Abstract
Background
The purpose of this study was to look into the presence of plasmid-mediated quinolone resistance (PMQR) genes and biofilm formation in several species of clinical Shigella isolates that were resistant to quinolones.
Methods
The stool samples of 150 patients (younger than 10 years) with diarrhea were collected in this cross-sectional study (November 2020 to December 2021). After cultivation of samples on Hektoen Enteric agar and xylose lysine deoxycholate agar, standard microbiology tests, VITEK 2 system, and polymerase chain reaction (PCR) were utilized to identify Shigella isolates. The broth microdilution method was used to determine antibiotic susceptibility. PMQR genes including qnrA, qnrB, qnrC, qnrD, qnrE, qnrS, qnrVC, qepA, oqxAB, aac(6′)-Ib-cr, and crpP and biofilm formation were investigated in quinolone-resistant isolates by PCR and microtiter plate method, respectively. An enterobacterial repetitive intergenic consensus polymerase chain reaction (ERIC-PCR) technique was used to determine the clonal relatedness of quinolone-resistant isolates.
Results
A total of 95 Shigella isolates including S. sonnei (53, 55.8%), S. flexneri (39, 41.1%), and S. boydii (3, 3.2%) were identified. The highest resistance rates of the isolates were against ampicillin (92.6%, n = 88/95). Overall, 42 of 95 (44.2%) isolates were simultaneously resistant against two or more quinolones including 26 (61.9%) S. sonnei and 16 (38.1%) S. flexneri. All isolates were multidrug-resistant (resistance to more than 3 antibiotics). The occurrence of PMQR genes was as follows: qnrS (52.4%), qnrA and aac(6′)-Ib-cr (33.3%), and qnrB (19.0%). The prevalence in species was as follows: 61.5% and 37.5% (qnrS), 19.2% and 56.3% (qnrA), 38.5% and 25.0 (aac(6′)-Ib-cr), and 19.2% and 18.8% (qnrB) for S. sonnei and S. flexneri, respectively. The other PMQR genes were not detected. In total, 52.8% (28/53) of quinolone-susceptible and 64.3% (27/42) of quinolone-resistant isolates were biofilm producers. Biofilm formation was not significantly different between quinolone-resistant and quinolone-susceptible isolates (P-value = 0.299). Quinolone-resistant isolates showed a high genetic diversity according to the ERIC-PCR.
Conclusion
It seems that qnrS, qnrA, and aac(6′)-Ib-cr play a significant role in the quinolone resistance among Shigella isolates in our region. Also the quinolone-resistant S. flexneri and S. sonnei isolates had a high genetic diversity. Hence, antibiotic therapy needs to be routinely revised based on the surveillance findings.
Similar content being viewed by others
Introduction
Apart from shigellosis, Shigella species are the pioneer cause of the bacillary dysentery in human. Shigella-associated diarrhea in children remains an important global human health problem, especially in developing countries [1]. It is estimated that 13.2% of all diarrhea-related mortality in the world are caused by Shigella species, making them the second most common cause of these deaths [1, 2]. Shigella is a member of the Enterobacterales family, and generally, four Shigella species, including Shigella sonnei, Shigella boydii, Shigella dysenteriae, and Shigella flexneri are responsible for shigellosis or milder forms of diarrheal disease [3]. Among them, S. sonnei is the most reported and sometimes dominant species in developed countries that causes mild, watery, or bloody diarrhea. While in low- and middle-income nations, S. flexneri is the major species that causes epidemic and endemic shigellosis. Likewise, the other two species (S. boydii and S. dysenteriae) are relatively rare [2, 4].
Fluoroquinolones belong to a family of synthetic broad-spectrum antibiotics. In addition to being effective antibiotics against multidrug-resistant bacteria, they are also among the most prescribed antibiotics for treating patients with shigellosis [4, 5]. Thus, quinolone-resistant Shigella species received a high rank among the global priority list of antibiotic-resistant bacteria published by the World Health Organization (WHO) [2, 3]. In recent years, fluoroquinolone-resistant Shigella species have emerged in many parts of the globe, particularly in Asia due to excessive use of these antibiotics [6].
Based on the available evidence, the resistance to fluoroquinolones in bacteria, including Shigella species, occurs mainly by point mutations in chromosomal genes encoding DNA gyrase (gyrA and gyrB) and topoisomerase IV (parC and parE) located in quinolone resistance-determining regions (QRDRs) [3, 5,6,7]. However, the plasmid-mediated quinolone resistance (PMQR) genes are also involved in this process through four main mechanisms, including the aminoglycoside acetyltransferase-encoding enzyme variant aac(6’)-lb-cr, qnr genes, efflux-pump-encoding qepA and oqxAB genes, and a recently detected phosphorylase gene (crpP) [3, 5, 8]. The aac(6’)-lb-cr gene codes a variant of the aminoglycoside acetyltransferase that acetylates aminoglycosides such as amikacin and kanamycin and fluoroquinolones such as ciprofloxacin and norfloxacin [9]. Currently, seven types of qnr genes have been demonstrated to be transferrable by plasmids, namely qnrA, qnrB, qnrC, qnrD, qnrE, qnrS, and qnrVC [10]. A different qnr protein belonging to the pentapeptide repeat protein (PRP) family is encoded by each gene that alters the target of quinolones [11]. A 56-kb conjugative plasmid, pOLA52, encodes oqxAB efflux pump via oqxA and oqxB genes, which confers resistance to several compounds, including fluoroquinolone antibiotics [12]. The quinolone efflux pump A (qepA) gene was first described in an Escherichia coli isolate from a urine specimen in 2007 [13]. This gene encodes a protein of 511 amino acids that significantly reduces the susceptibility to quinolones [12]. ATP-dependent phosphorylation of ciprofloxacin by CrpP enzyme that encoded by crpP gene, leads to a reduction in ciprofloxacin susceptibility. The crpP gene have mostly been identified in Pseudomonas aeruginosa, with lesser frequency reported in E. coli, Acinetobacter baumannii, and Klebsiella pneumoniae [8].
