Abstract
Background
The recruitment-to-inflation ratio (R/I) has been recently proposed to bedside assess response to PEEP. The impact of PEEP on ventilator-induced lung injury depends on the extent of dynamic strain reduction. We hypothesized that R/I may reflect the potential for lung recruitment (i.e. recruitability) and, consequently, estimate the impact of PEEP on dynamic lung strain, both assessed through computed tomography scan.
Methods
Fourteen lung-damaged pigs (lipopolysaccharide infusion) underwent ventilation at low (5 cmH2O) and high PEEP (i.e., PEEP generating a plateau pressure of 28–30 cmH2O). R/I was measured through a one-breath derecruitment maneuver from high to low PEEP. PEEP-induced changes in dynamic lung strain, difference in nonaerated lung tissue weight (tissue recruitment) and amount of gas entering previously nonaerated lung units (gas recruitment) were assessed through computed tomography scan. Tissue and gas recruitment were normalized to the weight and gas volume of previously ventilated lung areas at low PEEP (normalized-tissue recruitment and normalized-gas recruitment, respectively).
Results
Between high (median [interquartile range] 20 cmH2O [18–21]) and low PEEP, median R/I was 1.08 [0.88–1.82], indicating high lung recruitability. Compared to low PEEP, tissue and gas recruitment at high PEEP were 246 g [182–288] and 385 ml [318–668], respectively. R/I was linearly related to normalized-gas recruitment (r = 0.90; [95% CI 0.71 to 0.97) and normalized-tissue recruitment (r = 0.69; [95% CI 0.25 to 0.89]). Dynamic lung strain was 0.37 [0.29–0.44] at high PEEP and 0.59 [0.46–0.80] at low PEEP (p < 0.001). R/I was significantly related to PEEP-induced reduction in dynamic (r = − 0.93; [95% CI − 0.78 to − 0.98]) and global lung strain (r = − 0.57; [95% CI − 0.05 to − 0.84]). No correlation was found between R/I and and PEEP-induced changes in static lung strain (r = 0.34; [95% CI − 0.23 to 0.74]).
Conclusions
In a highly recruitable ARDS model, R/I reflects the potential for lung recruitment and well estimates the extent of PEEP-induced reduction in dynamic lung strain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In acute respiratory distress syndrome (ARDS), mechanical ventilation should sustain gas exchange while minimizing ventilator-induced lung injury (VILI) [1]. Dynamic lung strain, defined as the ratio of tidal volume (VT) to functional residual capacity (FRC), is one of the VILI determinants. In healthy pigs submitted to mechanical ventilation, dynamic lung strains higher than 1.5 has been shown to be “lethal” [2]. Less is known about the “critical” threshold in damaged, inhomogeneous lungs as during ARDS [3]. However, studies on patients showed that a dynamic strain of 0.27 may be deemed “high,” as it is associated with a proinflammatory lung response in patients with acute lung injury [4].
Well-established practices strongly emphasize the use of low VT and prone position to homogenize lung aeration [5, 6], while the role of positive end-expiratory pressure (PEEP) is still debated [7, 8]. In highly recruitable patients, PEEP recruits collapsed lung tissue, increasing FRC and decreasing dynamic lung strain [9, 10]. However, in every case, PEEP invariably inflates already aerated lung regions [10,11,12], increasing static lung strain [13] even in good recruiters. Nevertheless, evidence suggests that dynamic lung strain is more implicated in VILI generation than static lung strain [13,14,15] and, accordingly, tailoring PEEP to minimize dynamic lung strain is a physiologically straightforward target. In this context, a tool to define the impact of PEEP on dynamic lung strain would be welcome [16]. Computed tomography (CT) is the gold standard to assess lung strain and the impact of PEEP on alveolar recruitment [9, 17] but remains impractical for routine clinical use [18]. This moved clinical research toward the development of bedside strategies to best phenotype patient responses to PEEP in clinical practice.
The recruitment to inflation ratio (R/I) has been recently proposed to assess lung recruitability at the bedside [19]. Through a simplified derecruitment maneuver [20], this new index quantifies lung recruitability by scaling the compliance of recruited tissue (CREC) to that of the previously aerated lung at low PEEP [19]. Briefly, by simplifying the original multiple pressure/volume curve technique [21], the R/I discriminates recruiters from non-recruiters by assuming that if CREC at higher PEEP is at least 50% of the respiratory system compliance at lower PEEP (i.e., R/I > 0.5), the balance between PEEP-induced alveolar recruitment and inflation is in favor of recruitment [19].
By predicting and quantifying lung recruitability, the R/I should reflect the impact of PEEP on dynamic lung strain [22]. However, to our knowledge, no study has assessed whether R/I accurately reflects dynamic lung strain lung and recruitability compared with the “gold standard” CT scan method. Therefore, we conducted an experimental study on a high recruitable ARDS model ventilated with two PEEP levels (low and high) in the context of a low-tidal volume lung-protective strategy to investigate whether R/I reflects the impact of PEEP on dynamic lung strain and lung recruitability assessed through the CT scan method.
