Abstract
Introduction
Opportunistic infections (OIs) are more common and severe among people with suppressed immunity like those living with HIV/AIDS (PLWH). This study aimed to assess the prevalence of OIs and associated factors among PLWH attending antiretroviral therapy (ART) clinics in the Gedeo zone, Southern Ethiopia.
Methods
A facility based retrospective cohort study was conducted from April to June 2018 among PLWH attending ART clinics in Gedeo zone, Ethiopia from November 2016 – November 2017. A simple random sampling method was used to select the both paper based and electronic study participants’ charts. Adjusted odds ratios were calculated using multivariable logistic regression analysis for variables statistically significant at 95% confidence interval under bivariable logistic regression analysis, and significance was declared at P < 0.05.
Results
a total of 266 PLWH attended the selected ART clinics of Gedeo zone during the one year period were participated in the current study. The majority 104(39.1%) were within the age group 30–39, 106(60.2%) male, 184(69.2%) married, and 167(62.9%) urban residents. The study revealed the prevalence of OIs was 113(42.5%) with oral candidiasis 28(24.5%) the most prevalent followed by pulmonary tuberculosis 22(19.5%) and herpes zoster 15(13.4%). Further, study participants with ambulatory [AOR = 2.40(95% CI: 1.14, 5.03)], and bedridden [AOR = 3.27(95% CI:1.64, 6.52)] working functional status; with lower CD4 count: less than 200cells/mm3 [AOR = 9.14(95% CI: 2.75, 30.39)], 200–350cells/mm3 [AOR = 9.45(95% CI: 2.70,33.06)], 351-500cells/mm3 [AOR = 5.76(95% CI: 1.71, 19.39)]; being poor in ART adherence level [AOR = 10.05(95% CI: 4.31,23.46)]; being in stage III/IV WHO clinical stage of HIV/AIDS [AOR = 2.72(95% CI: 1.42, 5.20)]; and being chewing khat [AOR = 2.84(95% CI: 1.21, 6.65)] were found positively predicting the occurrence of OIs.
Conclusion
This study speckled a high prevalence of OIs with several predicting factors. Therefore, the study acmes there should be interventional means which tackles the higher prevalence of OIs with focus to the predicting factors like lower CD4 count level, less/bedridden working functional status, poor ART adherence level, advanced stage of HIV/AIDS stage and chewing khat.
Similar content being viewed by others
Introduction
Acquired Immunodeficiency Syndrome (AIDS) is a disease of immune system caused by Human Immune-deficiency Virus (HIV), and when left untreated/unsuccessfully treated, could be world’s most serious public health problems. According to the World Health Organization report, globally, at the end of 2021, there were about 38.4 million people living with HIV/AIDS, disproportionately affected the African region [1] including Ethiopia for instance, among 609,349 people were living with HIV/AIDS with 10,567 new infections, about 10,000 HIV/AIDS related deaths were recorded in 2022 [2].
OIs are infections that are more frequent or more severe due to immune suppression, which are principal cause of morbidity and mortality among PLWH [3]. In resource-limited settings, HIV/AIDS-related OIs are responsible for 90% of morbidity and mortality [4, 5] and are reason for the over 20% of hospital admissions [6]. Despite its drastic decrease since the introduction of ART, it is still high in developing countries [7]. For instance in Vietnam is 11.45% [8], Uganda, 27.5% [9], and Nigeria 22.4% [10], and in Ethiopia ranges from 7.5 to 88.4% [11,12,13,14,15,16,17] with regional distribution 7.5–55.3% in the northern [13, 15,16,17], 8.97–88.4% in the southern [12, 18, 19], 33.6% in Addis Ababa [14], and 48% in Eastern part of Ethiopia [11].
