Abstract
Background
Toxoplasma gondii is an intracellular opportunistic pathogenic protozoan that poses serious threats, particularly in immunocompromised individuals. In the absence of a robust prophylactic measure, the mitigation and management of toxoplasmosis present formidable challenges to public health. We recently found that GRA72 plays an important role in parasitophorous vacuole (PV) morphology, growth and virulence of T. gondii. However, whether gra72-deficient strain can be used as a vaccine remains unknown.
Methods
We first examined the attenuated virulence of gra72 gene knockout strain (PruΔgra72) and the parasite load in organs of the infected mice. Subsequently, we evaluated the immune-protective effects of the PruΔgra72 vaccination against challenge with various types of T. gondii tachyzoites and Pru cysts. Furthermore, levels of antibodies and cytokines induced by PruΔgra72 vaccination were examined. Statistical analysis was conducted by Student’s t-test or Mantel-Cox log-rank test based on data obtained from three independent experiments with GraphPad Prism 8.0.
Results
We found that PruΔgra72 strain exhibited a significantly attenuated virulence even at the highest dose of 5 × 107 tachyzoites in Kunming mice model. The significant decrease of brain cyst burden and parasite load in the organs of the PruΔgra72-infected mice suggested its potentiality as a live-attenuated vaccine. Hence, we explored the protective immunity of PruΔgra72 vaccination against toxoplasmosis. Results showed that vaccination with 5 × 106 PruΔgra72 tachyzoites triggered a strong and sustained Th1-biased immune response, marked by significantly increased levels of anti-T. gondii IgG antibodies, and significantly higher levels of Th1 type cytokines (IL-2, IL-12 and IFN-γ) compared to that of Th2 type (IL-4 and IL-10). Vaccination with 5 × 106 PruΔgra72 tachyzoites in mice conferred long-term protection against T. gondii infection by less virulent tachyzoites (ToxoDB#9 PYS and Pru strains) and Pru cysts, provided partial protection against acute infection by high virulent Type I RH tachyzoites and significantly decreased brain cyst burden of chronically infected mice.
Conclusions
The avirulent PruΔgra72 induced strong protective immunity against acute and chronic T. gondii infection and is a promising candidate for developing a safe and effective live-attenuated vaccine against T. gondii infection.
Graphical Abstract

Similar content being viewed by others
Background
Toxoplasmosis, a prevalent zoonotic parasitic disease, emanates from Toxoplasma gondii and endangers practically all warm-blooded animals, including humans [1]. Humans and animals are predominantly infected with T. gondii by ingesting tissue cysts or oocysts from feline excrement or through congenital routes infiltrating via the placental barrier [2]. Immunocompetent individuals typically remain asymptomatic, yet infections with virulent T. gondii strains in immunocompromised hosts may result in severe clinical manifestations, such as encephalitis, pneumonia, retinitis and myocarditis, particularly in pregnant women susceptible to fetal deformities or miscarriage [2, 3]. Currently, T. gondii remains a major hindrance to global livestock development and public health. Toxoplasma gondii is the only recognized species within the genus Toxoplasma with approximately 300 different genotypes, including the three major clonal lineages (Types I, II and III) which have distinct virulence in mice [4,5,6].
The effective control and prevention of zoonotic toxoplasmosis present significant challenges, given the intricate multi-stage lifecycle of T. gondii, the diversity of intermediate hosts and its potent evasion of the host immune system [7, 8]. Though combined therapy of pyrimethamine and sulfadiazine has been proven to be the most effective in treating tachyzoites, pharmacological interventions often entail various adverse effects and fail to completely eradicate bradyzoites, thereby facilitating latent infections and drug residues [9]. The development of effective vaccines has emerged as a primary strategy for preventing and managing this disease. Thus far, numerous T. gondii vaccines have been devised, including nucleic acid vaccines, protein vaccines, nanovaccines, live vector-based vaccines and live attenuated vaccines [8]. Among these, live-attenuated vaccines, which mimic the entire process of parasite infection in the host, stimulate the host’s immune system to provide effective immune protection [8, 10]. Toxoplasma gondii live vaccines, including strains S48, T-263 and TS-4, have demonstrated efficacy in bolstering host immunity against T. gondii infection [11]. Notably, the T-263 strain elicits robust immune responses in feline hosts, especially showing commendable efficacy in preventing oocyst shedding [12, 13]. Meanwhile, vaccination with the S48 strain serves as a prophylactic measure against congenital toxoplasmosis in ovine populations, concurrently mitigating parasitic burden in meat products and reinforcing overall food safety [11]. However, the S48 strain carries the risk of mutations and restoration of pathogenicity [8]. Presently, Toxovax®, derived from the S48 strain lineage, stands as the only commercially endorsed vaccine available in countries like New Zealand and the UK [14]. Despite considerable progress achieved in the aforementioned vaccine types, live-attenuated T. gondii vaccines have not yet achieved complete elimination of tissue cysts and eradication of toxoplasmosis [15]. Further research into efficient and deployable vaccines remains an urgent matter to be addressed.
With the extensive development and application of genetic engineering techniques, live-attenuated T. gondii mutants were recently constructed by deleting key genes associated with virulence or metabolism, and their protective efficacy against T. gondii was explored. The RHΔtkl1 strain elicits robust humoral and cellular immune responses in immunocompetent mice, effectively counteracting T. gondii infection [16]. Inoculation with ME49Δcdpk3 significantly attenuates in vivo virulence in murine hosts, markedly diminishes cyst formation and provides a pivotal protection against both acute and chronic T. gondii infections by diverse strains [17]. Additionally, the double-gene knockout strain lacking gra17 and the newly putative transporter gene (npt1) confers protection against T. gondii infection in mice by modulating inflammatory responses [18].
Dense granule proteins (GRAs), indispensable secretory proteins of T. gondii, are involved in regulating important physiological activities, such as host cell immune defense, protein transport, evasion and chronic infection [19]. Secreted upon host invasion, GRAs dissolve within the parasitophorous vacuole (PV) lumen, localize to the intravacuolar network (IVN) embedded the PV membrane, insert into the parasitophorous vacuole membrane (PVM) or are exported into the host cell to exert their effects [19]. GRA42 and GRA43 serve as protein partners, mediating the correct localization of various proteins such as GRA17, GRA23 and GRA35 to the PVM [20]. GRA39 is involved in lipid utilization, and the absence of GRA39 reduces the virulence of T. gondii in the host, resulting in a lower cyst burden [21]. GRA24 possesses the ability to prolong the autophosphorylation of p38α and can activate the expression of pro-inflammatory genes in macrophages [22]. These identified GRAs have been validated as promising candidates for the development of vaccines against T. gondii [23,24,25].