Methods
This study was conducted in the veterinary clinic of the University of Bari between June 2020 and September 2022, following approval of the Italian Ministry of Education, University and Research Committee (Prot. n.1234/2020-PR) on fourteen certified healthy mixed breeds of domestic pigs. All pigs were female and 6 months old and had a homogeneous weight of 47 [IQR 45–48] kg.
Experimental protocol
At the beginning of the study, the animals were anesthetized, paralyzed, intubated, and mechanically ventilated (Servo-I, Getinge, Sweden). Anesthesia and muscle paralysis were obtained by continuous infusion of propofol (6 mg/kg/h) and cisatracurium (5 mcg/kg/min); analgesia was obtained by a single shot of buprenorphine (300 mcg). ARDS-like lung injury was produced by a 1-h intravenous infusion of a lipopolysaccharide membrane of Escherichia coli (LPS) (300 μg/kg) diluted in 20 ml of NaCl solution [23, 24]. Central venous and arterial lines were inserted through ultrasound guide. Continuous monitoring, including electrocardiography, heart rate, SpO2, end-tidal carbon dioxide and invasive arterial pressure, was kept for the whole study. Cardiac output (CO) was continuously monitored through the PRAM system (Vytech, USA).
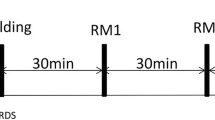
Static lung CT scans were acquired during prolonged end-expiratory and end-inspiratory breath-holds (approximately 40 s) in the helical mode, thickness 5 mm, pitch = 1, rotation time 1.0 s, 120 KVP, 180 mAs, FOV 50 cm, and standard and chest convolution kernel (GE HiSPEED CT/e Dual, General Electric, New York, NY). The experimental protocol is summarized in the supplementary Fig. 1. Lung CT, respiratory mechanics, hemodynamics, and blood gas analysis results were obtained at the end of each experimental ventilation phases.
Ventilation protocol and data acquisition
Constant flow volume-control ventilation was used for the whole study procedure. Respiratory rate (RR) was titrated to maintain pH within 7.35 and 7.45 and FiO2 was set to 1 for the whole study period. Three hours after beginning the LPS infusion, PEEP was set at 5 cmH2O (PEEPLOW phase) for 1 h. Afterward, the PEEP was increased to reach a plateau end-inspiratory airway pressure (PPLAT) of 28–30 cmH2O according to the ExPress protocol [25] (PEEPHIGH phase) while keeping VT constant, for 1 h.
A Fleisch-type pneumotacograph (n.2, Metabo, Lausanne, Switzerland) and a pressure transducer (sample rate = 200 Hz) measured flow and airway pressure, respectively. VT was calculated as the digital integration of the flow signal. The following parameters were recorded at the end of each PEEP step: VT, set PEEP, intrinsic PEEP (PEEPi;st) and PPLAT, the latter obtained through two second end-expiratory and end-inspiratory occlusions, respectively. Total PEEP (PEEPTOT) was computed as the sum of PEEP set and PEEPi;st. Driving pressure (ΔP) was calculated as (PPLAT − PEEPTOT). Respiratory system compliance (CRS) was computed as the ratio between VT and ΔP. The ventilatory ratio (Vr) was computed according to a standard formula described elsewhere [26]. Stress index (SI) was automatically calculated through the dedicated monitoring tool of the Servo-I Ventilator (Getinge, Sweden) [27]. All the signals were recorded and reviewed offline through dedicated software (ICU Lab, Kleistek, Bari, Italy).
Recruitment-to-inflation ratio assessment
At the end of PEEPHIGH phase, we performed a simplified, one-breath de-recruitment maneuver to estimate the difference in end-expiratory lung volume (EELV) between PEEPHIGH and PEEPLOW (\(\Delta\) EELV) [20]. To do this, RR was set at 6 breaths/min while maintaining the inspiratory to expiratory time ratio unchanged (i:e = 1:2), thus obtaining an expiratory time of 6.6 s. Immediately after, PEEPHIGH was abruptly decreased to PEEPLOW and the exhaled volume during the prolonged expiration was recorded [20]. \(\Delta\) EELV was calculated as the difference between the exhaled volume recorded during the one-breath de-recruitment maneuver and inspired tidal volume:
Considering that \(\Delta \text{EELV}\) includes two components: PEEPHIGH-induced recruited volume (VREC) and PEEPHIGH-induced inflation volume (i.e., the minimal predicted increase in lung volume due to PEEPHIGH) [21], the latter was calculated as the product of compliance at lower PEEP and the PEEP difference between the two steps:
Consequently, VREC was computed as [19]:
Finally, the compliance of recruited tissue (CREC) was obtained by:
and the recruitment-to-inflation ratio as the ratio between CREC and CRS at PEEPLOW [19]:
Of note, the R/I method mandates the assessment of any end-expiratory airway closure and of the corresponding airway opening pressure (AOP) [19]. To assess AOP, during ventilation at PEEPLOW (5 cmH2O), RR was set at 5 breaths/min and the inspiratory time was adjusted to achieve flow rate of 5 L/minute while VT was kept constant. During the procedure, that lasted a single breath, the time-airway opening pressure waveform was collected and analyzed on the ventilator screen. If present, AOP was identified as the inflection point on the pressure waveform above PEEPLOW and used instead of PEEPLOW for R/I calculation [19]. All the procedures for measuring R/I were verified trough a dedicated online tool (https://crec.coemv.ca).
