Abstract
Background
Individuals with severe mental disorders (SMDs; schizophrenia spectrum disorders, bipolar disorder, and major depressive disorder) are not only suffering from their mental conditions; they also have an attenuated physical health, augmenting their overall critical condition.
Objectives
We review and critically appraise the evidence based on (1) key physiological factors relating to aerobic endurance and skeletal muscle strength; (2) implications for physical function and health; and (3) effects of training interventions with different intensities evaluated in individuals with SMDs.
Findings
Reductions in aerobic endurance factors, peak oxygen uptake (VO2peak) and walking work efficiency, are paralleled by reductions in maximal skeletal muscle strength and power. In turn, the poor aerobic endurance and muscle strength lead to impaired physical function, increased risk of lifestyle-related diseases, and ultimately early death. Exercise has the potential to counteract the attenuated physical health in people with SMDs. While aerobic endurance training is shown to increase VO2peak due to plasticity of the oxygen transport system, strength training is documented to improve maximal muscle strength, power, and walking work efficiency as a result of adaptations in neuromuscular force developing factors.
Conclusions
In conclusion, improvements in these key determinants for physical health appear to be achievable in people with SMDs despite many being challenged by motivational difficulties with attending regular exercise and have beneficial implications for physical function during activities of daily living, lifestyle-related diseases, and early death.
Similar content being viewed by others
Key Points
-
Physical activity is often recommended in clinical treatment of people with severe mental disorders but appears not to result in increased life expectancy and reduced prevalence of CVD.
-
Physical training is an effective countermeasure to improve the low aerobic endurance and skeletal muscle strength in these individuals, factors directly associated with CVD and all-cause mortality, and should thus be included in clinical practice.
Introduction
People with severe mental disorders (SMDs; schizophrenia spectrum disorders, bipolar disorder, and major depressive disorder) have an estimated prevalence of ~ 1 to 18% worldwide [1,2,3,4]. Strikingly, people suffering SMDs have 10–20 years reduced life expectancy. The leading causes of death are lifestyle-related illnesses, in particular cardiovascular disease (CVD) [5,6,7]. While antipsychotic side effects and other factors such as smoking may augment poor physical health [8, 9], physical inactivity is suggested to be the origin of CVD development [10,11,12]. As a consequence, physical activities have been implemented as a countermeasure in treatment at a wide range of clinics around the globe [11, 13,14,15,16,17,18]. Paradoxically, the life expectancy gap in individuals with SMDs has continued to increase over the past 20–30 years [7, 19, 20]. Lack of access to and provision of health care, with subgroups of individuals particularly difficult to reach (e.g., relating to severity of illness) [21, 22], in combination with metabolic side effects of second-generation antipsychotics [23] may to some extent accentuate the inability to bridge the life expectancy gap. However, it should be questioned if many of the applied physical activities have a sufficient overload to improve critical components of physical health. Aerobic endurance and skeletal muscle strength, respectively, are acknowledged as key factors to healthy aging and longevity [24, 25], and a purposively judicious appraisal of the status of these measures in people with SMDs, and how they may effectively and substantially be improved by training interventions, is warranted.
The present article disseminates and critically appraises the existing literature on (1) aerobic endurance (maximal/peak oxygen uptake [\({\dot{\text{V}}}{\text{O}}_{{2{\text{max}}}}\)/\({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\)] and walking work efficiency) and skeletal muscle strength factors (maximal strength [one-repetition maximum, 1RM] and power) in individuals with SMDs; (2) the implications for physical function and longevity; and (3) the beneficial impact of exercise at different intensities along with safety and feasibility considerations. Specifically, the article separates between the distinctly different physiological effects of aerobic endurance and strength training and their critical importance in the war against inactivity in this patient population.
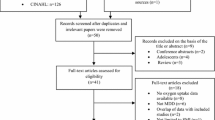
Search Criteria and Study Selection
The original articles reviewed were selected from a literature search on the PubMed/Medline database from inception to February 1, 2022. For the purpose of identifying studies reporting data on aerobic endurance factors, skeletal muscle strength, and physical function, searches for each SMD group were applied with the following combination of medical subject headings (MeSH) and specific terms: (exercise test OR aerobic capacity OR cardiorespiratory fitness, OR muscle strength OR maximal strength OR one-repetition maximum OR force-generating capacity OR power OR rate/rapid force development OR physical functional performance OR activities of daily living); AND (schizophrenia spectrum and other psychotic disorders OR bipolar and related disorders OR depressive disorder, major). To identify exercise interventions, searches for each SMD group were applied with the following combination of MeSH terms: (exercise OR endurance training OR high-intensity interval training OR resistance training); AND (schizophrenia spectrum and other psychotic disorders OR bipolar and related disorders OR depressive disorder, major). The literature search was performed individually by authors MFB and MN with relevant studies collated before inclusion and critical appraisal. Inclusion criteria were ≥ 1 of the target outcomes; endurance training applying an intensity of ≥ 70% of peak/maximal heart rate or a corresponding workload; or strength training with a load of ≥ 60% of 1RM, to ensure appropriate classification of protocols as endurance or strength training [26, 27]. Disagreements regarding the inclusion of studies were discussed between all authors until consensus was reached. Reference lists of reviews and included original articles were also searched manually to identify other relevant articles not previously found through electronic searches.
Oxygen Uptake
Physical Performance and Health: The Role of Maximal Oxygen Uptake
\({\dot{\text{V}}}{\text{O}}_{{2{\text{max}}}}\), commonly recognized as the single most important factor for endurance performance [28, 29], is defined as the “greatest rate of oxygen utilization under any given set of conditions” [30] and reflects all factors in the oxygen transport chain, from air to mitochondria [31]. In clinical populations, it is relatively common that criteria for appropriate \({\dot{\text{V}}}{\text{O}}_{{2{\text{max}}}}\) determination [32] are not reached because many individuals experience difficulty exercising to volitional exhaustion due to motivation, symptoms, medication, or fear. In this case, the highest achieved oxygen uptake measured during a given test is referred to as \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) [33]. Secondary testing criteria, such as respiratory exchange ratio, maximal/peak heart rate, and rating of perceived effort, are often applied to counter this shortcoming. Not being very faithful to the venerable Fick principle [34], which unmistakably states that both central and peripheral factors in the oxygen transport may limit the greatest oxygen utilization rate, the term cardiorespiratory (cardio- respiratory-) fitness is often used interchangeably with \({\dot{\text{V}}}{\text{O}}_{{2{\text{max}}}}\) in the clinical literature. Importantly, low \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) is also well acknowledged to be an important risk factor for CVD and premature mortality. This may be unsurprising considering \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) reflects cardiac function and output as well as all further steps in the oxygen transport chain to the mitochondria. Specifically, a \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) reduction by 1 metabolic equivalent of task (MET; 3.5 ml·kg-1·min-1 of oxygen uptake) is associated with increased risk of all-cause mortality and CVD by 12–13% and 15%, respectively [24, 35]. The survival benefit per MET increase has been firmly established through a wide range of studies of symptomatic and asymptomatic men and women at different ages [36], and particularly poor prognosis seems to be present for individuals with the lowest values [24, 35]. Additionally, \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) has also been shown to decrease by approximately 1 MET (~ 10%) per decade from the fourth decade of life [37].
