Abstract
Background
Exposure to chemical mixtures inherent in air pollution, has been shown to be associated with the risk of breast and lung cancers. However, studies on the molecular mechanisms of exposure to a mixture of these pollutants, such as hydrocarbons, in the development of breast and lung cancers are scarce. We utilized in silico toxicogenomic analysis to elucidate the molecular pathways linked to both cancers that are influenced by exposure to a mixture of selected hydrocarbons. The Comparative Toxicogenomics Database and Cytoscape software were used for data mining and visualization.
Results
Twenty-five hydrocarbons, common in air pollution with carcinogenicity classification of 1 A/B or 2 (known/presumed or suspected human carcinogen), were divided into three groups: alkanes and alkenes, halogenated hydrocarbons, and polyaromatic hydrocarbons. The in silico data-mining revealed 87 and 44 genes commonly interacted with most of the investigated hydrocarbons are linked to breast and lung cancer, respectively. The dominant interactions among the common genes are co-expression, physical interaction, genetic interaction, co-localization, and interaction in shared protein domains. Among these genes, only 16 are common in the development of both cancers. Benzo(a)pyrene and tetrachlorodibenzodioxin interacted with all 16 genes. The molecular pathways potentially affected by the investigated hydrocarbons include aryl hydrocarbon receptor, chemical carcinogenesis, ferroptosis, fluid shear stress and atherosclerosis, interleukin 17 signaling pathway, lipid and atherosclerosis, NRF2 pathway, and oxidative stress response.
Conclusions
Within the inherent limitations of in silico toxicogenomics tools, we elucidated the molecular pathways associated with breast and lung cancer development potentially affected by hydrocarbons mixture. Our findings indicate adaptive responses to oxidative stress and inflammatory damages are instrumental in the development of both cancers. Additionally, ferroptosis—a non-apoptotic programmed cell death driven by lipid peroxidation and iron homeostasis—was identified as a new player in these responses. Finally, AHR potential involvement in modulating IL-8, a critical gene that mediates breast cancer invasion and metastasis to the lungs, was also highlighted. A deeper understanding of the interplay between genes associated with these pathways, and other survival signaling pathways identified in this study, will provide invaluable knowledge in assessing the risk of inhalation exposure to hydrocarbons mixture. The findings offer insights into future in vivo and in vitro laboratory investigations that focus on inhalation exposure to the hydrocarbons mixture.
Similar content being viewed by others
Introduction
Air pollution, a pervasive mixture of chemicals and particulate matter (PM), is one of the greatest environmental risks to health. In 2019, the World Health Organization (WHO) estimated 11% of outdoor air pollution-related premature deaths were due to cancer within the respiratory tract [1].
Polycyclic aromatic hydrocarbons (PAHs) are among the chemicals found in the complex mixture of chemicals and PM in air pollution [2, 3]. Common sources of PAHs include household combustion devices, motor vehicles, industrial activities, and forest fires [2]. Exposure to airborne PAHs in both occupational and non-occupational settings were associated with the risk of developing breast and lung cancers [2,3,4,5,6,7,8]. Notably, a French prospective cohort study, of a large sample size with long-term exposure data of benzo(a)pyrene (BaP), showed significant association between airborne BaP exposure and overall breast cancer risk. The association was greater among women in menopausal transition and tobacco smokers [3]. Inevitably, the International Agency for Research on Cancer (IARC) classified BaP as a Group 1 carcinogen in humans, based on sufficient experimental evidence of carcinogenicity in animals and corroborated by consistent mechanistic evidence [9].
The IARC has also declared tobacco smoking to have sufficient and limited evidence in humans to cause lung and breast cancer, respectively [10]. Arguably, tobacco smoking is a good example of adverse health effects of exposure to chemicals mixture. This is because tobacco smoke contains more than 5,000 different chemicals, including PAHs, tobacco specific nitrosamines, aromatic amines, aldehydes, phenols, nitro compounds, volatile hydrocarbons, and other organic and inorganic chemicals [11]. Tobacco smokers who work at industrial facilities are at high risk of exposure to hydrocarbons mixture and the risks of breast and lung cancers have been shown to be greater among workers who smoke tobacco [3, 12]. Studies on the mechanism by which exposure to a mixture of hydrocarbons contributes to the development of breast and lung cancers are scarce and, indeed, a complex field to venture into. However, advances in toxicogenomics provide comprehensive databases on chemicals, genes, proteins, and diseases that one can utilize to gain insights into molecular pathways that chemical mixtures potentially influence in the development of a specific disease.
This article elucidates interactions of genes influenced by a mixture of carcinogenic hydrocarbons with those related to the development of breast and lung cancer. Importantly, the article demonstrates the capability of in silico data-mining for gauging probable molecular mechanisms of mixture-induced toxic effects. This may then assist in strategizing experimental studies to better understand the impact of airborne hydrocarbons in the development of breast and lung cancers. The findings of such studies would then contribute to the risk assessment of chemical mixtures to safeguard the health of people.
Methods
Selection of hazardous air pollutants
In 2019, Ismail et al. [13] undertook to prioritize the hazard classification of 188 chemicals in the Office of Environment Health Hazard Assessment (OEHHA) list of chemicals emitted from California refineries [14]. The prioritization was in accordance with the United Nations Globally Harmonized System of Classification and Labelling of Chemicals (UN GHS). The classifications considered were carcinogenicity (C), mutagenicity (M) and reproductive toxicity (R) from databases of nine countries. Out of the 188 chemicals, 67 were identified as carcinogens 1 A (known human carcinogen), 1B (presumed human carcinogen) or 2 (suspected human carcinogen) [13].
We confirmed the classification of these chemicals by referencing databases of six countries—Australia, European Union (EU), Japan, South Korea, Malaysia, and New Zealand—to reflect the latest classification. The reference databases (Table 1) were chosen as they were accessible in English on the open World Wide Web domain.
From the revised list, chemicals with the most stringent carcinogenicity classification (1/1A/1B) (Suppl Table 1) were then screened for hydrocarbons, as they are common air pollutants and contained in tobacco smoke. These hydrocarbons were further analyzed for gene interactions in the development of breast and lung cancers. The molecular pathways potentially influenced by these genes were elucidated to gain insights on potential molecular pathways affected by hydrocarbons mixture.
Comparative Toxicogenomic database (CTD) analysis
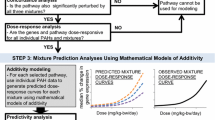
The hydrocarbons were grouped into alkanes/alkenes, halogenated hydrocarbons, and PAHs. The linkages between these groups of hydrocarbons and cancers of the breast and lung, were explored by analyzing the chemical-gene/protein interactions obtained from the Comparative Toxicogenomic Database (CTD; https://ctdbase.org/). The analysis was based on data downloaded in July 2023. The CTD is a public domain database that allows the integration of data to provide a better understanding of the interactions between environmental chemicals, genes, and diseases [15]. Chemicals, chemical-phenotypes, gene ontology and chemicals-disease associations are the examples of information provided by the CTD. The search for genes associated with breast and or lung cancers was based on the CAS number of each individual carcinogenic hydrocarbon and inference network. The data-mining process flow is depicted in Fig. 1. The respective inference score and the reference links are in Supplementary Table 2.
Identifying common genes for hydrocarbons mixture and breast and lung cancer development
The lists of genes extracted from the CTD were uploaded to an Excel spreadsheet. Further analysis was done with Cytoscape version 2.5.10—a free software package—to visualize, model and analyze molecular and genetic interaction networks [16].