Recently, our study showed that GRA72, possibly interacting with GRA47, is important for PV morphology, growth and virulence of T. gondii [26], consistent with a recent research [27]. Parasites deficient in GRA72 form abnormal morphology (bubble) PV, akin to Δgra17 parasites [28]. Additionally, GRA72 is also indispensable for the growth and virulence of T. gondii [28] and participates in the proper trafficking of GRA17 and GRA23 on the PVM [29]. Deletion of gra72 gene in Pru strain attenuated the virulence to mice at an infective dose of 1 × 106 tachyzoites [26]. Nevertheless, the potential of PruΔgra72 serving as a candidate vaccine for preventing toxoplasmosis remains unknown. Thus, the present study explored the immune-protective potential of the PruΔgra72 strain and evaluated the roles of humoral and cellular immunity in its protection against acute and chronic T. gondii infection in mice.
Methods
Mice and parasites
Eight-week-old female Kunming mice, susceptible to acute and chronic T. gondii infection compared to BALB/c and C57BL/6 mice [30], were purchased from Beijing Sibeifu Biotechnology Co., Ltd. All mice were fed under specific pathogen-free conditions at 50–60% humidity and 25 °C, provided with adequate food and water ad libitum. Mice were acclimatized for 1 week prior to the commencement of the experimental studies. Animal experiments were conducted following the principles of minimizing animal suffering and protecting animal welfare as much as possible. The tachyzoites of T. gondii Type I RH strain, Type II Pru strain, ToxoDB#9 PYS strain, the parental PruΔku80 strain (referred to as Pru) and the constructed gene knockout PruΔku80Δgra72 strain (referred to as PruΔgra72) [26] were replicated in human foreskin fibroblast (HFF) cells, maintained in DMEM containing 2% fetal bovine serum (FBS) and cultured in a CO2 incubator at 37 °C with 5% CO2. The cysts of the Type II Pru strain were obtained from the brain homogenate of infected mice, as described previously [31].
Optimization of PruΔgra72 vaccination dose
To assess the virulence of the PruΔgra72 strain in vivo, 8-week-old Kunming mice were infected by intraperitoneal injection with different doses (2 × 102, 5 × 102, 5 × 103, 5 × 104, 5 × 105, 5 × 106 and 5 × 107) of PruΔgra72 tachyzoites or (2 × 102 and 5 × 102) of wild-type Pru tachyzoites (8 mice per group). The clinical toxoplasmosis symptoms and mortality of all infected mice were observed twice every day for 30 days post-infection (dpi). The number of brain cysts in mice surviving at 30 days were counted. The presence of T. gondii in mice brain was determined with PCR targeting T. gondii B1 gene as previously described [32].
The parasite loads in organs (including eyes, brain, heart, liver, spleen, lungs, kidneys and intestines) of mice infected by 5 × 106 PruΔgra72 or Pru tachyzoites were determined 7 days post-infection using quantitative polymerase chain reaction (qPCR). Tissue DNA of various organs of infected mice was extracted using the TIANamp Genomic DNA Kit (Tiangen Biotech, DP304-03, Beijing, China). Sample DNA underwent normalization utilizing the mice U6 gene using ChamQ Universal SYBR qPCR Master Mix (Vazyme Biotech, Q711-02, Nanjing, China) to derive the CT values. Subsequently, parasite load was calculated using the standard curve analysis based on the Lg (tachyzoite number) and the corresponding CT values of the 529-bp fragment of extracted DNA from different gradient tachyzoites.
Protection against acute and chronic infection
Mice were intraperitoneally vaccinated with 5 × 106 PruΔgra72 tachyzoites or mock vaccinated with the same volume of PBS. To investigate the protective effect of PruΔgra72 immunization against acute T. gondii infection in mice, 102 and 103 RH or PYS tachyzoites along with 5 × 104 Pru tachyzoites (6 mice per group) were intraperitoneally injected into immunized and control mice at 60 and 120 days post-vaccination (dpv). The viability and number of tachyzoites injected into mice were examined by using the in vitro plaque assay [18].
For protection assessment against chronic infections, mice were inoculated with either 10 or 40 cysts (10 mice per group) at 60 and 120 dpv. The mortality and clinical toxoplasmosis symptoms were recorded within 1 month. At 30 dpi, the mouse cysts obtained from chronically infected mice were calculated under microscopic examination. Brain tissues without cysts were examined for B1 gene to further determine the infection status in mice.
Preparation of soluble T. gondii antigen (STAg)
The freshly harvested tachyzoites were washed three times with pre-cold PBS and resuspended in an appropriate volume of PBS, and the cellular integrity was disrupted by multiple freeze-thaw cycles. The suspension was sonicated on ice at a power of 80 W/s for 30 min to ensure efficient disruption and release of intracellular components. Following sonication, the suspension was centrifuged at 12,000 × g for 10 min to collect the supernatant containing the STAg and stored at -80 °C to maintain its stability and integrity.
Evaluation of T. gondii-specific antibodies in PruΔgra72-immunized mice
Immunological evaluations were carried out at 45, 60, 90 and 120 dpv to reveal differences in humoral immune responses between the vaccinated and unvaccinated groups. Total IgG and subclasses of IgG were detected using the mouse serum samples by ELISA to indicate humoral immune response profiles as previously described [33]. Briefly, 100 μl STAg per well, diluted to 1 μg/100 μl, was added to wells of a 96-well plate, followed by incubation at 37 °C for 2 h, then coated overnight at 4 °C. The antigen-coated ELISA plate was washed three times with 0.5% PBST, and the final wash was pat-dried before proceeding. Subsequently, non-specific binding sites were blocked by incubating with 5% BSA in a 37 °C incubator for 1 h, followed by another round of washing. Serum samples, diluted 1:100 in 1% BSA, were added to the wells and incubated at 37 °C. Next, the HRP-conjugated goat anti-mouse IgG (Abcam, AB97040, Cambridge, UK) was diluted at a ratio of 1:3000, while the goat anti-mouse IgG1 (Abcam, AB98693, UK) and IgG2a (Abcam, AB98698, UK) were diluted at a ratio of 1:5000 and then added to each respective well. After washing three times, TMB (3, 3′, 5, 5′-tetramethylbenzidine) Chromogen Solution for ELISA (Beyotime Biotech, P0209-100 ml, Shanghai, China) was used for color development. Upon stabilization of color development, a 2% sulfuric acid solution was added to terminate the reaction, and the optical density (OD) was measured at 450 nm.
Detection of cytokines in splenocyte supernatants in PruΔgra72-immunized mice
Following a previously described study [33], the spleens of immunized and non-immunized mice were gathered using sterile surgical forceps to prepare splenocyte suspensions for cytokine determination to discern cellular immune responses. The retrieved spleen was washed with RPMI-1640, gently ground on a 200-mesh nylon mesh to obtain a cell suspension and centrifuged at 1500 × g for 10 min to precipitate cellular debris. All separated splenic cells were immersed in red blood cell lysate for 3 min to procure a homogeneous splenic cell suspension. The suspension was then resuspended in RPMI-1640 culture medium supplemented with 10% FBS. The live cell number was determined utilizing the trypan blue exclusion method to ensure > 95% cell viability for subsequent analysis. The concentration of splenic lymphocytes was adjusted to 3 × 106 cells/ml and dispensed into individual wells. The splenocytes were then stimulated with STAg at a final concentration of 10 μg/ml to elicit an immune response. Following stimulation, the supernatants were harvested at specific time intervals: 24 h for IL-2 (BioLegend, 431,007, San Diego, USA) and IL-4 (BioLegend, 431,107, USA) assessment, 72 h for IL-10 (BioLegend, 431,417, USA) assessment and 96 h for IL-12 (BioLegend, 433,607, USA) and IFN-γ quantification (BioLegend, 430,807, USA). The collected supernatant was used to test the cytokine levels following the recommendations of the above-mentioned kits.