Also, a substantial amount of research has focused on the association between antibiotic resistance and biofilm production in bacteria. However, researchers are still attempting to define the association among creation of biofilms and resistance to antibiotics, as there are inconsistent results among different bacteria species [14]. Moreover, few studies have investigated the association between the formation of biofilms in Shigella isolates and quinolone resistance.
Consequently, the purpose of this study was to examine the frequency of PMQR genes and biofilm development in various species of clinical quinolone-resistant Shigella isolates. Also, the enterobacterial repetitive intergenic consensus polymerase chain reaction (ERIC-PCR) technique was used to examine the clonal relatedness of quinolone-resistant isolates.
Materials and methods
Ethics statement
Ethics approval was obtained from the University of Babylon, Hilla, Iraq (Project No: M220601) compliant with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations of the University of Babylon, Hilla, Iraq. Written consent was obtained from parents or guardians of all participants.
Study design and sample collection
In this cross-sectional study, stool samples were collected from 150 pediatric patients (younger than 10 years) with diarrhea referred to the private hospitals and treatment centers from November 2020 to December 2021. Exclusionary criteria were antibiotic use within 72 h of sample collection and being over 10 years in age, while inclusion criteria included any manifestation of fever, abdominal pain, cramps, vomiting or diarrhea. Sterile plastic containers were used to collect stool samples, which were immediately transferred to the microbiology laboratory for analysis.
Bacterial isolation and identification
A portion of all samples were inoculated on Hektoen Enteric (HE) Agar and Xylose Lysine Desoxycholate (XLD) Agar (Condalab, Madrid, Spain) and incubated at 37 ºC for 24 h. Also, a small percentage of specimens were enriched in 5 ml of Gram-negative (GN) broth (Condalab, Madrid, Spain) for six hours at 37 °C. The enriched specimens were sub-cultured on HE and XLD plates and placed at 37 ºC for 24 h [4]. The isolates that appeared green and red on HE and XLD, respectively, were considered presumptive Shigella isolates and identified using standard biochemical tests, including sulfide indole motility (SIM), citrate and urea hydrolysis, methyl red (MR) and Voges–Proskauer (VP), Kligler Iron Agar (KIA), and Lysine Iron Agar (LIA) [15]. Shigella isolates were confirmed by the VITEK 2 Compact system (bioMérieux, Marcy l’Étoile, France) according to the manufacturer protocol [16]. All isolates were further confirmed by polymerase chain reaction (PCR) of putative integrase as a specific marker for Shigella genus using previously described primers (Bioneer, South Korea) (Table 1) [17]. The QIAamp DNA Minikit (Qiagen GmbH, Hilden, Germany) was used for DNA extraction from Shigella isolates following the manufacturer instructions. PCR reaction (25 μL) was performed with the following program: 95 °C for 5 min, 35 cycles of 95 °C for 40 s, 60 °C for 30 s, 72°C for 30 s, and final extension at 72 °C for 5 min. The PCR products (5 μL) were loaded into 1% agarose gel and placed in 1X tris–acetate-EDTA (TAE) buffer contained ethidium bromide (0.5 μg/mL). The electrophoresis was performed for 45 min and amplicons were analyzed in a Bio-Rad gel documentation system (USA). In all experiments, S. sonnei ATCC® 25,931™ and S. flexneri ATCC® 29,903™ were used as quality control.
Antimicrobial susceptibility testing (AST)
The minimal inhibitory concentrations (MICs) of ciprofloxacin (32–0.03125 μg/mL), levofloxacin (32–0.03125 μg/mL), gatifloxacin (64–0.0625 μg/mL), ofloxacin (64–0.0625 μg/mL), imipenem (64–0.0625 μg/mL), meropenem (64–0.0625 μg/mL), ampicillin (512–0.05 μg/mL), amoxicillin/clavulanic acid (512–0.05 μg/mL), azithromycin (512–0.05 μg/mL), cefotaxime (64–0.0625 μg/mL), ceftriaxone (64–0.0625 μg/mL), ceftazidime (256–0.025 μg/mL), tetracycline (256–0.025 μg/mL), chloramphenicol (512–0.05 μg/mL), trimethoprim/sulfamethoxazole (64–0.0625 μg/mL), and cefepime (256–0.025 μg/mL) (Sigma-Aldrich, Darmstadt, Germany) were determined by broth microdilution method according to the Clinical Laboratory Standard Institute (CLSI) 2021 principles [18]. The Mueller–Hinton broth (Merck, Darmstadt, Germany) was used for AST. The breakpoints for resistance or susceptibility to each antibiotic were determined according to the CLSI 2021 criteria [18]. Multidrug-resistant (MDR) isolates were defined as those resistant to three or more antibiotics belong to different category [14]. Escherichia coli ATCC® 25,922™ was used as the control strain.
PMQR genes detection by PCR method
Uniplex PCR method was used to detect 11 PMQR genes in quinolone-resistant isolates using previously described primers (Bioneer, South Korea) as follows: qnrA, qnrB, qnrC, qnrD, qnrE, qnrS, qnrVC, aac(6′)-Ib-cr, qepA, oqxAB, and crpP [19,20,21,22]. The PCR reaction (25 μL) was performed in a Bio-Rad thermocycler (USA) with the following temperatures: 95 °C for 5 min, 35 cycles of 95 °C for 30 s, annealing (Table 1) for 30 s, 72°C for 30 s, and final extension at 72 °C for 5 min. The electrophoresis and visualization of the PCR products were performed similar to the previous stage.
