Abstract
Background
At present, unequal allocation of medical resources represents a major problem for medical service management in China and many other countries. Equity of intensive care unit (ICU) bed allocation is essential for timely and equitable access to medical care for critically ill patients. This study analysed the equity of ICU bed allocation in 31 provincial regions in China, and the associated factors, to provide a theoretical basis for improvement in the allocation of ICU beds.
Methods
The equity of ICU bed allocation was investigated in 31 provincial regions in China in 2021. The Gini coefficient combined with Lorenz curves were used to analyse the current status of ICU bed allocation by both population and service area. The spatial heterogeneity and aggregation of ICU bed density were analysed using the Global Moran’s index. The spatial distribution pattern was visualized via LISA maps using the Local Moran’s index. Three grey correlation models were constructed to assess the key factors influencing ICU bed density. Finally, robustness analysis was performed to test the reliability of the results.
Results
The allocation of ICU beds in China was highly inequitable by service area (Gini = 0.68) and showed better balance by population distribution (Gini = 0.14). The distribution of ICU beds by service area was highly spatially clustered (Global Moran’s I = 0.22). The bed utilization rate exhibited the strongest association with ICU bed density by population. Registered nurses per 10,000 square kilometres was the strongest factor affecting ICU bed density by service area.
Conclusions
The allocation of ICU beds by population is better than by service area; the allocation by service area is less equitable in China. These findings emphasise the need to implement better measures to reduce ICU bed equity differences between regions and balance and coordinate medical resources. Service area size, bed utilization, the number of registered nurses and other key factors should be considered when performing regional health planning for ICU bed supply. This will increase the equitable access to critical medical services for all populations.
Similar content being viewed by others
Text box 1. Contribution to the literature |
|---|
• The distribution of ICU beds by service area was highly spatially clustered in China. |
• The bed utilization rate and the number of registered nurses per 10,000 square kilometres exhibited the strongest associations with ICU bed density. |
• A methodological process for analysing the distribution of health resources was described. |
• ICU bed planning should take into account regional socioeconomic conditions, health human resources and medical services factors. |
Background
The balanced allocation of high-quality medical resources has always been a goal of the Chinese healthcare service. While studies have identified large regional differences in health resource allocation in China, a downward fluctuating trend has been observed since 2008 [1, 2]. Nonetheless, the contradiction between people’s demand for quality medical services and the uneven distribution of quality medical resources remains prominent. An imbalance in the spatial distribution of health resources is the main manifestation of inequity, especially between urban and rural areas in China.
Intensive care unit (ICU) beds are important but scarce medical resources in China and other countries globally. A study by the American Society of Critical Care Medicine in 2020 showed that there were 34.7 ICU beds per 100,000 people in the United States. Germany had 29.2 ICU beds per 100,000 people. South Korea had 10.6 ICU beds per 100,000 people. However, China had only 3.6 ICU beds per 100,000 people. Many studies have examined the availability of critical care services in many developed countries [3,4,5,6]. Results consistently show that the number of ICU beds is increasing, but most of this growth is occurring in a small number of highly populated regions. These findings highlight the need to implement inter-jurisdictional resource sharing during periods of substantially increased demand. Inadequate ICU beds lead to longer waits for critically ill patients, which increases inpatient mortality [7, 8].
In 1974, Townsend [9] published a discussion on the inequity of healthcare services in the Lancet. Since then, scholars around the world have continued to examine the fairness of the distribution of healthcare resources at different levels, such as the national, urban and community levels [10,11,12]. Improving the spatial equity of the distribution of healthcare resources is an important step in achieving equity in healthcare delivery [13]. Evaluation of intensive care services in hospitals is one of the most important indicators of the equity of healthcare services [14]. Song [15] found that spatial inequities in bed allocation can lead to disparities in access to care. At the same time, an inequitable spatial distribution of beds could also significantly impact healthcare outcomes, leading to higher cancer mortality rates for patients located outside of cities [16]. A study in Italy [17] found that ICU beds were more concentrated in densely populated urban areas while rural areas did not have access to intensive care services.
While a body of literature has explored the equitable distribution of health resources or hospital beds, there remains a lack of research on the equity of the distribution of ICU beds. For example, Xin and Yang found that mental health beds and health resource allocation were relatively equitably distributed with respect to the population distribution; however, the distribution of mental health beds by geographic region was inequitable [18, 19]. Although several studies have examined the relationship between hospital bed allocation and equity, most have only analysed the current situation. In addition, existing research lacks an analysis of the factors affecting critical care bed allocation.