Statistical analysis
All experimental data were obtained for three biological replicates and analyzed using GraphPad Prism 8.0 (GraphPad Software Inc., La Jolla, CA, USA). A two-tailed, unpaired Student’s t-test was employed to determine the significance of differences between two groups, including antibody levels, cytokine levels, cyst burden and parasite burden. The Mantel-Cox log-rank test is applied to assess differences in survival curves. Here, P < 0.05 was considered statistically significant, and P < 0.01, < 0.001, < 0.0001 represented varying degrees of significance.
Results
Attenuated virulence and optimization of vaccination dose in mice
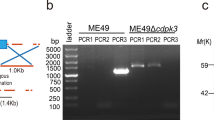
GRA72 plays important roles in PVM permeability and growth of T. gondii [26, 28]. Knockout of gra72 in Type II strain attenuated the parasite virulence [26, 28]. To determine whether this live-attenuated strain confers protection against T. gondii, the gene knockout PruΔgra72 strain constructed in our previous study was used in this study. The PCRs and the enlarged bubbled PVs of PruΔgra72 used in this study were consistent with that of PruΔgra72 in our previous study [26] (Additional file 1: Figure S1).
To assess the virulence and the potential of PruΔgra72 as a live-attenuated vaccine, varying dosages of PruΔgra72 tachyzoites were intraperitoneally administered in Kunming mice. Mice injected with the PruΔgra72 strain maintained a 100% survival rate even at the highest dose of 5 × 107 PruΔgra72 tachyzoites. However, all mice infected with 5 × 102 Pru tachyzoites were killed, and those with 2 × 102 Pru tachyzoites exhibited only a 25% survival rate (Fig. 1a). With the exception of mild messy fur observed in mice infected with the highest dose of 5 × 107 gene knockout tachyzoites, PruΔgra72-injected mice displayed no discernible clinical manifestations, while the Pru-infected mice manifested severe illness, such as lethargy, muscle weakness and decreased appetite within a week, ultimately leading to mortality. The surviving mice inoculated with 2 × 102 tachyzoites of the wild-type strain displayed an average cyst burden of 92 ± 12, whereas no cysts were detected in the brains of mice infected with 5 × 107 PruΔgra72. Cyst burden significantly decreased in mice inoculated with the PruΔgra72 strain compared to that of the Pru-infected group (P < 0.0001) (Fig. 1b). To reveal whether the PruΔgra72 parasites reach the brains of the infected mice, the brains of all surviving mice infected with PruΔgra72 were examined by amplifying the T. gondii B1 gene using PCR. The results showed that the positive rates of B1 gene in the brains of these mice with infection doses of 2 × 102, 5 × 102, 5 × 103, 5 × 104, 5 × 105, 5 × 106 and 5 × 107 were 12.5%, 12.5%, 25.0%, 25.0%, 62.5%, 87.5% and 87.5%, respectively (Additional file 2: Figure S2 and Additional file 3: Table S1). The positive rates of brain B1 gene were positively correlated with the infection doses. These results indicate that although the PruΔgra72 parasites could reach the mouse brain, they fail to form cysts. Collectively, these results revealed a significant attenuation of the virulence of PruΔgra72 to mice.
Virulence assessment of PruΔgra72 knockout strain in mice. (a) Survival curves of Kunming mice intraperitoneally infected with escalating doses (2 × 102, 5 × 102, 5 × 103, 5 × 104, 5 × 105, 5 × 106 and 5 × 107) of PruΔgra72 or (2 × 102 and 5 × 102) wild-type Pru tachyzoites. ****P < 0.0001, **P < 0.01. (b) Cyst numbers in brain tissues detected in the infected mice survived at 30 days post-infection. ****P < 0.0001
The parasite loads in various organs of the infected mice challenged with 5 × 106 PruΔgra72 or Pru tachyzoites at 7 dpi, including eyes, brain, heart, liver, spleen, lungs, kidneys and intestines, were obtained. PruΔgra72-infected mice exhibited parasite loads ranging from 101 to 103, while those infected with the wild-type Pru tachyzoites displayed parasite loads ranging from 103 to 105 (Fig. 2), showing the marked reduction of the parasite proliferation within the different organs in PruΔgra72-infected mice (Fig. 2). These results indicate that the absence of the gra72 gene has a profound impact on the in vivo replication and virulence of the parasite, and PruΔgra72 has potential to be used as a live-attenuated vaccine. Based on previous studies of the live attenuated RHΔompdcΔuprt and PruΔgra17 strains [34, 35], we chose the immunization dose of 5 × 106 PruΔgra72 tachyzoites for further research.
Reduced parasite burden in various murine organs of mice infected with PruΔgra72 tachyzoites. Parasite burden in the eyes (a), brain (b), heart (c), liver (d), spleen (e), lungs (f), kidneys (g) and intestines (h) of the mice inoculated with 5 × 106 Pru or PruΔgra72 tachyzoites at 7 days post-infection, which were assessed by quantitative polymerase chain reaction (qPCR) (n = 5 mice per group). ****P < 0.0001
PruΔgra72 confers protection against acute infection with various genotypes of T. gondii tachyzoites in mice
To determine the protective efficacy of PruΔgra72 vaccination against T. gondii acute infection (caused by tachyzoites), naive and vaccinated Kunming mice were challenged with 5 × 104 Type II (Pru strain) tachyzoites, 102 or 103 ToxoDB#9 (PYS strain) tachyzoites and 102 or 103 Type I (RH strain) tachyzoites at 60 dpv (Fig. 3). The results showed that the immunized mice achieved 100% survival when challenged with different doses of PYS and Pru tachyzoites compared to the blank mice, which were all killed within 13 days (Fig. 4a–c). By challenging mice with RH tachyzoites, PruΔgra72 extended mouse survival time, with survival rates ranging from 16.7% to 33.3% (Fig. 4d–e). Additionally, assessment of brain cysts revealed a complete absence of cyst formation in immunized mice challenged with 5 × 104 Pru strains, significantly decreased compared to that of the naive mice (Fig. 4f). In summary, vaccination with PruΔgra72 in mice can confer effective immune protection against T. gondii acute infection by tachyzoites of less virulent strains (PYS and Pru) and partial protection against infection caused by tachyzoites of the virulent RH strain.
