Abstract
Background
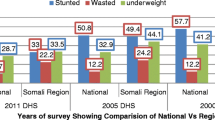
The National Family Health Survey-Round 3 in India during 2005–2006 recorded more children and women as anaemic compared to the prevailing situation eight years ago; more children also had wasting. Analysis of this dataset further linked adversity, rather than intrauterine biological processes, with under-nutrition running across generations. Against this background we conducted the present situation assessment in the Sundarbans area of India. The Sundarbans is world’s largest delta with mangrove forest and prone to natural disasters.
Methods
The current community based investigation was undertaken in five villages under Patharpratima block of the Sundarbans. Participants were selected randomly from the lists of eligible children (aged ≤5 year) and married women (≤49 year) prepared for each of the villages. Interviewer administered questionnaire, tools for anthropometry and hematologic auto-analyzer were used. Data from 561 children and 1145 married women (of which 55 were pregnant) were analysed.
Results
Underweight and stunting were recorded in 40 and 51 % of the children respectively. Of the 561 children, 47 (8 %), had severe acute malnutrition. Weight for height z-score reflecting acute and chronic state of nutritional deprivation revealed that four of the five villages were in critical stage. One fourth of the women had low body-mass-index (BMI). Hygienic practices of women were also poor; 41 % reportedly used water, mud/ash and not soap to wash hands after defecation. Anaemia prevalence in women of all the villages was >40 % underscoring a sever public health situation. Factors independently associated with anaemia in non-pregnant women (698/1090; 64 %) were residential-village, low (<18.5 kg/m2) BMI of women (Adjusted Odds Ratio; AOR = 1.39; 95 % CI of AOR 1.02–1.89), non-adoption of family planning method (AOR 1.86; 95 % CI of AOR 1.36–2.54; p < 0.001) and adopting contraceptive practices other than oral pills (AOR 1.84; 95 % CI of AOR 1.32–2.56; p < 0.001).
Conclusions
Sundarbans poses its unique public health challenge due to geographical-vulnerability. Securing nutritional support emerges as an immediate need for the study population residing in this natural-disaster prone area of islands and estuaries. The existing situation of anaemia in women requires innovative intervention development and would require addressing health seeking practices. Behavioural intervention appears to be the key.
Similar content being viewed by others
Background
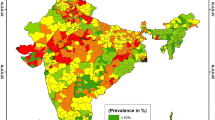
Analysis of maternal and child health in South Asia in early 2000 underscored the importance of health system strategies to improve the existing situation [1]. A relatively recent comparative study revealed that in the area of child survival, India lagged behind [2] other south and south-east Asian countries such as Nepal, Bangladesh and Indonesia. Contrasting the National Family Health Survey (NFHS Round 3) findings of 2005–2006 with that of an earlier survey, the study even highlighted that more children and women in India had anemia than in 1998 and more children showed wasting through malnutrition. A different team of researchers, who also used the NFHS 2005–2006 dataset, concluded that inter-generational mechanisms linking under-nutrition across subsequent generations seemed to depend particularly on continuity of adversity, rather than being determined by intrauterine biological processes [3]. Against this background, the current study was situated in the Sundarbans area of the district of south-24 Parganas in West Bengal, India. The overall purpose was to assess the situation of under-nutrition of children and anemia in women so that the government officials, civil society organizations and local communities could be appropriately informed and engaged in development of remedial measures.
Sundarbans, the largest delta of the world near bay of Bengal is a world heritage site, covers an area of 9630 km2 and is divided between Bangladesh and India. The area is prone to natural calamities. The Indian part of Sundarbans is smaller, covers 19 % of the total area and has a population of 4.5 million. It is situated 125 kms southeast to Kolkata, the capital city of West Bengal. Developmental challenges in the Sundarbans include but not restricted to low agricultural yield due to high soil salinity and ecological vulnerability from unpredictable climatic conditions [4]. Majority of the inhabitants depend on agriculture and face the challenge of considerable amount of land being engulfed by the rising sea level every year.
The present community based investigation was undertaken during 2012–2013 in the Patharpratima block of the Sundarbans (blocks represent planning and development units of a district). As the area was devastated along with other coastal districts of West Bengal following tropical cyclone AILA in 2009 [5, 6], the current investigation assumed importance from the larger perspective of changing environment and health vulnerability. We obtained approval of the scientific and institutional ethics committees of the National Institute of Cholera & Enteric Diseases (NICED), a premier institute of Indian Council of Medical Research (ICMR) located in Kolkata, prior to initiation of recruitment of the study participants.