Biofilm formation
A 96-well microtiter plate was used to assess the biofilm formation of quinolone-resistant and quinolone-susceptible isolates based on the previously described method with minor modifications [14]. The isolates were cultivated overnight in tryptic soy broth (Condalab, Madrid, Spain) and then were adjusted to a 0.5 McFarland standard turbidity. A total of 150 μL of these suspensions was dispensed in microtiter plate wells and incubated overnight at 37 °C. An initial three washes with phosphate-buffered saline (PBS) were done, followed by 20 min of fixation with methanol and 15 min of staining with 0.1% (v/v) crystal violet solution. Biofilm formation was measured at 550 nm optical density (OD550) using a microtiter plate reader (Thermo Fisher Scientific, USA). The isolates were categorized into four groups: non-biofilm (OD ≤ ODc), low-biofilm (ODc < OD ≤ 2 ODc), medium-biofilm (2 ODc < OD ≤ 4 ODc), and strong-biofilm (OD > 4 ODc) [14].
Clonal association by ERIC-PCR
The clonal association of quinolone-resistant isolates were investigated by ERIC-PCR. ERIC-PCR was performed in 25 μL volume using following program: 95 °C (15 min), 35 cycles [95 °C (30 s), 40 °C (45 s), and 72 °C (6 min)], and a final extension at 72 °C (10 min). The ERIC-PCR primers are shown in Table 1 [23]. Using a standard 1-kb DNA ladder (Fermentas, USA) as a reference, the ERIC-PCR patterns were evaluated by comparing positions of band lanes in each agarose gel (2%). To analyze the ERIC-PCR patterns, dendrograms were generated based on unweighted pair group method with arithmetic mean (UPGMA) and the Dice similarity coefficient using GelJ version 2.0 software [23, 24]. Shigella isolates with 90.0% or more similarity were considered to be clonally related.
Statistical analysis
Descriptive statistical analysis (frequency and prevalence of antibiotic resistance rates and PMQR genes) were performed using Statistical Package for the Social Sciences (SPSS) version 20.0 (SPSS Inc., Chicago, IL, USA). Fisher's exact test or Chi-square test were used to determine any significant correlations (P-value < 0.05) between variables.
Results
Shigella isolates
During the study period, a total of 95 presumptive Shigella isolates were collected and primarily identified using standard phenotypic and biochemical tests. Using VITEK 2 Compact system, the Shigella isolates were confirmed on species level in the following order: S. sonnei (53, 55.8%), S. flexneri (39, 41.1%), and S. boydii (3, 3.2%). No S. dysenteriae isolate was detected. All identified isolates showed the 159 bp specific band of putative integrase of Shigella genus in PCR assay. Shigella isolates were mostly retrieved from male patients (59, 62.1%) including 31 (52.5%) S. sonnei, 25 (42.4%) S. flexneri, and 3 (5.1%) S. boydii. The remaining were collected from females (36, 37.9%). There was no significant differences between the prevalence of Shigella species and gender of patients (P-value = 0.334). Also, most of the isolates were identified in pediatric patients aged from 4–6 years old (42, 44.2%), followed by 2–4 years old (28, 29.5%), 6–8 years old (13, 13.7%), < 2 years old (9, 9.5%), and 8–10 years old (3, 3.2%).
Antibiotic resistance rates
The AST revealed that 98.9% (n = 94/95) and 97.9% (n = 93/95) of Shigella isolates were susceptible to imipenem and meropenem, respectively (Table 2). S. sonnei, S. boydii, and S. flexneri showed the susceptibility rates of 100.0% (n = 53/53), 100.0% (n = 3/3), and 97.4% (n = 38/39) towards imipenem, respectively. The highest resistance rates of the Shigella isolates were against ampicillin (92.6%, n = 88/95), followed by amoxicillin/clavulanic acid (85.3%, n = 81/95), trimethoprim/sulfamethoxazole (76.8%, n = 73/95), ceftriaxone (56.8%, n = 54/95), and cefotaxime (50.5%, n = 48/95). All three species S. boydii (100.0%, n = 3/3), S. sonnei (90.6%, n = 48/53), and S. flexneri (94.9%, n = 37/39) were highly resistant to ampicillin, with no significant difference (P > 0.05). In total, 42 of 95 (44.2%) Shigella isolates were quinolone-resistant including 26 (61.9%) S. sonnei and 16 (38.1%) S. flexneri. No S. boydii isolate was quinolone-resistant. All 42 quinolone-resistant isolates were simultaneously resistant against two or more quinolones (Table 2). The highest co-resistance rate was observed against levofloxacin–ofloxacin (23.8%, n = 10/42), followed by ciprofloxacin–levofloxacin (21.4%, n = 9/42). The highest resistance rate was against ciprofloxacin (31.6%, n = 30/95) followed by ofloxacin (28.4%, n = 27/95), levofloxacin (26.3%, n = 25/95), and gatifloxacin (15.8%, n = 15/95), respectively. All isolates including 42 quinolone-resistant strains were MDR.
Prevalence of PMQR genes
In total, the PMQR genes were detected in 92.9% (39/42) of quinolone-resistant Shigella isolates including all quinolone-resistant S. flexneri (100.0%, n = 16/16) and 88.5% (n = 23/26) of quinolone-resistant S. sonnei. Four different PMQR genes were found to be associated with both quinolone-resistant S. sonnei and S. flexneri isolates in this study (Table 3, Fig. 1, Fig. 2, and Fig. 3). The occurrence of these genes in their descending order of positivity was as follows: qnrS (52.4%) > qnrA and aac(6′)-Ib-cr (33.3%) > qnrB (19.0%). The prevalence of different genes in Shigella species was as follows: 61.5% and 37.5% (qnrS), 19.2% and 56.3% (qnrA), 38.5% and 25.0 (aac(6′)-Ib-cr), and 19.2% and 18.8% (qnrB) for S. sonnei and S. flexneri, respectively. The co-incidence of PMQR determinants was detected in 40.5% (17/42) of quinolone-resistant isolates (Table 3). Statistically, there was no significant difference (P > 0.05) in the prevalence of the four PMQR genes in both Shigella species. The qnrC, qnrD, qnrE, qnrVC, qepA, oqxAB, and crpP genes were not detected in any isolate.