Gene-gene interaction network construction
The complex gene-gene interactions network of the common genes between the hydrocarbons and the selected cancers was constructed with GeneMANIA, a free in silico tool (http://www.genemania.org) that provides a flexible interface to query genomic, proteomic, and gene function data [17, 18]. The tools’ dataset are from various publicly available databases, such as Gene Expression Omnibus (GEO) for co-expression data [19]; BioGRID for physical and genetic interaction data [20]; I2D for predicted protein interaction data [21]; and Pathway Commons for pathway and molecular interaction data [22,23,24,25]. The database has almost 2300 networks from eight different organisms that collectively contain nearly 600 million interactions covering almost 164,000 genes [18]. GeneMANIA generates networks from the data either directly or using an in-house analysis pipeline to convert profiles to functional association networks [26]. Co-expression networks were filtered (by default) to remove weak correlations [18]. In this study, Homo sapiens was selected as a target organism in GeneMANIA analysis.
Molecular pathways enrichment analysis
Pathway analysis was performed by Cytoscape ClueGO together with CluePedia plug-in version 2.5.10. The common genes found between hydrocarbons that are associated with the selected cancer development were inserted into the Load Marker List section. The Kyoto Encyclopedia of Genes and Genomes (KEGG), Reactome, and WikiPathways [27,28,29] databases were selected in the ClueGO settings to extract the list of pathways. Enrichment right-sided hypergeometric test was used for the enrichment with a Bonferroni step-down correction and a κ score of 0.3 to link the terms [30]. ClueGO plug-in integrates GO terms and KEGG/BioCarta pathways. The plug-in was used to visualize molecular pathways and gene ontology that are linked to the examined common genes connected to the selected cancers. The organism analyzed was set to Homo sapiens. The output results (gene-pathway interactions) are shown in Supplementary Figs. 1 & 2 that were used to construct Figs. 2 and 3.
Results
Classification revision
Among the 67 chemicals screened, the classifications of seven chemicals were revised to a more stringent category: from category 2 (suspected human carcinogen) to category 1/1A/1B (known human carcinogen/presumed human carcinogen). This revision was based on Japan’s most stringent classification. The seven chemicals are 1,1,2,2-tetrachloroethane (CAS No. 79-34-5), analine (CAS No. 62-53-3), anthracene (CAS No. 120-12-7), biphenyl (CAS No. 92-52-4), dichloromethane (CAS No. 75-09-2), methyl isobutyl ketone (CAS No. 108-10-1), and styrene (CAS No. 100-42-5) (Suppl Table 1). With the revision, 41 of the 67 chemicals are category 1/1A/1B carcinogens, of which 27 are hydrocarbons (Suppl Table 1). Among the 27 hydrocarbons, 25 were identified as alkanes, alkenes, halogenated hydrocarbons, and PAHs.
Comparative Toxicogenomic database analysis
Among the 25 hydrocarbons, nine were excluded from further toxicogenomics analysis for absence of curated data in the CTD. The nine chemicals are isobutane (CAS No. 75-28-5), n-butane (CAS No. 106-97-8), 1,1,2,2-tetrachloroethane (CAS No. 79-34-5), 1,2-dichloroethane (CAS No. 107-06-2), vinyl bromide (CAS No. 593-60-2), polychlorinated biphenyl (CAS No. 1336-36-3), benz(a)anthracene (CAS No. 56-55-3), biphenyl (CAS No. 92-52-4), and benzo(e)pyrene (CAS No. 192-97-2) (Suppl Table 2).
In the alkanes/alkenes group, only two of the four chemicals contained gene interactions data. Isoprene (2-methyl-1,3-butadiene (CAS No. 78-79-5)) affects 12 and 8 genes associated with breast and lung cancer, respectively, whilst 1,3-butadiene (CAS No. 106-99-0) affects 63 genes linked to breast cancer development and 48 genes linked to lung cancer (Suppl Table 2).
In the halogenated group, six of the twelve chemicals affect genes linked to breast or lung cancer genes. Tetrachlorodibenzodioxin (TCDD) (CAS No. 1746-01-6) interacts with the greatest number of genes related to breast cancer development (489 genes), followed by trichloroethylene (CAS No. 79-01-6; 230 genes), tetrachloroethylene (CAS No. 127-18-4; 40 genes), and dichloromethane (CAS No. 75-09-2; 35 genes). Both 1,2 dichloropropane (CAS No. 78-87-5) and 1,2-dibromoethane (CAS No. 106-93-4) affect only five genes (Suppl Table 2). Regarding genes linked to lung cancer development, TCDD, carbon tetrachloride (CAS No. 56-23-5), dichloromethane, and vinyl chloride (CAS No. 75-01-4) affect 250, 184, 25, and 16 genes, respectively, whilst 1,2-dichloropropane and 1,2-dibromoethane affect less than ten genes (Suppl Table 2).
Among the nine chemicals in the PAHs group, BaP (CAS No. 50-32-8) affects the greatest number of genes related to breast cancer development (492 genes), followed by anthracene (CAS No. 120-12-7; 12 genes) (Suppl Table 2). In regard to interactions with lung cancer-associated genes, BaP affects the greatest number of genes (259 genes), followed by benzo(b)fluoranthene (CAS No. 205-99-2; 52 genes), chrysene (CAS No. 218-01-9; 35 genes), dibenz(a, h)anthracene (CAS No. 53-70-3; 34 genes), and benzo(k)fluoranthene (CAS No. 207-08-9; 33 genes) (Suppl Table 2).
Genes interacted with hydrocarbons mixture that are connected to breast and lung cancers
The data-mining revealed 87 and 44 genes linked to breast and lung cancer, respectively, interacted with most of the investigated hydrocarbons (Suppl Table 3).
The mutual molecular pathways in the development of breast and lung cancer that are linked to these genes are aryl hydrocarbon receptor (AHR) pathway, apoptosis, chemical carcinogenesis, ferroptosis, fluid shear stress and atherosclerosis, lipid and atherosclerosis, miRNA in DNA damage response, Nrf2 pathway, nuclear receptors meta-pathway, and oxidative stress response (Suppl Figs. 1 & 2; Suppl Tables 4 & 5).
Molecular pathways involved in breast cancer but not in lung cancer development are androgen receptor signaling, DNA methylation, estrogen metabolism and signaling, and interleukin-10 (IL-10) anti-inflammatory signaling (Suppl Fig. 1 & Suppl Table 4).
Interleukin-3, 4, 13 and 17 (IL-3, IL-4, IL-13, IL-17) signaling pathways, p53 signaling, oxidative damage response, and SUMOylation are involved in the development of lung cancer (Suppl Fig. 2 & Suppl Table 5) but not breast cancer.
Gene-gene interaction network affected by the common genes
GeneMANIA Cytoscape predictive plug-in provides information on interaction types between the common genes. The interaction types include: (a) Co-expression—two gene products are linked if their expression levels are similar across conditions in a gene expression study; (b) Genetic interaction—two genes are functionally associated if one gene is affected by alterations that occur to the second gene; (c) Physical Interaction—two genes product are linked if they interact at protein level; (d) Co-localization—genes expressed in the same tissue or proteins found in the same location; (e) Interaction in shared protein domains; and (f) Interaction predicted by the server [18].
Complex networks encompassing the whole set of interactions between the common genes linked to breast and lung cancers are presented in Supplementary Fig. 3. Co-expression (47.33% of interactions) and physical interaction (40.18%) are the dominant interactions among the common genes in breast cancer development, followed by genetic interaction (2.90%), co-localization (2.74%), and interaction in shared protein domains (0.54%) (Table 2). In the case of lung cancer development, co-expression is the dominant interaction between the common genes (46.88%), followed by physical interaction (24.17%), shared protein domain (7.61%), co-localization (7.43%), and genetic interaction (3.04%) (Table 2).
In gaining insights on the potential biological pathways that would be affected by exposure to a mixture of hydrocarbons, we focused on 16 genes common in the development of both cancers (Suppl Table 3). Among these genes, 12 are protein-coding genes and 4 are proto-oncogenes.