Methods
Study area
The Patharpratima block has 92 villages of which five were included in the current study. The three villages namely Durbachati, Ramganga and Gopalnagar (DC-RG-GN), being the field area of partnering civil society organization ‘Sundarban Social Development Centre’ (SSDC), were under the purview of the present health assessment. The two other villages namely Dakshinraypur (DR) and Sreenarayanpur Purnachandrapur (SNP), which were covered as comparators, were in close proximity to DC-RG-GN and did not have SSDC-presence. Projects carried out by SSDC at different points in time in DC-RG-GN were on ‘nutrition’, ‘water, sanitation and hygiene’ (WASH) and ‘issues around rights of children and women’. The current assessment provided an opportunity to examine if situations of health of women and children in villages with SSDC-presence were better than that in comparator villages. An upcoming initiative of SSDC aiming to reduce vulnerability to environment induced health hazards among women and children in the Sundarbans necessitated the current investigation as a pre-requisite.
Participants
Participants were selected randomly from the lists of eligible children (aged ≤5 year) and married women (≤49 year) prepared for each of the study villages. Informed consent was obtained from every participant before recruitment in the study. Guardians (mostly mothers) provided consent for participation of children. Data from 561 children and 1145 married women were used in analyses. Twelve of 561 families (2 %), participating in assessment of children, were common and became part of the assessment of women’s health as well. Random draw of the study participants from master lists resulted in such commonality. Based on earlier investigations, we expected 40 % ‘under-weight for age’ in children [7] and 25 % anaemia in women [8]. Sample sizes were calculated with 90 % confidence level and 8 % relative precision. Practicalities such as available resource (time and money) and feasibility of covering larger sample size calculated with relatively stringent assumptions (such as 95 % confidence and 5 % relative precision) guided us to follow less rigorous assumptions as discussed by Lwanga and Lemeshaw [9]. Based on the aforementioned considerations, required sample size for children was 634 and for women 1268. Number of the participants covered in analyses were less than the calculated sample sizes, mostly due to non-availability of identified individuals at their respective residences during survey visits and a few incomplete interviews. The difficult study terrain did not allow paying more than two visits for any defaulter in recruitment.
Study tools
The tools used in the present structured cross-sectional survey included interviewer administered questionnaire, instruments for anthropometric measurements and hematologic auto-analyzer. Women were interviewed one-on-one. The domains of inquiry, among other things, constituted socio-demographic profile, types of food consumed, general health issues, sources of drinking water used, handling of drinking water at home, water used for washing utensils and reproductive health. In order to create a composite score for ‘Standard of Living Index’ (SLI), we inquired also about ownership of house and house type, possession of agricultural land, presence of livestock, assets related to transportation (bicycle, bullock cart, moped etc.), goods for entertainment and communication (such as radio, television), toilet facilities used, access to electricity, sources of water used, fuel type used for cooking etcetera. Composite SLI-scores ranging from 0 to 14 were considered low, 15–24 as medium and 25–67 as high for a family [10]. The tool used to create SLI-score for the families either participating in assessment of health of women and/or of children was the same. The difference in socio-economic conditions encountered in women and children could thus be attributed to random draw of samples from two different master lists. Each child was subject to anthropometric measurements and information on their vaccination details were also collected.
Nutritional assessment in children
Nutritional assessment of children ≤24 months of age was carried out by measuring weights and lengths. Infantometer was used to measure length of these children in supine posture. For children >24 months of age, anthropometer rod was used for measuring height in standing position. Weight for age z-score, weight for height z-score and height for age z-scores were calculated to identify children with underweight, wasting and stunting respectively. Mid- upper arm circumference (MUAC) was measured at the midpoint of the distance between acromian process of scapula and olecranon process of ulnar bone of the left arm [11].
Estimated percentage of children belonging to ‘ < −2 weight for height (WfH) z-score’ group helped classifying study-villages in different categories in terms of wasting (reflects both acute as well as chronic form of under-nutrition) as suggested by the World Health Organization (WHO). According to WHO-criteria [12], <5 % children belonging to ‘ < −2 weight for height (WfH) z-score’ group indicates acceptable, 5–9.9 % poor, 10–14.9 % serious and >15 %, critical situation of under-nutrition.