Peak Oxygen Uptake and Severe Mental Disorders
Although persons with SMDs have different mental conditions, all subpopulations appear to have a substantially reduced \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) compared to healthy reference values [37]. In people with schizophrenia [38, 39], \({\dot{\text{VO}}}_{{2{\text{peak}}}}\) reductions typically range from − 7 to − 14 ml kg−1 min−1, while people with major depressive [40,41,42,43] and bipolar disorder [44, 45] display reductions of − 5 to − 10 and − 4 to − 5 ml kg−1 min−1, respectively, compared to reference populations (Table 1). Due to the application of direct pulmonary measurements during incremental exercise protocols to exhaustion, the gold standard for clinical \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) assessment, a robust body of evidence supports reduced \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) in people with SMDs. Interestingly, the extent to which the physiological age of people with SMDs is reduced, as expressed by \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\), also appears to mirror their 10–20 years of shorter life expectancy. However, identification of sex-specific \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) values appears to be rare, particularly in people with major depressive and bipolar disorder. In some cases, only \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) values relative to bodyweight (ml kg-1 min−1) are reported, which increases the difficulty of examining interstudy differences as bodyweight may differ considerably. Notably, \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) is commonly tested on cycle ergometers due to safety concerns. This may result in 5–10% lower values compared to treadmill tests and should be taken into account when interpreting results across studies [46].
While \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) remains a strong predictor of mortality, the relationship between physical activity and \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) is shown to be relatively weak and inconsistent in both people with schizophrenia spectrum disorders [38] and healthy adults [47], indicating that simply increasing physical activity without a concomitant increase in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) may not necessarily improve CVD and mortality risk prognosis.
Indirect Estimation of Peak Oxygen Uptake
Because direct measurements require expensive equipment, experienced test personnel, and may be difficult to undertake for some individuals, \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) is often estimated by indirect methods [48]. Unfortunately, it may result in gross inaccuracy [36]. Even when tests to exhaustion are applied, such as the Bruce [49] or BSU/Bruce ramp [50] protocols, the standard error of estimate is shown to be 3.2 and 3.4 ml kg−1 min−1, respectively. This implies that in 95 out of 100 cases, a patient with a \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) of, for example, 35 ml kg−1 min−1 will display a value within a range of ~ 13 ml kg−1 min−1, which corresponds to ~ 50 to 60% difference in risk assessment of all-cause mortality and CVD. It may also camouflage the gap between populations and the true change in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) following endurance training interventions. Consequently, while indirect \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) tests are certainly easier to carry out, results may be highly misleading.
Walking Work Efficiency in People with Severe Mental Disorders
Another important factor for aerobic endurance performance [51], along with V̇O2max, is work efficiency, the ratio between work output and oxygen uptake [52, 53]. Physical work conducted less efficiently implies that human locomotion requires more energy and oxygen consumption, resulting in impaired aerobic endurance and poorer physical function during activities of daily living. In the clinical setting, it is, because of functional relevance during daily tasks, commonly assessed when walking. Walking work efficiency is shown to be 14% lower in people with schizophrenia spectrum disorders compared to healthy references [54]. Analyzing men and women separately, work efficiency was reduced by 17% in the men and tended to be reduced by 9% in the women. To the best of our knowledge, this is the only study that has assessed this functionally important factor for aerobic endurance in people with schizophrenia, and it appears that no studies have examined walking work efficiency in individuals with major depressive or bipolar disorder. However, reduced walking work efficiency by 12% has also been documented in people with substance use disorders, with no difference between sexes [55], as well as individuals with preexisting CVD [56, 57].
Muscle Strength
Physical Performance, Health, and Skeletal Muscle Strength
Maximal muscle strength and power are key components affecting functional performance in everyday life and have both been acknowledged as independent risk factors of all-cause mortality [58,59,60]. Maximal muscle strength is typically measured as the heaviest weight one can lift once in a given movement (1RM) and decreases by approximately 1% per year from the fourth decade of life [61]. Power is a sub-component of maximal muscle strength and a product of work over time, i.e., force × velocity [25]. Interestingly, power declines at a faster rate compared to maximal muscle strength, approximately 3% per year [62], and there is mounting evidence that of these two factors, power may be more strongly associated with functional performance with aging [63].
Maximal Muscle Strength and Severe Mental Disorders
How maximal muscle strength is affected in individuals with SMDs is a growing area of research. Despite strong indications, there are still knowledge gaps in the literature in terms of whether, and to what extent, maximal muscle strength is reduced across all subpopulations of SMDs. Dynamic leg press 1RM is shown to be 13 and 19% lower in women and men with schizophrenia spectrum disorders, respectively, compared to age- and sex-matched controls (Table 2) [54]. Isometric unilateral hip and knee extension strength is shown to be 32 and 42% lower, respectively, in individuals with major depressive disorder compared to healthy controls [64]. While lower extremities maximal muscle strength appears to be undocumented in individuals with bipolar disorder, maximal isometric handgrip strength is shown to be consistently attenuated across all subpopulations with SMDs, with reductions ranging from 14 to 41% [65,66,67]. Apart from one study, our literature search failed to identify studies which included results describing sexes separately. Although relatively few studies have measured dynamic maximal muscle strength directly both in the lower and in the upper extremities in individuals with SMDs, the extent to which maximal strength is reduced, similarly to observations in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\), seems to comply with the 10–20-year reduction in life expectancy.
Skeletal Muscle Power and Severe Mental Disorders
Skeletal muscle power in the lower extremities is shown to be impaired by 25% in men and 30% in women with schizophrenia spectrum disorders compared with healthy references (Table 2) [54]. Standing broad jump performance, a proxy for lower extremities power assessment, is also documented to be reduced by 26 and 20% in individuals with schizophrenia spectrum disorders [65] and bipolar disorder [66], respectively, supporting the finding of blunted ability to produce force rapidly in these individuals. Sex-specific results, again, also appear to be lacking for skeletal muscle power in people with major depressive and bipolar disorder, increasing the difficulty of firmly establishing if neuromuscular force production is equally impaired in both sexes. However, given that lower extremity maximal muscle strength and power appears substantially reduced also in patients with substance use disorders undergoing clinical treatment [68], it may be that attenuated neuromuscular function is a prominent feature across psychiatric groups.