Computed tomography analysis
Quantitative CT scan analysis of all cranio-caudal CT scan slices above the diaphragm was performed using the Maluna software (Maluna version 2020, Goettingen, Germany) [17, 28]. For each slice, the entire left and right lungs were chosen as regions of interest by manually drawing their outer boundaries along the inside of the ribs and the inner boundaries along the mediastinal organs [17, 28]. The volume of each single voxel was computed as pixel area (0.35 mm2) times slice thickness (5 mm). The CT-Hounsfield unit (HU) number was used to define the density of each voxel [29, 30]. Given the voxel’s density and its relative volume, the voxel composition in gas and tissue (edema, interstitial water, blood, and lung structure) [29, 30] and the corresponding gas/tissue ratio (g/t) was automatically computed by the software [17, 28]. Thereby, the following Hounsfield unit (HU) ranges were used to define the different lung compartments: nonaerated, − 100 to + 100 HU; poorly aerated, − 101 to − 500 HU; normally aerated, − 501 to − 900 HU and hyperinflated, − 901 to − 1000 HU, while the volume of each compartment was obtained by multiplying the number of pixel found in each compartment to the voxel volume [17, 28, 29]. The total volume, tissue weight and gas volume of the entire lung are obtained by the Maluna software according to established methods [17, 28,29,30].
Alveolar recruitment assessed through CT scan analysis
PEEP-induced tissue recruitment (TREC, grams) was measured as the difference in weight between PEEPLOW and PEEPHIGH of nonaerated lung tissue [29, 30] (online supplement; supplementary Fig. 2). To estimate the amount of recruited gas volume (GASREC, milliliters), we replicated the method proposed by Chiumello et al. [31]. Briefly, the method assumes that the gas-to-tissue ratio (g/t) of the recruited tissue corresponds to the median g/t at PEEPHIGH [31]. Accordingly, GASREC was computed as:
Considering that: (1) the R/I normalizes CREC to CRS at PEEPLOW[19], and (2) compliance is an estimate of aerated lung size [32], we normalized TREC and GASREC to total end-expiratory lung weight and end-expiratory total gas volume at PEEPLOW, respectively, as follow:
Dynamic lung strain assessed through CT scan
In this study we considered PEEPLOW (5 cmH2O) as the baseline condition, and therefore, the EELV at PEEPLOW (EELVLOW) as FRC [15]. Based on this assumption, dynamic lung strain at PEEPLOW was computed as the ratio between VT and EELVLOW [13, 15], while dynamic lung strain at PEEPHIGH was computed as the ratio between VT and EELVLOW + GASREC [13, 15]:
Static lung strain was computed in agreement with standard formula [13, 15]:
where PEEPVOLUME expresses the PEEPHIGH-induced inflation of already aerated lung regions at PEEPLOW.
Having considered PEEPLOW as baseline condition, we assumed that the static lung strain at PEEPLOW was 0 [13, 15]. Then, we calculated PEEPVOLUME at PEEPHIGH as (DEELV − GASREC) and the static lung strain as follows [13, 15]:
Finally, global lung strain was calculated as the sum of static lung strain and dynamic lung strain [13, 15].
Endpoints
Primary endpoint: To determine whether the recruitment-to-inflation ratio reflects CT-scan measured PEEP-induced changes in dynamic strain.
Secondary endpoint: To determine whether R/I reflects CT-measured lung recruitability.
Statistical analysis
For this experimental observational study, without performing a formal sample size calculation, we planned to enroll 14 animals as a convenient sample size, consistently with other studies on similar topics [27, 33, 34]. All numerical variables are expressed as medians and interquartile ranges [IQRs]. Shapiro–Wilk’s test was used to test normality and, based on its results, paired Student’s t-test or nonparametric paired Wilcoxon test were used to compare the two experimental conditions. The Mardia test was used to verify multivariate normality assumption, then correlations between continuous parameters were assessed with r-Pearson’s correlation coefficient (95% CI). For significant results, linear regression model was performed, and linearity of the relationship was verified by checking the normality of the residuals. Analysis of the potential outliers and potential highest influential points was checked by Cook's distance, Leverage-Residual plot and sensitivity analysis. A p value < 0.05 was considered to indicate statistical significance. Statistical analyses were performed using SAS/STAT® Statistics version 9.4 (SAS Institute, Cary, NC, USA).