Gel electrophoresis of qnrB (488 bp) and aac(6’)-lb-cr (260 bp). Lane 1: DNA ladder (100 bp); Lane 2: Positive control of qnrB gene; Lanes 3: qnrS-positive Shigella sonnei isolate; Lane 4: Negative control: DNA/RNA free water; Lane 5: Positive control of aac(6’)-lb-cr gene; Lanes 6–8: aac(6’)-lb-cr-positive Shigella flexneri isolates; Lanes 9–11: aac(6’)-lb-cr-positive Shigella sonnei isolates; Lanes 12 and 13: aac(6’)-lb-cr-negative Shigella flexneri isolates
Gel electrophoresis of qnrA gene (630 bp). Lane 1 and 12: DNA ladder (100 bp); Lane 2: Negative control: DNA/RNA free water; Lanes 3: Positive control of qnrA gene; Lanes 4–6: qnrA-positive Shigella sonnei isolates; Lanes 7, 8, 9, and 11: qnrA-positive Shigella flexneri isolates; Line 10: qnrA-negative Shigella flexneri isolates
Biofilm formation
In total, 52.8% (28/53) of quinolone-susceptible isolates including 55.6% (15/27) of S. sonnei, 43.5% (10/23) of S. flexneri, and 100.0% (3/3) of S. boydii were low-biofilm producers. None of the quinolone-susceptible isolates were strong-biofilm producers or medium-biofilm producers. However, 64.3% (27/42) of quinolone-resistant isolates showed the biofilm formation phenomenon including 28.6% (12/42) strong-biofilm producers, 23.8% (10/42) medium-biofilm producers, and 11.9% (5/42) low-biofilm producers. Also, 15 isolates (35.7%, 15/42) were non-biofilm producers. In terms of Shigella species, 30.8% (8/26), 23.1% (6/26), 11.5% (3/26), and 34.6% (9/26) of quinolone-resistant S. sonnei were strong-biofilm producers, medium-biofilm producers, low-biofilm producers, and non-biofilm producers, respectively. Meanwhile, 25.0% (4/16), 25.0% (4/16), 12.5% (2/16), and 37.5% (6/16) of quinolone-resistant S. flexneri were strong-biofilm producers, medium-biofilm producers, low-biofilm producers, and non-biofilm producers, respectively. Biofilm formation was not significantly different between quinolone-resistant S. sonnei and quinolone-resistant S. flexneri isolates (P-value > 0.999). Moreover, the biofilm formation was not significantly different between quinolone-resistant and quinolone-susceptible Shigella isolates (P-value = 0.299).
Clonal association
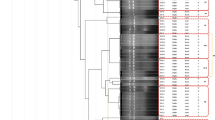
Based on the ERIC-PCR, 16 quinolone-resistant S. flexneri isolates were distributed to 4 clusters (A to D) including 2 to 3 isolates and 6 singletons with 12 various ERIC-types (E1 to E12), indicating a high genetic diversity among the isolates (Fig. 4). The ERIC-PCR patterns included 3 to 8 bands with various sizes ranging from 100 to 1000 bp for each isolate. Also, the 26 quinolone-resistant S. sonnei isolates were distributed to 3 clusters (A to C) including 2 to 3 isolates and 19 singletons with 24 various ERIC-types (E1 to E24), showing a high genetic diversity among the isolates (Fig. 5). The ERIC-PCR patterns included 3 to 9 bands with various sizes that ranged from 100 to 1300 bp for each isolate.
Discussion
In this study, S. sonnei (58.0%) was the most common cause of the shigellosis followed by S. flexneri (41.1%) and S. boydii (3.2%). In contrast to this study, previous reports suggested S. flexneri as the leading species of shigellosis in developing countries [25, 26]. However, most developing countries, including those in Southeast Asia, are recording a shift in the major etiological agent of shigellosis to S. sonnei [27]. In line with the current study, Teimourpour et al. [28] from Iran, reported S. sonnei (69.9%) as the most predominant species followed by S. flexneri (19.4%) and S. boydii (9.9%). On the other hand, the absence of S. dysenteriae in this study was not surprising, as the isolation of these species is relatively rare when compared to the other three species [4, 6]. Yu et al. [3] from China, also corroborated this result by recording a complete absence of S. dysenteriae in a study involving 118 Shigella isolates. These discrepancies may be due to the differences in the sample size, the race of studies population, and the hygiene situation of studied region.
Shigella infections are distributed differently based on age and gender worldwide. This study revealed the most incidence rate of Shigella isolates in males and in pediatric patients aged from 4–6 years old. In line with the current observations, Abbasi et al. [4] from Iran, Liu et al. [15] from China, and Jain et al. [25] from India reported a higher frequency rate of Shigella isolates in males than that of females. The descriptive epidemiology identified varying rates of shigellosis cases among males and females. Nevertheless, there is a lack of comprehensive explanations on the factors contributing to this disparity and the methods of transmission [29]. One of the reasons for this difference may be women's better personal hygiene habits [26, 29]. Moreover, males are more likely to be exposed to the environments contaminated with Shigella species [15]. Previous studies reported a more prevalence rate of Shigella infections in pediatric patients under 5 years which was consistent with our findings [15, 30]. Due to their low immunity and lack of prior exposure, children under five are more susceptible to shigellosis than older children [15].
