department. Emerg Med J. 2016;33:569–72.
Vivien B, Langeron O, Morell E, Devilliers C, Carli PA, Coriat P, et al. Early hypocalcemia in severe trauma. Crit Care Med. 2005;33:1946–52.
Ho KM, Yip CB. Concentration-dependent effect of hypocalcaemia on in vitro clot strength in patients at risk of bleeding: a retrospective cohort study. Transfus Med. 2016;26:57–62.
Matthay ZA, Kornblith LZ. Platelet contributions to trauma-induced coagulopathy: updates in post-injury platelet biology, platelet transfusions, and emerging platelet-based hemostatic agents. Curr Trauma Rep. 2019;5:202–9.
Vasudeva M, Mathew JK, Groombridge C, Tee JW, Johnny CS, Maini A, et al. Hypocalcemia in trauma patients: a systematic review. J Trauma Acute Care Surg. 2021;90:396–402.
Kronstedt S, Roberts N, Ditzel R, Elder J, Steen A, Thompson K, et al. Hypocalcemia as a predictor of mortality and transfusion: a scoping review of hypocalcemia in trauma and hemostatic resuscitation. Transfusion. 2022;62:S158–66.
Ditzel RM, Anderson JL, Eisenhart WJ, Rankin CJ, DeFeo DR, Oak S, et al. A review of transfusion- and trauma-induced hypocalcemia: is it time to change the lethal triad to the lethal diamond? J Trauma Acute Care Surg. 2020;88:434–9.
Mackay EJ, Stubna MD, Holena DN, Reilly PM, Seamon MJ, Smith BP, et al. Abnormal calcium levels during trauma resuscitation are associated with increased mortality, increased blood product use, and greater hospital resource consumption: a pilot investigation. Anesth Analg. 2017;125:895–901.
Hall C, Nagengast AK, Knapp C, Behrens B, Dewey EN, Goodman A, et al. Massive transfusions and severe hypocalcemia: an opportunity for monitoring and supplementation guidelines. Transfusion. 2021;61:S188–94.
Rossaint R, Afshari A, Bouillon B, Cerny V, Cimpoesu D, Curry N, et al. The European guideline on management of major bleeding and coagulopathy following trauma: sixth edition. Crit Care. 2023;27:1–45.
DeBot M, Sauaia A, Schaid T, Moore EE. Trauma-induced hypocalcemia. Transfusion. 2022;62:S274–80.
Imamoto T, Sawano M. Effect of ionized calcium level on short-term prognosis in severe multiple trauma patients: a clinical study. Trauma Surg Acute Care Open. 2023;8:e001083.
Matthay ZA, Fields AT, Nunez-Garcia B, Patel MH, Cohen MJ, Callcut RA, et al. Dynamic effects of calcium on in vivo and ex vivo platelet behavior after trauma. J Trauma Acute Care Surg. 2020;89:871–9.
Thies KC, Truhlář A, Keene D, Hinkelbein J, Rützler K, Brazzi L, et al. Pre-hospital blood transfusion-an ESA survey of European practice. Scand J Trauma Resusc Emerg Med. 2020;28:1–8.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424.
Imach S, Wafaisade A, Lefering R, Böhmer A, Schieren M, Suárez V, et al. The impact of prehospital tranexamic acid on mortality and transfusion requirements: match-pair analysis from the nationwide German TraumaRegister DGU®. Crit Care. 2021;25:1–10.
Zakrison TL, Austin PC, McCredie VA. A systematic review of propensity score methods in the acute care surgery literature: avoiding the pitfalls and proposing a set of reporting guidelines. Eur J Trauma Emerg Surg. 2018;44:385–95.
Lefering R, Huber-wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGUTM: the revised injury severity classification, version II. Crit Care. 2014;18:476.
Lefering R, Huber-Wagner S, Bouillon B, Lawrence T, Lecky F, Bouamra O. Cross-validation of two prognostic trauma scores in severely injured patients. Eur J Trauma Emerg Surg. 2020;47:1837.
Pape HC, Lefering R, Butcher N, Peitzman A, Leenen L, Marzi I, et al. The definition of polytrauma revisited: an international consensus process and proposal of the new “Berlin definition.” J Trauma Acute Care Surg. 2014;77:780–6.
Moore EE, Moore HB, Kornblith LZ, Neal MD, Hoffman M, Mutch NJ, et al. Trauma-induced coagulopathy. Nat Rev Dis Prim. 2021;7:30.
Polytrauma Guideline Update Group. Level 3 guideline on the treatment of patients with severe/multiple injuries: AWMF Register-Nr. 012/019. Eur J Trauma Emerg Surg. 2018;44(Suppl 1):3.
Pape HC, Moore EE, McKinley T, Sauaia A. Pathophysiology in patients with polytrauma. Injury. 2022;53:2400–12.
Simpson R, Praditsuktavorn B, Wall J, Morales V, Thiemermann C, Tremoleda JL, et al. Myocardial alterations following traumatic hemorrhagic injury. J Trauma Acute Care Surg. 2023;95:481–9.