Results
Respiratory mechanics, gas exchange and hemodynamics parameters
Table 1 reports respiratory mechanics, gas exchange and hemodynamic parameters in the two experimental conditions. PEEPLOW was by protocol 5 cmH2O while median PEEPHIGH resulting from the ExPress strategy was 20 cmH2O [18–21]. The median VREC was 540 ml [368–762]. The median R/I was 1.08 [0.88–1.82]. At PEEPHIGH, compared to PEEPLOW, CRS was 41 ml/cmH2O [32–50] versus 33 ml/cmH2O [23–42] (p = 0.037), stress index was 1.02 [1–1.03] versus 0.93 [0.82–0.97] (p = 0.001), PaO2/FiO2 was 167 mmHg [150–203] versus 108 mmHg [99–122] (p < 0.001), while PaCO2 and the ventilatory ratio remained unchanged. CO was 3.0 L/min [2.8–3.4] at PEEPHIGH versus 3.9 L/min [3.5–4.2] at PEEPLOW (p < 0.001).
R/I and lung strain
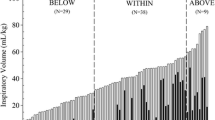
Figure 1 shows that going from PEEPLOW to PEEPHIGH, dynamic lung strain decreased from 0.59 [0.56–0.80] to 0.37 [0.29–0.44] (p < 0.001), static lung strain increased from zero to 0.53 [0.44–0.75] (p < 0.001) and global lung strain increased from 0.59 [0.56–0.80] to 0.93 [0.76–1.42] (p < 0.001). The inter-individual coefficient of variation of dynamic lung strain reduction was 69%. R/I was strongly correlated with D dynamic lung strain (r = − 0.93; [95% CI − 0.78 to − 0.98] p < 0.001) and, less strongly, with D global lung strain (r = − 0.56; [95% CI − 0.05 to − 0.84], p = 0.03). No correlation was found between R/I and D static lung strain (r = 0.32; [95% CI − 0.23 to 0.74], p = 0.23). The regression model between R/I and D dynamic lung strain showed intercept and slope of respectively, + 0.52 (95% CI 0.29 to 0.77) and − 2.55 (95% CI − 3.19 to − 1.91).
In the upper panel, box-violin graphs represent variation in global, dynamic and static lung strain going from PEEPLOW (light gray) to PEEPHIGH (dark gray). The lower panel depicts the correlations between recruitment-to-inflation (R/I) ratio and the changes in in global, dynamic and static lung strain going from PEEPLOW to PEEPHIGH. The dotted line represents linear regressions, and each dot represents one pig
Lung recruitability assessed through the CT-scan method
The absolute TREC and GASREC were 246 g [182–288] and 385 ml [318–668], respectively, whereas the normalized TREC and GASREC were 0.39 [0.25–0.55] and 0.85 [0.43–1.18], respectively. Table 2 and Fig. 2 report tissue weights and gas volumes of the different lung compartments (non-aerated, poorly aerated, normally aerated, hyperinflated) at end-expiration and end-inspiration, in the two experimental conditions. Figure 3 displays an experimental record of a representative animal, showing two lung CT slices acquired at end-expiration and the corresponding density histograms, in the two experimental conditions.
Left and middle panels: Representative computed tomography (CT) images and corresponding voxel density histograms of a large transverse lung section acquired under two different experimental ventilation conditions at end-expiration. Each image was interpreted using the UCLA color coding table (OsiriX image processing software, http://www.osirixfoundation.com, Geneva, Switzerland). Non-aerated lung tissue, ranging from − 100 to + 100 Hounsfield Units (HU), was depicted in shades of red (from dark red to orange), poorly aerated lung tissue (between − 500 to − 100 HU) was represented in shades of green, and normally aerated lung tissue (between − 900 to − 500 HU) was coded in dark and light blue. However, hyperinflated lung tissue (ranging from − 1000 to − 900 HU), which would have been represented in purple, was not observed upon raising PEEP from PEEPLOW to PEEPHIGH. Right panel: experimental records in a representative animal showing the air flow and the opening airway pressure (Pao) traces during both experimental ventilation conditions. Dashed lines indicate the constant flow period
R/I and lung recruitability
Figure 4 depicts the significant correlations between VREC (measured with the R/I method) and GASREC and TREC (measured with the CT scan method). Additionally, it shows that R/I was not correlated with absolute GASREC while was correlated with normalized GASREC (r = 0.89; [95% CI 0.71 to 0.97], p < 0.001), absolute TREC (r = 0.63; [95% CI 0.14 to 0.87], p < 0.01) and normalized TREC (r = 0.69; [95% CI 0.25 to 0.89], p < 0.01).