Body mass index (BMI) and measurement of hemoglobin in women
Women were assessed for height and weight by anthropometer rod and digital weighing scale respectively. Accuracy of the weighing machines were checked regularly against standard weights made available by bureau of standards, government of India. Women with low BMI were identified by using WHO cut-off (below 18.5 kg/m2) for Asian population [13]. Haemoglobin (Hb) estimation was carried out by using three part auto hematologic analyzer. The cut-off value used to define anaemia in non-pregnant women (aged ≥15 year) was Hb-level <120 g/l. As anaemia in pregnant women is defined at a lower haemoglobin level cut-off (<110 g/l), we have presented the data accordingly. Villages were classified depending on the prevailing situation of anaemia (<4.9 % prevalence indicating no public health problem, 5–19.9 % mild, 20–39.9 % moderate and ≥40 % prevalence indicating severe) [14].
Analyses
Applying WHO standards (WfH z < −3) as well as MUAC cut-off of 115 mm, we estimated the number of children with severe acute malnutrition (SAM). Both the criteria were applied as cases selected using weight-for-height z-score and MUAC are not the same [11]. Estimated percentage of children in two groups; one with a) z-score < −3SD and b) z-score < −2SD have been generated for descriptive statistics on underweight, wasting and stunting reflected through weight for age z-score (WfAz), weight for height z-score (wfhz) and height for age z-score (HfAz) respectively.
Blood specimen was collected from each of the consenting women for Hb-level estimation. Non-pregnant women with Hb-level <120 g/l were grouped as cases and the rest as comparators. Exposure variables tested for their association with the study outcome (presence of anaemia indicated by Hb-level <120 g/l) were selected a priori. Information on exposures were collected through interviewer administered questionnaire. Key exposures (explanatory variables), among other things, comprised of education, contraceptive practices, number of offspring, dietary habits and different hygienic and sanitary practices. Association of each of these exposure variables with anaemia, the binary outcome variable of interest, was examined through uni-variate analyses. Variables showing significant statistical association (p < 0.05 and confidence interval of odds ratios not capturing the null value of 1) with anaemia in uni-variate analyses and having conceptual relevance to intervention development along with biologic plausibility were entered simultaneously in a multivariate logistic regression model and adjusted for potential confounders such as ‘age’ and ‘residential-village’.
Analysis for determinants of anaemia in pregnant women could not be conducted due to low number of participants in this group. Software packages Epi-Info (version 6.4b, Centres for Disease Control, Atlanta, GA, in collaboration with World Health Organization, Geneva, Switzerland), WHO Anthropo (version 3.2.2) and SPSS (version 8.0 SPSS, Chicago, IL) were used for data analyses.
Results
Socio- demographic profile
Fifty four percent of the children surveyed were male (304/561); by faith most of the families they belonged to were Hindu (491/561; 87 %) and the rest Muslim. Thirty eight children (7 %) were below six month of age and the rest were within 6 to 60 month age bracket. While 196 children participated from DC-RG-GN (35 %), 180 were from DR (32 %) and 185 (33 %) were from SN. As per composite SLI score, a fifth of the children surveyed from DC-RG-GN belonged to low socio-economic strata and very few children in DR (14/180; 8 %) and SN (10/185; 5 %) were in this group. Overall, 12 % (66/561) of the children were in low, 57 % (319/561) in medium and 31 % (176/561) in high socio-economic group.
Of the 1145 married women recruited in the current survey, 55 were reportedly pregnant. The following results relate to 1090 non-pregnant women, about a third of whom, belonged to each of the three types of study villages (DC-RG-GN, DR and SNP). The mean age of the women was 29 year (median 27; SD ± 8; minimum 15; maximum 49). According to composite SLI score, 54 % (586/ 1090) belonged to families in low socio-economic category, 38 % (417/1090) in the middle and 8 % (87/1090) in higher bracket. While only 6 % of women were engaged in income generation activities, 93 % (1017/1090) reported their spouses being the bread winner of the families; Table 1 presents additional socio-demographic information.
Nutritional status of children & related issues
While severe underweight (WfA z-score < −3) and severe stunting (WfH z-score < −3) were observed in 14 % and 31 % of children respectively, overall prevalence of underweight and stunting (indicated by respective z-scores < −2) were 40 and 51 %. Categorization of villages based on prevalent situation of wasting, reflecting under-nutrition of both short and long duration, placed SNP in ‘serious’ (22/185; 12 %) and the rest of the villages in ‘critical’ zone of concern (DR 38/180; 21 % and DC-RG-GN 51/196; 26 %). Of the 561 children, 47 (8 %), were diagnosed with SAM.