The protein encoded by the 12 genes are baculoviral inhibitor of apoptosis (IAP) repeat-containing 5 (BIRC5), cyclin D1 (CCNDI), cytochrome P450 1B1 (CYP1B1), DNA methyltransferase 3 alpha (DNMT3A), estrogen receptor 1 (ESR1), glutathione S-transferase pi 1 (GSTP1), heme oxygenase 1 (HMOX1), interleukin 1 β (IL1B), interleukin 6 (IL6), transferrin receptor (TFRC), tumor necrosis factor (TNF), and tumor protein p53 (TP53). The 4 proto-oncogenes are c-Fos (FOS), Jun (JUN), HRas (HRAS) and Kras (KRAS) (Suppl Table 3).
Among the investigated hydrocarbons, 3 are associated with breast cancer development only: the halogenated hydrocarbon, trichloroethylene (TCE) and tetrachloroethylene, and anthracene, a polyaromatic hydrocarbon (Table 3). The chemical-gene interactions involved changes in mRNA and protein expression. All 3 chemicals do not interact with the HRAS and KRAS genes (Table 3).
TCE interacted with the other 14 genes: it increased the expression of mRNA and/or protein of BIRC5 [31, 32], CCND1 [33], CYP1B1 [34], ESR1 [35], FOS [35], GSTP1 [35], HMOX1 [31, 35, 36], IL1B [37], IL6 [35], JUN [31, 35, 37], TNF [38], and TP53 [39]. It also decreased mRNA expression of CCND1 [40], CYP1B1 [36], DNMT3A [31, 41], IL6 [42], JUN [43], TFRC [35], TNF [44], TP53 [34], and decreased HMOX1, IL6 and TNF protein expression [38, 45] (Table 3). The potential biological pathways affected by TCE are AHR pathway, apoptosis, chemical carcinogenesis, DNA methylation, estrogen metabolism and signaling, ferroptosis, fluid shear stress & atherosclerosis, IL-10 anti-inflammatory signaling, lipid and atherosclerosis, miRNA in DNA damage, Nrf2 pathway, and oxidative stress response (Fig. 2).
Tetrachloroethylene interacted with only 5 genes (BIRC5, FOS, JUN, TNF, and TP53). It increased the expression of BIRC5 and TP53 mRNAs and TNF protein, as well as decreased the expression of FOS and JUN proteins (Table 3). The potential biological pathways affected by tetrachloroethylene are AHR pathway, apoptosis, estrogen signaling, ferroptosis, fluid shear stress & atherosclerosis, lipid and atherosclerosis, miRNA in DNA damage, nuclear receptors meta-pathway, and oxidative stress response (Fig. 2). Tetrachloroethylene ability to increase the expression of BIRC5 mRNA (Table 3) suggests deregulation of apoptosis as a potential mechanism affected by tetrachloroethylene in the development of breast cancer. This is because BIRC5—a member of the inhibitor of apoptosis (IAP) family—inhibits caspase activation, which leads to deregulation of apoptosis and increase cellular proliferation [46].
Anthracene interacted with only 3 genes (CCND1, CYP1B1, and ESR1). It increased the expression of CYP1B1 mRNA, as well as CCND1 and ESR1 protein (Table 3). The potential biological pathways affected by anthracene are AHR pathway, chemical carcinogenesis, estrogen metabolism and signaling, estrogen-dependent nuclear events, miRNA in DNA damage, and nuclear receptors meta-pathway (Fig. 2).
In the case of lung cancer, the interactions of carbon tetrachloride, vinyl chloride,dibenz(a, h)anthracene, benzo(b)fluoranthene, benzo(k)fluoranthene, and chrysene with the 16 genes, involved up- and down-regulation at mRNA and protein levels, gene polymorphism, and gene mutagenesis (Table 4).
Carbon tetrachloride affected the up- and or down-regulation of all 16 genes at mRNA and or protein levels (Table 4). It increased the activity of DNMT3A, FOS, HMOX1, IL1B, IL6, JUN, and TNF. This implicates potential involvement of biological pathways associated with AHR pathway, apoptosis, chemical carcinogenesis, ferroptosis, fluid shear stress & atherosclerosis, oxidative stress response, and SUMOylation (Fig. 3).
Vinyl chloride interacted with only 6 genes. In addition to down regulating HMOX1, IL1B, IL6, and TP53 at mRNA level, as well as decreasing HMOX1 protein expression, it increased mutagenesis of both KRAS [47,48,49,50] and TP53 [47,48,49] genes (Table 4). When KRAS gene is mutated, it becomes an oncogene that can transform normal cells into cancer cells [51], whilst TP53 mutations resulted in uncontrolled cell growth leading to cancer development [52]. Thus, the potential mechanism by which vinyl chloride contributes to the development of lung cancer is associated with disruption of normal cellular processes and promotion of tumorigenesis. In the case of TNF, vinyl chloride increased the mRNA and protein activity (Table 4), indicating potential impact in tumor microenvironment.
Among the 4 PAHs associated with lung cancer, benzo(b)fluoranthene and benzo(k)fluoranthene interacted with 11 of the 16 genes, whilst chrysene and dibenz(a, h)anthracene interacted with 5 and 4 genes, respectively (Table 4). The upregulation of DNMT3A mRNA was increased by benzo(b)fluoranthene but not by the other 3 PAHs (Table 4). Similarly, the regulations of KRAS mRNA and protein were unaffected by all 4 PAHs, except for benzo(b)fluoranthene increased the mutagenesis of KRAS gene [53, 54]. It also increased TP53 protein expression and affected its activity [55] (Table 4). This suggests that benzo(b)fluoranthene and vinyl chloride affected similar biological pathways in the development of lung cancer. A comprehensive overview of the interaction between the 16 genes and PAHs that are linked to lung cancer is shown in Fig. 3.
In the development of both cancers, TCDD and BaP interacted with all 16 genes by affecting the respective mRNA and protein expression and or protein activity (Table 5). BaP can also affect the methylation of BIRC5 3’UTR, GSTP1 promoter, HRAS and IL1B 5’UTR, and phosphorylation of TP53 protein [56,57,58]. The alkenes, isoprene and 1,3-butadiene increased the mutagenesis of both HRAS and KRAS genes [59], whilst BaP increased the mutagenesis of KRAS gene [53, 54, 60, 61] (Table 5). Isoprene also increased the expression of CCND1 protein (Table 5). This indicates similar mechanism of actions by which isoprene, 1,3-butadiene and BaP contribute to the development of both breast and lung cancers.
Discussion
In utilizing the in silico toxicogenomic data-mining approach—to explore molecular mechanisms by which exposure to hydrocarbons mixture affects cancer development—we identified 16 genes common in the development of breast and lung cancers that interact with most of the investigated hydrocarbons. Proteins encoded by these genes: BIRC5, CCND1, TNF, and the proto-oncogenes FOS, JUN, HRAS, and KRAS, have all been implicated in cell cycle regulation directly or indirectly. The other 9 genes, CY1B1, DNMT3A, ESR1, GSTP1, HMOX1, IL1B, IL6, TFRC, and TP53 encode proteins involved in xenobiotic metabolism, gene regulation, oxidative damage response, inflammatory response, iron homeostasis, regulation of cell signaling pathways, and DNA damage response.
It is noted that these common genes may interact with carcinogens other than the investigated hydrocarbons. For example, acetaldehyde (CAS No. 75-07-0), asbestos (CAS No. 1332-21-4), bis(2-ethyl hexyl) phthalate (CAS No. 117-81-7), cadmium (CAS No. 7440-43-9), and chromium (CAS No. 18540-29-9) interacted with most of the 16 common genes, except BIRC5, DNMT3A, HRAS and KRAS (Suppl Table 6). The latter 4 genes interacted with carbon tetrachloride, 1,3-butadiene, TCDD, and BaP in the development of both breast and lung cancers.