Left panels: Correlations between the absolute extent of PEEP-induced recruited volume (VREC) and tissue recruitment (TREC, upper panel) and gas recruitment (GASREC, lower panel). Middle and right panels: Correlations between the recruitment-to-inflation ratio (R/I) and absolute and normalized values of TREC (upper panel) and GASREC (lower panel). The dotted line represents linear regression, and each dot represents one pig
Discussion
In this experimental study we found that R/I accurately reflects the impact of PEEP on dynamic lung strain and is closely correlated with normalized gas recruitment, as assessed through the “gold standard” CT scan method.
In patients with ARDS there is a consensus that higher PEEP levels should be applied only to “recruiters” [6] and accordingly, phenotyping patients according to the potential for lung recruitment would be advisable [35]. However, consensus on the clinical prediction of lung recruitability remains elusive. Various methods based on respiratory system compliance [36], oxygenation, shunts [37, 38] and pressure‒volume curves [21] have been proposed to determine the “best” PEEP. Large randomized control trials compared higher and lower PEEP settings setting PEEP according to physiological variables (oxygenation [37, 38], respiratory system compliance[25, 39], transpulmonary pressure [40]) but yielded disappointing results, showing no significant difference in terms of clinical benefit.
Recently, the R/I method has been introduced in clinical practice to predict lung recruitability through an easy-to-perform derecruitment maneuver, where the patient transitions from a higher to a lower PEEP level within a single breath, without being disconnected from the ventilator [20]. Unlike other respiratory mechanics-based methods, the R/I offers an estimate of recruited volume compared to the inflated volume. Based on the median R/I value in their original study patients cohort, Chen et al. identified R/I > 0.5 as a hallmark of “poor recruitment” and vice versa [19]. This suggests that when R/I is higher than 0.5, PEEP-induced inflation (increase in static strain) has a less injurious effect compared to the benefit of alveolar recruitment (decrease in dynamic lung strain), but further studies are needed to prove this assumption. However, it is important to consider that increasing PEEP, in addition to inducing a variable degree of alveolar recruitment, invariably generates static lung strain by distending previously aerated lung parenchyma (PEEPVOLUME). Another issue regards the wide PEEP transition to calculate R/I as originally proposed by Chen et al.; recently a more “granular” R/I measurement (i.e., calculating the R/I within narrower PEEP transitions) to identify the “best” compromise between recruitment and inflation [22].
From a physiological point of view, the impact of PEEP on dynamic lung strain depends on the ratio between the FRC at lower PEEP and PEEP-induced increase in FRC [13, 14]. We hypothesized that R/I may reflect the impact of PEEP on dynamic lung strain and documented a linear relationship between R/I and changes in dynamic lung strain (Fig. 1). However, hyperinflation may occur regardless recruitment. In this context, it is important to note that from a theorical viewpoint R/I cannot assess hyperinflation as it solely accounts for the ratio between the compliance of the recruited lung tissue (CREC) and total compliance at PEEPLOW (CRS) [19]. To substantiate this concept, we have performed a supplementary analysis showing that individual R/I and PEEP-induced hyperinflation are not correlated (r = 0.04; p = 0.89) (online supplement; Supplementary Fig. 3). Furthermore, the R/I is unsuitable to assess regional tidal hyperinflation. Accordingly, when setting high PEEP, hyperinflation (both global and regional) should be assessed regardless of the R/I value to achieve a fully protective ventilatory strategy.
The ability of R/I to predict PEEP-induced alveolar recruitment has been validated since now with respiratory mechanics [19]. However, CT-scan remains the gold standard for measuring PEEP-induced alveolar recruitment by quantifying TREC [12] and GASREC [31]. In our study, we observed poor correlations between R/I and absolute TREC and no correlation between R/I and GASREC (Fig. 4). Nevertheless, upon reflection, we reasoned that (a) R/I normalizes the compliance of PEEP-recruited lung tissue (CREC) to the total compliance at PEEPLOW (CRS); (b) compliance is an estimation of aerated lung size [32] and, finally, (c) recent studies have found that at low PEEP/ZEEP CRS is an estimate of FRC [41] and indeed we found a good correlation between CRS and total end-expiratory gas volume at PEEPLOW (r = 0.75; p < 0.01) (supplementary Fig. 7). Thus, we hypothesized that the correct correlation should have been between R/I and GASREC normalized to total lung capacity at PEEPLOW. When we conducted this correlation, we found a significant and strong relationship (r = 0.89, p < 0.001), as depicted in Fig. 4. We extended this reasoning to TREC normalized to total lung weight at PEEPLOW (r = 0.69, p < 0.01, Fig. 4). Additionally, we explored the relationship between VREC and TREC and GASREC measured with CT scan and, again, found significant correlations (r = 0.69 and r = 0.86 respectively, both p < 0.01, see Fig. 4). Overall, these findings seem the first to validate the performance of R/I against the gold standard CT-scan technique.