Shigella species isolated in this study displayed a wide spectrum of antibiotic resistance. The highest resistance rates were found to ampicillin (92.6%), amoxicillin/clavulanic acid (85.3%), and trimethoprim/sulfamethoxazole (76.8%). S. boydii completely resisted ampicillin, amoxicillin/clavulanic acid, cefotaxime, and trimethoprim/sulfamethoxazole with a rate of 100.0%. Despite having a low prevalence of isolation, S. boydii could pose a serious health concern. Similar results were previously reported by Abbasi et al. [4], Zamanlo et al. [31] and Farahani et al. [32] from neighboring geographical area, Liu et al. [16] from China, and Phiri et al. [26] from Malawi. In another study carried out in Kenya by Leting et al. [33], the Shigella isolates displayed almost similar resistance rate against ampicillin (100.0%) and amoxicillin/clavulanic acid (84.2%). This implied that these group of antibiotics are no more suitable for the treatment of shigellosis. This could have resulted due to the extensive usage of these antibiotics, especially in the treatment of diarrhea leading to high degrees of resistance. According to Behruznia et al. [34], Shigella species have become resistant to first-line drugs (trimethoprim–sulfamethoxazole and ampicillin), so that they are no longer recommended for the treatment of shigellosis. The increase in resistance by Shigella species calls for concerns as the United Kingdom, Northern Ireland, and numerous other nations have all reported cases of extensively drug-resistant (XDR) Shigella sonnei [35]. Besides, our findings revealed that almost 50.0% of Shigella isolates were resistant to third generation cephalosporins that was in line with the previous reports from Iran [4, 31]. However, in contrast to our findings, Madhavan et al. [30] from India and Liu et al. [36] from China reported lower resistance rates for these antibiotics. The high resistance rate to third generation cephalosporins in this study may be due to the emergence of extended-spectrum beta-lactamases (ESBLs)-producing Shigella isolates [37,38,39]. In recent years, there have been reports of the emergence of Shigella strains carrying ESBL genes from some parts of the world including China, Iran, and England [37,38,39].
In this study, the focus was on quinolone-resistant strains. In total, 44.2% of Shigella isolates were simultaneously resistant against two or more quinolones including 61.9% S. sonnei and 38.1% S. flexneri. This resistance rate was much higher than a previous report from neighboring country Iran in which only 4.4% of isolates were quinolone-resistant [28]. Also, in this study, the most resistance rate among quinolones was related to ciprofloxacin (31.6%) that was in line with a previous report from China [6]. Due to the widespread use of fluoroquinolones as first-line antibiotics to treat diarrhea in recent years, quinolone resistance has increased considerably. A lack of local antimicrobial resistance surveillance, easy access to antibiotics, and inappropriate prescription of antibiotics in our region may all be contributing factors to the situation's deterioration. However, the high quinolone-resistant rate for S. sonnei in this study was in good parallel with a previous report that showed 76% (313/411) of S. sonnei isolates collected from several countries were quinolone-resistant [40]. A previous study from India has also reported quinolone-resistant S. sonnei brought on by a combination of qnrB and gyrA mutations [41]. Based on the available evidence, men who have sex with men (MSM) in Taiwan are frequently infected with quinolone-resistant S. sonnei that has the same QRDR mutations [42].
The PMQR determinants have escalated into a serious global issue over the past few years [6]. To the best of our knowledge, this study was the first to investigate 11 different PMQR genes in quinolone-resistant Shigella isolates. The qnrS (52.4%) was the most frequent PMQR gene followed by qnrA and aac(6′)-Ib-cr (33.3%), and qnrB (19.0%). The qnrC, qnrD, qnrE, qnrVC, qepA, oqxAB, and crpP genes were not detected in any isolate. In a previous study from India [41], 18.7% of S. sonnei isolates harbored qnrC gene and no isolate was positive for qepA, qnrS, and qnrA. In another study from Iran, qnrC and qnrD genes were not detected in any Shigella isolates [43]. Also, in a previous research from China [44], qnrA, qnrC, qnrD and qepA genes were not found in S. flexneri isolates. However, Yang et al. [45] from China, reported the qepA gene in 2.05% of Shigella isolates. Moreover, based on the available evidence, there is no report of the presence of qnrE, qnrVC, and crpP genes in Shigella isolates from different countries.
Statistically, there was no significant difference in the prevalence of the four PMQR genes between S. sonnei and S. flexneri species. In a previous study from China, aac (6′)-Ib-cr was the most frequent gene found in quinolone-resistant Shigella isolates [46]. The frequency of selecting chromosomal mutants to decrease ciprofloxacin activity by N-acetylation of its piperazinyl substituent has been shown to be significantly increased by aac (6′)-Ib-cr [46]. In this study, qnrA was detected in 19.2% and 56.3% of S. sonnei and S. flexneri isolates, respectively. However, in a previous studies from China [44, 46], the Shigella isolates were negative for this gene. Based on evidence, China had a majority prevalence of qnrS in S. sonnei and S. flexneri, while India had a majority prevalence of qnrB [47]. Also, similar to this study, qepA gene was not detected in S. sonnei isolates from China [48]. In a previous study from India, the qnrS1 was detected in 47% of S. boydii isolate and no S. sonnei was positive for qnr genes that was in contrast to this study [49].
In this study, 52.8% of quinolone-susceptible and 64.3% of quinolone-resistant isolates were biofilm producers and the biofilm formation rates of resistant and susceptible isolates were not significantly different. In line with this study, no association was found between the biofilm formation and antibiotic resistance in Pseudomonas aeruginosa and Acinetobacter baumannii isolates in previous studies [50, 51]. However, several investigations have shown the positive correlation between biofilm production and antibiotic resistance [52, 53]. Despite extensive research, Shigella species have not been thoroughly characterized in terms of association of their biofilm formation with antimicrobial resistance. Hence, further studies are needed to reveal the molecular mechanisms involved in these processes.