Socioeconomic conditions may be an important factor leading to spatial inequality of health resources. Phua et al. found that the critical care bed capacity varies widely across Asia and is significantly lower in low- and lower-middle-income countries and regions, as compared to upper-middle-income and high-income countries and regions [20]. Studies have shown that the size of the elderly population, local economic development, and health investment by government departments are key factors influencing the allocation of beds [21,22,23,24,25]. Health human resources also make a spatial difference in the bed distribution. Using a retrospective decadal analysis, one study found that preferential policies have been successful in increasing the number of beds in health facilities, but not the number of healthcare workers in ethnic minority regions. A large body of evidence supports an association between medical services and the spatial distribution of beds. Chow et al. found that the supply of emergency department beds cannot keep pace with the growing patient demand for acute care in California [26]. In summary, socioeconomic conditions, human resources for health, and healthcare delivery should be considered as factors influencing critical care bed allocation.
The aim of this study was to address the above gaps in the literature by assessing the spatial equity of the distribution of ICU beds in China and identifying key influencing factors. This study also provides a standardized methodological process for analysing the distribution of health resources. The results offer a basis for policy decisions and the allocation of intensive care resources in China and other similar countries.
Methods
Data source
The number of beds in this study was defined as the actual number of beds in the intensive care medicine departments of hospitals in 31 provinces and regions of mainland China in 2021. The number of ICU beds, the number of hospital admissions and discharges, the bed utilization rate, the number of practising physicians, and the number of registered nurses (RNs) were extracted from the China Health Statistics Yearbook 2022. The regional population and per capita GDP were derived from the China Statistical Yearbook 2022. The service area data were obtained from the Statistical Table of Administrative Divisions published by the Ministry of Civil Affairs.
Main variables
The main indicator, ICU bed allocation, was assessed based on the number of ICU beds by population and by service area. The number of ICU beds per 100,000 population (ICU bed density by population) was calculated based on the total number of ICU beds in each province in China in 2021 divided by the total population of the corresponding province. Similarly, the number of ICU beds per 10,000 square kilometres (ICU bed density by service area) was calculated based on the total number of ICU beds in each province in 2021 divided by the land area of each province. According to the availability of data, this study analysed the spatial distribution of ICU beds by province in China in 2021.
The allocation of ICU beds is influenced by diverse and complex factors including socioeconomic conditions, health human resources, and medical services in every province. The indicators of socioeconomic conditions used in this study included the size of the population aged 65 years and above, per capita GDP, and health expenditure as a percentage of fiscal expenditure. The indicators of health human resources included the number of practising physicians per 100,000 population, the number of practising physicians per 10,000 square kilometres, the number of RNs per 100,000 population and the number of RNs per 10,000 square kilometres. The indicators of medical services included the number of patients discharged from ICU, the inpatient mortality rate, the bed utilization rate, the average length of stay and the daily inpatient bed days for physicians. The details are shown in Table 1.
Statistical analysis
Figure 1 depicts a methodological flow chart of the study. Based on the allocation of ICU beds in the 31 provincial regions in China, fairness analysis and evaluation were first performed using the Gini coefficients and Lorenz curves. Second, the spatial heterogeneity and aggregation of ICU bed allocation were evaluated via spatial autocorrelation analysis. Third, grey relational models were used to analyse the key factors influencing the allocation of ICU beds. Finally, a robustness test was performed. The health resource agglomeration degree (HRAD) was examined to verify the Gini coefficient and spatial aggregation analyses, and correlation analysis was performed to test the robustness of the grey relational models.
Lorenz curves and Gini coefficients
The Lorenz curve is a curve that reflects the equity of income distribution or property distribution in society. It is now also widely used in studies of equity in the distribution of health resources [27, 28]. This is accomplished by using the cumulative percentage of the population or area as the horizontal axis and the cumulative ratio of ICU beds as the coordinates. Then, the Lorenz curve is plotted by connecting these points. In a Lorenz curve graph, the diagonal line is the line of absolute equity. The closer the Lorenz curve is to the line of perfect equity, the better the equity. Absolute fairness is reached when the Lorenz curve overlaps with the line of perfect fairness.
The Gini coefficient is widely used to assess inequities in the distribution of health resources. It is the best quantitative indicator for evaluating the equity of resources [29]. It is calculated by the ratio of the area between the Lorenz curve and the diagonal versus the entire area below the diagonal. The Gini coefficient ranges from 0 to 1. The higher the value of the Gini coefficient, the greater the inequality. Different Gini coefficient values indicate different degrees of fairness: a value less than 0.2 suggests absolute fairness; a value between 0.2 and 0.3 suggests relative fairness; a value between 0.3 and 0.4 suggests adequate fairness; a value higher than 0.4 indicates relative unfairness; a value higher than 0.5 indicates absolute unfairness [30]. In this study, the Gini coefficient was calculated according to the following formula [31]:
In the formula, n is the number of provinces (here, n = 31); Xi is the cumulative proportion of the population (or service area) of each province to the population (or service area) of China; Yi is the cumulative proportion of the number of ICU beds in each province to the number of ICU beds in the country, ordered from the smallest to the largest ICU bed ratio in each province. All data analyses were performed in STATA 16.0.
