Abstract
Background
Hip fractures in older adults are significant contributors to severe functional decline and disability as well as hospitalization and increased health care costs. Research shows that timely referral to geriatric rehabilitation leads to better patient outcomes. Currently, a wide variability in the timing, the frequency, and the choice of appropriate setting for rehabilitation of hip fracture patients exists.
Aim
Evaluate the feasibility, acceptability, and preliminary effectiveness of PATH4HIP, a pathway intervention for timely transfer of post-operative geriatric hip fracture patients from hospital to rehabilitation to home.
Methods
This is a single-arm, pragmatic feasibility study to measure reach, effectiveness, adoption, implementation, and maintenance of PATH4HIP, a pathway for post-operative hip fracture patients from a large academic health science center to a geriatric rehabilitation service in Ottawa, Canada. During a 6-month period, all hip fracture patients, 65 years of age or older who have undergone surgery and have met the eligibility criteria (n = 96), will be transferred to the geriatric rehabilitation service no later than post-operative day 6. Patients (n = 10–12) and clinicians who are working on the orthopedic team (n = 10–12) and on the geriatric rehabilitation service (n = 10–12) will be invited to participate in an interview to share their feedback on the intervention’s feasibility and acceptability and to provide suggestions to improve PATH4HIP. Descriptive statistics will be used to summarize results of the quantitative data and content analysis will be used to analyze the qualitative data. The study will be open for recruitment from January to July 2022.
Discussion
If feasible, PATH4HIP will result in the reduction of the post-operative acute care length of stay to less than or equal to 6 days, while having no detrimental effect on rehabilitation outcomes such as functional gains, or discharge destination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Hip fractures in older adults are significant contributors to severe functional decline and disability as well as hospitalization and increased health care costs [1,2,3,4]. In Canada, approximately 30,000 hip fractures occur annually with one hip fracture currently costing on average $37,500 in 1-year costs across multiple sectors [5]. These health care costs have been reported as comparable to those of other countries [6,7,8].
Best practice guidelines recommend standardized processes, including early post-operative mobilization [1, 9,10,11]. Specifically, hospital care pathways should adopt the goal of active rehabilitation starting no later than 6 days after the patient’s surgery [1]. Inpatient geriatric rehabilitation is considered the gold standard and represents a critical component of post-operative hip fracture care when striving to maximize functional recovery [12]. Geriatric rehabilitation involves a multidisciplinary set of evaluative, diagnostic, and therapeutic interventions with the aim of restoring functional ability and enhancing residual functional capability in elderly individuals with disabling impairments [13, 14]. One systematic review of 17 trials (n = 4780) demonstrated that inpatient rehabilitation specifically targeted at geriatric patients improved outcomes related to function, improved outcomes related to admission to nursing homes, and decreased mortality rates [15]. Furthermore, another study found that geriatric hip fracture programs were associated with savings from the perspective of health and social services and were more effective than usual care in reducing length of stay, improving function, and increasing the rate of returning home after discharge [16]. Studies have also demonstrated shortened acute care length of stay without compromising rehabilitation outcomes for hip fracture patients [17,18,19,20,21,22].
Despite this, many hospitals are still facing challenges in meeting these targets. Evidence suggests that delays to the start of rehabilitation exist as well as a wide variability in timing, frequency, and choice of appropriate setting for rehabilitation [2]. The purpose of our study is to pilot PATH4HIP, a pathway intervention for timely transfer of post-operative geriatric hip fracture patients from hospital to rehabilitation to home. Our specific objectives include to (1) determine the feasibility and acceptability of the PATH4HIP intervention; (2) evaluate PATH4HIP’s preliminary effects on acute and rehabilitation length of stay, functional gains in rehabilitation, and discharge destination; and (3) refine methods in preparation for a larger trial.
Methods
This study is approved by the Ottawa Health Science Network Research Ethics Board (#20180469-01H), the Bruyère Research Ethics Board (#M16-18-036), and the University of Ottawa Research Ethics Board (#H-08-18-1061). The protocol is formulated in accordance with the SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement (see Additional file 1) [23] (Fig. 1). This protocol is version 3.0, dated of January 4, 2022. The study is scheduled to open for recruitment in January 2022.