Forty six percent of the surveyed children reportedly were born at home and the rest experienced institutional delivery. Breast feeding was initiated by 70 % (393/561) of the mothers within an hour and 15 % within 6 h of child birth. The rest reported initiating breast feeding within a day or even later after delivery. Colostrum was fed to newborn children by 89 % of the mothers. In response to the question ‘how many days did you feed your child with only breast milk’, 6 of the 561 respondents (1 %) reported not breast feeding their children at all and 113 (20 %) reported exclusive breast feeding for less than six months. About a fifth of the mothers reported feeding water (plain water, anis water, honey water or sugar candy water as part of ritualistic practice) to newborn who were supposed to have breast milk only.
‘Full immunization’ is defined under the national immunization program in India as administration of Bacillus of Calmette-Guerin (BCG), three doses of oral polio vaccine, three doses of diphtheria-pertussis-tetanus (DPT) injection and measles vaccine to 12–23 month old children. In our study cohort 119 children belonged to the age group of 12 to 23 month. Ninety two of such 119 (78 %) children were estimated to be fully immunized.
Hygienic practices
Sources of drinking water, types of toilets used, water used in utensil washing, and hand washing practices after defecation were explored as indicators of hygiene. While 99.5 % of non-pregnant women (1085/1090) used tube-well (hand pump) water, only one reported using pond water and the rest few used pipe-water supply for drinking purpose. Eighty percent of the women reported washing utensils with pond water. While open defecation was reported by 13 % (147/1090), pond-side latrine (a covered space for defecation where faecal contamination of environment takes place as in open defecation) reportedly was used by 7 % (78/1090) and about one third of the respondents used pit latrine (376/1090). Forty three percent women (465/1090) said that they were using sanitary latrine. Forty one percent women (437/1090) reported not using soap to wash hands after defecation; they rather used water, soil, ash etcetera. Distributions of these and other key exposure variables in women with anaemia and those who were not anaemic have been detailed in Table 2.
Health of women
Sixty percent pregnant (33/55) and 64 % non-pregnant women (698/1090) were anaemic; 24 % (266/1090) of the non-pregnant women had lower than normal BMI. One fourth of the non-pregnant anaemic women had hypochromic microcytic red blood cells (mean corpuscular volume <81 fl) indicating a probable state of iron deficiency.
Association between key risk factors and anaemia in non-pregnant women were examined (Table 2). Religious affiliation, involvement of women in income generation activities, self-reported dietary habits (barring intake of germinated gram, which is a rich source of vitamin B12 & folic acid), handling of drinking water at home, utensil wash practice, open air defecation and hand wash practice following defecation were not associated with anaemia. Factors independently associated with anaemia in non-pregnant women in multivariate model were identified after adjusting for age, residential-village, school attendance, number of offspring born to a woman, BMI, frequency of intake of germinated gram and contraceptive practice (Table 3). While women residing in DC-RG-GN had about 1.5 times the odds (adjusted OR 1.42; 95 % CI of adjusted OR 1.01 - 2.01; p < 0.042) of having anaemia compared to women in SNP, women with BMI < 18.5 kg/m2 had similar odds of being anaemic. Also women currently not practising any family planning method (adjusted OR 1.86; 95 % CI of adjusted OR 1.36–2.54; p < 0.001) or using contraceptive methods other than oral pills for family planning had about twice the odds of being anaemic compared to those using oral hormonal contraceptive pills (adjusted OR 1.84; 95 % CI of adjusted OR 1.32–2.56; p < 0.001).
Discussion
The current investigation reveals a concerning situation of under-nutrition in children and anemia in women in the Sundarbans area of West Bengal. Findings emerging from this study have implications for intervention development. However effective health service delivery in the natural-disaster prone geographical locations of Sundarbans crisscrossed by estuaries and islands in the Bay of Bengal is a public health challenge and effective engagement of local communities in intervention development is paramount. The poor state of healthcare infrastructure in Sundarbans has been highlighted in earlier investigations by researchers [15]. Worth noting in this context is that the present situation assessment was located in the Patharpratima block, one of the six blocks recorded to have relatively better healthcare facilities compared to others [16].