Pulmonary tuberculosis is the most common OI observed in different local and international studies [4, 8, 11,12,13,14, 16, 19] followed by oral candidiasis [4, 11,12,13, 16, 17, 19] and Herpes zoster [11, 15]. Further, helminthes [4], diarrhea [4, 13, 17], pneumonia [12, 16] and toxoplasmosis [16] were also observed among PLWH on ART. Furthermore, CD4 cell count < 200 cells/mm3 [11,12,13, 20], HIV/AIDS clinical stage III and IV [11,12,13,14,15, 17], low hemoglobin level [12, 16, 17], non/poor-adherence level to ART drug [12, 16, 17], not using prophylaxis [11], bedridden functional status [16], high viral load (≥ 1000 copies/ml) [21], previous history of OIs [16, 20], low literacy level [15], history of smoking [20] and chewing khat [17] have been reported as associated with the occurrence of OIs among these populations. Additionally, the prevalence of helminthes, candidiasis, diarrheal, bacterial pneumonia, and genital ulcer disease were reported as consistently higher in women while TB and Kaposi’s sarcoma were higher among men [4]. In fact, literatures also revealed that, prevalence of OIs are higher among older age groups usually in over thirty years [4, 17].
Further, even though, Gedeo zone implemented the new HIV treatment protocol [5, 22,23,24] since November 2016, a month after World Health Organization launched the program, no study was conducted to summarize the overall prevalence of OIs in the zone with regard to measure the impact of the new HIV treatment program. This study assessed the prevalence of OIs and associated factors among adult PLWH on ART in Gedeo Zone, Southern Ethiopia, by including factors like adherence level of PLWH to ART drug and duration since diagnosed for the disease, which were bypassed by most related studies.
Therefore, this study provides summarized information about the extent of OIs among PLWH which provides baseline data and identify potential risk factors for its acquisition, which helps policymakers and program managers mainstreaming HIV/AIDS activities.
Materials and methods
Study design, study setting, and period
A facility based retrospective cohort study was employed from April 1 to June 1 2018 among PLWH attending ART clinics in Gedeo zone, Ethiopia from November 2016 – November 2017. Gedeo zone is located 360 km from Addis Ababa in the southern part of Ethiopia. The total population of the zone is 1,139,429. Among a total of 38 health institutions, six health centers: Haroresa, Yirgachefe, Wonago, Bule, Gedeb, Chelelekitu, and Dila University Referral Hospitals providing comprehensive ART services were purposely included in this study.
Sample size calculation, participants, and their recruitment method
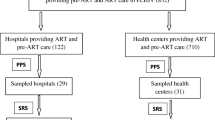
We computed the required sample size using a single population formula based on assumptions: previous estimates of OIs among PLWH [19], absolute precision of 5%, and Zα/2 = 1.96 at 95% confidence interval (CI), 10% contingency for charts to be excluded due to incomplete information’s, the final sample size calculated was 266.
The inclusion follows charts of PLWH whose age was at least 18 years, and attended the selected ART clinics from November 2016 to November 2017 with full information intended by this study. Then, simple sampling method was used to select the both paper and electronic based charts based on the proportion of PLWH attended the selected ART clinics within determined one year (November 2016 to 2017).
Study variables and its measurement methods
The outcome variable of this study was the prevalence of OIs among PLWH. PLWH with any of infections like Cervical Cancer, Chronic Diarrhea, Cryptococci Meningitis, Esophageal Candidacies, Extra Pulmonary TB, Herpes Zoster, Kaposi’s sarcoma, Lymphoma, Oral Candidacies, Pneumocystis Carinii Pneumonia (PCP), Pulmonary TB, Recurrent Bacterial Pneumonia and Toxoplasmosis of the CNS were considered as having OIs. The information on the outcome variable, socio-demographic, background, and clinical characteristics were obtained by reviewing recent information sheets of the charts of PLWH attended the selected hospitals within the determined one year period. The data extraction checklist was developed from the patient registration form for HIV/AIDS care and ART clinic intake of the Federal Ministry of Health (FMOH) and previous studies [17, 25, 26]. The quality of the data was ensured by using pre-tested and refined checklists and collected by trained data collectors and supervisors.