Study design and setting
This is a single-arm, pragmatic feasibility study using the RE-AIM framework [24] to measure REACH (how to reach the intended population), EFFECTIVENESS (how to tell if the intervention is effective), ADOPTION (how to develop organizational support to deliver the intervention), IMPLEMENTATION (how to ensure the intervention is delivered properly), and MAINTENANCE (how to incorporate the delivery long-term).
The study will take place in a large academic health science center and on a geriatric rehabilitation service of a complex continuing care organization in Ottawa, Ontario, Canada.
Intervention
The intervention is described using the Template for Intervention Description and Replication (TIDieR) guidelines [25]. PATH4HIP, the pathway for timely referral of geriatric hip fracture patients to rehabilitation, adheres to the best practice guidelines that mandate that all hip fractures require rehabilitation [1, 9,10,11]. All patients who meet the defined eligibility criteria will be accepted and transferred to geriatric rehabilitation no later than post-operative day 6. PATH4HIP is an approach to help identify, prioritize, and refer geriatric hip fracture patients and consists of four steps: Step 1: Identify eligible patients and obtain consent; Step 2: Provide patient and family teaching; Step 3: Determine readiness for transfer; and Step 4: Finalize logistics for transfer. Figure 2 is a basic visual representation of the PATH4HIP steps.
The roles of each team member during the post-operative days 1–5 are defined as follows:
Step 1—Identify eligible patients and obtain consent
Post-operative days 0–1
A senior nurse or delegate will review the daily census through the electronic chart data report and will identify patients that meet the preliminary inclusion criteria. The hospitalist will also support in identifying eligible patients. The orthopedic resident will determine weight bearing status and range of motion restrictions post-surgery. The senior nurse will confirm patient consent for rehabilitation and will initiate the referral to the subacute team. A geriatric rehabilitation physician will be available to answer questions regarding eligibility and medical stability.
Post-operative days 1–3
Nurses will communicate the patient status for eligibility at daily discharge rounds. Physiotherapy will collaborate with the team to establish baseline ambulation and to facilitate the patient consent process. The subacute consult assessor will verify that the patient meets the inclusion criteria. The clinical admission coordinator at the geriatric rehabilitation service will liaise with the subacute team to obtain the status of eligible patients.
Step 2—Provide patient and family teaching
Post-operative days 1–3
Clinical nurses will provide the PATH4HIP patient and family education materials (e.g., pamphlet and video) and will document in the patient’s chart once completed. The subacute consult assessor will meet with the eligible patient and will explain the geriatric rehabilitation program in more detail.
Post-operative days 3–5
The clinical team will reinforce rehabilitation best practices and answer questions from patients and families. The orthopedic resident will support the team’s recommendations for the patient and for the family regarding appropriate rehabilitation needs.
Step 3—Determine readiness for transfer
Post-operative days 2–5
The senior nurse will communicate with members of the team at discharge rounds regarding readiness for transfer. Clinical nurses will update the patient status (delirium, wound, pain, etc.) at discharge rounds. The physiotherapist will provide an update on the patient’s mobility status at discharge rounds. The hospitalist will evaluate each patient daily for delirium and medical stability to promptly address any issues. The hospitalist will also provide feedback to the team regarding the medical stability of the patient. The orthopedic resident will monitor patients for surgical post-op complications.
Step 4—Finalize logistics for transfer
Post-operative days 3–5
The subacute consult assessor will complete the rehabilitation referral and will flag priority for the geriatric rehabilitation admission team. The senior nurse will communicate with the clinical admission coordinator in the geriatric rehabilitation program. The senior nurse will also communicate with the clerk to book the transport to geriatric rehabilitation. The manager of patient flow in geriatric rehabilitation will make themselves available should any challenges need to be addressed.
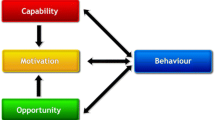
The implementation strategy, informed by behavioral change techniques [26] from our previous barriers and enablers’ analysis [27], consists of flags in the clinical pathway, standardized transfer of information, high-risk delirium screening, dashboard to provide immediate feedback to clinicians, patient information, multidisciplinary workshops, and reminders and sustained site engagement. Further information about the implementation strategy is described in Table 1.
Sample size
The primary outcome is to estimate feasibility, which will be determined by study adherence. In this proposed 6-month study, we expect a total sample of 96 participants (16 eligible individuals per month × 6 months). With a sample size of 96 participants, proportion of 75% of eligible participants who are transferred to geriatric rehabilitation by post-operative day 6 could be estimated to within a 95% confidence interval of ± 8.7% [28,29,30,31].