Eight percent of children in the present survey had SAM. Prevalence of wasting in four of the five study-villages was assessed to be ‘critical’ - affecting one fifth of the surveyed population. In this context, it is important to note that of 19 million severe acute malnourished children in all developing countries, 8 million (42 %) are in India. This number constitutes one-third of the global burden [17, 18].
It is important to note from the perspective of intervention development that about 90 % of SAM children do not present with medical complications and can be cared for in their communities without admitting them to a health facility, whereas those with medical complications need such admissions. Children managed at specialized units located at health facilities also require follow up services at their households after discharge in order to maintain a continuum of care and support and to prevent relapse [19, 20]. The eastern Indian state of Bihar has generated encouraging results through community based intervention in this regard [21]. The current investigation, by highlighting a severe state of under-nutrition in Sundarbans, thus underscores the need for establishing outreach activities paired with facility based intervention. Given the state of wasting among children in the study area indicating both acute and chronic malnutrition, improvement in basic food supply as well as supplementary feeding is warranted [12]. Immunization program for children in the Sundarbans also need to be beefed up as ‘full immunization’ coverage was estimated in our study population to be 78 %. Worth noting in this context is a sub-study among under-five children we conducted in Ramganga village where 89 diarrhoeic children were contrasted with 105 children not experiencing such episodes. The study showed that children on exclusive breast feeding for less than six months had greater chance of having diarrhoea compared to their counterparts who were breast-fed for longer periods; similarly those who had food from ‘anganwadi’ centre under integrated child development scheme suffered less [22] from diarrhoea compared to those who did not attend such centres.
Inappropriate child feeding practices were reported by women during the current study. While 90 % of the mothers fed newborns with colostrum, and about a fifth followed ritualistic practices such as feeding newborns with anis water, honey water, sugar candy water or even plain water; 20 % had put their children exclusively on breast for less than six months. Our findings corroborated with that of other investigators who recorded poor knowledge, attitude as well as practices of mothers as regards to child feeding in the Patharpratima block of the Sundarbans [23]. In addition, our study recorded ritualistic practices based on perception of mothers and highlight the need for developing socio-culturally appropriate behaviour change communication.
Lastly, a fourth of the married women in reproductive age group in the study villages suffered from poor health indicated by lower than normal BMI. Hygienic practices were also at a poor state; 41 % of the women reported using water, mud/ash and not soap to wash hands after defecation. Village-disaggregated data revealed that the prevalence of anaemia in women in all the villages was of concern. Factors independently associated with anaemia in women were non-adoption of family planning, non-use of oral contraceptive pill as a family planning method and residence at DC-RG-GN. As usage of hormonal oral contraceptive pills (OCP) by women is known to improve the level of iron reserve in women as indicated by increased haemoglobin as well as ferritin level [24] and also by reducing menstrual blood loss [25], it was necessary to inquire about OCP and non-OCP based family planning methods in detail. However, family planning methods followed by women would not suffice as sole explanatory factor behind prevalence of anaemia in women of reproductive age group in the study area as ‘number of children of women’ did not have statistically significant association with anaemia. Detailed dietary habits, available and absorbable iron present in the food items consumed, sanitary practices (keeping in mind the link between open defecation and soil-transmitted helminths) and chronic morbidities experienced by women would also need to be researched in-depth.
It is noteworthy that 78 % women did not report consumption of any red meat. While potential intervention around such observations and findings on the link between family planning method and anaemia could be conceived, it is important to note that a review of interventions from Indian states of Uttar Pradesh, Maharashtra, Gujarat, Rajasthan, Jharkhand, West Bengal and Bangalore has highlighted evidence gaps existing in the country regarding management of iron deficiency anaemia [26]. Implementing effective intervention to reduce anaemia in women in a setting like Sundarbans would therefore require innovation. At a smaller scale though, dissemination of current situation assessment findings to local level stakeholders including district magistrates, civil society organizations, local village administration (panchayat) and participating women fostered positive health seeking behaviour [27]. However, the population-level challenge still remains as the recently released preliminary findings of NFHS-Round 4 (2015–2016) for the district of south 24-Parganas reveals that 20 % of the women in 15–49 years age group is recorded to have BMI lower than normal and 69 % of non-pregnant women in the same age group has anaemia [28].