Schematic illustration of the study design assessing the potential of PruΔgra72 as a live-attenuated vaccine. Virulence assessment of PruΔgra72 (a), vaccination with PruΔgra72 tachyzoites (b), immune responses induced by vaccination (c), protection assessment against acute infection by Toxoplasma gondii tachyzoits (d), chronic infection by Pru cysts (e) and long-term T. gondii infection (f)
Immunization with PruΔgra72-induced protection against acute and chronic Toxoplasma gondii infection at 60 days post-vaccination (dpv). Mice immunized with 5 × 106 PruΔgra72 tachyzoites were challenged with varying doses of T. gondii tachyzoites, including 102 PYS tachyzoites (a), 103 PYS tachyzoites (b), 5 × 104 Pru tachyzoites (c), 102 RH tachyzoites (d) and 103 RH tachyzoites (e). Survival rates were monitored for 30 days (n = 6 mice per group). ***P < 0.001, **P < 0.01. (f) Brain cyst numbers of the surviving mice infected with 5 × 104 Pru tachyzoites at 30 days after infection. ****P < 0.0001. Additionally, mice were orally infected with 10 or 40 Pru cysts (g–h), and their survival rates were observed over 1 month (n = 10 mice per group) **P < 0.01. i Brain cyst burden of the surviving mice challenged with cysts at 30 days after infection. ****P < 0.0001
PruΔgra72 confers protection against chronic infection by cysts in mice
To further assess the potential application of PruΔgra72 in protection against chronic T. gondii infection, 10 or 40 Pru cysts were orally administered to the immunized mice and naive mice at 60 dpv (Fig. 3). All the immunized mice survived after challenge with low or high doses of cysts. However, the unvaccinated mice exhibited clinical symptoms at 8 dpi, with ruffled fur and reduced appetite, and began dying at 11 dpi, with survival rates of 40% and 30% at low and high doses, respectively (Fig. 4g–h). These findings indicate that immunization with PruΔgra72 conferred protective efficacy against chronic infection in mice.
PruΔgra72 vaccination decreases brain cyst burden of chronically infected mice
The brain tissue of all surviving mice at 30 days in 60 dpv challenged groups were collected and used to determine the parasite cyst numbers. Non-immunized mice exposed to low-dose cysts showed an average cyst count of 346 ± 135 and 626 ± 215 cysts under high-dose cyst attack (Fig. 4i). However, the immunized mice demonstrated markedly reduced cyst burdens, with averages of merely 3 ± 8 and 5 ± 9 cysts in the immunized mice challenged with low and high dose of Pru cysts, respectively (Fig. 4i). Statistical analysis reveals a significant difference of brain cyst burden between the vaccinated and non-vaccinated groups (P < 0.0001). The positive rates of B1 gene in brain tissue of all immunized mice challenged by 10 and 40 cysts were 60%, suggesting that although most immunized mice brains were infected with T. gondii, the parasites failed to form brain cysts (Additional file 4: Figure S3 and Additional file 5: Table S2). These results suggest that immunization with PruΔgra72 tachyzoites reduces the brain cyst burden of chronically T. gondii-infected mice.
Immunization with PruΔgra72 provides long-term protection against T. gondii infection
To further investigate whether vaccination with PruΔgra72 provides long-term protection against T. gondii infection in mice, three genotypes of T. gondii tachyzoites with different virulence (Type I RH strain, Type II Pru strain and ToxoDB#9 PYS strain) were intraperitoneally injected into Kunming mice at 120 dpv to observe their clinical symptoms and survival rates for 30 days (Fig. 3). While all non-immunized mice were killed when challenged with the same dose of tachyzoites of PYS or Pru strains (Fig. 5a–c), the immunized mice showed 100% survival rates when challenged with 102 PYS or 5 × 104 Pru tachyzoites (Fig. 5a, c). When challenged by 103 tachyzoites of the PYS strain, only one mouse in the immunized group died on the 21st day, maintaining a high survival rate of 83.3% (Fig. 5b). However, PruΔgra72 vaccination did not effectively protect against challenge infection with the virulent RH strain, and the immunized mice challenged with 102 tachyzoites of the RH strain displayed a survival rate of only 16.7%, and all mice challenged by 103 tachyzoites of the RH strain succumbed to the infection (Fig. 5d–e). Despite the relatively low survival rates compared to that in mice groups challenged with PYS or Pru strains, PruΔgra72 vaccination still extended the survival time of mice challenged with the RH strain.
Immunization with PruΔgra72 induced enduring protection against Toxoplasma gondii infection by tachyzoites and cysts. a–e Mice were challenged with 102 or 103 tachyzoites of the ToxoDB#9 PYS strain, 5 × 104 tachyzoites of the Type II Pru strain or 102 or 103 tachyzoites of the Type I RH strain at 120 days post-vaccination (dpv). Clinical symptoms and survival statuses were recorded for 30 days (n = 6 mice per group). ***P < 0.001, **P < 0.01. f Brain cyst numbers in mice infected with 5 × 104 Pru tachyzoites at 30 days after infection and mice infected with 5 × 102 Pru tachyzoites served as the control group. ****P < 0.0001. The survival rates of mice orally administered 10 cysts (g) or 40 cysts (h) were recorded over a 1-month period (n = 10 mice per group). ****P < 0.0001, ***P < 0.001. i Brain cyst burden was quantified at 30 days post-infection from both non-immunized and immunized and surviving mice. ****P < 0.0001
For assessment of long-term protection against T. gondii cyst infection, 10 or 40 cysts were used to orally infect the naive and immunized mice (Fig. 3). The immunized group displayed high survival rates of 90% and 100%, respectively, while the survival rates of the naive group challenged with 10 and 40 Pru cysts were 20% and 0% (Fig. 5g–h). The surviving naive mice had an average brain cyst burden of 604 ± 186, while the immunized group challenged with 10 and 40 cysts had brain cyst burdens of 6 ± 13 and 4 ± 6 per brain, respectively (Fig. 5i). The positivity rates of brain B1 gene in these surviving mice were 66.7% and 80%, respectively (Additional file 4: Figure S3 and Additional file 5: Table S2), showing an increase compared to that at 60 dpv, which may possibly have resulted from the decreased resistance to cysts due to the prolonged immunization time. These results indicate that PruΔgra72 vaccination could not provide complete defense against infection with tachyzoites of the virulent RH strain but can offer long-term protection against low-virulent T. gondii tachyzoites and cyst-induced chronic infections.
Vaccination stimulates a notable specific immune response
To characterize the immunogenicity of PruΔgra72 vaccination, serum samples were collected at 45, 60, 90 and 120 dpv to monitor levels of T. gondii-specific IgG and IgG subclasses by quantitative ELISA (Fig. 3). The results showed that PruΔgra72 vaccination induced significantly high levels of anti-T. gondii-specific IgG and IgG subclasses (IgG1 and IgG2a) in mice at all time points compared to that of the naive mice (Fig. 6a–c). Furthermore, IgG2a level was significantly higher than IgG1 level in all vaccination time points (Additional file 6: Figure S4a). These results demonstrated that PruΔgra72 vaccination induces balanced Th1 and Th2 responses, with a predilection towards Th1 dominance.