Global and local spatial autocorrelation analysis
In order to assess the correlations between ICU beds and their spatial locations in each province of China, global and local spatial autocorrelation analyses were performed by calculating the Global Moran’s Index and Local Moran’s Index, respectively. The test level was set at α = 0.05. A Moran’s I greater than zero indicates that the study unit has a positive spatial autocorrelation. A Moran’s I less than zero indicates that the study unit has a negative spatial autocorrelation. A Moran’s I equal to zero indicates that the study unit has no autocorrelation; it has a random distribution. The Global Moran’s I was used to assess the overall spatial autocorrelation. The Local Moran’s I was used to estimate the local autocorrelations between individual provinces and their neighbouring provinces by plotting the Local Indicators of Spatial Association (LISA). The formula for the Global Moran’s I is as follows [32]:
where n is the total number of provinces (n = 31); xi and xj are the population/service area of provinces i and j; \(\:\stackrel{-}{x}\) is the average number of ICU beds per population/service area for the 31 provinces; and wij is the spatial weight between provinces i and j.
The equation used to calculate Local Moran’s I is as follows [32]:
The parameters in Eq. (3) are defined as described for Eq. (2). The results of the Local Moran’s I analysis contain five types. Among them, “high-high”, “high-low”, “low-high” and “low-low” are four significant types. The “high-high” and “low-low” types represent a high/low level of ICU beds in a province and a high/low level of ICU beds in its neighbouring provinces. The “high-low” and “low-high” types represent high/low levels of ICU beds in a province, but low/high levels of ICU beds in neighbouring provinces. The “no statistically significant difference” type means that there is no significant correlation between the level of ICU beds in the province and its neighbouring provinces. This indicates that the allocation of ICU beds in each province is randomly distributed. The spatial autocorrelation analysis was performed using Arc Gis 10.5 software.
Grey relational analysis
In this study, GRA models were used to examine the extent of influence of various indicators on the distribution of ICU beds by population/service area. GRA models have been successfully applied in many fields such as engineering, management science, economics, environmental science, energy and healthcare/nursing [33, 34]. In 1985, Deng [35] added grey relational grade (GRG) to the GRA model; this model has a value between 0.5 and 1. The closer the value is to 1, the higher the correlation. Three related GRA models were utilized in this study. Deng’s GRA model measures the effect of one variable on another [36]. X0=(x0(1), x0(2), ., x0(n)) is the underlying/reference sequence representing the dependent variable. Xi=(xi(1), xi(2), ., xi(n)) is a set of comparison sequences representing the independent variables. GRG γ0i or γ(X0, Xi) is derived after a series of operations. Deng’s GRG is given by Eq. (4) and Eq. (5) [37]. Absolute GRG measures the association or correlation between variables [38]. If Xi= (xi(1), xi(2), ., xi(n)) and Xj=(xj(1), xj(2), ., xj(n)) are two data series representing two variables related to ICU beds, the absolute GRG Eq. (6) is derived. The second synthetic GRA (SSGRA) model is given by Eq. (7) [39].
where δ∈(0,1) is the discriminant coefficient; the value of δ is usually taken as 0.5 [39].
where \(\:{\rho\:}\) represents the second synthetic (SS) GRG; ɛ represents the absolute GRG; and γ represents the GRG between the grey data sequences Xi and Xj. Deng’s GRG relies on grey relational/incidence coefficients of particular points, the absolute GRG relies on an integral (relatively comprehensive) perspective, whereas the SS GRG reflects the overall closeness between two sequences based on particular points and integral perspectives.
HRAD
Spatial equity in the distribution of ICU beds was examined using the health resource agglomeration method [40]. The HRAD reflects the proportion of the total number of ICU beds in a region that are clustered in 1% of the country’s service area. HRADi>1 indicates that the fairness of ICU bed allocation is high by geographic size in a region. HRADi=1 indicates that the allocation of ICU beds by service area in a region is in absolute fairness. HRADi<1 indicates that the allocation of ICU beds by service area in a region is in poor fairness [40]. The calculation formula is as follows:
where HRi denotes the number of ICU beds in a region; HRn denotes the total number of ICU beds in the country; Ai denotes the service area of a region; and An denotes the service area of the country.