Based on the ERIC-PCR, quinolone-resistant S. flexneri and S. sonnei isolates had a high genetic diversity. This incredibly complex pattern makes it possible that various strains of the same species circulate in our region. These results were in good parallel with the previous reports from Malawi [26], Peru [54], and Latin America [55]. To prove that the Shigella strains in this study were genetically unrelated, additional research utilizing more exact typing techniques, such as whole-genome sequencing (WGS) and multi-locus sequence typing (MLST), would be required [26]. This study had some limitations as the other quinolone resistance mechanisms (mutations in QRDRs) were not investigated.
Conclusion
This study demonstrated the predominance of S. sonnei and S. flexneri in our region. The Shigella isolates showed high resistance to ampicillin, amoxicillin/clavulanic acid, and trimethoprim/sulfamethoxazole and all isolates were MDR. It seems that qnrS, qnrA, and aac(6′)-Ib-cr play significant role in the quinolone resistance among Shigella isolates in our region. There was no statistical association between biofilm formation and quinolone resistance. Also the quinolone-resistant S. flexneri and S. sonnei isolates had a high genetic diversity. Hence, antibiotic therapy needs to be routinely monitored based on the surveillance programs.
Availability of data and materials
The datasets in the present study are accessible from the corresponding author, Saki M.
Abbreviations
- ERIC-PCR:
-
Enterobacterial repetitive intergenic consensus polymerase chain reaction
- MIC:
-
Minimal inhibitory concentration
- MLST:
-
Multi-locus sequence typing
- PMQR:
-
Plasmid-mediated quinolone resistance
- QRDRs:
-
Quinolone resistance-determining regions
- WGS:
-
Whole-genome sequencing
References
Duchen D, Haque R, Chen L, Wojcik G, Korpe P, Nayak U, et al. Host genome-wide association study of infant susceptibility to Shigella-associated diarrhea. Infect Immun. 2021;89(6):e00012-21.
Bengtsson RJ, Simpkin AJ, Pulford CV, Low R, Rasko DA, Rigden DJ, Hall N, Barry EM, Tennant SM, Baker KS. Pathogenomic analyses of Shigella isolates inform factors limiting shigellosis prevention and control across LMICs. Nat Microbiol. 2022;7(2):251–61.
Yu X, Zhang D, Song Q. Profiles of gyrA mutations and plasmid-mediated quinolone resistance genes in Shigella isolates with different levels of fluoroquinolone susceptibility. Infect Drug Resist. 2020;13:2285–90.
Abbasi E, Abtahi H, van Belkum A, Ghaznavi-Rad E. Multidrug-resistant Shigella infection in pediatric patients with diarrhea from central Iran. Infect Drug Resist. 2019;12:1535–44.
Bush NG, Diez-Santos I, Abbott LR, Maxwell A. Quinolones: mechanism, lethality and their contributions to antibiotic resistance. Molecules. 2020;25(23):5662.
Zhang WX, Chen HY, Tu LH, Xi MF, Chen M, Zhang J. Fluoroquinolone resistance mechanisms in Shigella isolates in Shanghai, China, between 2010 and 2015. Microb Drug Resist. 2019;25(2):212–8.
Li J, Wei Y, Wang J, Li Y, Shao G, Feng Z, et al. Characterization of mutations in DNA gyrase and topoisomerase IV in field strains and in vitro selected quinolone-resistant Mycoplasma hyorhinis mutants. Antibiotics. 2022;11(4):494.
Zhu Z, Yang H, Yin Z, Jing Y, Zhao Y, Fu H, et al. Diversification and prevalence of the quinolone resistance crpP genes and the crpP-carrying Tn6786-related integrative and conjugative elements in Pseudomonas aeruginosa. Virulence. 2021;12(1):2162–70.
Kareem SM, Al-Kadmy IM, Kazaal SS, Ali AN, Aziz SN, Makharita RR, et al. Detection of gyrA and parC mutations and prevalence of plasmid-mediated quinolone resistance genes in Klebsiella pneumoniae. Infect Drug Resist. 2021;14:555–63.
Wang C, Yin M, Zhang X, Guo Q, Wang M. Identification of qnrE3 and qnrE4, new transferable quinolone resistance qnrE family genes originating from Enterobacter mori and Enterobacter asburiae, respectively. Antimicrob Agents Chemother. 2021;65(8):e00456-e521.
Salah FD, Soubeiga ST, Ouattara AK, Sadji AY, Metuor-Dabire A, Obiri-Yeboah D, et al. Distribution of quinolone resistance gene (qnr) in ESBL-producing Escherichia coli and Klebsiella spp. in Lomé Togo. Antimicrob Resist Infect Control. 2019. https://doi.org/10.1186/s13756-019-0552-0.
Cayci YT, Korkmaz F, Biyik I, Bilgin K, Birinci A. Investigation of oqxAB and qepA the quinolone resistance determinants in carbapenem resistant Enterobactericeae isolates. Acta Med Mediterr. 2020;36(6):3409–13.
Yamane K, Wachino J, Suzuki S, Kimura K, Shibata N, Kato H, et al. New plasmid-mediated fluoroquinolone efflux pump, QepA, found in an Escherichia coli clinical isolate. Antimicrob Agents Chemother. 2007;51(9):3354–60.
Qian W, Li X, Yang M, Liu C, Kong Y, Li Y, et al. Relationship between antibiotic resistance, biofilm formation, and biofilm-specific resistance in Escherichia coli isolates from Ningbo. China Infect Drug Resist. 2022;15:2865–78.
Mahon CR, Lehman DC. Textbook of Diagnostic Microbiology. St. Louis, Missouri: Elsevier Saunders; 6th ed, 2018.