The chemical-gene interactions profile suggests complex crosstalk involving DNA damage, transcriptional and post-transcriptional regulations, as well as translational and post-translational regulations, that affect various biological pathways common to cancer development. These biological pathways include gene mutation, cell cycle progression, oxidative stress and damage responses, inflammatory responses, and DNA damage responses.
In our mapping of biological pathways for breast cancer, DNMT3A, an enzyme responsible for de novo DNA methylation, is shown to be involved in miRNA expression (Suppl Fig. 1). The crosstalk between DNA methylation and miRNA expression can drive the pathogenesis of a disease. For instance, miRNAs can influence DNA methylation patterns by targeting transcripts of proteins responsible for DNA methylation, such as DNMT3A. Conversely, the methylation of miRNA promoter regions can inhibit their transcription, affecting their ability to regulate gene expression. Such crosstalk has been shown to drive the hormone-dependent phenotype of breast cancer [62].
In the case of lung cancer, the function of DNMT3A may be modified by SUMOylation a process of attaching and detaching small proteins called Small Ubiquitin-like Modifier (SUMO) to and from target proteins. This may lead to changes in the methylation of genes involved in cell growth and division, potentially contributing to uncontrolled cell proliferation. SUMOylation of other target proteins has been shown to enhance lung cancer metastasis [63].
The nature of chemical interaction in a mixture of hydrocarbons, such as additive, synergistic, potentiation, and antagonism cannot be discerned from this study due to inherent limitations of the study approach. However, the differences in chemical-gene interactions observed among the hydrocarbons provide insights into potential impact of exposure to hydrocarbons mixture.
For example, TCE—a halogenated hydrocarbon associated with increased risk of breast cancer in male and female workers [64, 65]—may potentiate the risk of lung cancer from exposure to dibenz(a, h)anthracene and the risk of both breast and lung cancer from exposure to BaP. The potential mechanism for such potentiation is increased DNA damage through DNA adduct formation and increased cellular proliferation through deregulation of apoptosis. TCE upregulates TP53 protein expression [39], as well as BIRC5 mRNA and protein expression [31, 32]. Elevated cellular TP53 protein has been shown to increase bioactivation of PAHs, such as dibenz(a, h)anthracene and BaP, by the enzyme cytochrome P450 1A1 (CYP1A1), which resulted in the elevation of DNA adduct levels [66]. BIRC5, on the other hand, inhibits caspase activation, which leads to deregulation of apoptosis and increase cellular proliferation [39].
In the case of vinyl chloride co-exposed with dibenz(a, h)anthracene and BaP, the DNA adduct formation via p53-dependent CYP1A1 bioactivation of the two PAHs, may be reduced as vinyl chloride is known to increase mutagenesis of the TP53 gene [48, 49].
Chemical carcinogenesis
Chemical carcinogenesis that pivots on the AHR pathway appears to be the bridge linking the development and progression of breast and lung cancers. AHR plays a "double-edged sword" that promotes or suppresses tumorigenesis, depending on cell and tissue context and mode of AHR activation. In breast cancer, AHR shapes the tumor microenvironment and modifies immune tolerance [67], whilst in lung cancer, AHR is involved in the regulation of cell proliferation, angiogenesis, inflammation, and apoptosis [68].
AHR is a multi-functional transcription factor activated by a variety of ligands, such as BaP, benz(a)anthracene, TCDD, and metabolites of tryptophan, heme and arachidonic acid, indigoids, and equilenin (reviewed in [69]). These ligands can be agonist, antagonist or selective AHR modulators [70]. Upon ligand binding, the cytosolic AHR-ligand complex is translocated into the nucleus where it heterodimerizes with the aryl hydrocarbon nuclear transporter (ARNT) before binding to the xenobiotic/dioxin response elements (XREs/DREs) in the promoter of target genes and triggers their expression [71]. These genes are involved in many physiological functions, such as xenobiotic metabolism [71], immune response [72], cell cycle and proliferation [73, 74], lipid metabolism [75, 76], tumor promotion [77, 78], and negative regulation of AHR pathway [76]. Perturbations of these physiological functions have been shown to be associated with cancer development and progression, which suggests a complex role of AHR in chemical carcinogenesis.
In xenobiotic metabolism, AHR activates transcriptional up-regulation of the cytochrome P450 1A1 (CYP1A1) and CYP1B1 genes. Most of the investigated hydrocarbons are linked to these two genes. Some are substrates for both enzymes. For example, the first step of BaP hydroxylation to BaP-7,8-epoxide, and the final epoxidation step to form BaP-7,8-dihydrodiol-9,10-epoxide (BPDE) are catalyzed by CYP1A1 and CYP1B1 enzymes in the lung and breast tissues [79,80,81], BPDE is a highly genotoxic metabolite that binds to deoxyguanosine at position N-2 to form DNA adducts [82]. Cigarette smoke was reported to induce CYP1A1 and CYP1B1 expressions in lung tissue of smokers and of lung cancer patients (both smokers and non-smokers) [83,84,85], which correlates with increased levels of BPDE and DNA adducts [86,87,88,89,90]. Bulky BaP-like DNA adducts were also detected in breast cancer patients [91, 92]. PAHs reactive metabolites are known to cause point mutations in RAS proto-oncogenes, such as codon 13 and codon 61 of the HRAS gene (reviewed in [93]). These observations suggest that the AHR/CYP450-dependent DNA adducts formation is a likely pathway to be affected by exposure to hydrocarbons mixture in the development of breast and lung cancers.
Several mechanisms by which AHR modulates the cell cycle have been proposed to account for the pro-/anti-proliferative action of AHR agonists observed with tumor cells in vitro [67, 68, 78]. One of the proposed ligand-activated mechanisms involved transcriptional upregulation of the CDKN1B gene by agonist-activated AHR binding to the gene’s promoter region [94, 95]. However, this mechanism has not been demonstrated in the development and progression of either breast or lung cancer. Being an inhibitor of cyclin-dependent kinase activity, increased CDKN1B activity limits phosphorylation of retinoblastoma protein (Rb), resulting in restriction of E2F-dependent gene expression and progression through the cell cycle [70]. In the absence of ligand, AHR complexed with cyclin D and the cyclin-dependent kinases CDK4/6 to promote cell cycle progression in human breast cancer cells [96]. TCDD, the atypical AHR agonist, dissociates the AHR/cyclinD/CDK complex to induce cell cycle arrest [96]. This contradictory role of AHR may reflect the impact of exposure to hydrocarbon mixtures on cell proliferation, as most of the investigated hydrocarbons are AHR agonists with different affinity to the receptor [70]. Similar contradictory effects of AHR on cell cycle progression were also observed in human lung cancer cells [97]. The impact of exposure to mixtures of 2-methyl-1,3-butadiene, carbon tetrachloride, TCDD, and BaP on this pathway may contribute to the development of breast and or lung cancer as these hydrocarbons interacted with CDKN1B gene (Suppl Table 2).