Correlation analysis
Spearman’s rank correlation analysis was performed to test the robustness of the GRA results. The raw data for the included variables affecting ICU bed density were converted into rank data. Based on their average descending position in the overall data, a corresponding rank was assigned, and Spearman’s rank correlation coefficients were calculated. Factors with high correlations were identified to explore the factors that play a dominant role in the ICU bed density.
Results
Basic data on ICU beds
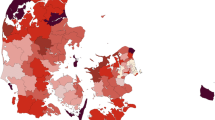
The distribution of ICU beds by population in the 31 provinces in 2021 is shown in Fig. 2. The distribution of ICU beds by service area is shown in Fig. 3. It can be seen that the overall distribution of ICU beds by population was relatively uniform. Bed density by service area was not uniform and was concentrated in more developed provinces such as Beijing and Shanghai.
The national average number of beds per 100,000 population was 4.46 and the average number of beds per 10,000 square kilometres was 213.0. Among the 31 provinces in China, the top three provinces in terms of the number of beds per 100,000 population were Henan, Xinjiang and Zhejiang; the bottom three provinces were Ningxia, Tibet and Jilin. The top three regions in terms of the number of beds per 10,000 square kilometres were Shanghai, Beijing and Henan. The bottom three regions were Inner Mongolia, Qinghai and Tibet. The allocation of ICU beds by population and service area in each province in China is shown in Supplementary File 1.
Equity analysis of ICU beds
Lorenz curves of ICU beds by population and service area at the provincial level in China are shown in Fig. 4. The Gini coefficients of provincial-level ICU beds by population and service area in 2021 were 0.14 and 0.68, respectively. ICU bed allocation by population showed absolute equity, but ICU bed allocation by service area showed absolute unfairness.
Spatial autocorrelation analysis of ICU beds
In 2021, the Global Moran’s I for critical care beds by population allocation was 0.04, but the p value was 0.51 (p > 0.05). This indicates that the difference in ICU bed configuration by population was not statistically significant and there was no significant spatial autocorrelation. The Global Moran’s I allocated by service area was 0.22 (p < 0.05), showing significant spatial clustering. This indicates that the areas with an abundance (or scarcity) of ICU beds in the 31 provinces in China exhibited more concentrated spatial geographic distributions.
Because the p-value of the Global Moran’s I for ICU beds distributed by population was not significant, there was no research significance for performing local autocorrelation analysis for ICU beds allocated by population. Thus, the local autocorrelation analysis only examined ICU beds allocated by service area. The results of the local spatial autocorrelation analysis of ICU beds distributed by area are shown in Fig. 5. The “high-high” type was concentrated in Jiangsu and Zhejiang in eastern China. The “low-low” type was concentrated in Xinjiang, Tibet, Qinghai, Gansu Province, Sichuan, Ningxia and Inner Mongolia in western China. The “high-low” type was observed in Heilongjiang in the central region. There were no “low-high” clusters. The overall picture is one of “low-low” agglomeration in western China and “high-low” agglomeration in central China. The central region was characterized by “high-low” aggregation, with occasional “low-low” aggregation. “High-high” clusters were observed in the eastern region. The rest of the country exhibited non-significant distributions.
Grey correlation analysis of ICU bed allocation
Factors affecting health resource allocation were extracted according to a literature review. A total of 12 indicators in three major categories were screened and analysed as variables affecting the allocation of ICU beds in this study, as shown in Table 1.
The results of the grey correlation ranking of ICU beds allocated by service area differed significantly from those configured by population (Table 2). For ICU beds allocated by service area, Deng’s GRA model and the SS GRA model showed that the number of RNs per 10,000 square kilometres significantly influenced (and was correlated with) ICU bed allocation. In contrast, the absolute GRA model showed that the number of practising physicians per 100,000 population was the most important factor in the distribution of ICU beds. This was followed by the average length of stay in hospital, the number of RNs per 100,000 population, and the bed utilization rate.
Robustness analysis
Clustering degree analysis of ICU beds based on geographical density
According to the geographical distribution of ICU beds, there were obvious differences in the allocation of ICU bed resources among different provinces. The average HRAD of the 31 provinces was 3.06. This indicates that the distribution of ICU bed resources was generally equitable. However, the HRAD values of Shaanxi, Yunnan, Ningxia, Gansu, Heilongjiang, Jilin, Xinjiang, Inner Mongolia, Qinghai and Tibet were all less than 1. This indicates that the allocation of ICU bed resources in these regions was in a state of scarcity in terms of geographical distribution, and the fairness of service area allocation was slightly worse. Aside from the 10 provinces mentioned above, the remaining 21 provinces had HRAD values of ICU beds greater than 1. This suggests that these 21 provinces had better equity in the allocation of ICU bed resources. The difference between the province with the largest and the smallest degree of clustering was 2237 times (Shanghai 22.37, Tibet 0.01). This verifies the existence of provincial inequity in the allocation of ICU beds by service area and obvious geographic aggregation. The full details of the HRAD analysis of ICU beds by service area in China are presented in Supplementary File 2.