PruΔgra72 vaccination elicits Th1/Th2-type immune responses in mice. a–c The IgG (a), IgG1 (b) and IgG2a (c) levels of the sera from the immunized and naive mice collected at 45, 60, 90 and 120 days post-vaccination (dpv) (n = 6 mice per group). Mice immunized with PruΔgra72 displayed significantly elevated levels of IgG and IgG subclasses compared to the control group. ****P < 0.0001, ***P < 0.001. d–h The Th1 and Th2 cytokine levels of the splenocytes from the immunized and naive mice collected at 45, 60, 90 and 120 dpv, including IL-2 (d), IL-4 (e), IL-10 (f) and IL-12 (g) and IFN-γ (h) (n = 6 mice per group). ****P < 0.0001, ***P < 0.001, **P < 0.01, *P < 0.05. ns indicates no statistical significance
To further elucidate the immune response, splenocytes of the immunized and naive mice collected at 45, 60, 90 or 120 dpv were cultured in vitro and stimulated with STAg to detect cytokines by ELISA (Fig. 3). Th1-type cytokines (IL-2, IL-12 and IFN-γ) and Th2-type cytokines (IL-4 and IL-10) were significantly upregulated by PruΔgra72 vaccination at all time points, except IL-12 level at 120 dpv (Fig. 6d–h). The level of IFN-γ was the most prominent among all examined cytokines, significantly surpassing that of other cytokines such as IL-2, IL-4, IL-10 and IL-12 (Additional file 6: Figure S4b–e).
Discussion
In recent years, numerous GRAs have been proven as promising candidate proteins for developing T. gondii vaccines. Among them, GRA7 can be used to develop a DNA vaccine to trigger a strong antibody response and higher levels of IFN-γ [36]. The recombinant protein GRA12 enclosed in PLGA nanoparticles shows effectiveness as a vaccine against acute toxoplasmosis [37]. The live-attenuated RHΔgra17 induces high levels of Th1 and Th2 cell-mediated immune responses and provides some degree of protection against homologous and heterologous virulent strains in mice [38].
Previous studies have indicated the significance of the novel GRA72 in modulating the permeability of the PVM and its association with the growth of T. gondii [26, 27]. Gene knockout strains like PruΔgra72 or ME49Δgra72 exhibit reduced virulence in mice, suggesting their potential as live-attenuated vaccines. In this study, virulence assays showed that Kunming mice survived after infection with even 5 × 107 PruΔgra72 tachyzoites, with slight clinical symptoms of toxoplasmosis, but no brain cysts were observed. Additionally, deletion of the gra72 gene in the Pru strain significantly reduced parasite load in organs of the infected mice. The PruΔgra72 strain has the potential as a toxoplasmosis vaccine candidate.
Studies of genetic diversity of T. gondii isolates have revealed the existence of around 300 different genotypes; some of them are quite different in their virulence to mice [4,5,6, 39]. In our study, we found that PruΔgra72 vaccination fully protected mice against attacks by Type II Pru strain and ToxoDB#9 PYS strain and prolonged the survival time of mice infected by Type I RH strain. These results indicated that PruΔgra72 can protect mice against acute infection by low-virulent T. gondii strains. Currently, less virulent candidate vaccine strains such as ME49Δcdpk3, PruΔgra76 and RHΔtkl1 have been evaluated for their protective efficacy against tachyzoite infection using mouse models [16, 17, 40]. Among them, ME49Δcdpk3 and PruΔgra76 did not provide 100% protection against the highly virulent RH strain, similar to PruΔgra72 [17, 40]. However, RHΔtkl1 offers sufficient protection for mice against Type I RH or ToxODB#9 (PYS or TGC7) tachyzoites, in which all RHΔtkl1-immunized mice survived the challenge infection of tachyzoites of the highly virulent Type I RH strain [16]. Immunization with T. gondii uracil auxotrophs, which were completely avirulent because of the lack of carbamoyl phosphate synthetase II (CPSII) gene, induces long-term protective immunity against RH strain in mice [41].
The persistent presence of cysts containing T. gondii bradyzoites causes chronic infection, posing substantial health risks to the host [42]. We simulated the chronic infection in mice by orally administering Pru cysts at 60 or 120 dpv. The results showed that PruΔgra72 vaccination significantly improved the survival rates and decreased the brain cyst burden of mice chronically infected by Pru cysts. The effective protection against chronic T. gondii infection might be associated with the strong humoral and cellular immune responses elicited in mice by the vaccination, in which the Th1 response has been shown to be beneficial in both the clearance of tachyzoites during the acute phase and the suppression of cyst formation [43, 44]. Consequently, vaccination with PruΔgra72 can effectively combat low-virulent strains and chronic infections. Nonetheless, it is imperative to acknowledge the study’s limitations, notably the absence of assessment regarding congenital infections and chronic infection by oocysts, two important T. gondii infection routes, which warrants further investigation.
Immune response skewed towards Th1 has advantages in enhancing the host defense against T. gondii [43, 44]. Consistent with results of previous studies of live-attenuated vaccines, such as ME49Δcdpk3, ME49Δα-amy and RHΔompdcΔuprt [17, 33, 35], mice administered PruΔgra72 displayed sustained and elevated levels of IgG and IgG subclass antibodies at 45, 60, 90 and 120 dpv. Despite a marked increase in both IgG1 and IgG2a levels in immunized mice compared to that of the non-immunized mice, IgG2a levels were significantly higher than IgG1 levels, suggesting a prevailing Th1 response among the coexistence of Th1 and Th2 immune reactions in mice vaccinated with PruΔgra72, consistent with previous findings [35, 38]. These antibodies may proficiently obstruct the host cell invasion by the parasites, opsonize the parasites through phagocytosis mechanisms and activate the classical complement pathway to effectively defend against T. gondii [8].
IL-12 and IFN-γ exert pivotal roles in driving Th1 cell-mediated immunity and are essential cytokines for controlling parasitic infections [42, 45]. Mice lacking the IFN-γ gene or receptor are vulnerable to death after T. gondii infection [42]. IL-2 is an additional key factor in the protective response [8]. In this study, the levels of IFN-γ and IL-2 detected in the splenocyte supernatants were significantly increased by PruΔgra72 vaccination. The increased expression level of cytokines might play important roles in immune protection, enabling the mice to resist T. gondii infections. Previous studies have shown a significant correlation between IFN-γ and IgG2a antibody production [46]. This is consistent with our results as the level of IgG2a is significantly higher than that of IgG1. Similarly, the level of IFN-γ is also significantly higher than that of other cytokines. In mice, both cellular and humoral immune responses tend to skew towards a Th1-type response.
Excessive immune responses pose a potential threat; therefore, regulating host-specific immunity is crucial for the overall survival of the host [47]. IL-10 plays a key role in alleviating tissue damage caused by strong Th1-type responses, inhibiting lymphocytes from secreting IFN-γ, while IL-4 also plays a similar role [42]. Our study found that the levels of Th2-type anti-inflammatory cytokines (IL-4 and IL-10) were elevated after PruΔgra72 vaccination, which may alleviate the increase of pro-inflammatory mediators and reduce collateral damage to the mice and help to better regulate Th1-type cytokines.