From a methodological point of view, it is important to discuss that the method to quantify PEEP-induced alveolar recruitment through CT scan is not uniformly agreed upon [42]. In our study, we quantified recruitment according to Gattinoni et al. [12] as PEEP-induced re-aeration of non-aerated lung tissue (weight of recruited tissue = weight of non-aerated tissue at PEEPLOW – weight of non-aerated tissue at PEEPHIGH). However, another approach considers PEEP-induced differences in non-aerated plus poorly aerated lung tissues [49]. Nevertheless, when we applied both these approaches to quantify TREC, we found no significant difference and a good correlation between the two methods (r = 0.82; p < 0.01). Also, the quantification of GASREC, lung strain, and the correlations between the R/I and these variables were not affected by the method to calculate TREC. We present these results in the online supplement (see online supplement Figs. 4, 5 and 6).
In our study, we used the approach employed in the ExPress trial to set PEEPHIGH (increasing PEEP up to a plateau pressure of 30 cmH2O) [25]. However, Chiumello and colleagues demonstrated that the ExPress PEEP-setting strategy does not consistently correlate with lung recruitability and is associated with higher risks of hyperinflation in patients with the higher quartile of hyperinflated tissue on CT scans [43]. Nevertheless, we point out that increasing PEEP to enhance lung recruitability is a well-established practice in the management of moderate-to-severe acute respiratory distress syndrome [6] and, furthermore, recently Protti et al. showed in COVID-related ARDS (CARDS) that when higher PEEP levels are applied to patients with high recruitability (similar to our experimental model), the balance between recruitment and hyperinflation is towards recruitment [44]. Finally, an ongoing multicenter trial designed to individualize PEEP based on the R/I approach adopts a PEEP-setting strategy similar to that of the ExPress trial [45].
Our study has limitations. First, it was conducted in a highly recruitable model of ARDS, which limits the generalizability of our findings. However, if confirmed by clinical studies, our experimental data may prove useful in supporting PEEP settings in the significant subset of highly recruitable patients. Second, we did not conduct an a priori sample size calculation for this study. However, from a post hoc power analysis resulted that for a Type III F test of one predictor in a regression model with a significance level of 0.05, a sample size of 14 has a power > 0.99 to detect a R-square of 0.87 between the tested predictor (Delta Dynamic Lung Strain) and response (R/I). Third, our results were obtained in the supine position, which does not necessarily imply their reproducibility in the prone position [46]. Fourth: Our results may have been influenced by the different approaches between CT scan and R/I assessments. Indeed (see Methods and Supplemental Fig. 1), by experimental design, we performed a CT scan at low PEEP followed by a CT scan at high PEEP, whereas the R/I was obtained by suddenly decreasing PEEP from a high to a low level, as per the R/I protocol. These different approaches could have influenced the "volume history" of our model and certainly may represent a study bias, even though the CT scans were taken after 1 h of application of each PEEP level, suggesting a stable condition. Probably, a brief recruiting maneuver applied when moving from the lower to the higher PEEP level could have helped to resolve this point. Fifth: manually delineating CT regions of interest may have introduced a potential bias in the CT-scan analysis. However, this approach aligns with similar investigations in animal models [17]. Finally, we do not provide data about blood or lung samples assessing inflammation and VILI in the two experimental conditions, so we can only speculate on the eventual impact of higher PEEP on VILI.
Conclusions
In a highly recruitable model of ARDS, we found that the R/I reflects the impact of PEEP on dynamic lung strain and normalized gas recruitment, as assessed through the CT-scan method.
Availability of supporting data
The study dataset used is available upon a justified request.
Abbreviations
- PEEP:
-
Positive end-expiratory pressure
- ARDS:
-
Acute respiratory distress syndrome
- VILI:
-
Ventilator-induced lung injury
- CT:
-
Computed tomography
- R/I:
-
Recruitment to-inflation ratio
- PLR:
-
Potential for lung tissue recruitment
- FRC:
-
Functional residual capacity
- VT :
-
Tidal volume
- PPLAT :
-
Plateau end-inspiratory airway pressure
- ΔP:
-
Driving pressure
- CRS :
-
Compliance of respiratory system
- SI:
-
Stress index
- CO:
-
Cardiac output
- LPS:
-
Lipopolysaccharide
- RR:
-
Respiratory rate
- CREC :
-
Compliance of tissue recruited
- VREC :
-
Recruited volume
- EELV:
-
End-expiratory lung volume
- AOP:
-
Airway opening pressure
References
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369:2126–36.
Protti A, Cressoni M, Santini A, Langer T, Mietto C, Febres D, et al. Lung stress and strain during mechanical ventilation: any safe threshold? Am J Respir Crit Care Med. 2011;183:1354–62.