The mechanisms by which AHR shapes the tumor microenvironment are unclear, but it has been proposed that systemic and tumor-localized generation of endogenous AHR ligands heightened AHR expression/activity, which may establish a pro-inflammatory yet immune-suppressive tumor micro-environment. This favors tumor survival and escapes from immune surveillance, which results in tumor progression [70]. Indeed, AHR overexpression that is correlated with elevated expression of inflammatory markers, including interleukin-8 (IL-8), has been observed in human breast tumors [98]. IL-8 has been identified as a critical gene that mediates breast cancer invasion and metastasis to the lungs [99]. The involvement of IL1B—one of the 16 common genes identified in this study—in this mechanism has not been elucidated in both breast and lung cancer development and progression. Our mapping, however, showed IL1B is involved in modulating the IL-17 signaling pathway, lipid and atherosclerosis pathway, and fluid shear stress and atherosclerosis pathway in both breast and lung cancer development. It is plausible that the impact of PAHs mixture on these pathways may involve AHR activation, as fluid shear stress in endothelial cells has been shown to modulate CYP1A-dependent AHR activation [100, 101], but the mechanism of activation remains unclear [67, 68].
Adaptive responses to cellular damage
AHR activation has also been shown to be associated with the oxidative stress response pathway. For example, exposure of estrogen receptor (ER) positive breast cancer cells to low doses of PAHs mixture activated AHR and overexpressed CYP1 isoforms, which correlated with increased expression of antiapoptotic and antioxidant proteins [102].
Besides catalyzing the biotransformation of PAHs to DNA damaging reactive metabolites, CYP1A1 and CYP1B1 catalyze the oxidation of estradiol (E2) to 2-hydroxyestradiol and 4-hydroxyestradiol, which subsequently undergo one-electron oxidation to produce unstable semiquinones (SQs) intermediates [103], potential mutagens that can damage DNA [104, 105]. Additionally, redox cycling can occur, where the SQs can pass their unpaired electron to molecular oxygen, forming a superoxide anion and restoring the catechol. Superoxide anion can then be metabolized to other reactive oxygen species (ROS), including hydrogen peroxide (H2O2) [103, 105]. Another contributor of ROS in breast cancer cells is the expression of CYP2E1, which increased significantly in breast tumors and adjacent tissues [106]. CYP2E1 also regulates autophagy, stimulates stress in the endoplasmic reticulum, and suppresses the metastatic potential of breast cancer cells [107], indicative of the protective role of CYP2E1.
Excessive ROS can cause DNA damage, as well as lipid and protein oxidation, which triggers an oxidative stress response that involves activation of the NRF2-KEAP1 signaling pathway. This pathway modulates the expression of genes encoding antioxidant proteins, such as superoxide dismutase and HMOX1. The latter is involved in the maintenance of cellular homeostasis by catalyzing the oxidation of heme to carbon monoxide, biliverdin, and ferrous iron. These biologically active compounds participate in cellular protection by reducing oxidative injury, attenuating the inflammatory response, inhibiting cell apoptosis, and regulating cell proliferation [108]. In mouse, HMOX1 activity increased tumor growth and angiogenic potential, as well as decreased apoptosis in lung cancer progression [109], whilst in rat and human breast cancer cells, HMOX1 activity inhibits proliferation [110].
Notably, the NRF2-KEAP1 signaling pathway is linked to ferroptosis, one of the common pathways in the development of breast and lung cancer mapped out in this study.
Ferroptosis
Ferroptosis is a non-apoptotic programmed cell death, which has gained traction as a new target for treating tumors [111]. It is regulated by a complex signaling pathway that is dependent on lipid peroxidation and iron accumulation [111, 112]. Evidence that supports the potential physiological roles of ferroptosis in tumorigenesis resides in the way it is induced in cancer cells. This includes activation of the RAS–RAF–MEK–ERK pathway and induction in cancer cells with mutant RAS, as well as dependency on iron, which is known to be important for cancer cell proliferation (reviewed in [112]). Induction of ferroptosis has been shown to suppress tumor growth, but ferroptotic damage favors tumor growth by triggering inflammation-associated immunosuppression in the tumor microenvironment [112]. Therefore, the three key features of ferroptosis: iron accumulation, increased lipid peroxidation and inability to efficiently reduce lipid peroxidases, must be well regulated to strike the delicate balance of survival and damage in tumorigenesis.
Little is known about ferroptosis role in breast and lung cancer progression, and the impact of exposure to hydrocarbons mixture on such association. However, several studies have found important correlations between mutations in tumor suppressor gene and proto-oncogene, TP53 and RAS, and in genes encoding proteins involved in stress response pathways. One of these pathways is the NRF2 signaling pathway [112], which is one of the common molecular pathways identified in this study.
Depending on the pathological condition, the transcription factor NRF2 serves as either an anti- or pro-ferroptotic activator. Under oxidative stress conditions, NRF2 complexed with its chaperon protein to bind to the ARE (Antioxidant Response Element) on the promoter region of its target genes with anti- or pro-ferroptotic functions. An example of iron-related NRF2 target gene that promotes ferroptotic cascade is HMOX1, which catalyzes the cleavage of heme to form biliverdin, carbon monoxide, and ferrous iron (Fe2+) [113]. Chemical-induced ferroptotic cell death driven by increased HMOX1 expression was observed in HT-1080, neuroblastoma and glioblastoma cell lines [114,115,116]. An example of NRF2 acting as anti-ferroptotic activator is in its regulating the expression of enzymes responsible for glutathione synthesis, as well as preventing lipid peroxidation and reducing oxidized CoQ10, a key membrane antioxidant (GPX4 and FSP1) [113]. Notably, GSTP1 has been shown to be involved in tumor development through the ferroptosis pathway [117] and was suggested to be a novel negative regulator of ferroptosis that may play an important role in lung cancer radiotherapy by inhibiting ferroptosis [118]. Crosstalk mechanisms between the RAS–RAF–MEK–ERK pathway and the NRF2 signaling pathway, with the involvement of GSTP1 in ferroptosis during tumorigenesis in breast and lung cells, and impact of exposure to halogenated and polyaromatic hydrocarbons on the crosstalk mechanisms have yet to be explored.
The role of AHR and NRF2 in regulating ferroptosis in breast and lung cancer cells is unclear, but AHR has been shown to promote the development of non-small cell lung cancer (NSCLC) by inducing the expression of SLC7A11, a key regulator of ferroptosis [119].
In sum, as most hydrocarbons are AHR ligands, the impact of inhalation exposure to hydrocarbons mixture on these physiological functions is complex, given the distinct classes of AHR ligands: agonist, antagonist and selective AHR modulators [70]. However, this study revealed an important role of AHR in being the bridge linking the development and progression of breast and lung cancers as it is involved (directly and or indirectly) in the regulation of biological pathways mapped out in this study. Notably, the mechanism by which IL1B regulates IL-8—a critical gene that mediates breast cancer invasion and metastasis to the lungs [99]—and the role of AHR in such mechanism, is worth pursuing.
Conclusion
Within the inherent limitations of in silico toxicogenomics associated tools, we were able to elucidate the molecular pathways of breast and lung cancer development potentially affected by exposure to hydrocarbons mixture. In silicon data-mining depends on the online sources and the quality of the interactions present in them. Complex molecular pathways were obtained by drawing statistical associations between chemical-gene-disease relationships. Therefore, dose-response relationship, interaction profile of hydrocarbons mixture, route and duration of exposure to the investigated hydrocarbons mixture, along with individual sensitivity of exposed subjects, cannot be drawn from this study. In conclusion, our findings should be regarded as insights into future in vivo and in vitr laboratory investigations that focus on inhalation exposure to the hydrocarbons mixture.
Data availability
All data generated or analyzed during this study are included in this published article. Additional supplementary data are available from the corresponding author upon request.