Testing of Maximal Muscle Strength and Power
To the best of our knowledge, data from dynamic tests of maximal muscle strength and power in the functionally important lower extremities are scarce, particularly pertaining to individuals with major depressive and bipolar disorder. Further, a range of tests have been utilized and maximal muscle strength is predominantly documented in upper extremities small muscle mass [65,66,67]. Measurements of lower extremities maximal muscle strength and power are relatively simple to conduct, and thus it is somewhat surprising that handgrip testing applying dynamometers appears to be a far more popular choice. However, the lower extremities ensure the ability to perform daily activities important for independent living, such as walking, stair climbing, and chair rising. Consequently, assessment of lower extremities muscle strength provides clinically relevant information. Additionally, since dynamic tests resemble human locomotion more closely than isometric measurements, the former will likely have higher transfer value to assessment of weight-bearing functional performance. As for V̇O2 measurements, direct assessment maximal muscle strength and power is preferable with regards to accuracy and reliability.
The Importance of Allometric Scaling in Maximal Muscle Strength and Power Testing
A muscle’s force development potential is directly proportional to its cross-sectional area [69]. Maximal muscle strength and power are thus greatly affected by size of body proportions. People with SMDs are often overweight compared to healthy individuals, and direct comparisons of results between groups may be misleading. Comparing two geometrically similar individuals with different height and body mass, one would expect the larger individual to perform better in absolute terms of weight lifted (kg) for a given movement, while dividing force produced (cross-sectional area; L2) by body mass (volume; L3) would lead to underestimation of the performance. Allometric scaling accounts for this effect by dividing the outcome variable by body mass raised to the power of 0.67 (or L2/3) [69]. Previous studies have sought to include persons with SMDs and healthy references with similar characteristics by matching for age and sex [67], body mass index [65, 66], or height and weight [64]. This certainly leads to more accurate assessments; however, the application of allometric scaling may further facilitate intergroup/interstudy comparisons when different test protocols are utilized.
Implications for Physical Function, CVD Risk, and Early Death
Impairments in aerobic endurance and/or muscle strength imply that typical activities of daily living either require a higher percentage of an individual’s physical capacity, and thus are experienced as more vigorous, or not successfully completed at all. Two recent studies show that people with schizophrenia perform on par with 20–30 years older healthy references (− 20 to − 60%) during functional performance tests, i.e., walking, chair-rising, stair climbing, and balance [54, 70]. Walking performance is also shown to be reduced by − 23 and − 16% in individuals with major depressive [64] and bipolar disorder [71], respectively, compared to healthy controls. Notably, maximal muscle strength and power are associated (r = 0.4–0.7) with functional performance across all subpopulations (Fig. 1, schizophrenia spectrum disorders) [54, 64, 72]. Further, given robust evidence highlighting the inverse relationship between \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) and maximal muscle strength with risk of CVD and mortality, the current literature underpins that these factors combine to attenuate functional performance and elevate the risk of CVD and early death, ultimately compounding the critical condition of individuals with SMDs.
Relationship between muscular force-generating capacity and functional performance in force-demanding tasks. Associations between allometrically scaled one-repetition maximum (1RM) and performance in 30-s sit-to-stand test (A) and stair test (B). Associations between allometrically scaled rapid force development and performance in 30-s sit-to-stand test (C) and stair test (D). Used with permission from Nygård et al. [54].
Exercise is Medicine for People with Severe Mental Disorders
For exercise to produce a measurable training effect, it must involve stimuli greater than the one usually encountered through everyday life in order to create an overload [73]. Exercise, i.e., subjecting a person to a training load or physical work, must be of adequate frequency, duration, and intensity to improve the function of key physiological systems [73]. By extension, when physical activity or exercise is available as treatment, a lack of overload due to one or more of these factors, which closely relates to changes in physical capacity and thus prognosis of adverse outcomes, may be of critical concern. Endurance and strength training represent two distinctly different types of training where the former has the purpose of overloading factors involved in oxygen transport and/or anaerobic energy production and the latter has the purpose of overloading factors involved in skeletal muscle force production. Both training types may independently contribute to adaptations that improve health and physical function in people with SMDs. Thus, it is important to consider the effects of endurance and strength training separately, and not combine them in the inaccurate term “physical activity.”
In individuals with SMDs, mean attrition rates of 17–27% have been reported from exercise interventions [16, 74, 75], on par or somewhat higher compared with control conditions and similar to what is commonly observed in sedentary individuals (18%) [76]. Importantly, for individuals who complete these interventions, attendance rates of 75–90% are usually reported with 2–3 training sessions per week (Tables 3, 4) [13, 41, 77,78,79]. This should be considered relatively high, albeit illness severity and the presence of supervision from qualified personnel are shown to influence dropout and exercise adherence [16, 74]. Exact dropout and attendance rates for individuals with bipolar disorder are unclear due to a dearth of exercise interventions specifically targeting this patient group. With that caveat, when exercise is available as treatment, the data suggest that exercise interventions are generally well accepted and feasible in individuals with SMDs.
Endurance Training and Severe Mental Disorders
Moderate Aerobic Intensity
Although \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) is shown to be 1.5–3 METs lower in individuals with SMDs, there is promising evidence that endurance training may counteract the low values (Table 3). Applying pulmonary \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) measurements, Lin et al. [80] demonstrated that 12 weeks of moderate intensity (60–75% of peak heart rate) endurance treadmill training for 45–60 min, three times a week, resulted in improvements of 2.1 ml kg−1 min−1 in people with schizophrenia spectrum disorders. In contrast, using indirect \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) estimation, Scheewe et al. [81] reported no change in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) after 6 months of moderate intensity (45–75% of heart rate reserve) endurance training performed twice a week. The training intervention, however, may have counteracted a decline, as this was observed following control conditions. In individuals with major depressive disorder, 6 weeks of moderate intensity (50% of maximal workload) endurance training conducted for 45 min three times a week, improved pulmonary assessed \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) by 2.8 ml kg−1 min−1 [41]. The relatively larger improvement may relate to the particularly low fitness observed in the subjects (27.1 and 26.5 ml kg−1 min−1). Interestingly, individuals with a very low \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) (< ~30 ml kg-1 min−1) are primarily shown to be limited by working muscles’ ability to utilize oxygen during maximal effort, while this is suggested to not be the case for individuals with a somewhat higher \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) [82]. Thus, a very low initial \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) implies that individuals are more easily exposed to a training overload, have a larger potential for improvement, and that their training-induced adaptations may be governed by other physiological factors compared to less untrained counterparts.