Correlation analysis
The density of ICU beds according to population was positively correlated with only the number of discharged patients. The correlation coefficient was 0.549. In contrast, the number of ICU beds by service area was correlated with multiple variables. The ranking of correlation coefficients from largest to smallest was as follows: the number of practising physicians per 10,000 square kilometres was 0.972; the number of RNs per 10,000 square kilometres was 0.968; the proportion of health expenditure to fiscal expenditure was 0.697; the per capita GDP was 0.659; the utilization rate of hospital beds was 0.533; the number of people aged 65 years and above was 0.513. These results are consistent with the rank outcome of the grey correlation analysis. The full correlation analysis results are detailed in Supplementary File 3.
Discussion
The purpose of this study was to understand the spatial equity of ICU bed allocation in mainland China and explore the key factors influencing the density of ICU beds, so as to provide a reference for the rational allocation of ICU beds.
The results revealed that there was significant unfairness in the allocation of ICU beds by service area in China. The distribution of beds in provinces and cities was uneven and the gap was large. For example, the density of ICU beds in Shanghai and Beijing exhibited absolute advantages. The numbers of ICU beds per 10,000 square kilometres in the three provinces in southwest China were less than 1/10 of those in Shanghai and Beijing. Even Hebei, which borders Beijing, was ranked at the bottom of the eastern region. Previous studies have assessed the equity of the allocation of health resources in China, finding that the resource allocation in Xinjiang, Guangdong, Gansu and other regions was quite different, with unfair service allocation [41,42,43]. This is related to the long-standing population-oriented bed allocation policy in China. When service area allocation is taken into account, sparsely populated regions like Inner Mongolia and Tibet will have fewer ICU beds. Health resource allocation policy based on allocation by population rather than by area can ensure a more equitable distribution of beds. Similar results have been found in other studies [44]. Bed allocation shows obvious economic clustering. Regional economic imbalances are also an important factor affecting the distribution of beds.
A study in Iran found that when indicators of available treatment beds are low and unevenly distributed, beds can be allocated using criteria such as geography, demographics, length of stay and bed utilization to establish a balance between demand and supply [45]. Similar to the situation in China, there are significant regional differences in the allocation of health resources in Sudan, and a resource allocation model that takes into account the population size and health outcome variables of each state has been adopted [46]. These strategies to address unequal allocation of health resources by service area are worthy of attention in developing countries.
In addition, the current results demonstrated that the spatial distribution of ICU beds in China exhibited obvious geographical clustering. Among them, the high-high area of ICU beds was mainly distributed in the eastern region, and the low-low area was concentrated in the western region. Jiangsu and Zhejiang, which are economically developed areas in the east, are densely divided, and these two regions have some of the highest-quality hospital resources in the country. Therefore, the number of ICU beds per square kilometre is high, resulting in a high-high type area. In the geographically remote western and some central regions, the large area leads to an extreme shortage of ICU beds per square kilometre. Research by Pan [47] demonstrated that western China provinces are at a distinct disadvantage in terms of bed allocation. The eastern provinces are able to allocate more critical care beds due to the advantage of their rich medical resources. Under the market economic system, the allocation of health resources tends to cluster in the central city. Another reason for the geographical agglomeration of ICU bed allocation is the regional imbalance of economic development. Differences in location and economic development affect the level of healthcare resource concentration and produce the Matthew effect (the poorer get poorer, the richer get richer). The current results suggest that the Chinese government needs to focus on the 10 provinces where HRAD values were low, including Shaanxi, Yunnan, Ningxia, Gansu, Heilongjiang, Jilin, Xinjiang, Inner Mongolia, Qinghai and Tibet. Geographic factors should be properly considered in order to implement a more equitable regional allocation policy for ICU beds.
Several factors were found to influence ICU bed allocation by population and service area. Here, we discuss the top-ranked correlates. One of the most important indicators influencing the allocation of beds by population was the number of discharges from the ICU. This is consistent with the findings of existing studies [48, 49]. This finding suggests that the demand for ICU beds in a region is the central factor influencing the distribution of beds. This result implies that the ICU bed allocation strategy based on population is consistent with the supply-demand economy principle in China. However, ICU beds are a scarce health resource, thus, equity principles are also very important. Allocation only according to population may lead to spatial inequality. The current results suggest that the strategy of allocating ICU beds by population in China satisfies the economic principle of balancing supply and demand. When critically ill patients can be discharged quickly, the vacated beds can be used for other patients in need of critical care, thus improving the efficiency of treatment and solving the problem of insufficient beds in critical situations.