Abbreviations
- A2M:
-
Alpha-2-macroglobulin
- ABCA8:
-
ATP binding cassette subfamily A member 8
- ABCB1:
-
ATP binding cassette subfamily B member 1
- ABCB1B:
-
ATP-binding cassette, sub-family B
- ABCC1:
-
ATP binding cassette subfamily C member 1
- ABCG2:
-
ATP binding cassette subfamily G member 2
- ABL1:
-
Abl tyrosine kinase proto-oncogene 1
- ACACB:
-
Acetyl-CoA carboxylase beta
- ACE:
-
Angiotensin I converting enzyme
- ACHE:
-
Acetylcholinesterase
- ACSM1:
-
Acyl-CoA synthetase medium chain family member 1
- ACTA2:
-
Actin alpha 2
- ACTB:
-
Actinβ
- ACVR1:
-
Activin A receptor type 1
- ADA:
-
Adenosine deaminase
- ADAR:
-
Adenosine deaminase RNA specific
- ADAM10:
-
ADAM metallopeptidase domain 10
- ADAM28:
-
ADAM metallopeptidase domain 28
- ADAM33:
-
ADAM metallopeptidase domain 33
- ADAMTS1:
-
ADAM metallopeptidase with thrombospondin type 1 motif 1
- AFP:
-
Alpha fetoprotein
- AGR2:
-
Anterior gradient 2
- AHR:
-
Aryl hydrocarbon receptor
- AKAP12:
-
A-kinase anchoring protein 12
- AKT1:
-
Akt kinase
- AKT2:
-
AKT serine/threonine kinase 2
- ALDOA:
-
Aldolase, fructose-bisphosphate A
- ALK:
-
ALK receptor tyrosine kinase
- ALKBH8:
-
AlkB homolog 8
- ALX4:
-
ALX homeobox 4
- ANGPTL4:
-
Angiopoietin like 4
- ANK3:
-
Ankyrin 3
- ANKRD18A:
-
Ankyrin repeat domain 18 A
- ANKRD20A2P:
-
Ankyrin repeat domain 20 family member A2
- ANKRD34A:
-
Ankyrin repeat domain 34 A
- ANXA2:
-
Annexin A2
- AOC4P:
-
Amine oxidase copper containing 4,pseudogene
- APC:
-
APC regulator of WNT signaling pathway
- APC2:
-
APC regulator of WNT signaling pathway 2
- APOA1:
-
Apolipoprotein A1
- APOBEC3A:
-
Apolipoprotein B mRNA editing enzyme catalytic subunit 3 A
- APOBEC3B:
-
Apolipoprotein B mRNA editing enzyme catalytic subunit 3B
- APOC3:
-
Apolipoprotein C3
- APOE:
-
Apolipoprotein E
- APRT:
-
Adenine phosphoribosyltransferase
- AR:
-
Androgen receptor
- ARAF:
-
A-Raf proto-oncogene
- AREG:
-
Amphiregulin
- ARF1:
-
ADP ribosylation factor 1
- ARHGDIA:
-
Rho GDP dissociation inhibitorα
- ARHGEF5:
-
Rho guanine nucleotide exchange factor 5
- ARID1A:
-
AT-rich interaction domain 1 A
- ARRDC3:
-
Arrestin domain containing 3
- ARTN:
-
Artemin
- AS3MT:
-
Arsenite methyltransferase
- ATG10:
-
Autophagy related 10
- ATG101:
-
Autophagy related 101
- ATM:
-
ATM serine/threonine kinase
- ATOX1:
-
Antioxidant 1 copper chaperone
- ATP6AP1L:
-
ATPase H + transporting accessory protein 1 like (pseudogene)
- ATP7B:
-
ATPase copper transportingβ
- ATSDR:
-
Agency for Toxic Substances and Disease Registry
- AURKA:
-
Aurora kinase A
- AVPI1:
-
Arginine vasopressin induced 1
- AZGP1:
-
α-2-glycoprotein 1,zinc-binding
- B4GAT1:
-
Beta-1,4-glucuronyltransferase 1
- BAG1:
-
BAG cochaperone 1
- BAP1:
-
BRCA1 associated protein 1
- BARD1:
-
BRCA1 associated RING domain 1
- BAX:
-
CL2 associated X
- BCAR3:
-
BCAR3 adaptor protein
- BCHE:
-
Butyrylcholinesterase
- BCL2:
-
BCL2 apoptosis regulator
- BCL2A1:
-
BCL2 related protein A1
- BCL2L1:
-
BCL2 like 1
- BECN1:
-
Beclin 1
- BGN:
-
Biglycan
- BHLHE41:
-
Basic helix-loop-helix family member e41
- BIRC2:
-
Baculoviral IAP repeat containing 2
- BIRC5:
-
Baculoviral IAP repeat containing 5
- BMP2:
-
Bone morphogenetic protein 2
- BMP4:
-
Bone morphogenetic protein 4
- BMPR2:
-
Bone morphogenetic protein receptor type 2
- BRAF:
-
B-Raf proto-oncogene, serine/threonine kinase
- BRCA1:
-
BRCA1 DNA repair associated
- BRCA2:
-
BRCA2 DNA repair associated
- BRF1:
-
BRF1 RNA polymerase III transcription initiation factor subunit
- BRIP1:
-
BRCA1 interacting helicase 1
- BTN3A2:
-
Butyrophilin subfamily 3 member A2
- C1QBP:
-
Complement C1q binding protein
- CA12:
-
Carbonic anhydrase 12
- CADM1:
-
Cell adhesion molecule 1
- CALEPA:
-
California Environmental Protection Agency
- CALML3:
-
Calmodulin like 3
- CAS:
-
Chemical Abstract Service
- CASP7:
-
Caspase 7
- CASP8:
-
Caspase 8
- CAT:
-
Catalase
- CAV1:
-
Caveolin 1
- CBR2:
-
Carbonyl reductase 2
- CCL18:
-
C-C motif chemokine ligand 18
- CCL20:
-
C-C motif chemokine ligand 20
- CCN1:
-
Cellular communication network factor 1
- CCN2:
-
Cellular communication network factor 2
- CCND1:
-
Cyclin D1
- CCNE1:
-
Cyclin E1
- CCNG1:
-
Cyclin G1
- CCNH:
-
Cyclin H
- CCT5:
-
Chaperonin containing TCP1 subunit 5
- CD109:
-
CD109 molecule
- CD274:
-
CD274 molecule
- CD40:
-
CD40 molecule
- CD74:
-
CD74 molecule
- CDA:
-
Cytidine deaminase
- CDH1:
-
Cadherin 1
- CDH13:
-
Cadherin 13
- CDH2:
-
Cadherin 2
- CDH5:
-
Cadherin 5
- CDKN1A:
-
Cyclin dependent kinase inhibitor 1 A
- CDKN1B:
-
Cyclin dependent kinase inhibitor 1B
- CDKN1C:
-
Cyclin dependent kinase inhibitor 1 C
- CDKN2A:
-
Cyclin dependent kinase inhibitor 2 A
- CEACAM1:
-
CEA cell adhesion molecule 1
- CENPF:
-
Centromere protein F
- CES1:
-
Carboxylesterase 1
- CES1F:
-
Carboxylesterase 1 F
- CFL1:
-
Cofilin 1
- CHD4:
-
Chromodomain helicase
- DNA:
-
Binding protein 4
- CHEK1:
-
Checkpoint kinase 1
- CHEK2:
-
Checkpoint kinase 2
- CHRNA2:
-
Cholinergic receptor nicotinic α 2 subunits
- CHRNA3:
-
Cholinergic receptor nicotinic α 3 subunits
- CHRNA5:
-
Cholinergic receptor nicotinic α 5 subunits
- CHRNA7:
-
Cholinergic receptor nicotinic α 7 subunits
- CHRNB4:
-
Cholinergic receptor nicotinic β 4 subunits
- CHST15:
-
Carbohydrate sulfotransferase 15
- CLCA2:
-
Chloride channel accessory 2
- CLDN1:
-
Claudin 1
- CLDN4:
-
Claudin 4
- CLIC1:
-
Chloride intracellular channel 1
- CLPTM1L:
-
Cleft lip and palate associated transmembrane protein 1
- CLTB:
-
Clathrin light chain B
- CLUL1:
-
Clusterin like 1
- CNR2:
-
Cannabinoid receptor 2
- COL6A1:
-
Collagen type VI α 1 chain
- COL7A1:
-
Collagen type VII α 1 chain
- COMT:
-
Catechol-O-methyltransferase
- COTL1:
-
Coactosin like F-actin binding protein 1
- COX17:
-
Cytochrome c oxidase copper chaperone COX17
- CPE:
-
Carboxypeptidase E
- CPT1A:
-
Carnitine palmitoyltransferase 1 A
- CRHR1:
-
Corticotropin releasing hormone receptor 1
- CRP:
-
C-reactive protein
- CSF1:
-
Colony stimulating factor 1
- CSF1R:
-
Colony stimulating factor 1 receptor
- CSF2:
-
Colony stimulating factor 2
- CSF3:
-
Colony stimulating factor 3
- CST6:
-
Cystatin E/M
- CTD:
-
Comparative Toxicogenomic Database
- CTNNB1:
-
Catenin beta 1
- CTU1:
-
Cytosolic thiouridylase subunit 1
- CTU2:
-
Cytosolic thiouridylase subunit 2
- CUL5:
-
Cullin 5
- CWH43:
-
Cell wall biogenesis 43 C-terminal homolog
- CXCL1:
-
C-X-C motif chemokine ligand 1
- CXCL12:
-
C-X-C motif chemokine ligand 12
- CXCL14:
-
C-X-C motif chemokine ligand 14
- CXCL2:
-
C-X-C motif chemokine ligand 2
- CXCL3:
-
C-X-C motif chemokine ligand 3
- CXCL8:
-
C-X-C motif chemokine ligand 8
- CXCL9:
-
C-X-C motif chemokine ligand 9
- CXCR4:
-
C-X-C motif chemokine receptor 4
- CYP17A1:
-
Cytochrome P450 family 17 subfamily A member 1
- CYP19A1:
-
Cytochrome P450 family 19 subfamily A member 1
- CYP1A1:
-
Cytochrome P450 family 1 subfamily A member 1
- CYP1A2:
-
Cytochrome P450 family 1 subfamily A member 2
- CYP1B1:
-
Cytochrome P450 family 1 subfamily B member 1
- CYP24A1:
-
Cytochrome P450 family 24 subfamily A member 1
- CYP2A6:
-
Cytochrome P450 family 2 subfamily A member 6
- CYP2B1:
-
Cytochrome P450 family 2 subfamily B member 1
- CYP2D6:
-
Cytochrome P450 family 2 subfamily D member 6
- CYP2E1:
-
Cytochrome P450 family 2 subfamily E member 1
- CYP3A4:
-
Cytochrome P450 family 3 subfamily A member 4
- DAB2IP:
-
DAB2 interacting protein
- DAP3:
-
Death associated protein 3
- DAPK1:
-
Death associated protein kinase 1
- DDIT3:
-
DNA damage inducible transcript 3
- DDR1:
-
Discoidin domain receptor tyrosine kinase 1
- DEK:
-
DEK proto-oncogene
- DEPP1:
-
DEPP autophagy regulator 1
- DES:
-
Desmin
- DHFR:
-
Dihydrofolate reductase
- DIO3:
-
iodothyronine deiodinase 3
- DKK1:
-
Dickkopf WNT signaling pathway inhibitor 1
- DLL1:
-
Delta like canonical Notch ligand 1
- DLL4:
-
Delta like canonical Notch ligand 4
- DLL4:
-
Delta like canonical Notch ligand 4
- DNAI7:
-
Dynein axonemal intermediate chain 7
- DNASE1L3:
-
Deoxyribonuclease 1 like 3
- DNMT1:
-
DNA methyltransferase 1
- DNMT3A:
-
DNA methyltransferase 3α
- DNMT3B:
-
DNA methyltransferase 3β
- DOK1:
-
Docking protein 1
- DOK2:
-
Docking protein 2
- DOK3:
-
Docking protein 3
- DPYD:
-
Dihydropyrimidine dehydrogenase
- DSC3:
-
Desmocollin 3
- DTX3:
-
Deltex E3 ubiquitin ligase 3
- DYNC2H1:
-
Dynein cytoplasmic 2 heavy chain 1
- E2F1:
-
E2F transcription factor 1
- EAF2:
-
ELL associated factor 2
- ECHA:
-
European Chemicals Agency
- EDNRB:
-
Endothelin receptor type B
- EEF1B2:
-
Eukaryotic translation elongation factor 1 beta 2
- EEF2:
-
Eukaryotic translation elongation factor 2
- EFEMP1:
-
EGF containing fibulin extracellular matrix protein 1
- EFNA1:
-
Ephrin A1
- EFNB2:
-
Ephrin B2
- EGF:
-
Epidermal growth factor
- EGFR:
-
Epidermal growth factor receptor
- EGR1:
-
Early growth response 1
- EHMT2:
-
Euchromatic histone lysine methyltransferase 2
- EIF2S2:
-
Eukaryotic translation initiation factor 2 subunitβ
- EIF6:
-
Eukaryotic translation initiation factor 6
- ELK3:
-
ETS transcription factor ELK3
- ELP1:
-
Elongator acetyltransferase complex subunit 1
- ELP3:
-
Elongator acetyltransferase complex subunit 3
- EMSY:
-
EMSY transcriptional repressor, BRCA2 interacting
- EMX2:
-
Empty spiracles homeobox 2
- ENO1:
-
Enolase 1
- EP300:
-
E1A binding protein p300
- EPA/RPF:
-
USEPA relative potency factor applied
- EPB41L3:
-
Erythrocyte membrane protein band 4.1 like 3
- EPHB4:
-
EPH receptor B4
- EPHX1:
-
Epoxide hydrolase 1
- EPOR:
-
Erythropoietin receptor
- ERBB2:
-
Erb-b2 receptor tyrosine kinase 2
- ERBB3:
-
Erb-b2 receptor tyrosine kinase 3
- ERCC1:
-
ERCC excision repair 1,endonuclease non-catalytic subunit
- ERCC6:
-
ERCC excision repair 6,chromatin remodeling factor
- ERGIC3:
-
ERGIC and golgi 3
- ESR1:
-
Estrogen receptor 1
- ESR2:
-
Estrogen receptor 2
- ESRRA:
-
Estrogen related receptorα
- ETS2:
-
ETS proto-oncogene 2,transcription factor
- ETV4:
-
ETS variant transcription factor 4
- EVL:
-
Enah/Vasp-like
- EU:
-
European Union
- EXO1:
-
Exonuclease 1
- EZH2:
-
Enhancer of zeste 2 polycomb repressive complex 2 subunit
- F3:
-
Coagulation factor III, tissue factor
- FABP7:
-
Fatty acid binding protein 7
- FAS:
-
Fas cell surface death receptor
- FASLG:
-
Fas ligand
- FASN:
-
Fatty acid synthase
- FBL:
-
Fibrillarin
- FBXW7:
-
F-box and WD repeat domain containing 7
- FEN1:
-
Flap structure-specific endonuclease 1
- FGD5:
-
FYVE, RhoGEF and PH domain containing 5
- FGF10:
-
Fibroblast growth factor 10
- FGF3:
-
Fibroblast growth factor 3
- FGF4:
-
Fibroblast growth factor 4
- FGF9:
-
Fibroblast growth factor 9
- FGFR1:
-
Fibroblast growth factor receptor 1
- FGFR2:
-
Fibroblast growth factor receptor 2
- FHIT:
-
Fragile histidine triad diadenosine triphosphatase
- FHL2:
-
Four and a half LIM domains 2
- FKBPL:
-