Liu Y, Shen W, Sun Y, Lv N, Sun K, Hu L, et al. Virulence-related gene distribution among Shigella isolates in Anhui, China: The association with antimicrobial resistance. Infect Drug Resist. 2020;13:3637–47.
Kim HJ, Ryu JO, Song JY, Kim HY. Multiplex polymerase chain reaction for identification of Shigellae and four Shigella species using novel genetic markers screened by comparative genomics. Foodborne Pathog Dis. 2017;14(7):400–6.
Clinical and Laboratory Standards Institute, Performance Standards for Antimicrobial Susceptibility Testing. 31et ed. CLSI supplement M100-S31, Wayne, PA: Clinical and Laboratory Standards Institute; 2021.
Amin MB, Saha SR, Islam MR, Haider SA, Hossain MI, Chowdhury AH, et al. High prevalence of plasmid-mediated quinolone resistance (PMQR) among E. coli from aquatic environments in Bangladesh. Plos One. 2021;16(12):e0261970.
Lin J, Chen DQ, Hong J, Huang H, Xu X. Prevalence of qnrVC genes in Pseudomonas aeruginosa clinical isolates from Guangdong. China Curr Microbiol. 2020;77(8):1532–9.
Papa-Ezdra R, Caiata L, Palacio R, Outeda M, Cabezas L, Bálsamo A, et al. Prevalence and molecular characterization of carbapenemase-producing Enterobacterales in an outbreak-free setting in a single hospital in Uruguay. J Glob Antimicrob Resist. 2021;24:58–62.
Chávez-Jacobo VM, Hernández-Ramírez KC, Silva-Sánchez J, Garza-Ramos U, Barrios-Camacho H, Ortiz-Alvarado R, et al. Prevalence of the crpP gene conferring decreased ciprofloxacin susceptibility in enterobacterial clinical isolates from Mexican hospitals. J Antimicrob Chemother. 2019;74(5):1253–9.
Codjoe FS, Brown CA, Smith TJ, Miller K, Donkor ES. Genetic relatedness in carbapenem-resistant isolates from clinical specimens in Ghana using ERIC-PCR technique. PLoS ONE. 2019;14(9): e0222168.
Heras J, Domínguez C, Mata E, Pascual V, Lozano C, Torres C, et al. GelJ–a tool for analyzing DNA fingerprint gel images. BMC Bioinform. 2015;16:270.
Jain PA, Kulkarni RD, Dutta S, Ganavali AS, Kalabhavi AS, Shetty PC, et al. Prevalence and antimicrobial profile of Shigella isolates in a tertiary care hospital of North Karnataka: a 12-year study. Indian J Med Microbiol. 2020;38(1):101–8.
Phiri AF, Abia AL, Amoako DG, Mkakosya R, Sundsfjord A, Essack SY, et al. Burden, antibiotic resistance, and clonality of Shigella spp. implicated in community-acquired acute diarrhoea in Lilongwe Malawi. Trop Med Infect Dis. 2021;6(2):63.
Chung The H, Bodhidatta L, Pham DT, Mason CJ, Ha Thanh T, Voong Vinh P, et al. Evolutionary histories and antimicrobial resistance in Shigella flexneri and Shigella sonnei in Southeast Asia. Commun Biol. 2021;4:353.
Teimourpour R, Babapour B, Esmaelizad M, Arzanlou M, Peeri-Doghaheh H. Molecular characterization of quinolone resistant Shigella spp. isolates from patients in Ardabil. Iran Iran J Microbiol. 2019;11(6):496–501.
Zhao ZY, Chen Q, Zhao B, Hannah MN, Wang N, Wang YX, et al. Relative transmissibility of shigellosis among male and female individuals: a modeling study in Hubei Province, China. Infect Dis Poverty. 2020;9(1):39.
Madhavan A, Balakrishnan S, Vasudevapanicker J. Antibiotic susceptibility pattern of Shigella isolates in a tertiary healthcare center. J Lab Physicians. 2018;10:140–4.
Zamanlou S, Rezaee MA, Aghazadeh M, Ghotaslou R, Nave HH, Khalili Y. Genotypic diversity of multidrug resistant Shigella species from Iran. Infect Chemother. 2018;50(1):29–37.
Farahani NN, Jazi FM, Nikmanesh B, Asadolahi P, Kalani BS, Amirmozafari N. Prevalence and antibiotic susceptibility patterns of Salmonella and Shigella species isolated from pediatric diarrhea in Tehran. Arch Pediatr Infect Dis. 2018;6(4): e57328.
Leting SK, Musyoki SK, Maiyoh GK. Characterization and drug susceptibility pattern of Salmonella and Shigella in children below five years: a cross-sectional study conducted in Lodwar, Turkana County, in Northern Kenya. Pan Afr Med J. 2022;9(42):13.
Behruznia P, Sadredinamin M, Hashemi A, Hajikhani B, Nojookambari NY, Behruznia M, et al. Decreased susceptibility of Shigella isolates to azithromycin in children in Tehran. Iran Can J Infect Dis Med Microbiol. 2022;2022:4503964.
World Health Organization. Disease Outbreak News; Extensively drug-resistant Shigella sonnei infections-Europe. at: https://www.who.int/emergencies/disease-outbreak-news/item/extensively-drug-resistant-shigella-sonnei-infections---europe.
Liu H, Zhu B, Qiu S, Xia Y, Liang B, Yang C, et al. Dominant serotype distribution and antimicrobial resistance profile of Shigella spp. in Xinjiang, China. PLoS One. 2018;13(4):e0195259.
Bian F, Yao M, Fu H, Yuan G, Wu S, Sun Y. Resistance characteristics of CTX-M type Shigella flexneri in China. Biosci Rep. 2019;39(9):BSR20191741.