Statistical methods
Data collected was checked for completeness, consistency, codded and entered into Epi Data version 4.2 and exported to SPSS version 23 for analysis. Before analysis, the data were arranged, edited, and cleaned by running simple frequencies and cross-tabulations. In order to manage confounding variables, variables that were shown statistically significant with the occurrence level of OIs at P < 0.05 under bivariable logistic regression analysis were reexamined using multivariable logistic regression analysis, and those variables with P < 0.05 were deemed to be factors truly affects the occurrence of OIs.
Results
Socio-demographic characteristics of the study participants
We analyzed data extracted from charts of 266 PLWH who were taking ART drugs from November 1, 2016, to November 1, 2017 in the Gedeo zone of Ethiopia. The mean age of the study participants was 37 with standard deviation 11.9 years. The majority of the study participants were male: 160(60.2%), found in age group 30–39: 104(39.1%), married: 184(69.2%), orthodox Christian religion followers: 132(49.6%), attended primary education: 100(37.6%), and urban residents: 167(62.8%). Further, the majority 73(27.4%) of the study participants were found merchants in their occupation (Table 1).
Clinical and functional characteristics of the study participants
The majority of PLWH participated in this study had CD4 count level < 200cells/mm3: 82 (30.8%), hemoglobin level at least 10gm/dl: 179(67.3%), and body weight: > 60 kg: 159(59.8%). Further, the majorities were from stage I/II of WHO clinical staging of HIV/AIDS: 148(55.7%), functional working status: 150(56.4%), and have good adherence level to ART drugs 169(63.5%). Likewise, the majority were receiving Isoniazid: 172(64.7%) and cotrimoxazole as prophylaxis: 114(42.9%) with aim to control OIs (Table 2).
Magnitude and type of opportunistic infections
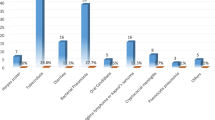
The study revealed, the overall prevalence of OIs found was 113(42.5%) with Oral candidiasis 28(24.8%) the predominant OIs followed by pulmonary tuberculosis 22(19.5%), herpes zoster 15(13.4%) and chronic diarrhea 12(10.6%). Furthermore, esophageal candidiasis nine(8.0%), Pneumocystic carnii Pneumonia: eight(7.1%), recurrent bacterial pneumonia: seven(6.2%), Kaposi’s sarcoma: four(3.5%), extra pulmonary tuberculosis: three(2.7%), Cryptococci meningitis: three(2.7%) and Toxoplasmosis: two(1.8%) were also retrieved from the records (Fig. 1).
Further, of the 113(42.5%) PLWH who developed OIs within the allotted one-year period, 71(44.3%) were men, 28(58.3%) were in the 40–49 age group, 104(69.3%) had a functional working status, 46(56.0%) had a CD4 count of fewer than 200 cells/mm3, 47(79.7%) had poor art drug adherence, 68(57.7%) were found to be in the advanced stage of the WHO clinical stage of HIV/AIDS, 48(55.1%) had low hemoglobin, and 41(49.9%) chews khat (Table 3).
Association of factors with the occurrence of opportunistic infections
We used binary logistic regression analysis to determine the association of selected variables with the occurrence level of OIs among PLWH participated in the current study. Variables statistically significant at P < 0.05 under bivariate logistic regression analysis were rechecked under multivariable logistic regression analysis. Accordingly, a number of variables like being male in gender [COR = 1.85(95% CI: 1.10, 3.10)], being found in older age group (≥ 50years) [COR = 2.71(95% CI: 1.16, 6.32)], being found in bedridden functional status [COR = 2.83(95% CI: 1.54, 5,18)], having low CD4 count level: < 200 cells/mm3 [COR = 15.08(95%CI: 5.48, 41.47)], 200–350 cells/mm3 [COR = 12.59(95%CI: 4,45, 35.61)], 351–500 cells/mm3 [COR = 6.21(2.15, 17.95)], having poor adherence level to ART drug [COR = 10.79(95% CI: 5.25, 22.17)], being in advance stage of WHO clinical stage of HIV/AIDS [COR = 4.39(95% CI: 2.59, 7.43)], having low level of hemoglobin [COR = 2.78(95% CI: 1.64, 4.71)], having behavioral characteristics of chewing khat [COR 5.01(95% CI: 2.70, 9.35)], and alcohol drinking [COR = 3.78(95% CI: 1.27, 11.21)] were found statistically significantly associated with the occurrence level of OIs under bivaraible logistic regression analysis at P < 0.05.