Eligibility
The inclusion criteria are as follows: patients (1) aged 65 and older with a unilateral hip fracture, (2) anticipated discharge to community, (3) post-operative hemoglobin greater than 70 g per liter, (4) consult services signed off for acute medical issues, and (5) pre-fracture ambulating independently with or without gait aid. The exclusion criteria are as follows: (1) pathologic fracture, metastatic cancer diagnosis, (2) on dialysis, chemotherapy, and/or radiation treatment, (3) living in long-term care, and (4) acute agitated delirium.
Data collection
The study of the use of PATH4HIP will have three stages: (1) introductory stage, (2) 6-month of PATH4HIP use, and (3) qualitative and quantitative evaluation.
-
(1)
Introductory stage
All clinicians who are working on the orthopedic unit and on the geriatric rehabilitation service will be invited to attend multidisciplinary workshops to introduce PATH4HIP. The research assistant will track all clinicians approached and clinician attendance. Following the workshops, participants will be asked to complete a survey including sociodemographic information (age, gender, professional role, clinical unit, and years in practice), their opinion on the intervention, and any feedback that could be used to improve PATH4HIP.
-
(2)
Six-month of PATH4HIP use
A daily census list of all potential hip fracture patients will be generated. The unit manager (or a senior nurse) and a subacute care assessor on the orthopedic unit will apply the PATH4HIP eligibility criteria. Patients who are eligible will be enrolled in PATH4HIP. A trained research assistant will track all patients who are included, all patients who are excluded, including the reasons for exclusion, and all patients who refuse to go to geriatric rehabilitation along with their reasons for refusal. The research assistant will also track the adherence to all steps of PATH4HIP, the reasons for any non-adherence, and the completion status of PATH4HIP.
-
(3)
Qualitative and quantitative evaluation
Prior to discharge from geriatric rehabilitation, the research assistant will obtain informed consent and conduct 60-min audio recorded semi-structured interviews with patients (n = 10–12) in person or by video call to gather their opinion and to gather specific information on what can be improved to enhance their experience. Clinicians who are working on the orthopedic team (n = 10–12) and on the geriatric rehabilitation service (n = 10–12) will be invited to participate in an audio-recorded 30–45-min interview to share their feedback on the intervention’s feasibility and acceptability and to provide suggestions to improve PATH4HIP.
Using administrative databases, we will collect the following information for all unilateral hip fracture patients during the study period to compare participants and non-participants: age, gender, ethnicity, relationship status, living situation, Elixhauser score, comorbidities, total acute length of stay, post-surgery length of stay, discharge destination, return to the emergency department (30 days), readmissions (90 days), geriatric rehabilitation length of stay, functional gains, and discharge destination post geriatric rehabilitation.
Outcomes
Evaluation will be based on feasibility, acceptability, and preliminary effects following the RE-AIM framework [24] as follows:
REACH: proportion of individuals who participate, proportion of excluded patients, proportion of patient refusals, reason for excluded patients and refusals, proportion of clinicians approached to participate in the workshops, proportion of clinicians who attended the workshops, and clinicians’ opinion on the intervention following the workshops
EFFECTIVENESS: acute care and rehabilitation length of stays (median), % discharged back to community, % transfer back to acute care and reason, and proportion of functional gains in rehabilitation. The Functional Independence Measure (FIM) [32] will be used to calculate the difference between the patients’ functional status at rehabilitation admission and discharge. The FIM is a disability measure that consists of 18 items each rated on a scale of 1 (most dependent) to 7 (most independent) according to the degree of assistance required to perform a specific activity in six domains: self-care, sphincter control, mobility, locomotion, communication, and social cognition. The total FIM score ranges from 18 to 126. The FIM consists of two major criteria, the motor FIM (score 13–91), and cognitive FIM (score 5–35) [32]
ADOPTION: proportion of patients that completed PATH4HIP
IMPLEMENTATION: proportion of hip fracture geriatric patients referred from acute care to geriatric rehabilitation, proportion of patients who are discharged by post-op day 6, proportion of patients where intervention was delivered as per the study protocol, reasons for any deviations, adaptations made to intervention during study, and average cost of intervention (time and money)
MAINTENANCE: patients’ opinions on the intervention: ease of use of the patient information, relevance of information, follow-up with clinicians including their opinion of the content and its relevance, and follow-up with administrators on organizational plans for PATH4HIP
Dimensions of REACH, ADOPTION, IMPLEMENTATION, and MAINTENANCE will be assessed to answer objective 1 (feasibility and acceptability of the PATH4HIP intervention) and dimension of EFFECTIVENESS will be assessed to answer objective 2 (PATH4HIP’s preliminary effects). All data sources, methods, and outcome/process measures for each dimensions of the RE-AIM framework [24] are further described in Table 2.