In addition to live attenuated T. gondii vaccines, DNA vaccines and protein vaccines have also been investigated in animal models. Consistent with immune responses induced by live attenuated vaccines, several DNA or protein vaccines also induce Th1-type cellular and humoral immune response, such as the DNA vaccine expressing heat shock protein 40 (HSP40) [48], a double C2 domain protein (DOC2) or rhoptry protein 9 (ROP9) [49, 50], protein vaccine of recombinant extracellular signal-regulated kinases 7 (ERK7) or calcium-dependent protein kinase 1 (CDPK1) [51, 52]. However, protection against T. gondii induced by these DNA or protein vaccines was not 100% because of incomplete protective immunity induced by single or multiple genes/proteins. In the present study, although significant protection against T. gondii in mice was induced by PruΔgra72 vaccination, this live attenuated PruΔgra72 vaccine may be practically useful for food-producing animals and cats, but not for humans, because of its resistance to pyrimethamine.
Conclusions
The findings of our study showed that PruΔgra72 vaccination triggers the host immune responses, eliciting a balanced Th1/Th2 immune reaction that confers long-lasting immunity against both mild and relatively virulent T. gondii strains, resulting in the prolonged survival time, improved survival rates and decreased brain cyst burden. As such, PruΔgra72 represents a promising candidate as a potentially live-attenuated vaccine. Nevertheless, the mouse model in this study showcases the immunogenicity and effectiveness of PruΔgra72; further assessment in diverse susceptible and economically important animal models is imperative to ascertain its safety and efficacy. Furthermore, despite the effective protection against chronic infection displayed by PruΔgra72 immunization, the persistence of brain cysts remains a concern. Low level protection against infection by tachyzoites of the highly virulent RH strain warrants continued research to advance the development of live-attenuated vaccines against T. gondii.
Availability of data and materials
The datasets supporting the findings of this article are included within the paper and its supplementary materials.
Abbreviations
- PV:
-
Parasitophorous vacuole
- IgG:
-
Immunoglobulin G
- IL-2:
-
Interleukin-2
- IL-12:
-
Interleukin-12
- IFN-γ:
-
Interferon-γ
- IL-4:
-
Interleukin-4
- IL-10:
-
Interleukin-10
- GRAs:
-
Dense granule proteins
- IVN:
-
Intravacuolar network
- PVM:
-
Parasitophorous vacuole membrane
- HFF:
-
Human foreskin fibroblast
- DMEM:
-
Dulbecco’s Modified Eagle Medium
- FBS:
-
Fetal bovine serum
- qPCR:
-
Quantitative polymerase chain reaction
- dpi:
-
Days post-infection
- dpv:
-
Days post-vaccination
- STAg:
-
Soluble T. gondii antigen
- ELISA:
-
Enzyme-linked immunosorbent assay
- PBST:
-
Phosphate buffered saline with tween
- BSA:
-
Bovine serum albumin
- TMB:
-
3, 3′, 5, 5′-Tetramethylbenzidine
- OD:
-
Optical density
References
Lourido S. Toxoplasma gondii. Trends Parasitol. 2019;35:944–5.
Elsheikha HM, Marra CM, Zhu XQ. Epidemiology, pathophysiology, diagnosis, and management of cerebral toxoplasmosis. Clin Microbiol Rev. 2021;34:e00115-e119.
Mulu Gelaw Y, Worku Dagnew G, Degu Alene G, Gangneux JP, Robert-Gangneux F. Toxoplasma gondii seroprevalence among pregnant women in Africa: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2024;18:e0012198.
Su C, Khan A, Zhou P, Majumdar D, Ajzenberg D, Dardé ML, et al. Globally diverse Toxoplasma gondii isolates comprise six major clades originating from a small number of distinct ancestral lineages. Proc Natl Acad Sci U S A. 2012;109:5844–9.
Shwab EK, Zhu XQ, Majumdar D, Pena HFJ, Gennari SM, Dubey JP, et al. Geographical patterns of Toxoplasma gondii genetic diversity revealed by multilocus PCR-RFLP genotyping. Parasitology. 2014;141:453–61.
Liu Q, Wang ZD, Huang SY, Zhu XQ. Diagnosis of toxoplasmosis and typing of Toxoplasma gondii. Parasit Vectors. 2015;8:292.
Lima TS, Lodoen MB. Mechanisms of human innate immune evasion by Toxoplasma gondii. Front Cell Infect Microbiol. 2019;9:103.
Wang JL, Zhang NZ, Li TT, He JJ, Elsheikha HM, Zhu XQ. Advances in the development of anti-Toxoplasma gondii vaccines: challenges, opportunities, and perspectives. Trends Parasitol. 2019;35:239–53.
Dunay IR, Gajurel K, Dhakal R, Liesenfeld O, Montoya JG. Treatment of toxoplasmosis: historical perspective, animal models, and current clinical practice. Clin Microbiol Rev. 2018;31:e00057-e117.
Zou J, Huang XX, Yin GW, Ding Y, Liu XY, Wang H, et al. Evaluation of Toxoplasma gondii as a live vaccine vector in susceptible and resistant hosts. Parasit Vectors. 2011;4:168.
Hiszczyńska-Sawicka E, Gatkowska JM, Grzybowski MM, Długońska H. Veterinary vaccines against toxoplasmosis. Parasitology. 2014;141:1365–78.
Mévélec MN, Lakhrif Z, Dimier-Poisson I. Key limitations and new insights into the Toxoplasma gondii parasite stage switching for future vaccine development in human, livestock, and cats. Front Cell Infect Microbiol. 2020;10:607198.
Li Y, Zhou H. Moving towards improved vaccines for Toxoplasma gondii. Expert Opin Biol Ther. 2018;18:273–80.
Buxton D, Thomson K, Maley S, Wright S, Bos HJ. Vaccination of sheep with a live incomplete strain (S48) of Toxoplasma gondii and their immunity to challenge when pregnant. Vet Rec. 1991;129:89–93.
Hill D, Dubey JP. Toxoplasma gondii: transmission, diagnosis and prevention. Clin Microbiol Infect. 2002;8:634–40.
Wang JL, Liang QL, Li TT, He JJ, Bai MJ, Cao XZ, et al. Toxoplasma gondii tkl1 deletion mutant is a promising vaccine against acute, chronic, and congenital toxoplasmosis in mice. J Immunol. 2020;204:1562–70.
Wu M, Liu S, Chen Y, Liu D, An R, Cai H, et al. Live-attenuated ME49Δcdpk3 strain of Toxoplasma gondii protects against acute and chronic toxoplasmosis. NPJ Vaccines. 2022;7:98.
Liang QL, Sun LX, Elsheikha HM, Cao XZ, Nie LB, Li TT, et al. RHΔgra17Δnpt1 strain of Toxoplasma gondii elicits protective immunity against acute, chronic and congenital toxoplasmosis in mice. Microorganisms. 2020;8:352.