However, after controlling some confounders under multivariable logistic regression analysis, only being found in ambulatory working functional status [AOR = 2.40(95% CI: 1.14, 5.03)], and bedridden working functional status [AOR = 3.27(95% CI:1.64, 6.52)], having lower CD4 count level: less than 200cells/mm3 [AOR = 9.14(95% CI: 2.75, 30.39)], 200–350cells/mm3 [AOR = 9.45(95% CI: 2.70,33.06)], and 351-500cells/mm3 [AOR = 5.76(95% CI: 1.71, 19.39)]; being found in poor ART drug adherence level [AOR = 10.05(95% CI: 4.31,23.46)]; being found in advanced clinical stage of HIV/AIDS [AOR = 2.72(95% CI: 1.42, 5.20)]; and being chewing khat [AOR = 2.84(95% CI: 1.21, 6.65)] were found retained to positively predict the occurrence of OIs at P < 0.05 (Table 3).
Discussion
This study assessed prevalence of OIs and associated factors among adult PLWH taking ART drug in Gedeo Zone, Southern Ethiopia, and revealed 113(42.5%) prevalence of OIs during the one year determined follow-up period. This finding is higher than study findings from Vietnam (11.45%) [8], Uganda (15.3%) [9], Nigeria (22.4%) [10], and study findings from Ethiopia such as Mekelle (7.5%) [16], Sodo town (8.97%) [18], and Gondar (19.7%) [13]. The observed difference could be due to difference in sample size among the studies, and/or a longer follow-up period observed in some studies. For instance, a study from Mekelle is a cohort study, followed the cohorts for 36 months while a study from Sodo town, followed the cohorts for 10 years, which implies the risk of developing OIs is highest at its early stage [27] compared to studies conducted using non-cohort study design. This finding is comparable with study findings from Ethiopia: Addis Ababa (33.6%) [14], Debre Markos (42.9%) [17], and Wolaita (45.3%) [19]. However, lower than study findings from other parts of Ethiopia: Southern Tigray (55.3%) [15], Eastern Ethiopia (48%) [11], and Dawro (88.4%) [12]. This difference could be due to variation in host immunity, socio-economic, nutritional status, and/or differences in the duration of the study and sample size.
In this study, oral candidiasis was found the predominant OI followed by pulmonary tuberculosis and herpes zoster. However, in contrast to this study finding, pulmonary tuberculosis was found the most common OI revealed by numerous study findings from developing countries including Ethiopia [4, 8, 11,12,13,14, 16], Dawro [12], Eastern Ethiopia [11], Mekelle [16], and Uganda [4]. The possible reason for the lower prevalence of tuberculosis in the current study could be due to the provision of IPT, which was more than (64%), as the majority (57.1%) of PLWH who were not initiated on CPT exhibited OI, might have contributed to the higher proportion of oral candidiasis.
The most prevalent OIs revealed by the current study; pulmonary tuberculosis (19.5%) is higher than other study findings from Ethiopia: Gondar (9.72%) [13], Southern zone Tigray (9.5%) [15], Debremarkos (9.7%) [17], Arbaminch (7.2%) [20] and Debre Tabor (5%) [21]; oral candidiasis (24.8%) in line with study findings from Nigeria [10], Debre Markos [17], and Eastern Ethiopia [11] while herpes zoster (13.4%) is higher than study findings from India (4.2%) [28], Eastern Ethiopia (11.2%) [11], Southern Tigray (10.8%) [15], Wolaita (15.5%) [19], and Nigeria (0.6%) [10]. These capricious finding in the regions indicates, the need of further studies aimed to understand the reasons behind for these disparity.
This study revealed, being found in advanced stage of HIV/AIDS, having lower CD4 cell count level, being found in bedridden/ambulatory functional status, chewing khat and being poorly adhered to ART drug were found linked with the occurrence level of OIs.