Data analysis
Quantitative analysis
Sociodemographic information
We will use appropriate descriptive statistics (mean and standard deviation for normally distributed continuous variables [e.g., age], median and interquartile range for skewed continuous variables [e.g., acute care and rehabilitation length of stays], frequency and proportion for categorical variables [e.g., type of rehabilitation service]). We will also describe and compare the participants and non-participants’ sociodemographic and clinical information during the study period.
Objective 1 (feasibility and acceptability of the PATH4HIP intervention)
All outcomes under the dimensions of REACH, ADOPTION, and IMPLEMENTATION will be measured using proportions and reported with a 95% confidence interval.
Objective 2 (PATH4HIP’s preliminary effects)
We will use descriptive statistics for outcomes under the dimension of EFFECTIVENESS as follows. For normally distributed continuous data, we will use mean and standard deviation (e.g., % discharged back to community, % transfer back to acute care). For skewed continuous data, we will report median and interquartile range (e.g., acute care and rehabilitation length of stays). For categorical data, we will report frequency and proportion [e.g., functional gains in rehabilitation (admission and discharge functional independence measure (FIM) [32]). All data analysis will be performed with IBM SPSS Statistics version 23.
Qualitative analysis
Objective 1 (feasibility and acceptability of the PATH4HIP intervention): All interviews will be transcribed verbatim. Two researchers will independently code the transcripts, and we will perform coding and content analysis on the transcripts using an iterative process until consensus on the coding and content analysis is reached [33]. The qualitative data analysis software (NVivo, QSR International) will be used to manage all the qualitative data.
Data management
The principal investigator will oversee all aspects of the study. All data will be stored in accordance with the research ethics board procedures and requirements for storage and security of data. Hardcopy files will be kept securely in a locked filing cabinet. Electronic files will be stored on a secure server and files with participant identifying information will be password protected. Participants will be allocated a unique study participant identification number, which will be used in any documentation associated with the study. Audio recordings of the interviews will be destroyed after verbatim transcripts have been prepared. Only the study investigators and research assistants will have access to the study data. Ethics auditing procedures will be determined by the research ethics board. Research records will be stored for a period of 10 years.
Progression criteria
Progression to a larger follow-up study will be determined by the following criteria:
-
(1)
At least 75% of patients that are deemed eligible for PATH4HIP agree to participate
-
(2)
At least 75% of the participants are transferred to geriatric rehabilitation by post-operative day 6
Based on the CONSORT guidelines for pilot and feasibility studies [28], we will report against these criteria using a traffic light system: red (not to proceed), amber (proceed with amendments), or green (proceed).
Discussion
Study results will inform future work to test the effectiveness of the intervention across multiple sites. If successful, this approach has the potential to be spread across multiple settings for hip fracture patient transitions from acute care to rehabilitation.
Strengths and limitations
This study has several strengths. The intervention was developed from a systematic barriers and enablers analysis [27] using the Theoretical Domains Framework [34, 35]. Currently, most quality improvement approaches tend to lack a theoretical base for conceptualizing clinical decision-making and behavior change processes. This often makes it difficult to apply emerging evidence and spread change across a variety of health care settings. In contrast, our approach designed based on the results of a theory-based barriers and enablers analysis [27] allowed us to study the challenges of hip fracture transfer from acute care to rehabilitation from the perspectives of clinicians, administrators, senior leaders, patients, and families. PATH4HIP was then designed using a prioritization analysis of behavior change techniques [26] that we will implement in this current study in order to support the adherence and sustainability of the intervention. Our theory-informed intervention will also allow us to select monitoring metrics that can be replicated in other organizations and will assist in discerning the mechanisms behind how and why an intervention succeeds or fails. Our design of PATH4HIP and its implementation strategy have emphasized cross-sectoral collaboration, between acute and subacute care. Most importantly, this study also prioritizes best practices for hip fracture outcomes and embeds them at the heart of the intervention design, using a low-cost solution.