High Aerobic Intensity
Similar to what has been observed in healthy individuals [53] and other patient populations [83, 84], endurance training with high aerobic intensity seems to yield greater increases in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) compared to endurance training with moderate aerobic intensity. In line with this notion, high-intensity aerobic interval training (4-min intervals at ~ 90% of peak heart rate with intermittent active rest periods) was demonstrated to increase pulmonary measured treadmill \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) by 3.1–4.2 ml kg−1 min−1 (~ 1 to 1.5 METs) in men and women with schizophrenia spectrum disorders [13, 85]. This rapid improvement toward normality has been documented after 24 training sessions following 8–12 weeks in in-patients with schizophrenia undergoing residential treatment as well as out-patients (Fig. 2). Similarly, in the same SMD population, 12 weeks of training with moderate-to-high aerobic intensity (60 to ≥ 90% of peak heart rate) performed for 45 min, three times a week, increased \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) by 3.1 ml kg−1 min−1 [79]. The high aerobic intensity-induced \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) improvements appear to be on par with increases of ~1 to 1.5 METs observed in other cohorts, such as patients with substance use disorder [86], coronary artery disease [83], and young adults [53]. Although one study failed to document aerobic interval training-induced improvement in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) with intention-to-treat analyses in people with schizophrenia [87], explorative ad hoc analyses revealed a \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) difference of 4.7 ml kg−1 min−1 after training between subjects instructed by personnel with (2.4 ml kg−1 min−1 increase) or without (2.2 ml kg−1 min−1 decrease) competence in supervising the sessions.
Individual values of peak oxygen uptake (l/min) pre- and post-12 weeks of aerobic interval training for the training groups with high adherence (A), low adherence (B) and controls (C). High adherence was set as completion of ≥ 70% of training sessions per protocol (n = 7) and low adherence as ≤ 70% of training sessions per protocol (n = 9). Values reported are mean and standard error. Used with permission from Brobakken et al. [13].
People with major depressive disorder also increased their \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) with ~ 1 MET, as estimated with a submaximal cycle test, after 10 weeks of interval training (16–17 on the Borg scale) [77]. Our literature search did not identify any prospective endurance training interventions specifically targeting individuals with bipolar disorder. However, a study by Romain et al. [17] documented that treadmill intervals with 30-s exercise bouts improved indirectly estimated \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) and was well accepted by a group of overweight individuals with psychosis in which bipolar disorder constituted 30% of the cohort.
Although high aerobic intensity training is typically applied to improve \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) in people with lifestyle-related illnesses, it is also shown to improve walking work efficiency by 12% (19.8–22.2%) in people with schizophrenia spectrum disorders, yielding a substantial reduction in oxygen cost of submaximal walking. This improvement has previously been observed in healthy adults [53] and heart failure patients [84], with work efficiency improvements of 10 and 15%, respectively, being reported. Few studies have previously documented the effects of endurance training on work efficiency in other cohorts with SMDs. Minghetti et al. [40] reported that heart rate during a submaximal oxygen uptake test tended to decrease (4%) following 12 weeks of sprint interval training in men and women with major depressive disorder, but without a concomitant change in oxygen uptake, which may relate to the different exercise and testing conditions applied, or to the efficacy of the training protocol in improving walking work efficiency specifically.
Collectively, the data suggest that while people with SMDs display reduced aerobic endurance, they may benefit greatly from the effects of endurance training. Endurance training with moderate aerobic intensity evidently may lead to important \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) increases in subjects with the lowest values; however, incorporating higher aerobic intensities appears to induce greater gains in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\).
Strength Training and Severe Mental Disorders
Moderate Intensity
The interest in offering individuals with SMDs strength training as part of clinical treatment is growing [11] and has promising results (Table 4). Most interventions have included people with schizophrenia spectrum disorders and moderate training intensities. Leone et al., including people with schizophrenia, showed that after 8 weeks of strength training at 50–80% of 1RM, leg and bench press 1RM increased by 25 (25%) and 16 kg (25%), respectively [88]. Moreover, Silva et al. [89] showed improvements in chest press (30 kg; 27%) and arm extension (46kg; 45%) 1RM in men with schizophrenia who partook in 20 weeks of multimodal lower and upper extremities strength training, twice weekly, at an intensity increasing gradually from 40 to 85% (2–3 sets of 6–15 repetitions). However, the subjects did not improve their performance in some of the other exercises involved in the program, indicating that the training load applied may have been too low or not well tolerated.
In older (60–80 years old) people with major depressive disorder, maximal strength increased by ~ 40% following 12 weeks of strength training twice weekly with moderate intensity (3 sets of 8–12 repetitions) in both lower and upper extremities exercises [90]. Although a direct comparison is challenging due to lack of absolute load per exercise being reported, this improvement appears to be on par with the 35% (24kg) increase in leg extension 1RM previously observed in young adults following conventional strength training with moderate intensity (3 sets of 10 repetitions) after 24 training sessions [91].
Our literature search failed to identify prospective strength training interventions targeting people with bipolar disorder specifically; thus, it is unclear if the results from other SMDs extend to this group. However, a pilot study of 7 individuals with mood disorders, predominantly consisting of bipolar disorder, showed increased 1RM by 19 (25%) and 6 kg (13%) in leg and bench press, respectively, after 8 weeks of strength training at 50–80% of 1RM performed to exhaustion [78]. This improvement was accompanied by 7 cm (37%) increased vertical jump performance. Further, in a mixed sample consisting of both people with schizophrenia spectrum disorders and bipolar disorder, Strassnig et al. [92] applied a moderate-intensity (3 sets of 10–12 repetitions) strength training protocol twice a week for 8 weeks, with emphasis on high intended velocity in the concentric phase, improving 1RM and power in exercises such as leg extension (1RM: 37 kg, 17%; power: 26%) and chest press (1RM: 9 kg, 19%; power: 13%).
High Intensity
Two studies in people with schizophrenia spectrum disorders have applied strength training with high intensity (4 sets of 4 repetitions at 90% of 1RM), referred to as maximal strength training (MST) in the studies. MST aims to improve muscle strength predominantly through neural adaptations by applying heavy loads and maximal intended velocity. However, an MST-induced increase in fast twitch muscle fiber area and percentage has also been documented [93]. One of the MST studies revealed that leg press 1RM increased by 83 kg (38%) in in-patients with schizophrenia [94], while the other study revealed an increase in leg press 1RM by 51 kg (29%) and power by 43 N m s−1 (20%) in out-patients with schizophrenia spectrum disorders [95]. Notably, in the latter study, subjects who performed ≥ 50% of the training sessions demonstrated normalization of both 1RM and power compared to healthy references after 24 sessions (Fig. 3) [95]. Similar increases in 1RM and power following MST have also been observed in, for example, patients with substance use disorders [96, 97], coronary artery disease [56], peripheral arterial disease [57], and young adults [91]. However, a significant caveat may be that the increase in muscle strength following MST was inversely associated (r = − 0.5) with defined daily dose of antipsychotic medication [95], suggesting that subjects undertaking greater doses may experience blunted ability to improve muscle force production with strength training.