Conclusion
Despite several limitations such as cross-sectional nature of our investigation necessitating simultaneous collection of information on outcome (such as anaemia in women) as well as key risk factors and lack of in-depth investigation about causes of anaemia in women, the present situation assessment has unearthed serious public health situation prevailing in the Sundarbans area of West Bengal, India. Limited availability of resources also did not allow in-depth exploration of dietary assessments of the study population. However, two key parameters - under-nutrition in children and anaemia in women - have served important role in assessing the health of the study population. While, in view of the existing ‘critical’ state of under-nutrition, securing food and nutrition for the entire underserved villages has emerged as an immediate need, the situation of anaemia in women calls for innovative intervention development. Active engagement of local level stakeholders, community and health authorities would be critical in all such endeavours.
Abbreviations
- AOR:
-
Adjusted odds ratio
- BCG:
-
Bacillus of Calmette-Guerin
- BMI:
-
Body Mass Index
- CI:
-
Confidence interval
- DC-RG-GN:
-
Durbachati-Ramganga-Gopalnagar (villages)
- DPT:
-
Diphtheria-Pertussis-Tetanus
- DR:
-
Dakshinraypur (village)
- HfA:
-
Height for age
- ICMR:
-
Indian council of medical research
- MUAC:
-
Mid-upper arm circumference
- NFHS:
-
National family health survey
- NICED:
-
National Institute of Cholera & Enteric Diseases
- OR:
-
Odds Ratio
- SAM:
-
Severe acute malnutrition
- SC:
-
Save the children
- SD:
-
Standard deviation
- SN:
-
Sreenarayanpur-purnachandrapur
- SSDC:
-
Sundarbans social development centre
- WfA:
-
Weight for age
- WfH:
-
Weight for height
- WHO:
-
World Health Organization
References
Bhutta ZA, Gupta I, De’Silva H, Manandhar D, Awasthi S, Moazzem Hossain SM, et al. Maternal and child health: is south Asia ready for change. BMJ. 2004;328:816–9.
Jha P, Laxminarayan R. Choosing Health: an entitlement for all Indians. Toronto: Centre for Global Health Research; 2009. p. 12–13.
Subramanian SV, Ackerson LK, Smith GD. Parental BMI and Childhood under-nutrition in India: an assessment of intrauterine influence. Pediatrics. 2010;126:e663–71. doi:10.1542/peds.2010-0222.
Singh OP. Long-term trends in the frequency of severe cyclones of Bay of Bengal: observations and simulations. Mausam. 2007;58:59–66.
Centre for Science and Environment. Living with changing climate: Impact, vulnerability and adaptation challenges in Indian Sundarbans. (supported by) DanChurch Aid, Church of Sweden, Swedish International Development Agency (SIDA) and Evangelischer Entwicklungsdienst e.V (EED) 2012.
Panda S, Pati KK, Bhattacharya MK, Koley H, Pahari S, Nair GB. Rapid situation & response assessment of diarrhoea outbreak in a coastal district following tropical cyclone AILA in India. Indian J Med Res. 2011;13:395–400.
Bharati S, Chakrabarty S, Som S, Pal M, Bharati P. Socio-economic determinants of underweight children in West Bengal, India. Asian Pac J Trop Med. 2010;3:322–7.
Sengupta B and Chakrabarti S. Study of anaemia among rural women of some districts of West Bengal with a view to use biotechnological methods. (Final Report DBT /WB sanction letter No.: 61/ 1(5)-BT Estt /RD-3/08 dt 05.02.2008) Ramakrishna Mission Seva Pratisthan Vivekananda Institute of Medical Sciences.
Lwanga SK, Lemeshaw S. Sample size determination in health studies: a practical manual. Geneva: World Health Organization; 1991. p. 2–3.
IIPS and Macro International. National Family Health Survey (NFHS-2), 1998–99: India. Mumbai: International Institute of Population Sciences; 2000.
World Health Organization & UNICEF. WHO child growth standards and the identification of severe acute malnutrition in infants and children - a joint statement by the World Health Organization and the United Nations Children’s Fund. 2009.
World Health Organization Regional Office for the Eastern Mediterranean. Field guide on rapid nutritional assessment in emergencies. 1995.
WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
World Health Organization (WHO) & Centre for Disease Control (CDC), Atlanta. In: De BB, McLean E, Egli I, Cogswell M, editors. Worldwide prevalence of anemia 1993–2005: WHO global database on anemia. 2008.