This proposed study is a single-arm, pragmatic feasibility study and therefore will also have some limitations due to the lack of a control group. Although timely access to rehabilitation is a best practice for geriatric hip fracture patients [1, 9,10,11], it is possible that we will need to adapt the intervention during the study period due to unanticipated consequences. We will document these changes as they may inform the methods required for a larger study to evaluate PATH4HIP across multiple sites.
Availability of data and materials
No additional data are available.
References
Health Quality Ontario. Ministry of Health and Long-Term Care. Quality-Based Procedures: Clinical Handbook for Hip Fracture. Toronto: Health Quality Ontario; 2013. p. 97 . Available from: http://www.hqontario.ca/evidence/publications-and-ohtac- recommendations/clinicalhandbooks.
Haugan K, Halsteinli V, Døhl Ø, Basso T, Johnsen LG, Foss OA. Health care services and costs after hip fracture, comparing conventional versus standardised care: a retrospective study with 12-month follow-up. Injury. 2021:S0020-1383(21)00072-3. https://doi.org/10.1016/j.injury.2021.01.034 Epub ahead of print. PMID: 33551261.
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90. https://doi.org/10.7326/0003-4819-152-6-201003160-00008 PMID: 20231569; PMCID: PMC3010729.
Leal J, Gray AM, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK, et al. Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int. 2016;27(2):549–58. https://doi.org/10.1007/s00198-015-3277-9 Epub 2015 Aug 19. PMID: 26286626; PMCID: PMC4740562.
Nikitovic M, Wodchis WP, Krahn MD, Cadarette SM. Direct health-care costs attributed to hip fractures among seniors: a matched cohort study. Osteoporos Int. 2013;24(2):659–69. https://doi.org/10.1007/s00198-012-2034-6 Epub 2012 Jun 27. PMID: 22736067; PMCID: PMC3557373.
Budhia S, Mikyas Y, Tang M, Badamgarav E. Osteoporotic fractures: a systematic review of U.S. healthcare costs and resource utilization. Pharmacoeconomics. 2012;30(2):147–70. https://doi.org/10.2165/11596880-000000000-00000 PMID: 22187933.
Cadarette SM, Katz JN, Brookhart MA, et al. Trends in drug prescribing for osteoporosis after hip fracture, 1995–2004. J Rheumatol. 2008;35:319–26.
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006;35(5):293–305. https://doi.org/10.1016/j.semarthrit.2005.11.001 PMID: 16616152.
National Clinical Guideline Centre. 2019 surveillance of Hip fracture: management (NICE guideline CG124). London: National Institute for Health and Care Excellence (NICE). 2019. Available from:https://www.ncbi.nlm.nih.gov/books/NBK552246/.
Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–7. https://doi.org/10.5435/JAAOS-D-14-00432 PMID: 25624365.
Rehabilitative Care Alliance. Rehabilitative Care Best Practices for Patients with Hip Fracture; 2018. Available from: http://rehabcarealliance.ca/uploads/File/Initiatives_and_Toolkits/Frail_Seniors/Hip_Fracture_Rehabilitative_Care_Best_Practices_Framework.pdf
Handoll HHG, Cameron ID, Mak JCS, Finnegan TP. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev. 2009;Issue 4. Art. No.:CD007125. https://doi.org/10.1002/14651858.CD007125.pub2.
Holstege MS, Caljouw MA, Zekveld IG, van Balen R, de Groot AJ, van Haastregt JC, et al. Changes in geriatric rehabilitation: a national programme to improve quality of care. The Synergy and Innovation in Geriatric Rehabilitation study. Int J Integr Care. 2015;15:e045. https://doi.org/10.5334/ijic.2200 PMID: 27118962; PMCID: PMC4843176.
Wells JL, Seabrook JA, Stolee P, Borrie MJ, Knoefel F. State of the art in geriatric rehabilitation. Part I: review of frailty and comprehensive geriatric assessment. Arch Phys Med Rehabil. 2003;84(6):890–7.
Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ. 2010;340:c1718.
Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al. Geriatric rehabilitation following fractures in older people: a systematic review. Health Technol Assess. 2000;4(2):i-iv–1-111 PMID: 10702905.
Levy C, Ocampo-Chan S, Huestis L, Renzetti D. Early rehabilitation for patients with hip fractures: spreading change across the system. Healthc Q. 2017;20(1):29–33.
Haugan K, Johnsen LG, Basso T, Foss OA. Mortality and readmission following hip fracture surgery: a retrospective study comparing conventional and fast-track care. BMJ Open. 2017;7(8):e015574. https://doi.org/10.1136/bmjopen-2016-015574 PMID: 28851773; PMCID: PMC5724094.
Pollmann CT, Røtterud JH, Gjertsen JE, Dahl FA, Lenvik O, Årøen A. Fast track hip fracture care and mortality - an observational study of 2230 patients. BMC Musculoskelet Disord. 2019;20(1):248. https://doi.org/10.1186/s12891-019-2637-6. PMID: 31122228; PMCID: PMC6533651.
Mine Y, Fujino Y, Sabanai K, Muramatsu K, Otani M, Kubo T, et al. Effectiveness of regional clinical pathways on postoperative length of stay for hip fracture patients: a retrospective observational study using the Japanese Diagnosis Procedure Combination database. J Orthop Sci. 2020;25(1):127–31. https://doi.org/10.1016/j.jos.2019.02.002 Epub 2019 Feb 22. PMID: 30799165.
Kristensen PK, Thillemann TM, Søballe K, Johnsen SP. Are process performance measures associated with clinical outcomes among patients with hip fractures? A population-based cohort study. Int J Qual Health Care. 2016;28(6):698–708. https://doi.org/10.1093/intqhc/mzw093 PMID: 27591269.
Nijmeijer WS, Folbert EC, Vermeer M, Vollenbroek-Hutten MMR, Hegeman JH. The consistency of care for older patients with a hip fracture: are the results of the integrated orthogeriatric treatment model of the Centre of Geriatric Traumatology consistent 10 years after implementation? Arch Osteoporos. 2018;13(1):131. https://doi.org/10.1007/s11657-018-0550-5 PMID: 30456430.
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. Gesundheitswesen. 2016;78(3):175–88.
Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions 1st ed. Great Britain: Silverback Publishing; 2014.
Backman C, Harley A, Papp S, French-Merkley V, Beaulé PE, Poitras S, Dobransky J, Squires JE. Barriers and Enablers to Early Identification, Referral and Access to Geriatric Rehabilitation Post-Hip Fracture: A Theory-Based Descriptive Qualitative Study. Geriatr Orthop Surg Rehabil. 2022;13:21514593211047666. https://doi.org/10.1177/21514593211047666.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016;2:64.
Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. https://doi.org/10.1186/1471-2288-10-1.
Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010;10:67.
Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31:180–91.
Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. Am J Phys Med Rehabil. 1993;72(2):84–9. https://doi.org/10.1097/00002060-199304000-00005 PMID: 8476548.
Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med. 2017;7(3):93–9. https://doi.org/10.1016/j.afjem.2017.08.001 Epub 2017 Aug 21. PMID: 30456117; PMCID: PMC6234169.
Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. BMJ Qual Saf. 2005;14(1):26–33.
Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77.
Funding
Funding was received from the Bruyère Academic Medical Organization (BAMO) Innovation fund.
Author information
Authors and Affiliations
Contributions
CB and AH were major contributors in writing the manuscript. All co-authors (SP, STP, RB, PEB, VFM, CW) were involved in the design of the project and critically appraised and edited the manuscript. All authors (CB, AH, SP, STP, RB, PEB, VFM, CW) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was granted by the Ottawa Health Science Network Research Ethics Board (#20180469-01H), the Bruyère Research Ethics Board (#M16-18-036), and the University of Ottawa Research Ethics Board (#H-08-18-1061).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The Standard Protocol Items Recommendations for Trials (SPIRIT) checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Backman, C., Harley, A., Papp, S. et al. Feasibility, acceptability, and preliminary effects of PATH FOR timely transfer of geriatric HIP fracture patients from hospital to rehabilitation to home (PATH4HIP): a protocol for a mixed method study. Pilot Feasibility Stud 8, 124 (2022). https://doi.org/10.1186/s40814-022-01079-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01079-z