The higher the odds linked to advanced stage of HIV/AIDS is in line with study findings from Ethiopia [11,12,13,14,15, 17], India, and Nigeria [10, 28]. The link of the factor with occurrence level of OIs could be due to the fact that the progression of the disease through elusive symptoms to advanced stage is correlated with lengthy immune suppression and make them susceptible multiple OIs [29].
The higher the odds linked to lower CD4 cell count level is in line with study findings from developing countries [11,12,13, 20]. The link of the factors with occurrence level of OIs could be due to the fact that the occurrence of OIs is linked with lower CD4 cell count level, which could be due to the fact that CD4 cells play a central role in the activation of both humoral and cellular immune response to fight against infection, which results in protective effect against OIs [29].
The higher the odds linked to poor adherence level of ART drug ten times higher than the odds of good ART drug adherence level could be due to the fact that, the poor the adherence level to ART drug reduces the effectiveness of the drugs, and accelerating viral replication and immune suppression which favors the development of OIs while good adherence for ART drug have the vice-versa effect [30]. This finding is in line with study findings from Ethiopia [12, 16, 17]. Mind the fact that, adequate suppression of HIV replication requires strict adherence to ART drug, that is why studies highlights poor adherence is frequently associated with clinical and immunological failure [30] and treatment failure [31, 32]. In support of other study findings [11, 16], the higher OIs revealed by this study, could be due to the lower CD4 count level of the study participants; which increases the risk of OIs [30].
The higher the odds of bed ridden patients could be due to their poor appetite and low nutritional absorption rate leading to malnutrition which results in immune impairment, and make them susceptible for OIs. Further, the higher odds linked to chewing khat is in line with study finding from Ethiopia [17]. This could be due to people who chew khat usually develops mental health impairment, imbalances the judgment level of brain, and even affects normal physiology of other systems, which indirectly impacts ART drug adherence level [17, 33].
This study provides important information regarding the acquisition of OIs with wise way of reviewing both electronic and paper based charts of the study participants. We also acknowledged that the current study has some limitations like used retrospective design which is prone to bias unless precaution is done, and the data included was a data of one year follow-up, inconclusive as large data.
Conclusion
Despite the fact that the country is implementing the high efficacy ART, this study revealed higher prevalence of OIs. Therefore, there should be an intervention tackles the higher prevalence of OIs revealed by the current study by considering predicting factors like advanced HIV/AIDS clinical stage, low CD4 cell count level, bedridden/ambulatory functional status, personal habits like Khat chewing and poor ART adherence level.
Data availability
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
References
WHO. The Global Health Observatory. 2022 [updated July 2022; cited 2022 December 19]. https://www.who.int/data/gho/data/themes/hiv-aids
Institute EPH. HIV related estimates and Projectionsin Ethiopia for the Year 2021–2022. Addis Ababa: Ethiopian Public Health Institute 2022 August 2022. Report No.
Masur H, Brooks JT, Benson CA, Holmes KK, Pau AK, Kaplan JE. Prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: updated guidelines from the Centers for Disease Control and Prevention, National Institutes of Health, and HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Diseases: Official Publication Infect Dis Soc Am. 2014;58(9):1308–11.
Rubaihayo J, Tumwesigye NM, Konde-Lule J, Wamani H, Nakku-Joloba E, Makumbi F. Frequency and distribution patterns of opportunistic infections associated with HIV/AIDS in Uganda. BMC Res Notes. 2016;9(1):501.
Benson CA, Brooks JT, Holmes KK, Kaplan JE, Masur H, Pau A. Guidelines for prevention and treatment opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC. the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America; 2009.
Krentz H, Dean S, Gill M, Longitudinal assessment. (1995–2003) of hospitalizations of HIV-infected patients within a geographical population in Canada. HIV Med. 2006;7(7):457–66.
