Abstract
Background
Extensive vaccination programs are being implemented worldwide for coronavirus disease 2019 (COVID-19). With the spread of vaccination, swelling of the lymph nodes after vaccination is frequently seen. We encountered a patient who developed left axillary lymphadenoma following vaccine administration.
Case presentation
The patient was a Japanese woman in her 80 s who had previously undergone surgery for right breast cancer. She received two injections of the Pfizer-BioNTech COVID-19 vaccine in her left arm. Approximately 3 months later, she complained of left axillary swelling, and imaging resulted in a diagnosis of left axillary lymphangioma. In accordance with the patient’s wishes, we performed axillary mass resection. The pathological diagnosis was lymphangioma.
Conclusion
Our examination findings indicated that congestion of the axillary lymph vessels might have been caused by upper-arm injections of the COVID-19 vaccine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Extensive vaccination programs are being implemented worldwide for coronavirus disease 2019 (COVID-19). According to the package insert for the Pfizer-BioNTech COVID-19 vaccine, the incidence of lymphadenitis as an adverse event is low [1]. However, unilateral axillary lymphadenopathy has been a common unsolicited adverse event after vaccination with either the Moderna or Pfizer-BioNTech COVID-19 vaccine [2]. Moreover, various organizations recommend that COVID-19 vaccination should be performed on the contralateral side of patients who have unilateral upper-arm edema or those who have undergone axillary surgery to prevent edema on the vaccinated side [3, 4]. Here, we report our experience with a Japanese patient who developed a left axillary lymphangioma following left upper-arm vaccination with a COVID-19 vaccine.
Case presentation
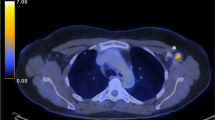
A Japanese woman in her 80 s received a second injection of the Pfizer-BioNTech COVID-19 vaccine in her left deltoid muscle in 2021. She had a history of right breast cancer (T1N0M0) and had undergone breast-conserving surgery and sentinel node biopsy in her 70 s. Postoperative follow-up examinations were continued, and no sign of recurrence, including in the left axial region, was observed until 2021. There was no evidence of trauma to the left axial region. Her early adverse reaction following vaccination was mild pain at the inoculation site on the day of vaccination and the following day. However, 3 months after the second vaccination, she noticed left axillary swelling and visited the outpatient department at the Tokushima Breast Care Clinic. No lymphedema was found on her upper arm, but an elastic-soft left axillary mass was detected, and breast ultrasonography (US) revealed a 6-cm cystic mass. Computed tomography (CT) revealed a cystic mass without any solid pattern near the normal lymph nodes, and a lymphangioma was suspected (Fig. 1a, b).
Non-enhanced magnetic resonance imaging (MRI) revealed a 6.2 × 3.4 × 7.4-cm mass having a clear boundary, smooth surface and nearly homogeneous internal pattern. Compared with the surrounding muscle, the mass had a low signal on T1-weighted imaging (Fig. 2a) and a high signal on T2-weighted imaging (Fig. 2b). Internally, there was no solid pattern or high signal intensity on diffusion-weighted imaging, and a benign cystic mass (lymphangioma or synovial cystitis) was suggested. US revealed a multilobulated cystic mass and branches from the mass connected to the axillary vein (Fig. 3). Finally, a left axillary lymphangioma was diagnosed, and we suggested follow-up with drainage or resection. However, she expressed a strong desire for surgical resection because of the severe axillary discomfort. She underwent tumorectomy for the left axillary mass under general anesthesia. The mass did not adhere to the surrounding tissue and could be smoothly resected. On the cut surface, the tumor was a thin-walled transparent cyst filled with clear, yellowish fluid (Fig. 4a). Pathologic examination showed a large cystic region and anastomosing vasculature (Fig. 4b), both of which were lined with small, bland-appearing endothelial cells that were positive for D2-40 on immunostaining (Fig. 4c, d). Normal lymph nodes were found near the tumor. These findings were consistent with those of lymphangioma. The patient was discharged on the 7th day after surgery. The postoperative course is good as of the most recent follow-up, and the outpatient follow-up continues.