Blader IJ, Coleman BI, Chen CT, Gubbels MJ. Lytic cycle of Toxoplasma gondii: 15 Years Later. Annu Rev Microbiol. 2015;69:463–85.
Wang Y, Cirelli KM, Barros PDC, Sangaré LO, Butty V, Hassan MA, et al. Three Toxoplasma gondii dense granule proteins are required for induction of Lewis rat macrophage pyroptosis. Mbio. 2019;10:e02388-18.
Nadipuram SM, Kim EW, Vashisht AA, Lin AH, Bell HN, Coppens I, et al. In vivo biotinylation of the Toxoplasma parasitophorous vacuole reveals novel dense granule proteins important for parasite growth and pathogenesis. Mbio. 2016;7:e00808-16.
Braun L, Brenier-Pinchart MP, Yogavel M, Curt-Varesano A, Curt-Bertini RL, Hussain T, et al. A Toxoplasma dense granule protein, GRA24, modulates the early immune response to infection by promoting a direct and sustained host p38 MAPK activation. J Exp Med. 2013;210:2071–86.
Shi Y, Li J, Yang W, Chen J. Protective immunity induced by DNA vaccine containing TgGRA35, TgGRA42, and TgGRA43 against Toxoplasma gondii infection in Kunming mice. Front Cell Infect Microbiol. 2023;13:1236130.
Xu XP, Liu WG, Xu QM, Zhu XQ, Chen J. Evaluation of immune protection against Toxoplasma gondii infection in mice induced by a multi-antigenic DNA vaccine containing TgGRA24, TgGRA25 and TgMIC6. Parasite. 2019;26:58.
Zhu Y, Xu Y, Hong L, Zhou C, Chen J. Immunization with a DNA vaccine encoding the Toxoplasma gondii’ s GRA39 prolongs survival and reduce brain cyst formation in a murine model. Front Microbiol. 2021;12:630682.
Zheng XN, Li TT, Elsheikha HM, Wang M, Sun LX, Wu XJ, et al. GRA47 is important for the morphology and permeability of the parasitophorous vacuole in Toxoplasma gondii. Int J Parasitol. 2024;25:S0020-7519(24)00135-8. https://doi.org/10.1016/j.ijpara.2024.06.003.
Tachibana Y, Hashizaki E, Sasai M, Yamamoto M. Host genetics highlights IFN-γ-dependent Toxoplasma genes encoding secreted and non-secreted virulence factors in in vivo CRISPR screens. Cell Rep. 2023;42:112592.
Bitew MA, Gaete PS, Swale C, Maru P, Contreras JE, Saeij JPJ. Two Toxoplasma gondii putative pore-forming proteins, GRA47 and GRA72, influence small molecule permeability of the parasitophorous vacuole. Mbio. 2024;15:e0308123.
Paredes-Santos TC, Bitew MA, Swale C, Rodriguez F, Krishnamurthy S, Wang Y, et al. Genome-wide CRISPR screen identifies genes synthetically lethal with GRA17, a nutrient channel encoding gene in Toxoplasma. PLoS Pathog. 2023;19:e1011543.
Zhang NZ, Wang M, Xu Y, Petersen E, Zhu XQ. Recent advances in developing vaccines against Toxoplasma gondii: an update. Expert Rev Vaccines. 2015;14:1609–21.
Zhang NZ, Xu Y, Wang M, Petersen E, Chen J, Huang SY, et al. Protective efficacy of two novel DNA vaccines expressing Toxoplasma gondii rhomboid 4 and rhomboid 5 proteins against acute and chronic toxoplasmosis in mice. Expert Rev Vaccines. 2015;14:1289–97.
Wang JL, Li TT, Elsheikha HM, Liang QL, Zhang ZW, Wang M, et al. The protein phosphatase 2A holoenzyme is a key regulator of starch metabolism and bradyzoite differentiation in Toxoplasma gondii. Nat Commun. 2022;13:7560.
Yang J, Yang C, Qian J, Li F, Zhao J, Fang R. Toxoplasma gondii α-amylase deletion mutant is a promising vaccine against acute and chronic toxoplasmosis. Microb Biotechnol. 2020;13:2057–69.
Li TT, Wang JL, Liang QL, Sun LX, Zhang HS, Zhang ZW, et al. Effect of deletion of gra17 and gra23 genes on the growth, virulence, and immunogenicity of type II Toxoplasma gondii. Parasitol Res. 2020;119:2907–16.
Shen Y, Zheng B, Sun H, Wu S, Fan J, Ding J, et al. A live attenuated RHΔompdcΔuprt mutant of Toxoplasma gondii induces strong protective immunity against toxoplasmosis in mice and cats. Infect Dis Poverty. 2023;12:60.
Jongert E, de Craeye S, Dewit J, Huygen K. GRA7 provides protective immunity in cocktail DNA vaccines against Toxoplasma gondii. Parasite Immunol. 2007;29:445–53.
Sun HC, Deng PM, Fu Y, Deng JH, Xie RH, Huang J, et al. Protective efficacy of Toxoplasma gondii GRA12 or GRA7 recombinant proteins encapsulated in PLGA nanoparticles against acute Toxoplasma gondii infection in mice. Front Cell Infect Microbiol. 2023;13:1209755.
Wang JL, Elsheikha HM, Zhu WN, Chen K, Li TT, Yue DM, et al. Immunization with Toxoplasma gondii GRA17 deletion mutant induces partial protection and survival in challenged mice. Front Immunol. 2017;8:730.
Galal L, Ariey F, Gouilh MA, Dardé ML, Hamidović A, Letourneur F, et al. A unique Toxoplasma gondii haplotype accompanied the global expansion of cats. Nat Commun. 2022;13:5778.
Zheng XN, Sun LX, Elsheikha HM, Li TT, Gao J, Wu XJ, et al. A newly characterized dense granule protein (GRA76) is important for the growth and virulence of Toxoplasma gondii. Int J Parasitol. 2024;54:109–21.
Fox BA, Bzik DJ. De novo pyrimidine biosynthesis is required for virulence of Toxoplasma gondii. Nature. 2002;415:926–9.
Pittman KJ, Knoll LJ. Long-term relationships: the complicated interplay between the host and the developmental stages of Toxoplasma gondii during acute and chronic infections. Microbiol Mol Biol Rev. 2015;79:387–401.
Wu M, An R, Chen Y, Chen T, Wen H, Yan Q, et al. Vaccination with recombinant Toxoplasma gondii CDPK3 induces protective immunity against experimental toxoplasmosis. Acta Trop. 2019;199:105148.
Zhang NZ, Gao Q, Wang M, Elsheikha HM, Wang B, Wang JL, et al. Immunization with a DNA vaccine cocktail encoding TgPF, TgROP16, TgROP18, TgMIC6, and TgCDPK3 genes protects mice against chronic toxoplasmosis. Front Immunol. 2018;9:1505.
Yarovinsky F. Innate immunity to Toxoplasma gondii infection. Nat Rev Immunol. 2014;14:109–21.