Previous studies have reported that nurses are more closely associated with inpatient services [50]. The current study examined the impact of the number of RNs on ICU bed density. This variable ranked highly in the bed density analysis both per 100,000 population and per 10,000 square kilometres. RN allocation was more sensitive to ICU bed density compared to practising physicians. The number of people over the age of 65 years was also an important correlate of ICU beds allocated by area. As the population ages, these older individuals may be more likely to require critical care. The GDP per capita was also associated with the allocation of ICU beds. This is consistent with the results of Chen, who found that GDP can have a positive impact on health resource allocation [51]. According to the current study results, it is recommended that the allocation of ICU beds be planned and rationalized on the basis of the socioeconomic development, demographic structure, health and disease conditions, needs of different populations, and hospital operations in the 31 provinces in China.
Conclusions
Reducing spatial inequality in ICU bed allocation by service area should be one of the key policy objectives for the high-quality development of China’s healthcare system. The results of this study suggest that there is a large disparity in the distribution of ICU beds per square kilometre across different regions in China. However, there is little disparity in the distribution of ICU beds per 100,000 population. No significant spatial autocorrelations were observed in the aggregation of ICU beds by population allocation, while significant aggregation was observed by service area distribution. The bed utilization rate had the strongest association with ICU bed allocation by population. The geographic density of RNs was a strong factor associated with ICU bed allocation by service area. Adequate numbers of practising physicians and RNs can help to balance the critical care bed spatial allocation and improve the spatial equity of access to critical care services.
Strengths and limitations of the study
Several limitations of this study should be noted. First, this study was cross-sectional. Therefore, it was not possible to evaluate the trends in the evolution of critical care bed density during the recent healthcare reform process in China or to explore causality. Moreover, this study considered a limited number of correlates and may have omitted important influential variables. Third, the feasibility, cost-effectiveness and potential unintended consequences of the policy recommendations proposed in this study were not fully considered. Based on this, subsequent studies could conduct more detailed research on the factors affecting ICU bed allocation.
Data availability
The survey data collected and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive Care Unit
- GDP:
-
Gross Domestic Product
- HRAD:
-
Health Resource Agglomeration Degree
- LISA:
-
Local Indicators of Spatial Association
- GRA:
-
Grey Relational Analysis
- GRG:
-
Grey Relational Grade
- SSGRA:
-
Second Synthetic GRA
References
Li Q, Wei J, Jiang F, Zhou G, Jiang R, Chen M, Zhang X, Hu W. Equity and efficiency of health care resource allocation in Jiangsu Province, China. Int J Equity Health. 2020;19(1):211.
Wang Z, He H, Liu X, Wei H, Feng Q, Wei B. Health resource allocation in Western China from 2014 to 2018. Arch Public Health. 2023;81(1):30.
David J, Wallace DC, Angus CW, Seymour AE, Barnato, Kahn JM. Critical care bed growth in the United States. A comparison of regional and national trends. Am J Respir Crit Care Med. 2015;191(4):410–6.
Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–53.
Martin JM, Hart GK, Hicks P. A unique snapshot of intensive care resources in Australia and New Zealand. Anaesth Intensive Care. 2010;38(1):149–58.
Robert A, Fowler P, Abdelmalik G, Wood D, Foster N, Gibney N, Bandrauk, Alexis F, Turgeon et al. François Lamontagne, Anand Kumar, Ryan Zarychanski: Critical care capacity in Canada: results of a national cross-sectional study. Critical care 2015, 19(1):133.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Barnaby DP, Becker LB, Chelico JD, Cohen SL, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–9.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):2120.
Townsend P. Inequity and the Health Service. Lancet. 1974;1(7868):1179–90.
Alexander GL, Madsen RW, Miller EL, Wakefield DS, Wise KK, Alexander RL. The state of nursing home Information Technology Sophistication in Rural and Nonrural US markets. J Rural Health. 2017;33(3):266–74.
Fylkesnes K, Jakobsen MD, Henriksen NO. The value of general health perception in health equity research: a community-based cohort study of long-term mortality risk (Finnmark cohort study 1987–2017). SSM - Popul Health. 2021;15(634):100848.
Evans NG, Sekkarie MA. Allocating scarce medical resources during armed conflict: ethical issues. Disaster Military Med. 2017;3(1):5.