Pathological findings. Resected specimen of the axilla cystic tumor (a). In the cystic region, the inner surface was lined with flattened endothelial cells (b; hematoxylin–eosin staining). The endothelial cells were positive for D2-40 by immunostaining and determined to be lymphatic vessels (c and d)
Discussion
Lymphangiomas are tumorous lesions composed primarily of lymphatic cysts that occur mainly in children (most are congenital). The congenital cause is thought to be obstruction of the lymph vessels during the fetal period [5]. On the other hand, on rare occasions, lymphangiomas also occur in adults due to the obstruction of lymph vessels because of some cause (i.e., inflammation, trauma, radiotherapy, a thrombus) that leads to lymphatic fluid retention. The head and neck are the most common site for cystic lymphangiomas. Ultrasonographic findings include unilocular or multilocular anechoic mass. CT findings show non-enhancing cystic lesions with homogenous attenuation; visceral and osseous lesions often show contrast enhancement. Surgical resection may be indicated for large, deep lesions, especially if symptomatic [6, 7]. Here, we report a case of lymphangioma in the left axial region following injection of the Pfizer-BioNTech COVID-19 vaccine to the left upper arm.
We let the patient choose between conservative treatment and tumor removal. At the patient’s request, surgery was performed, which confirmed the diagnosis of lymphangioma. Although a causal relationship between vaccination and lymphangioma cannot be proven, we cannot rule out the possibility that the lymph vessels were congested because of an inflammatory response in the axillary lymph nodes and vessels. The following observations support this possibility: (1) the symptoms first manifested after the second vaccination; (2) there were no abnormal findings in the left axillary region in the 2008 CT examination or the 2021 US examination; (3) the left axillary region had incurred no trauma; and (4) no radiotherapy had been performed following the earlier surgery for the right breast cancer.
Conclusions
Our findings indicated the possibility that occlusion of the axillary lymph vessels was caused by upper-arm injections of the COVID-19 vaccine. Further accumulation of cases is expected to elucidate the cause and pathogenesis of lymphangioma.
Availability of data and materials
The data are not available for public access because of patient privacy concerns.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- US:
-
Ultrasonography
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
COMIRNATY- covid-19 vaccine, mRNA injection, suspension Pfizer Laboratories Div Pfizer Inc. https://labeling.pfizer.com/ShowLabeling.aspx?id=15623 Accessed Jan 10, 2022.
Lehman CD, D’Alessandro HA, Mendoza DP, Succi MD, Kambadakone A, Lamb LR. Unilateral lymphadenopathy after COVID-19 vaccination: a practical management plan for radiologists across specialties. J Am Coll Radiol. 2021;18:843–52.
Consensus document on COVID-19 vaccination, Lymphoedema Support Network. Accessed Jan 10, 2022; 2022.
Advice for coronavirus vaccination—Lymphoedema or breast cancer. https://www.thebls.com/news-details/advice-for-coronavirus-vaccination-lymphoedema-or-breast-cancer. Accessed Jan 10, 2022. British Lymphology Society.
Godart S. Embryological significance of lymphangioma. Arch Dis Child. 1966;41:204–6.
Davidson AJ, Hartman DS. Lymphangioma of the retroperitoneum: CT and sonographic characteristic. Radiology. 1990;175:507–10.
Lindberg MR. Diagnostic pathology soft tissue tumors. 3rd ed. Elsevier; 2019. p. 446–9.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SS drafted the manuscript. HI, HT, TY, MS and HT supervised the writing of manuscript. SS, HI, TI, NM, MA, KO, AI, MT and MS provided managements of patient. MT and CH evaluated the radiographic images. YS and HU performed the histopathological evaluation. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient gave oral consent to this case report.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sasa, S., Inoue, H., Inui, T. et al. Axillary lymphangioma that developed following COVID-19 vaccination: a case report. surg case rep 8, 131 (2022). https://doi.org/10.1186/s40792-022-01488-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-022-01488-5