Low A, Gavriilidis G, Larke N, B-Lajoie M-R, Drouin O, Stover J, et al. Incidence of opportunistic infections and the impact of antiretroviral therapy among HIV-infected adults in low-and middle-income countries: a systematic review and meta-analysis. Clin Infect Dis. 2016;62(12):1595–603.
Tanuma J, Lee KH, Haneuse S, Matsumoto S, Nguyen DT, Nguyen DTH, et al. Incidence of AIDS-Defining opportunistic infections and mortality during antiretroviral therapy in a cohort of adult HIV-Infected individuals in Hanoi, 2007–2014. PLoS ONE. 2016;11(3):e0150781.
Rubaihayo J, Tumwesigye NM, Konde-Lule J, Makumbi F. Forecast analysis of any opportunistic infection among HIV positive individuals on antiretroviral therapy in Uganda. BMC Public Health. 2016;16(1):766.
Iroezindu M, Ofondu E, Hausler H, Van Wyk B. Prevalence and risk factors for opportunistic infections in HIV patients receiving antiretroviral therapy in a resource-limited setting in Nigeria. J AIDS Clin Res. 2013;3:002.
Mitiku H, Weldegebreal F, Teklemariam Z. Magnitude of opportunistic infections and associated factors in HIV-infected adults on antiretroviral therapy in eastern Ethiopia. HIV/AIDS (Auckland NZ). 2015;7:137–44.
Solomon FB, Angore BN, Koyra HC, Tufa EG, Berheto TM, Admasu M. Spectrum of opportunistic infections and associated factors among people living with HIV/AIDS in the era of highly active anti-retroviral treatment in Dawro Zone hospital: a retrospective study. BMC Res Notes. 2018;11(1):604.
Damtie D, Yismaw G, Woldeyohannes D, Anagaw B. Common opportunistic infections and their CD4 cell correlates among HIV-infected patients attending at antiretroviral therapy clinic of Gondar University Hospital, Northwest Ethiopia. BMC Res Notes. 2013;6(1):534.
Dereje N, Moges K, Nigatu Y, Holland R. Prevalence And Predictors Of Opportunistic Infections Among HIV Positive Adults On Antiretroviral Therapy (On-ART) Versus Pre-ART In Addis Ababa, Ethiopia: A Comparative Cross-Sectional Study. HIV/AIDS (Auckland, NZ). 2019;11:229 – 37.
Weldearegawi TZ, Gerensea H, Berihu H, Gidey G, Welearegay MZ. The magnitude of opportunistic infections and associated factors in HIV-infected adults on antiretroviral therapy in southern zone Tigray, Ethiopia: a cross-sectional study. Pan Afr Med J. 2020;35:126.
Arefaine ZG, Abebe S, Bekele E, Adem A, Adama Y, Brockmeyer H. Incidence and predictors of HIV related opportunistic infections after initiation of highly active antiretroviral therapy at Ayder Referral Hospital, Mekelle, Ethiopia: a retrospective single centered cohort study. PLoS ONE. 2020;15(4):e0229757.
Moges N, Kassa G. Prevalence of opportunistic infections and associated factors among HIV positive patients taking anti-retroviral therapy in DebreMarkos Referral Hospital, Northwest Ethiopia. J AIDs Clin Res. 2014;5(5):1–300.
Woldegeorgis BZ, Diro CW, Yohannes B, Kerbo AA, Asgedom YS. Incidence and predictors of opportunistic infections in adolescents and adults after the initiation of antiretroviral therapy: a 10-year retrospective cohort study in Ethiopia. Front Public Health. 2022;10.
Mihiretu A, Yilma Y, Worku A, Bereket A. Opportunistic infections among HIV/AIDS patients taking anti-retroviral therapy at tertiary care hospital in Wolaita Zone, Southern Ethiopia. J AIDS Clin Res. 2017;8(2).
Mama M, Manilal A, Tesfa H, Mohammed H, Erbo E. Prevalence of Pulmonary Tuberculosis and Associated factors among HIV positive patients attending antiretroviral therapy clinic at Arba Minch General Hospital, Southern Ethiopia. open Microbiol J. 2018;12:163–71.