Snapper CM, Peschel C, Paul WE. IFN-gamma stimulates IgG2a secretion by murine B cells stimulated with bacterial lipopolysaccharide. J Immunol. 1988;140:2121–7.
Mordue DG, Monroy F, La Regina M, Dinarello CA, Sibley LD. Acute toxoplasmosis leads to lethal overproduction of Th1 cytokines. J Immunol. 2001;167:4574–84.
Li ZY, Lu J, Zhang NZ, Chen J, Zhu XQ. Immune responses induced by HSP60 DNA vaccine against Toxoplasma gondii infection in Kunming mice. Korean J Parasitol. 2018;56:237–45.
Zhang NZ, Gao Q, Wang M, Hou JL, Zhang FK, Hu LY, et al. Protective efficacy against acute and chronic Toxoplasma gondii infection induced by immunization with the DNA vaccine TgDOC2C. Front Microbiol. 2018;9:2965.
Chen J, Zhou DH, Li ZY, Petersen E, Huang SY, Song HQ, et al. Toxoplasma gondii: protective immunity induced by rhoptry protein 9 (TgROP9) against acute toxoplasmosis. Exp Parasitol. 2014;139:42–8.
Li ZY, Guo HT, Calderón-Mantilla G, He JJ, Wang JL, Bonev BB, et al. Immunostimulatory efficacy and protective potential of putative TgERK7 protein in mice experimentally infected by Toxoplasma gondii. Int J Med Microbiol. 2020;310:151432.
Huang SY, Chen K, Wang JL, Yang B, Zhu XQ. Evaluation of protective immunity induced by recombinant calcium-dependent protein kinase 1 (TgCDPK1) protein against acute toxoplasmosis in mice. Microb Pathog. 2019;133:103560.
Acknowlegment
Not applicable.
Funding
This work was supported by the Shanxi Provincial Key Research and Development Program, China (grant no. 2022ZDYF126), Shanxi Provincial Agricultural and Rural Research Program, China (grant no. LXXMsxnd202101), the Science and Technology Innovation Program of Shanxi Agricultural University (grant no. 2023BQ26), the Research Fund of Shanxi Province for Introduced High-level Leading Talents (grant no. RFSXIHLT202101) and the Special Research Fund of Shanxi Agricultural University for High-level Talents (grant no. 2021XG001).
Author information
Authors and Affiliations
Contributions
XNZ and XQZ conceived and designed the study. JL and XNZ performed the experiments, analyzed the data and wrote the manuscript. YK, ZXW, SFY and YYT participated in the implementation of the study. XNZ and XQZ critically revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The protocols and procedures used in the present study involving animal experiments were approved by the Institutional Animal Care and Use Committee of Shanxi Agricultural University (approval no. SXAU-EAW-2021XM121001). The animals were handled in accordance with good animal practices required by the Animal Ethics Procedures and Guidelines of the People′ s Republic of China.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
13071_2024_6461_MOESM1_ESM.tif
Additional file 1: Figure S1. Generation of the gra72 knockout strain in Type II Pru strain of Toxoplasma gondii. (a) Schematic illustration of constructing the mutant strain using CRISPR/Cas9-mediated homologous recombination to disrupt the gra72 gene and replace the conding sequence with a DHFR cassette conferring resistance to pyrimethamine. (b) PCR identification of PruΔgra72 knockout strain. PCR1 and PCR3 were utilized to discern the integration of 5′ and 3′ homologous DHFR cassette targeting the gra72 gene, while PCR2 was employed to validate the successful knockout of gra72. (c) Morphological characterization of the PVs fromed by PruΔgra72 and Pru tachyzoites in HFF cells at 60 h post-infection. In comparison to the wild-type Pru strain, the PruΔgra72 exhibited a “bubble” morphology of PVs. Scale bars, 10 µm.
13071_2024_6461_MOESM2_ESM.tif
Additional file 2: Figure S2. The results of PCR targeting B1 gene in brain tissues of mice infected with 2 × 102 (a), 5 × 102 (a), 5 × 103 (b), 5 × 104 (b), 5 × 105 (c), 5 × 106 (c) and 5 × 107 (d) PruΔgra72 tachyzoites, showing an increasing positivey rate for Toxoplasma gondii infection with higher infective doses. A1–8, results from the surviving mice infected with 2 × 102 PruΔgra72 tachyzoites; B1–8, results from the surviving mice infected with 5 × 102 PruΔgra72 tachyzoites; C1–8, results from the surviving mice infected with 5 × 103 PruΔgra72 tachyzoites; D1–8, results from the surviving mice infected with 5 × 104 PruΔgra72 tachyzoites; E1–8, results from the surviving mice infected with 5 × 105 PruΔgra72 tachyzoites; F1–8, results from the surviving mice infected with 5 × 106 PruΔgra72 tachyzoites; G18, results from the surviving mice– infected with 5 × 107 PruΔgra72 tachyzoites. P, positive control; N, negative control.
13071_2024_6461_MOESM3_ESM.pdf
Additional file 3: Table S1. Brain cyst burden and B1 gene detection results in mice infected with Pru or PruΔgra72 tachyzoites in virulence assays.
13071_2024_6461_MOESM4_ESM.tif
Additional file 4: Figure S3. The results of PCR targeting B1 gene in brain tissues of mice immunized with PruΔgra72 and challenged with Pru tachyzoites (a) and cysts (b–c). A1–6, results from the surviving mice challenged with 5 × 104 Pru tachyzoites at 60 days post-vaccination (dpv); B1–6, results from the surviving mice challenged with 5 × 104 Pru tachyzoites at 120 dpv; C1–10, results from the surviving mice challenged with 10 cysts at 60 dpv; D1–10, results from the surviving mice challenged with 40 cysts at 60 dpv; E1–9, results from the surviving mice challenged with 10 cysts at 120 dpv; F1–10, results from the surviving mice challenged with 40 cysts at 120 dpv. P, positive control; N, negative control.
13071_2024_6461_MOESM5_ESM.pdf
Additional file 5: Table S2. Brain cyst burden and B1 gene detection results in mice immunized with PruΔgra72 and challenged with Pru tachyzoites or cysts.
13071_2024_6461_MOESM6_ESM.tif
Additional file 6: Figure S4. Levels of IgG2a antibodies in the PruΔgra72-immunized mouse group were significantly higher than levels of IgG1 antibodies at 45, 60, 90 and 120 days post-vaccination (dpv) (a). ****P < 0.0001. Level of IFN-γ significantly surpasses that of other cytokines (IL-2, IL-4, IL-10 and IL-12) at 45, 60, 90 and 120 dpv (b–e). ****P < 0.0001, ***P < 0.001.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Kang, Y., Wu, ZX. et al. Live-attenuated PruΔgra72 strain of Toxoplasma gondii induces strong protective immunity against acute and chronic toxoplasmosis in mice. Parasites Vectors 17, 377 (2024). https://doi.org/10.1186/s13071-024-06461-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-024-06461-9