Farajzadeh Sheikh A, Moradi Bandbal M, Saki M. Emergence of multidrug-resistant Shigella species harboring extended-spectrum beta-lactamase genes in pediatric patients with diarrhea from southwest of Iran. Mol Biol Rep. 2020;47(9):7097–106.
Charles H, Prochazka M, Thorley K, Crewdson A, Greig DR, Jenkins C, et al. Outbreak of sexually transmitted, extensively drug-resistant Shigella sonnei in the UK, 2021–22: a descriptive epidemiological study. Lancet Infect Dis. 2022;22(10):1503–10.
Chung The H, Boinett C, Pham Thanh D, Jenkins C, Weill FX, Howden BP, et al. Dissecting the molecular evolution of fluoroquinolone-resistant Shigella sonnei. Nat Commun. 2019;10(1):4828.
Das A, Natarajan M, Mandal J. The emergence of quinolone resistant Shigella sonnei, Pondicherry. India PLoS One. 2016;11: e0160290.
Chiou CS, Izumiya H, Kawamura M, Liao YS, Su YS, Wu HH, et al. The worldwide spread of ciprofloxacin-resistant Shigella sonnei among HIV-infected men who have sex with men. Taiwan Clin Microbiol Infect. 2016;22(4):383.e11-383.e16.
Jomehzadeh N, Ahmadi K, Ataee N, Afzali M. Molecular detection of genes encoding resistance to tetracycline and quinolones among Shigella strains isolated from children with acute diarrhea in southwest Iran. Iran J Microbiol. 2023;15(5):625.
Qin T, Qian H, Fan W, Ma P, Zhou L, Dong C, et al. Newest data on fluoroquinolone resistance mechanism of Shigella flexneri isolates in Jiangsu Province of China. Antimicrob Resist Infection Control. 2017;6:97.
Yang H, Duan G, Zhu J, Zhang W, Xi Y, Fan Q. Prevalence and characterisation of plasmid-mediated quinolone resistance and mutations in the gyrase and topoisomerase IV genes among Shigella isolates from Henan, China, between 2001 and 2008. Int J Antimicrob Agents. 2013;42(2):173–7.
Cao M, Wang W, Zhang L, Liu G, Zhou X, Li B, et al. Epidemic and molecular characterization of fluoroquinolone-resistant Shigella dysenteriae 1 isolates from calves with diarrhea. BMC Microbiol. 2021;21:6.
Zhu Z, Shi Y, Zhou X, Li B, Zhang J. Molecular characterization of fluoroquinolone and/or cephalosporin resistance in Shigella sonnei isolates from yaks. BMC Vet Res. 2018;14:177.
Qian HM, Qin TT, Liu GY, Li J, Ma P, Kong XX, et al. First report of the qnrA determinant in Shigella sonnei isolated from China. Epidemiol Infect. 2017;145(11):2193–6.
Sethuvel DP, Perumalla S, Anandan S, Michael JS, Ragupathi NK, Gajendran R, et al. Antimicrobial resistance, virulence & plasmid profiles among clinical isolates of Shigella serogroups. Indian J Med Res. 2019;149(2):247.
Gajdács M, Baráth Z, Kárpáti K, Szabó D, Usai D, Zanetti S, et al. No correlation between biofilm formation, virulence factors, and antibiotic resistance in Pseudomonas aeruginosa: Results from a laboratory-based in vitro study. Antibiotics (Basel). 2021;10(9):1134.
Donadu MG, Mazzarello V, Cappuccinelli P, Zanetti S, Madléna M, Nagy ÁL, et al. Relationship between the biofilm-forming capacity and antimicrobial resistance in clinical Acinetobacter baumannii isolates: results from a laboratory-based in vitro study. Microorganisms. 2021;9(11):2384.
Zhou X, Li M, Xu L, Shi C, Shi X. Characterization of antibiotic resistance genes, plasmids, biofilm formation, and in vitro invasion capacity of Salmonella enteritidis isolates from children with gastroenteritis. Microb Drug Resist. 2019;25(8):1191–8.
Fricks-Lima J, Hendrickson CM, Allgaier M, Zhuo H, Wiener-Kronish JP, Lynch SV, et al. Differences in biofilm formation and antimicrobial resistance of Pseudomonas aeruginosa isolated from airways of mechanically ventilated patients and cystic fibrosis patients. Int J Antimicrob Agents. 2011;37(4):309–15.
Lluque A, Mosquito S, Gomes C, Riveros M, Durand D, Tilley DH, et al. Virulence factors and mechanisms of antimicrobial resistance in Shigella strains from periurban areas of Lima (Peru). Int J Med Microbiol. 2015;305(4–5):480–90.
Sati HF, Bruinsma N, Galas M, Hsieh J, Sanhueza A, Ramon Pardo P, et al. Characterizing Shigella species distribution and antimicrobial susceptibility to ciprofloxacin and nalidixic acid in Latin America between 2000–2015. PLoS ONE. 2019;14(8): e0220445.
Acknowledgements
None.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NSKAK, BSAA, RMJE, and HOMAD: conceptualisation, data curation, formal analysis, investigation, methodology, project administration, writing—original draft preparation, writing— review and editing. SYA, AN, and DCN: data curation, formal analysis, writing-original draft preparation, writing—review and editing. MHGK, SSA, and MS: investigation, writing—review and editing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the University of Babylon, Hilla, Iraq (Project No: M220601) compliant with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations of the University of Babylon, Hilla, Iraq. Written consent was obtained from parents or guardians of all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Al-Khafaji, N.S.K., Almjalawi, B.S.A., Ewadh, R.M.J. et al. Prevalence of plasmid-mediated quinolone resistance genes and biofilm formation in different species of quinolone-resistant clinical Shigella isolates: a cross-sectional study. Eur J Med Res 29, 419 (2024). https://doi.org/10.1186/s40001-024-02007-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-02007-y