Nieman GF, Satalin J, Andrews P, Aiash H, Habashi NM, Gatto LA. Personalizing mechanical ventilation according to physiologic parameters to stabilize alveoli and minimize ventilator induced lung injury (VILI). Intensive Care Med Exp. 2017. https://doi.org/10.1186/s40635-017-0121-x.
González-López A, García-Prieto E, Batalla-Solís E, Amado-Rodríguez L, Avello N, Blanch L, et al. Lung strain and biological response in mechanically ventilated patients. Intensive Care Med. 2012;38:240–7.
Pellegrini M, Del Sorbo L, Ranieri VM. Finding the optimal tidal volume in acute respiratory distress syndrome. Intensive Care Med. 2024. https://doi.org/10.1007/s00134-024-07440-5.
Grasselli G, Calfee CS, Camporota L, Poole D, Amato MBP, Antonelli M, et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 2023;49:727–59.
Cressoni M, Cadringher P, Chiurazzi C, Amini M, Gallazzi E, Marino A, et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189:149–58.
Grieco DL, Bongiovanni F, Chen L, Menga LS, Cutuli SL, Pintaudi G, et al. Respiratory physiology of COVID-19-induced respiratory failure compared to ARDS of other etiologies. Crit Care. 2020;24:529.
Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178:346–55.
Caironi P, Cressoni M, Chiumello D, Ranieri M, Quintel M, Russo SG, et al. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181:578–86.
Grasso S, Fanelli V, Cafarelli A, Anaclerio R, Amabile M, Ancona G, et al. Effects of high versus low positive end-expiratory pressures in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171:1002–8.
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–86.
Protti A, Andreis DT, Monti M, Santini A, Sparacino CC, Langer T, et al. Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med. 2013;41:1046–55.
Protti A, Votta E, Gattinoni L. Which is the most important strain in the pathogenesis of ventilator-induced lung injury: dynamic or static? Curr Opin Crit Care. 2014;20:33–8.
Garciá-Prieto E, López-Aguilar J, Parra-Ruiz D, Amado-Rodríguez L, López-Alonso I, Blázquez-Prieto J, et al. Impact of recruitment on static and dynamic lung strain in acute respiratory distress syndrome. Anesthesiology. 2016;124:443–52.
Spinelli E, Grieco DL, Mauri T. A personalized approach to the acute respiratory distress syndrome: recent advances and future challenges. J Thorac Dis. 2019;11:5619–25.
Grasso S, Stripoli T, Sacchi M, Trerotoli P, Staffieri F, Franchini D, et al. Inhomogeneity of lung parenchyma during the open lung strategy: a computed tomography scan study. Am J Respir Crit Care Med. 2009;180:415–23.
Dianti J, Morris IS, Urner M, Schmidt M, Tomlinson G, Amato MBP, et al. Linking acute physiology to outcomes in the ICU: challenges and solutions for research. Am J Respir Crit Care Med. 2023;207:1441–50.
Chen L, Del Sorbo L, Grieco DL, Junhasavasdikul D, Rittayamai N, Soliman I, et al. Potential for lung recruitment estimated by the recruitment-to-inflation ratio in acute respiratory distress syndrome a clinical trial. Am J Respir Crit Care Med. 2020;201:178–87.
Chen L, Chen GQ, Shore K, Shklar O, Martins C, Devenyi B, et al. Implementing a bedside assessment of respiratory mechanics in patients with acute respiratory distress syndrome. Crit Care Critical Care. 2017;21:1–11.
Dellamonica J, Lerolle N, Sargentini C, Beduneau G, Di Marco F, Mercat A, et al. PEEP-induced changes in lung volume in acute respiratory distress syndrome. Two methods to estimate alveolar recruitment. Intensive Care Med. 2011;37:1595–604.
Grieco DL, Pintaudi G, Bongiovanni F, Anzellotti GM, Menga LS, Cesarano M, et al. Recruitment-to-inflation ratio assessed through sequential end-expiratory lung volume measurement in acute respiratory distress syndrome. Anesthesiology. 2023;139(6):801–14.
Guillon A, Preau S, Aboab J, Azabou E, Jung B, Silva S, et al. Preclinical septic shock research: why we need an animal ICU. Ann Intensive Care. 2019. https://doi.org/10.1186/s13613-019-0543-6.
Rosenthal C, Caronia C, Quinn C, Lugo N, Sagy M. A comparison among animal models of acute lung injury. Crit Care Med. 1998;26:912–6.
Mercat A, Richard JCM, Vielle B, Jaber S, Osman D, Diehl JL, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:646.
Sinha P, Calfee CS, Beitler JR, Soni N, Ho K, Matthay MA, et al. Physiologic analysis and clinical performance of the ventilatory ratio in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2019;199:333–41.
Grasso S, Terragni P, Mascia L, Fanelli V, Quintel M, Herrmann P, et al. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med. 2004;32:1018–27.