12-Week effects of maximal strength training on scaled rapid force development and one-repetition maximum (1RM) in the per-protocol training group (TG; n = 17) and control group (CG; n = 19) compared to healthy references. Patients included in the per-protocol analyses completed ≥ 50% of the training sessions. Values are mean and standard error. ##P < .01 difference in change between groups, §§P < .01 difference from healthy references at 12 weeks. Used with permission from Nygård et al. [95].
In addition to improving muscle strength, strength training, similarly to the improvement observed after endurance training, has also shown its potential to mitigate reduced walking work efficiency present in these individuals. In fact, MST is shown to increase walking work efficiency by 20% (17.3–20.7%) in men and women with schizophrenia spectrum disorders [94]. In contrast, another study in people with schizophrenia reported no change in walking work efficiency following MST [95], which may be due to greater variance in walking disabilities and energy expenditure, causing less improvement. The effects of strength training on work efficiency have, to our knowledge, not been replicated in other cohorts with SMDs. However, studies in people with lifestyle-related illnesses, such as coronary artery disease [56], peripheral arterial disease [57], and healthy young adults [91], have reported similar reductions in oxygen cost of walking after MST, likely due to a shift in the motor unit recruitment spectrum and contraction cycle phase [93]. Taken together, the evidence suggests that individuals with SMDs experience the same plasticity in the neuromuscular system and that performing high-intensity strength training may improve walking work efficiency.
Considering effect sizes, the same seems to apply for strength training as for endurance training; important improvements in 1RM and power are expected following training with moderate intensity in individuals with the poorest starting point. However, strength training which applies higher intensities appears to improve skeletal muscle strength more. The importance of high intensity is also highlighted in a current meta-review regarding exercise as treatment for individuals with SMDs [11]. If strength training is to be offered as part of treatment for people with SMDs, applying the most efficacious training regime in standard clinical practice should be considered.
Safety Considerations
For endurance and strength training to be delivered as, or in conjunction with, standard clinical care, and act as effective countermeasures to poor physical health, the treatment must be considered safe. Notably, endurance and strength training, also with high intensities, are prescribed at a lower relative intensity than a subject’s maximal physical capacity. In individuals with low \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\), such as individuals with SMDs, this typically results in the treadmill endurance training being performed at uphill walking pace, generally considered to be a strenuous activity at high aerobic intensity but with low impact on the lower extremities [98]. For strength training, although the eccentric action phase may produce higher forces, maximal force is produced during the concentric phase, yet both lifting phases are performed in a slow and controlled manner due to heavy external loads, reducing risk of muscle injuries [93, 99]. Furthermore, given that these training regimes have been applied in other populations arguably frailer, such as heart patients [98], peripheral arterial disease patients [100, 101], old adults [93], hip fracture patients [102], and osteoporotic women [103], they should be considered safe also for individuals with SMDs [104].
Endurance and Strength Training: Implications for Physical Function, CVD Risk, and Early Death
Increased aerobic endurance and/or skeletal muscle strength following training should result in improved physical function in individuals with SMDs. Indeed, a combination of high-intensity aerobic endurance training and MST did improve \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\), 1RM, and power along with chair-raising performance (14%) in people with schizophrenia spectrum disorders [13, 95]. Although the improvement in this functional performance test was strongly related (r = 0.6) to the increase in power [95], it was not apparent as an intergroup difference with no further improvements observed in walking or stair climbing performance. This is in contrast with what is typically observed in older adults [25], and indicates that the interplay between these factors may be influenced by illness-specific factors such as antipsychotics or sedation [105]. Two previous studies which applied aerobic endurance and strength training along with functional performance exercises in people with schizophrenia spectrum [88] and mood disorders [78] documented improved estimated \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\), 1RM, and power, as well as chair-raising (~ 20 to 25%) and stair climbing (~ 40%) performance. Although aerobic endurance and muscle strength are, in of themselves, measures of physical function, specific training as add-on treatment may be warranted for additional improvements in typical activities of daily living.
Given that \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) and muscle strength are independently related to CVD and all-cause mortality, it is encouraging that physical training, particularly applying high intensities, elicits adaptations similar to previous observations in healthy adults and lifestyle-related illnesses. Notably, a 1 MET increase in \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\) as observed following endurance training is associated with reduced risk of all-cause mortality by 12% and CVD by 13–15% [24, 35]. Further, comparing terciles in maximal muscle strength, being in the middle–upper strength cohort is associated with 20–26% less risk of early death from all causes [58], underlining the importance of applying efficacious training regimes for individuals with SMDs who display reduced life expectancy from physical comorbidity.
Conclusions and Perspectives
Recognizing the paradox that recommendations of physical activity in clinical treatment of people with SMDs do not result in increased life expectancy and reduced prevalence of CVD, a closer look at training interventions that have returned effective results is needed. In conclusion, the current review confirms that key physiological factors for health and longevity like \({\dot{\text{V}}}{\text{O}}_{{2{\text{peak}}}}\), walking work efficiency, maximal skeletal muscle strength and power, are reduced in individuals with SMDs. However, effective training interventions, ensuring sufficient overload on factors involved in oxygen transport and skeletal muscle force production, are demonstrated to counteract this reduction. Particularly, promising results appear to be evident after interventions incorporating higher training intensities. Compliance rates following such interventions are also high. Of notable concern, our literature search failed to identify prospective clinical trials with physical training specifically targeting people with bipolar disorder. Integrating effective training as part of standard clinical practice not only seems feasible and well accepted by people with SMDs yielding relatively low attrition, but may also improve physical function, cardiovascular health, and ultimately life expectancy.
Physical training is a well-acknowledged, feasible, and efficacious countermeasure to improve the low aerobic endurance and skeletal muscle strength observed in individuals with SMDs, factors directly associated with all-cause mortality. It is therefore concerning that it is rarely integrated, or delivered as adjunctive treatment, in standard clinical care for these patient groups. Variation in rates and causes for dropout from exercise interventions between diagnostic groups of SMDs suggest that a patient-centered tailored approach, optimally involving primary and secondary healthcare services [106] or strategies to promote autonomous motivation [107], may facilitate treatment adherence. This comprehensive support may be considered resource demanding; however, SMDs are associated with substantial societal cost due to the often-required extensive healthcare services from an early age. It is time to improve clinical practice to include effective physical training. Considering the increased mortality and poor somatic health of people with SMDs, it could be regarded unethical not to do so as it has the potential to improve key factors for health and longevity without detrimental side effects. Structured physical training may not only be beneficial for the individuals and their families but may also help reduce dependence on healthcare services.