Whitehead J, Pearson AL, Lawrenson R, Atatoa-Carr P. Framework for examining the spatial equity and sustainability of general practitioner services. Aust J Rural Health. 2018;26(5):336–41.
Losonczy LI, Papali A, Kivlehan S, Calvello Hynes EJ, Calderon G, Laytin A, Moll V, Al Hazmi A, Alsabri M, Aryal D, et al. White Paper on early critical care services in low resource settings. Ann Glob Health. 2021;87(1):105.
Song C, Wang Y, Yang X, Yang Y, Tang Z, Wang X, Pan J. Spatial and temporal impacts of socioeconomic and environmental factors on Healthcare resources: A County-Level bayesian local Spatiotemporal regression modeling study of Hospital beds in Southwest China. Int J Environ Res Public Health. 2020;17(16):5890.
Oliveira NPD, Cancela MC, Martins LFL, de Souza DLB. Spatial distribution of advanced stage diagnosis and mortality of breast cancer: socioeconomic and health service offer inequalities in Brazil. PLoS ONE. 2021;16(2):e0246333.
Pecoraro F, Luzi D, Clemente F. Spatial inequity in Access to Intensive Care Unit beds at Regional Level in Italy. Stud Health Technol Inf. 2021;281:809–13.
Xin F, Zhang W, Guo Y, Cai J, Xie B. Equity assessment of the distribution of mental health beds in China: based on longitudinal data from 2011 to 2020. BMC Health Serv Res. 2022;22(1):1453.
Jin J, Wang J, Ma X, Wang Y, Li R. Equality of Medical Health Resource Allocation in China based on the Gini Coefficient Method. Iran J Public Health. 2015;44(4):445–445.
Phua J, Kulkarni AP, Redjeki IS, Sann KK, Shrestha BR, Palo JEM, Hashemian SMR, Nor MBM, Patjanasoontorn B, Ling L, et al. Critical Care Bed Capacity in Asian countries and regions. Crit Care Med. 2020;48(5):654–62.
Yong Zhou K, Zhao J, Han S, Zhao, Cao J. Geographical pattern evolution of Health resources in China: spatio-temporal dynamics and spatial mismatch. Trop Med Infect Disease. 2022;7(10):292.
Luo F, Huang Y, Jiang L, Gou QF. Ethnic disparities and temporal trends in health resource allocation: a retrospective decadal analysis in Sichuan, a multi-ethnic Province of Southwest China (2009–2019). BMC Health Serv Res. 2024;24(1):541.
Wells CL-VM, Brett S. Exploratory study of staff perceptions of shift safety in the critical care unit and routinely available data on workforce, patient and organisational factors. BMJ Open. 2020;10(6):e034101.
Marshall MF, Schwenzer KJ, Orsina M, Fletcher JC Jr. Influence of political power, medical provincialism, and economic incentives on the rationing of surgical intensive care unit beds. Crit Care Med. 1992;20(3):387–94.
Jay Pan, Shallcross D. Geographic distribution of hospital beds throughout China: a county-level econometric analysis. Internationa J Equity Health. 2016;15(1):19.
Chow JL, Niedzwiecki MJ, Hsia RY. Trends in the supply of California’s emergency departments and inpatient services, 2005–2014: a retrospective analysis. BMJ Open. 2017;7(5):e014721.
Lope DJ, Demirhan H, Dolgun A. Bayesian estimation of the effect of health inequality in disease detection. Int J Equity Health. 2022;21(1):118.
Fan X, Zhang W, Guo Y, Cai J, Xie B. Equity assessment of the distribution of mental health beds in China: based on longitudinal data from 2011 to 2020. BMC Health Serv Res. 2022;22(1):1453.
Yan W, Qin C, Tao L, Guo X, Liu Q, Du M, Zhu L, Chen Z, Liang W, Liu M, et al. Association between inequalities in human resources for health and all cause and cause specific mortality in 172 countries and territories, 1990–2019: observational study. BMJ. 2023;381:e073043.
Erdenee O, Paramita SA, Yamazaki C, Koyama H. Distribution of health care resources in Mongolia using the Gini coefficient. Hum Resour Health. 2017;15(1):56.
Hsu YE, Lin W, Tien JJ, Larry TY. Measuring inequality in physician distributions using spatially adjusted Gini coefficients. Int J Qual Health C. 2017;28(6):657–64.
Tappo S, Laohasiriwong W, Puttanapong N. Spatial association of socio-demographic, environmental factors and prevalence of diabetes mellitus in middle-aged and elderly people in Thailand. Geospat Health. 2022;17(2):1091.
Yang L, Cheng J. Analysis of inequality in the distribution of general practitioners in China: evidence from 2012 to 2018. Prim Health Care Res Dev. 2022;23:e59.