Camporota L, Camporota L, Caricola EV, Caricola EV, Caricola EV, Bartolomeo N, et al. Lung recruitability in severe acute respiratory distress syndrome requiring extracorporeal membrane oxygenation. Crit Care Med. 2019;47:1177–83.
Gattinoni L, Pelosi P, Crotti S, Valenza F. Effects of positive end-expiratory pressure on regional distribution of tidal volume and recruitment in adult respiratory distress syndrome. Am J Respir Crit Care Med. 1995;151:1807–14.
Gattinoni L, Pesenti A, Bombino M, Baglioni S, Rivolta M, Rossi F, et al. Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology. 1988;69:824–32.
Chiumello D, Marino A, Brioni M, Cigada I, Menga F, Colombo A, et al. Lung recruitment assessed by respiratory mechanics and computed tomography in patients with acute respiratory distress syndrome what is the relationship? Am J Respir Crit Care Med. 2016;193:1254–63.
Gattinoni L, Marini JJ, Pesenti A, Quintel M, Mancebo J, Brochard L. The, “baby lung” became an adult. Intensive Care Med. 2016;42:663–73.
Langer T, Castagna V, Brusatori S, Santini A, Mauri T, Zanella A, et al. Short-term physiologic consequences of regional pulmonary vascular occlusion in pigs. Anesthesiology. 2019;131:336–43.
Zeng C, Zhu M, Motta-Ribeiro G, Lagier D, Hinoshita T, Zang M, et al. Dynamic lung aeration and strain with positive end-expiratory pressure individualized to maximal compliance versus ARDSNet low-stretch strategy: a study in a surfactant depletion model of lung injury. Crit Care. 2023;27:307.
Constantin J-M, Jabaudon M, Lefrant J-Y, Jaber S, Quenot J-P, Langeron O, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019;7:870–80.
Kacmarek RM, Villar J, Sulemanji D, Montiel R, Ferrando C, Blanco J, et al. Open lung approach for the acute respiratory distress syndrome: a pilot, randomized controlled trial. Crit Care Med. 2016;44:32–42.
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36.
Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:637–45.
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura ÉA, Laranjeira LN, de Paisani DM, Damiani LP, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335–45.
Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2019;321:846–57.
Grassi A, Teggia-Droghi M, Borgo A, Szudrinsky K, Bellani G. Feasibility of setting the tidal volume based on end-expiratory lung volume: a pilot clinical study. Crit Care Explor. 2024;6: e1031.
Amato MBP, Santiago RRDS. The recruitability paradox. Am J Respir Crit Care Med. 2016;193:1192–5.
Chiumello D, Cressoni M, Carlesso E, Caspani ML, Marino A, Gallazzi E, et al. Bedside selection of positive end-expiratory pressure in mild, moderate, and severe acute respiratory distress syndrome. Crit Care Med. 2014;42:252–64.
Protti A, Santini A, Pennati F, Chiurazzi C, Cressoni M, Ferrari M, et al. Lung response to a higher positive end-expiratory pressure in mechanically ventilated patients with COVID-19. Chest. 2022;161:979–88.
Grieco DL, Maggiore SM, Bellani G, Spadaro S, Spinelli E, Tonetti T, et al. Individualized positive end-expiratory pressure guided by end-expiratory lung volume in early acute respiratory distress syndrome: study protocol for the multicenter, randomized IPERPEEP trial. Trials. 2022. https://doi.org/10.1186/s13063-021-05993-0.
Del Sorbo L, Tisminetzky M, Chen L, Brochard L, Arellano D, Brito R, et al. Association of lung recruitment and change in recruitment-to-inflation ratio from supine to prone position in acute respiratory distress syndrome. Crit Care. 2023;27:140.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
F.M., D.L.G. and S.G. conceived the study, carried out the measurements and data analysis and drafted the manuscript. L.P, R.D.M and S.S. participated in the study design and revised the manuscript. N.B. conducted the signal and statistical analysis. M.F., A.M.C, L.L. and F.S made substantial contributions to data acquisition. All authors read and approved the final manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted following approval of the Italian Ministry of Education, University and Research Committee (Prot. n.1234/2020-PR).
Consent for publication
Available.
Competing interests
Salvatore Grasso in the past 2 years received fees for lectures and board membership from: Getinge Critical Care (Solna SW), Estor Critical Care (Pero, Milan Italy). Domenico Luca Grieco has received speaking fees by Gilead, Intersurgical, MSD and GE, reports having received travel accommodation by Fisher and Paykel, and discloses a research grant by GE. The other authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murgolo, F., Grieco, D.L., Spadaro, S. et al. Recruitment-to-inflation ratio reflects the impact of peep on dynamic lung strain in a highly recruitable model of ARDS. Ann. Intensive Care 14, 106 (2024). https://doi.org/10.1186/s13613-024-01343-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01343-w