Availability of Data and Materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Merikangas KR, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Archiv General Psychiatry. 2011. https://doi.org/10.1001/archgenpsychiatry.2011.12.
Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168.
McGrath J, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008. https://doi.org/10.1093/epirev/mxn001.
Andrade L, et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatric Res. 2003. https://doi.org/10.1002/mpr.138.
Crump C, et al. Comorbidities and mortality in bipolar disorder: a Swedish national cohort study. JAMA psychiatry. 2013. https://doi.org/10.1001/jamapsychiatry.2013.1394.
Crump C, et al. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry. 2013. https://doi.org/10.1176/appi.ajp.2012.12050599.
Laursen TM, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0067133n.
Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects. CNS drugs. 2005. https://doi.org/10.2165/00023210-200519001-00001.
Paton C, et al. Obesity, dyslipidaemias and smoking in an inpatient population treated with antipsychotic drugs. Acta Psychiatr Scand. 2004. https://doi.org/10.1111/j.1600-0447.2004.00372.x.
Lee I-M, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet. 2012. https://doi.org/10.1016/S0140-6736(12)61031-9.
Stubbs B, et al. EPA guidance on physical activity as a treatment for severe mental illness: a meta-review of the evidence and Position Statement from the European Psychiatric Association (EPA), supported by the International Organization of Physical Therapists in Mental Health (IOPTMH). Eur Psychiatry. 2018. https://doi.org/10.1016/j.eurpsy.2018.07.004.
Vancampfort D, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017. https://doi.org/10.1002/wps.20458.
Brobakken MF, et al. Aerobic interval training in standard treatment of out-patients with schizophrenia: a randomized controlled trial. Acta Psychiatr Scand. 2019. https://doi.org/10.1111/acps.13105.
Schuch FB, et al. Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J Psychiatric Res. 2015. https://doi.org/10.1016/j.jpsychires.2014.11.005.
Deenik J, et al. Implementation barriers and facilitators of an integrated multidisciplinary lifestyle enhancing treatment for inpatients with severe mental illness: the MULTI study IV. BMC Health Serv Res. 2019. https://doi.org/10.1186/s12913-019-4608-x.
Vancampfort D, et al. Prevalence and predictors of treatment dropout from physical activity interventions in schizophrenia: a meta-analysis. Gen Hosp Psychiatry. 2016. https://doi.org/10.1016/j.genhosppsych.2015.11.008.
Romain AJ, et al. Effects of high intensity interval training among overweight individuals with psychotic disorders: a randomized controlled trial. Schizophr Res. 2019. https://doi.org/10.1016/j.schres.2018.12.021.
Richardson CR, et al. Integrating physical activity into mental health services for persons with serious mental illness. Psychiatric Serv. 2005. https://doi.org/10.1176/appi.ps.56.3.324.
Laursen TM, et al. Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J Clin Psychiatry. 2007. https://doi.org/10.4088/jcp.v68n0612.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007. https://doi.org/10.1001/archpsyc.64.10.1123.
De Hert M, et al. Physical illness in patients with severe mental disorders: I—prevalence, impact of medications and disparities in health care. World Psychiatry. 2011. https://doi.org/10.1002/j.2051-5545.2011.tb00014.x.
Sokal J, et al. Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. J Nerv Mental Dis. 2004. https://doi.org/10.1097/01.nmd.0000130135.78017.96.
Vancampfort D, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015. https://doi.org/10.1002/wps.20252.
Myers J, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002. https://doi.org/10.1056/NEJMoa011858.
Aagaard P, et al. Role of the nervous system in sarcopenia and muscle atrophy with aging: strength training as a countermeasure. Scand J Med Sci Sports. 2010. https://doi.org/10.1111/j.1600-0838.2009.01084.x.
Åstrand PO, et al. Textbook of work physiology. Champaign, USA: Human Kinetics; 2003. p. 313–68.
McDonagh MJ, Davies CT. Adaptive response of mammalian skeletal muscle to exercise with high loads. Eur J Appl Physiol Occup Physiol. 1984;52(2):139–55.
Pate RR, Kriska A. Physiological basis of the sex difference in cardiorespiratory endurance. Sports Med. 1984. https://doi.org/10.2165/00007256-198401020-00001.
Wiswell RA, et al. Maximal aerobic power, lactate threshold, and running performance in master athletes. Med Sci Sports Exercise. 2000. https://doi.org/10.1097/00005768-200006000-00021.
Wagner PD. An integrated view of the determinants of maximum oxygen uptake. 1988; https://doi.org/10.1007/978-1-4684-5481-9_22.
Wagner PD. New ideas on limitations to VO2max. Exercise Sport Sci Rev. 2000;28(1):10–4.
Wang E, et al. Stroke volume does not plateau in female endurance athletes. Int J Sports Med. 2012;33(9):734–9.
Poole DC, Jones AM. Measurement of the maximum oxygen uptake Vo2max: Vo2peak is no longer acceptable. J Appl Physiol. 2017. https://doi.org/10.1152/japplphysiol.01063.2016.
Fick A. About the measurement of blood quantum in the ventricles of the heart. Physiomed Soc Wurzung. 1870;2:16–7.
Kodama S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009. https://doi.org/10.1001/jama.2009.681.
Ross R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016. https://doi.org/10.1161/CIR.0000000000000461.
Edvardsen E, et al. Reference values for cardiorespiratory response and fitness on the treadmill in a 20- to 85-year-old population. Chest. 2013. https://doi.org/10.1378/chest.12-1458.
Brobakken MF, et al. A comprehensive cardiovascular disease risk profile in patients with schizophrenia. Scand J Med Sci Sports. 2019. https://doi.org/10.1111/sms.13371.
Andersen E, et al. Physical activity pattern and cardiorespiratory fitness in individuals with schizophrenia compared with a population-based sample. Schizophr Res. 2018. https://doi.org/10.1016/j.schres.2018.05.038.
Minghetti A, et al. Sprint interval training (SIT) substantially reduces depressive symptoms in major depressive disorder (MDD): a randomized controlled trial. Psychiatry Res. 2018. https://doi.org/10.1016/j.psychres.2018.04.053.
Kerling A, et al. Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord. 2015. https://doi.org/10.1016/j.jad.2015.01.006.
Boettger S, et al. Physical fitness and heart rate recovery are decreased in major depressive disorder. Psychosom Med. 2009. https://doi.org/10.1097/PSY.0b013e3181a55303.
Donath L, et al. Ventilatory inefficiency in major depressive disorder: a potential adjunct for cardiac risk stratification in depressive disorders? Progress Neuro-Psychopharmacol Biol Psychiatry. 2010. https://doi.org/10.1016/j.pnpbp.2010.04.007.