Anand G, Alagumurthi N, Elansezhian R, Palanikumar K, Venkateshwaran N. Investigation of drilling parameters on hybrid polymer composites using grey relational analysis, regression, fuzzy logic, and ANN models. J Braz Soc Mech Sci. 2018;40(4):214.
David K. Grey system and grey relational model. ACM SIGICE Bull. 1994;20(2):2–9.
Javed SA, Syed AM, Javed S. Perceived organizational performance and trust in project manager and top management in project-based organizations. Grey Syst. 2018;8(3):230–45.
Liu S, Zhang H, Yang Y. Explanation of terms of grey incidence analysis models. Grey Syst. 2017;7(1):136–42.
Wang Y, Gao Y, Sun L, Li Y, Zheng B, Zhai W. Effect of physical properties of Cu-Ni-graphite composites on tribological characteristics by grey correlation analysis. Results Phys. 2017;7:263–71.
Javed SA, Liu S, Mahmoudi A, Nawaz M. Patients’ satisfaction and public and private sectors’ health care service quality in Pakistan: application of grey decision analysis approaches. Int J Health Plann Manage. 2018;34(1):e168–82.
Dai G, Li R, Ma S. Research on the equity of health resource allocation in TCM hospitals in China based on the Gini coefficient and agglomeration degree: 2009–2018. Int J Equity Health. 2022;21(1):145.
Su W, Du L, Fan Y, Wang P. Equity and efficiency of public hospitals’ health resource allocation in Guangdong Province, China. Int J Equity Health. 2022;21(1):138.
Liu Y, Niu H, Tian X, Zhang M, Jiang F, Qian Y, Cao J. Research on equity of medical resource allocation in Yangtze River Economic Belt under healthy China strategy. Front Public Health. 2023;21(1):1175276.
Hengna R, Chen L, Huang Y. Spatial and temporal analysis of China’s healthcare resource allocation measurements based on provincial data: 2010–2021. Front Public Health. 2023;11:1269886.
Wen Liu Y, Liu P, Twum, Li S. National equity of health resource allocation in China: data from 2009 to 2013. Internationa J Equity Health. 2016;15:68.
Soroush F, Nabilou B, Faramarzi A, Yusefzadeh H. A study of the evacuation and allocation of hospital beds during the Covid-19 epidemic: a case study in Iran. BMC Health Serv Res. 2022;22(1):864.
Ismail M. Regional disparities in the distribution of Sudan’s health resources. East Mediterr Health J. 2020;26(9):1105–14.
Pan J, Shallcross D. Geographic distribution of hospital beds throughout China: a county-level econometric analysis. Intl J Equity Health. 2016;15(1):179.
Plotnikoff KM, Krewulak KD, Hernandez L, Spence K, Foster N, Longmore S, Straus SE, Niven DJ, Parsons Leigh J, Stelfox HT, et al. Patient discharge from intensive care: an updated scoping review to identify tools and practices to inform high-quality care. Crit Care. 2021;25(1):438.
Cuzco C, Torres-Castro R, Torralba Y, Manzanares I, Munoz-Rey P, Romero-Garcia M, Martinez-Momblan MA, Martinez-Estalella G, Delgado-Hito P, Castro P. Nursing Interventions for Patient Empowerment during Intensive Care Unit Discharge: a systematic review. Int J Environ Res Public Health. 2021;18(21):11049.
Talat C, Ashok P, Gustav S, Vishy V, Suresh A, Ayman EM, Sandro R. Trauma intensive care unit (TICU) at Hamad General Hospital. Qatar Med J. 2019;2019(2):5.
Chen C, Zheng M, Zhu J. How does fiscal decentralization Affect Health outcomes? Evidence from China. Risk Manag Healthc Policy. 2023;16:1893–903.
Acknowledgements
This paper cited the China Health Statistical Yearbooks and China Statistical Yearbooks, which provide the data for this study. We also thank the NativeEE (www.nativeee.com), which offered the edited services.
Funding
This work was funded by the Humanities and Social Sciences Research Planning Fund Program of the Ministry of Education of China (23YJAZH166) and Health Commission of Hubei Province scientific research project (WJ2023Z009).
Author information
Authors and Affiliations
Contributions
CX was responsible for conceptualization and study design. HC, YX, QQ managed, analyzed and interpreted the data. CX, HC and JC wrote the first draft of the paper and revised the manuscript. HC and YX contributed equally to this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, H., Xia, Y., Qin, Q. et al. Spatial equity and factors associated with intensive care unit bed allocation in China. Arch Public Health 82, 169 (2024). https://doi.org/10.1186/s13690-024-01402-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-024-01402-5