Kiros T, Dejen E, Tiruneh M, Tiruneh T, Eyayu T, Damtie S et al. Magnitude and Associated factors of Pulmonary Tuberculosis among HIV/AIDS patients attending antiretroviral therapy clinic at Debre Tabor Specialized Hospital, Northwest Ethiopia, 2019. HIV/AIDS (Auckland, NZ). 2020;12:849–58.
Wold Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. World Health Organization; 2016.
World Health Organization. Rapid advice: antiretroviral therapy for HIV infection in adults and adolescents-November 2009. 2009.
Barnabas G, Sibhatu MK, Berhane Y. Antiretroviral therapy program in Ethiopia benefits from virology treatment monitoring. Ethiop J Health Sci. 2017;27(1):1–2.
Deyessa N. Study of prevalence of opportunistic infections among HIV/AIDS patients in Addis Ababa public hospitals. Addis Ababa University; 2011.
World Health Organization. Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy. July 2017. 2017.
Mitiku H, Weldegebreal F, Teklemariam Z. Magnitude of opportunistic infections and associated factors in HIV-infected adults on antiretroviral therapy in eastern Ethiopia. HIV/AIDS (Auckland, NZ). 2015;7:137.
Dabla V, Gupta AK, Singh I. Spectrum of opportunistic infections among HIV seropositive patients in Delhi region-a study by Delhi State AIDS control society. J Med Disorders. 2015;3(1):1.
Rubaihayo J, Tumwesigye NM, Konde-Lule J, Wamani H, Nakku-Joloba E, Makumbi F. Prevalence and Factors Associated with opportunistic infections in HIV positive patients on antiretroviral therapy in Uganda. 2015.
Lenjiso GA, Endale BS, Bacha YD. Clinical and immunological failure among HIV-positive adults taking first-line antiretroviral therapy in dire Dawa, eastern Ethiopia. BMC Public Health. 2019;19(1):771.
Feleke R, Geda B, Teji Roba K, Weldegebreal F. Magnitude of antiretroviral treatment failure and associated factors among adult HIV-positive patients in Harar public hospitals, Eastern Ethiopia. SAGE Open Med. 2020;8:2050312120906076.
Demsie DG, Bantie AT, Allene MD, Alema NM, Gebrie D. Antiretroviral treatment failure among HIV-positive adults taking first-line therapy and associated risk factors at Adigrat General hospital, Adigart, Ethiopia 2019: a cross sectional study. Int J Surg Open. 2020;26:16–21.
Soboka M, Tesfaye M, Feyissa GT, Hanlon C. Khat use in people living with HIV: a facility-based cross-sectional survey from South West Ethiopia. BMC Psychiatry. 2015;15:69. https://doi.org/10.1186/s12888-015-0446-5. PMID: 25879767; PMCID: PMC4394566.
Acknowledgements
We would like to acknowledge Addis Ababa University for supported this study.
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
G.G., N.T., and D.M. initiated the study. G.G. developed the study concept. NT coordinated the team discussions, and drafted the manuscript including the tables. K.B., D.M., and N.T. edited and reviewed the manuscript very critically. All authors contributed to the conceptualization, developing the data collection tools, writing, and reviewing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out after getting ethical clearance letter with protocol number: aau/chs/ahnsg04/2018 from Institutional Review Board of Addis Ababa University, College of Health Sciences. Following the approval of the ethical clearance, official letter of cooperation was written to Gedeo Zone Health Bureau and Dilla University Referral Hospital from the Department of Nursing and Midwifery of AAU. After obtained permission form the zone health bureau, the purpose of the study was explained to each ART clinic’s heads and all research ethical issues were kept under the legal framework of the institutional board. All the necessary precautions were taken to keep all documents in a safe and secure.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declared; don’t have any conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gebremichael, G., Tadele, N., Gebremedhin, K.B. et al. Opportunistic infections among people living with HIV/AIDS attending antiretroviral therapy clinics in Gedeo Zone, Southern Ethiopia. BMC Res Notes 17, 225 (2024). https://doi.org/10.1186/s13104-024-06888-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-024-06888-4