Schuch FB, et al. Effects of a single bout of maximal aerobic exercise on BDNF in bipolar disorder: a gender-based response. Psychiatry Res. 2015. https://doi.org/10.1016/j.psychres.2015.07.072.
Vancampfort D, et al. Cardiorespiratory fitness in outpatients with bipolar disorder versus matched controls: an exploratory study. J Affect Disord. 2016. https://doi.org/10.1016/j.jad.2016.03.057.
Hermansen L, Saltin B. Oxygen uptake during maximal treadmill and bicycle exercise. J Appl Physiol. 1969. https://doi.org/10.1152/jappl.1969.26.1.31.
Dyrstad SM, et al. Cardiorespiratory fitness in groups with different physical activity levels. Scand J Med Sci Sports. 2016. https://doi.org/10.1111/sms.12425.
Vancampfort D, et al. Cardiorespiratory fitness in severe mental illness: a systematic review and meta-analysis. Sports Med. 2017. https://doi.org/10.1007/s40279-016-0574-1.
Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973. https://doi.org/10.1016/0002-8703(73)90502-4.
Kaminsky LA, Whaley MH. Evaluation of a new standardized ramp protocol: the BSU/Bruce Ramp protocol. J Cardiopulm Rehabil Prev. 1998. https://doi.org/10.1097/00008483-199811000-00006.
Helgerud J. Maximal oxygen uptake, anaerobic threshold and running economy in women and men with similar performances level in marathons. Eur J Appl Physiol Occup Physiol. 1994. https://doi.org/10.1007/BF00244029.
Åstrand PO, Rodahl K, Dahl HA, Strømme SB. Evaluation of physical performance on the basis of tests. In: Textbook of work physiology. Champaign: Human Kinetics; 2003. p. 273–98.
Helgerud J, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007. https://doi.org/10.1249/mss.0b013e3180304570.
Nygard M, et al. Patients with schizophrenia have impaired muscle force-generating capacity and functional performance. Scand J Med Sci Sports. 2019. https://doi.org/10.1111/sms.13526.
Flemmen G, Wang E. Impaired aerobic endurance and muscular strength in substance use disorder patients: implications for health and premature death. Medicine (Baltimore). 2015. https://doi.org/10.1097/md.0000000000001914.
Karlsen T, et al. Maximal strength training restores walking mechanical efficiency in heart patients. Int J Sports Med. 2009. https://doi.org/10.1055/s-0028-1105946.
Wang E, et al. Maximal strength training improves walking performance in peripheral arterial disease patients. Scand J Med Sci Sports. 2010. https://doi.org/10.1111/j.1600-0838.2009.01014.x.
Ruiz JR, et al. Association between muscular strength and mortality in men: prospective cohort study. BMJ. 2008. https://doi.org/10.1136/bmj.a439.
Ortega FB, et al. Muscular strength in male adolescents and premature death: cohort study of one million participants. BMJ. 2012. https://doi.org/10.1136/bmj.e7279.
Metter EJ, et al. Arm-cranking muscle power and arm isometric muscle strength are independent predictors of all-cause mortality in men. J Appl Physiol. 2004. https://doi.org/10.1152/japplphysiol.00370.2003.
Lindle RS, et al. Age and gender comparisons of muscle strength in 654 women and men aged 20–93 yr. J Appl Physiol. 1997. https://doi.org/10.1152/jappl.1997.83.5.1581.
Reid KF, et al. Longitudinal decline of lower extremity muscle power in healthy and mobility-limited older adults: influence of muscle mass, strength, composition, neuromuscular activation and single fiber contractile properties. Eur J Appl Physiol. 2014. https://doi.org/10.1007/s00421-013-2728-2.
Byrne C, et al. Ageing, muscle power and physical function: a systematic review and implications for pragmatic training interventions. Sports Medicine. 2016. https://doi.org/10.1007/s40279-016-0489-x.
Bader J, et al. Muscle strength and gait patterns of depressed people. Der Nervenarzt. 1999. https://doi.org/10.1007/s001150050486.
Vancampfort D, et al. A comparison of physical fitness in patients with bipolar disorder, schizophrenia and healthy controls. Disabil Rehabil. 2016. https://doi.org/10.3109/09638288.2015.1114037.
Vancampfort D, et al. Health-related physical fitness in patients with bipolar disorder vs healthy controls: an exploratory study. J Affect Disord. 2015. https://doi.org/10.1016/j.jad.2014.12.058.
Lawrie SM, et al. The difference in patterns of motor and cognitive function in chronic fatigue syndrome and severe depressive illness. Psychol Med. 2000. https://doi.org/10.1017/s0033291799001816.
Mosti MP, et al. Impaired skeletal health and neuromuscular function among amphetamine users in clinical treatment. Osteoporos Int. 2016;27(3):1003–10.
Åstrand PO, Rodahl K, Dahl HA, Strømme SB. Body dimensions and muscular exercise. In: Textbook of work physiology. Champaign: Human Kinetics; 2003. p. 299–312.
Zechner MR, Anderson EZ, Gill KJ. Old before their time: comparisons of people with SMI and healthy older adults. Psychiatr Rehabil J. 2021. https://doi.org/10.1037/prj0000496.
Vancampfort D, et al. The functional exercise capacity in patients with bipolar disorder versus healthy controls: a pilot study. Psychiatry Res. 2015. https://doi.org/10.1016/j.psychres.2015.07.040.
Vancampfort D, et al. Depressive symptoms and muscular fitness contribute independently to the ability to perform daily life activities in people with bipolar disorder. Nord J Psychiatry. 2016. https://doi.org/10.3109/08039488.2016.1161072.
Åstrand PO, Rodahl K, Dahl HA, Strømme SB. Physical training. In: Textbook of work physiology. Champaign: Human Kinetics; 2003. p. 313–68.
Stubbs B, et al. Dropout from exercise randomized controlled trials among people with depression: a meta-analysis and meta regression. J Affect Disord. 2016. https://doi.org/10.1016/j.jad.2015.10.019.
Sylvia LG, et al. Feasibility and acceptability of a lifestyle intervention for individuals with bipolar disorder. J Psychiatric Pract. 2019. https://doi.org/10.1097/PRA.0000000000000426.
Reljic D, et al. Prevalence and predictors of dropout from high-intensity interval training in sedentary individuals: a meta-analysis. Scand J Med Sci Sports. 2019. https://doi.org/10.1111/sms.13452.
Danielsson L, et al. Exercise or basic body awareness therapy as add-on treatment for major depression: a controlled study. J Affect Disord. 2014. https://doi.org/10.1016/j.jad.2014.06.049.