G Mazumdar P, Kanjilal B, Barman D, Mandal A. Revisiting the Role of Geographical Accessibility in Women’s Access to Healthcare. Rajasthan: Institute of Health Management Research; 2009.
Dipanwita D. Spatial inequality in healthcare infrastructure in Sundarban, West Bengal, India. Int Res J Soc Sci. 2014;3:15–22.
International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005–2006. Mumbai (India): IIPS; 2007.
UNICEF. Tracking progress on child and maternal nutrition: a survival and development priority. New York: UNICEF; 2009.
Collins S, Sadler K, Dent N, Khara T, Guerrero S, Myatt M, et al. Key issues in the success of community-based management of severe malnutrition. Food Nutr Bull. 2006;27:S49–82.
National Rural Health Mission, Ministry of Health and Family Welfare, Government of India. Operational guidelines on facility based management of children with severe acute malnutrition. 2011.
Burza S, Mahajan R, Marino E, Sunyoto T, Shandilya C, Tabrez M, et al. Community-based management of severe acute malnutrition in India: new evidence from Bihar. Am J Clin Nutr. 2015;101:847–59.
SSDC-NICED-Save the Children. Health status of women and children in Sundarbans. 2014. p. 10–1.
Institute of Health Management Research (IIHMR). Combating Malnutrition in Children in Disaster Prone Patharpratima Block of Sundarbans, West Bengal (India), Baseline Study Report (submitted to Tdh Foundation). January 2012.
Task Force for Epidemiological Research on Reproductive Health, United Nations Development Programme/United Nations Population Fund/World Health Organization/World Bank Special Programme of Research, Development and Research Training in Human Reproduction, World Health Organization, Geneva, Switzerland. Effects of contraceptives on hemoglobin and ferritin. Contraception. 1998;58:261–73.
Carey M, Allen RH. Non-contraceptive uses and benefits of combined oral contraception. Obstetrician Gynaecologist. 2012;14:223–8. doi:10.1111/j-1744-4667.2012.00126.x.
USAID & Vistaar. Community-level interventions to prevent and treat anemia: a review of evidence from India. Evidence Review Series 3; March 2008.
Save the Children. Environmental Health: stories from the Sundarbans (supported by Sweden). 2013. p. 2–3.
International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey-4: District Fact Sheet South 24 Parganas West Bengal 2015–2016. (Assistance from Ministry of Health & Family Welfare; Government of India, USAID, UKaid, Bill & Melinda Gates Foundation, UNICEF, UNFPA, McArthur Foundation). 2016.
Acknowledgements
Not applicable.
Funding
The study was supported entirely by extramural financial assistance received by NICED from Save the Children (SC), West Bengal Office who in turn was supported by Sweden. The decision makers at SC office about funding did not have any role in the design, collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets generated or analysed during the current study are not publicly available due to unique geographical vulnerability and sensitivity attached to the study location situated at the bordering area between India and Bangladesh but are available from the corresponding author on reasonable request.
Authors’ contributions
While SP, CP and GP were responsible for study design, SP, GP, SoP and JH contributed in study tool development and SP, CP and SoP were involved in supervising implementation of the current assessment. SP, SoP & JH were involved in data cleaning and analyses. All the authors provided critical inputs in various stages of study execution and read and approved the final version of the article for submission.
Authors’ information
Not applicable.
Competing interests
While SaP conducted the assessment on behalf of NICED, SoP and JH were staff of the assessment Project. During the present assessment CS, served as a staff of Save the Children (SC, Bal Rakshak Bharat), West Bengal State Office that extended financial support under extramural assistance to NICED (ICMR) for conducting the study and GP belonged to the collaborating civil society organization SSDC that received grants from SC for intervention in localities in the study district.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The present study obtained approval from the “Institutional Ethics Committee” of the National Institute of Cholera & Enteric Diseases (Indian Council of Medical Research), Registration No. ECR/416/Inst./WB/2013 (Under DCGI) and informed consent was obtained from the each of the study participants (when adult) and from the legal guardians of the minors (under-5-children) prior to recruitment.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Panda, S., Sadhu, C., Pramanik, G. et al. Concerning public health situation of under-nutrition in children and anemia in women in Indian Sundarbans delta: a community based cross-sectional investigation. BMC Nutr 2, 65 (2016). https://doi.org/10.1186/s40795-016-0105-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-016-0105-3