Davenport R, Curry N, Fox E, Lucas J, Evans A, Shanmugaranjan S, et al. Early and empirical high-dose cryoprecipitate for hemorrhage after traumatic injury: the CRYOSTAT-2 randomized clinical trial. JAMA. 2023;330:1882–91.
Bouzat P, Charbit J, Abback PS, Huet-Garrigue D, Delhaye N, Leone M, et al. Efficacy and safety of early administration of 4-factor prothrombin complex concentrate in patients with trauma at risk of massive transfusion: the PROCOAG randomized clinical trial. JAMA. 2023;329:1367–75.
Kivimäki M, Singh-Manoux A, Ferrie JE, David BG. Post hoc decision-making in observational epidemiology-is there need for better research standards? Int J Epidemiol. 2013;42:367–70.
Wang X, Piantadosi S, Le-Rademacher J, Mandrekar SJ. Statistical considerations for subgroup analyses. J Thorac Oncol. 2021;16:375–80.
Hiemstra B, Keus F, Wetterslev J, Gluud C, Van Der Horst ICC. DEBATE-statistical analysis plans for observational studies. BMC Med Res Methodol. 2019;19:1–10.
James MFM, Roche AM. Dose-response relationship between plasma ionized calcium concentration and thrombelastography. J Cardiothorac Vasc Anesth. 2004;18:581–6.
Vallentin MF, Granfeldt A, Meilandt C, Povlsen AL, Sindberg B, Holmberg MJ, et al. Effect of intravenous or intraosseous calcium vs saline on return of spontaneous circulation in adults with out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2021;326:2268–76.
Kelly A, Levine MA. Hypocalcemia in the critically ill patient. J Intensive Care Med. 2013;28:166–77.
Zhang Z, Xu X, Ni H, Deng H. Predictive value of ionized calcium in critically ill patients: an analysis of a large clinical database mimic ii. PLoS ONE. 2014;9:e95204.
Yan D, Xie X, Fu X, Pei S, Wang Y, Deng Y, et al. U-shaped association between serum calcium levels and 28-day mortality in patients with sepsis: a retrospective analysis of the MIMIC-III database. Shock. 2023;60:525–33.
Qin X, Cen J, Hu H, Chen X, Wei Z, Wan Q, et al. Non-linear relationship between albumin-corrected calcium and 30-day in-hospital mortality in ICU patients: a multicenter retrospective cohort study. Front Endocrinol. 2022;13:1–11.
Collage RD, Howell GM, Zhang X, Stripay JL, Lee JS, Angus DC, et al. Calcium supplementation during sepsis exacerbates organ failure and mortality via calcium/calmodulin-dependent protein kinase kinase signaling. Crit Care Med. 2013;41:6–10.
Sood A, Singh G, Singh TG, Gupta K. Pathological role of the calcium-sensing receptor in sepsis-induced hypotensive shock: therapeutic possibilities and unanswered questions. Drug Dev Res. 2022;83:1241–5.
Forsythe RM, Wessel CB, Billiar TR, Angus DC, Rosengart MR. Parenteral calcium for intensive care unit patients. Cochrane Database Syst Rev. 2008. https://doi.org/10.1002/14651858.CD006163.pub2.
Aberegg SK. Ionized calcium in the ICU should it be measured and corrected? Chest. 2016;149:846–55.
Malcolm DS, Zaloga GP, Holaday JW. Calcium administration increases the mortality of endotoxic shock in rats. Crit Care Med. 1989;17(9):900–3.
Carlstedt F, Eriksson M, Kiiski R, Larsson A, Lind L. Hypocalcemia during porcine endotoxemic shock: effects of calcium administration. Crit Care Med. 2000;28:2909–14.
Reiffel JA. Propensity score matching: the ‘devil is in the details’ where more may be hidden than you know. Am J Med. 2020;133:178–81.
Acknowledgements
Not applicable.
Funding
This study received no funding.
Author information
Authors and Affiliations
Consortia
Contributions
DH participated in the study conception and design, data acquisition, statistical analysis, data interpretation, and drafted the manuscript. MF, CG, NB, and SV participated in the study conception and design, data interpretation and revised the manuscript. RL participated in data interpretation, statistical analysis, and revised the manuscript. CM supervised the study, participated in the study conception and design, data interpretation and revised the manuscript. All authors revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The present study is reported within the publication guidelines of the TraumaRegister DGU® and registered as TR-DGU project ID 2023-022. Because of the retrospective study design, no approval by the ethical committee was needed.
Consent for publication
Not applicable.
Competing interests
RL declares that his institute has an ongoing service agreement with AUC GmbH, the holder of TraumaRegister DGU®, which includes statistical support in analysis of registry data. All other authors declared no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society (DGU).
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Helsloot, D., Fitzgerald, M., Lefering, R. et al. Calcium supplementation during trauma resuscitation: a propensity score-matched analysis from the TraumaRegister DGU®. Crit Care 28, 222 (2024). https://doi.org/10.1186/s13054-024-05002-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-05002-1