Leone M, et al. Effects of an exercise program on the physiological, biological and psychological profiles in patients with mood disorders: a pilot study. Int J Psychiatry Clin Pract. 2018. https://doi.org/10.1080/13651501.2018.1425458.
Kimhy D, et al. The impact of aerobic exercise on brain-derived neurotrophic factor and neurocognition in individuals with schizophrenia: a single-blind. Randomized clin trial. Schizophr Bull. 2015. https://doi.org/10.1093/schbul/sbv022.
Lin J, et al. Aerobic exercise and yoga improve neurocognitive function in women with early psychosis. NPJ Schizophr. 2015. https://doi.org/10.1038/npjschz.2015.47.
Scheewe TW, et al. Exercise therapy, cardiorespiratory fitness and their effect on brain volumes: a randomised controlled trial in patients with schizophrenia and healthy controls. Eur Neuropsychopharmacol. 2013. https://doi.org/10.1016/j.euroneuro.2012.08.008.
Gifford JR, et al. Symmorphosis and skeletal muscle V̇O2 max : in vivo and in vitro measures reveal differing constraints in the exercise-trained and untrained human. J Physiol. 2016. https://doi.org/10.1113/jp271229.
Rognmo Ø, et al. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004. https://doi.org/10.1097/01.hjr.0000131677.96762.0c.
Wisløff U, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007. https://doi.org/10.1161/circulationaha.106.675041.
Heggelund J, et al. Effects of high aerobic intensity training in patients with schizophrenia: a controlled trial. Nord J Psychiatry. 2011. https://doi.org/10.3109/08039488.2011.560278.
Flemmen G, Unhjem R, Wang E. High-intensity interval training in patients with substance use disorder. Biomed Res Int. 2014. https://doi.org/10.1155/2014/616935.
Andersen E, et al. Effect of high-intensity interval training on cardiorespiratory fitness, physical activity and body composition in people with schizophrenia: a randomized controlled trial. BMC Psychiatry. 2020. https://doi.org/10.1186/s12888-020-02827-2.
Leone M, et al. Impact of an exercise program on the physiologic, biologic and psychologic profiles in patients with schizophrenia. Schizophr Res. 2015. https://doi.org/10.1016/j.schres.2015.03.002.
Silva BA, et al. A 20-week program of resistance or concurrent exercise improves symptoms of schizophrenia: results of a blind, randomized controlled trial. Rev Bras Psiquiatr. 2015. https://doi.org/10.1590/1516-4446-2014-1595.
Moraes HS, et al. Is strength training as effective as aerobic training for depression in older adults? A randomized controlled trial. Neuropsychobiology. 2020. https://doi.org/10.1159/000503750.
Heggelund J, et al. Maximal strength training improves work economy, rate of force development and maximal strength more than conventional strength training. Eur J Appl Physiol. 2013. https://doi.org/10.1007/s00421-013-2586-y.
Strassnig MT, et al. High velocity circuit resistance training improves cognition, psychiatric symptoms and neuromuscular performance in overweight outpatients with severe mental illness. Psychiatry Res. 2015. https://doi.org/10.1016/j.psychres.2015.07.007.
Wang E, et al. Impact of maximal strength training on work efficiency and muscle fiber type in the elderly: Implications for physical function and fall prevention. Exp Gerontol. 2017. https://doi.org/10.1016/j.exger.2017.02.071.
Heggelund J, et al. Therapeutic effects of maximal strength training on walking efficiency in patients with schizophrenia—a pilot study. BMC Res Notes. 2012. https://doi.org/10.1186/1756-0500-5-344.
Nygård M, et al. Strength training restores force-generating capacity in patients with schizophrenia. Scand J Med Sci Sports. 2021. https://doi.org/10.1111/sms.13863.
Unhjem R, et al. Maximal strength training as physical rehabilitation for patients with substance use disorder; a randomized controlled trial. BMC Sports Sci Med Rehabil. 2016;8:7.
Nygard M, et al. Maximal strength training improves musculoskeletal health in amphetamine users in clinical treatment. Osteoporos Int. 2018;29(10):2289–98.
Helgerud J, et al. Interval and strength training in CAD patients. Int J Sports Med. 2011. https://doi.org/10.1055/s-0030-1267180.
Helgerud J, et al. Maximal strength training in patients with Parkinson’s disease: impact on efferent neural drive, force-generating capacity, and functional performance. J Appl Physiol. 2020. https://doi.org/10.1152/japplphysiol.00208.2020.
Helgerud J, et al. Plantar flexion training primes peripheral arterial disease patients for improvements in cardiac function. Eur J Appl Physiol. 2009;106(2):207–15.
Mosti MP, et al. Concurrent strength and endurance training improves physical capacity in patients with peripheral arterial disease. Scand J Med Sci Sports. 2011;21(6):e308-14.
Berg OK, et al. Early maximal strength training improves leg strength and postural stability in elderly following hip fracture surgery. Geriatr Orthop Surg Rehabil. 2021;12:21514593211015104.
Mosti MP, et al. Maximal strength training in postmenopausal women with osteoporosis or osteopenia. J Strength Cond Res. 2013. https://doi.org/10.1519/JSC.0b013e318280d4e2.
Martland R, et al. Can high-intensity interval training improve physical and mental health outcomes? A meta-review of 33 systematic reviews across the lifespan. J Sports Sci. 2020. https://doi.org/10.1080/02640414.2019.1706829.
Kirschner M, Aleman A, Kaiser S. Secondary negative symptoms—a review of mechanisms, assessment and treatment. Schizophr Res. 2017. https://doi.org/10.1016/j.schres.2016.05.003.
Brobakken MF, et al. One-year aerobic interval training in outpatients with schizophrenia: a randomized controlled trial. Scand J Med Sci Sports. 2020. https://doi.org/10.1111/sms.13808.
Vancampfort D, et al. The importance of self-determined motivation towards physical activity in patients with schizophrenia. Psychiatry Res. 2013. https://doi.org/10.1016/j.psychres.2013.10.004.
Acknowledgements
The authors would like to thank all participants included in the studies and the contribution of colleagues without whom the completion of this work would be impossible.
Funding
Open access funding provided by Norwegian University of Science and Technology.
Author information
Authors and Affiliations
Contributions
MFB and EW developed the concept for the manuscript; MFB and MN both independently searched the literature; MFB, MN, and EW analyzed the available data; all authors contributed substantially to the draft and critically revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable
Consent for Publication
Not applicable
Competing interests
Mathias Forsberg Brobakken, Mona Nygård and Eivind Wang declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brobakken, M.F., Nygård, M. & Wang, E. Physical Health Impairment and Exercise as Medicine in Severe Mental Disorders: A Narrative Review. Sports Med - Open 8, 115 (2022). https://doi.org/10.1186/s40798-022-00490-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-022-00490-3