FKBP prolyl isomerase like
- FLACC1:
-
Flagellum associated containing coiled-coil domains 1
- FLNA:
-
Folliculin
- FLT1:
-
Fms related receptor tyrosine kinase 1
- FN1:
-
Fibronectin 1
- FOS:
-
Fos proto-oncogene, AP-1 transcription factor subunit
- FOSB:
-
FosB proto-oncogene, AP-1 transcription factor subunit
- FOSL2:
-
FOS like 2,AP-1 transcription factor subunit
- FOXA1x:
-
Forkhead box A1
- FOXM1:
-
Forkhead box M1
- FOXP3:
-
Forkhead box P3
- FOXQ1:
-
Forkhead box Q1
- FST:
-
Follistatin
- FTO:
-
FTO alpha-ketoglutarate dependent dioxygenase
- FUBP1:
-
Far upstream element binding protein 1
- GALNT16:
-
Polypeptide N-acetylgalactosaminyltransferase 16
- GAST:
-
Gastrin
- GATA6:
-
GATA binding protein 6
- GC:
-
GC vitamin D binding protein
- GCLC:
-
Glutamate-cysteine ligase catalytic subunit
- GDF10:
-
Growth differentiation factor 10
- GEO:
-
Gene Expression Omnibus
- GJA1:
-
Gap junction protein α 1
- GJB1:
-
Gap junction protein beta 1
- GNAI2:
-
G protein subunit α i2
- GNMT:
-
Glycine N-methyltransferase
- GPER1:
-
G protein-coupled estrogen receptor 1
- GPI:
-
Glucose-6-phosphate isomerase
- GPNMB:
-
Glycoprotein nmb
- GPX1:
-
Glutathione peroxidase 1
- GPX2:
-
Glutathione peroxidase 2
- GPX3:
-
Glutathione peroxidase 3
- GPX4:
-
Glutathione peroxidase 4
- GRB7:
-
Growth factor receptor bound protein 7
- GRIK2:
-
Glutamate ionotropic receptor kainate type subunit 2
- GSK3B:
-
Glycogen synthase kinase 3β
- GSTM1:
-
Glutathione S-transferase mu 1
- GSTP1:
-
Glutathione S-transferase pi 1
- GSTP2:
-
Glutathione S-transferase, pi 2
- GSTT1:
-
Glutathione S-transferase theta 1
- GUCY1A2:
-
Guanylate cyclase 1 soluble subunit α 2
- GZMB:
-
Granzyme B
- H1-2:
-
H1.2 linker histone, cluster member
- H19:
-
H19 imprinted maternally expressed transcript
- H2AX:
-
H2A.X variant histone
- H2BC12:
-
H2B clustered histone 12
- H2BC4:
-
H2B clustered histone 4
- H6PD:
-
Hexose-6-phosphate dehydrogenase/glucose 1-dehydrogenase
- HADHB:
-
Hydroxyacyl-CoA dehydrogenase trifunctional multienzyme complex subunitβ
- HAPLN4:
-
Hyaluronan and proteoglycan link protein 4
- HES1:
-
Hes family bHLH transcription factor 1
- HEY1:
-
Hes related family bHLH transcription factor with YRPW motif 1
- HEY2:
-
Hes related family bHLH transcription factor with YRPW motif 2
- HEYL:
-
Hes related family bHLH transcription factor with YRPW motif like
- HHEX:
-
Hematopoietically expressed homeobox
- HIC1:
-
HIC ZBTB transcriptional repressor 1
- HIF1A:
-
Hypoxia inducible factor 1 subunit alpha
- HILPDA:
-
Hypoxia inducible lipid droplet associated
- HMMR:
-
Hyaluronan mediated motility receptor
- HMOX1:
-
Heme oxygenase 1
- HNRNPK:
-
Heterogeneous nuclear ribonucleoprotein K
- HNRNPL:
-
Heterogeneous nuclear ribonucleoprotein L
- HNRNPR:
-
Heterogeneous nuclear ribonucleoprotein R
- HOXB13:
-
Homeobox B13
- HOXB9:
-
Homeobox B9
- HOXD11:
-
Homeobox D11
- HP:
-
Haptoglobin
- HPSE:
-
Heparinase
- HRAS:
-
HRas proto-oncogene, GTPase
- HRG:
-
Histidine rich glycoprotein
- HSP90AA1:
-
Heat shock protein 90 alpha family class A member 1
- HSPA1B:
-
Heat shock protein family A (Hsp70) member 1B
- HTRA1:
-
HtrA serine peptidase 1
- IARC:
-
International Agency for Research in Cancer
- lIBSP:
-
Integrin binding sialoprotein
- ICAM5:
-
Intercellular adhesion molecule 5
- ID3:
-
Inhibitor of DNA binding 3
- IDO1:
-
Indoleamine 2,3-dioxygenase 1
- IDS:
-
Iduronate 2-sulfatase
- IER2:
-
Immediate early response 2
- IFNB1:
-
Interferon β 1
- IFNG:
-
Interferon gamma
- IGBP1:
-
Immunoglobulin binding protein 1
- IGF1:
-
Insulin like growth factor 1
- IGF1R:
-
Insulin like growth factor 1 receptor
- IGFBP5:
-
Insulin like growth factor binding protein 5
- IGFBP7:
-
Insulin like growth factor binding protein 7
- IKBKG:
-
Inhibitor of nuclear factor kappa B kinase regulatory subunit gamma
- IL10:
-
Interleukin 10
- IL1B:
-
Interleukin 1β
- IL1R2:
-
Interleukin 1 receptor type 2
- IL2:
-
Interleukin 2
- IL24:
-
Interleukin 24
- IL6:
-
Interleukin 6
- IQSEC1:
-
IQ motif and Sect. 7 domain ArfGEF 1
- IRF1:
-
Interferon regulatory factor 1
- IRF4:
-
Interferon regulatory factor 4
- ITSN2:
-
Intersectin 2
- JAG1:
-
Jagged canonical Notch ligand 1
- JAG2:
-
Jagged canonical Notch ligand 2
- JMJD6:
-
Jumonji domain containing 6
- JUN:
-
Jun proto-oncogene
- JUNB:
-
JunB proto-oncogene
- JUND:
-
JunD proto-oncogene
- KCNH1:
-
Potassium voltage-gated channel subfamily H member 1
- KDR:
-
Kinase insert domain receptor
- KIT:
-
KIT proto-oncogene
- KLHDC10:
-
Kelch domain containing 10
- KLHDC7A:
-
Kelch domain containing 7 A
- KLK10:
-
Kallikrein related peptidase 10
- KMT2D:
-
Lysine methyltransferase 2D
- KRAS:
-
KRAS proto-oncogene
- KRT14:
-
Keratin 14
- KRT18:
-
Keratin 18
- KRT5:
-
Keratin 5
- KRT8:
-
Keratin 8
- L3MBTL3:
-
L3MBTL histone methyl-lysine binding protein 3
- LAMTOR5:
-
Late endosomal/lysosomal adaptor, MAPK and MTOR activator 5
- LBX1:
-
Ladybird homeobox 1
- LDHAL6B:
-
Lactate dehydrogenase A like 6B
- LDHB:
-
Lactate dehydrogenase B
- LECT2:
-
Leukocyte cell derived chemotaxin 2
- LEF1:
-
Lymphoid enhancer binding factor 1
- LEP:
-
Leptin
- LEPR:
-
Leptin receptor
- LGR6:
-
Leucine rich repeat containing G protein-coupled receptor 6
- LIMD2:
-
LIM domain containing 2
- LINC00115:
-
Long intergenic non-protein coding RNA 115
- LINC00671:
-
Long intergenic non-protein coding RNA 671
- LLGL1:
-
LLGL scribble cell polarity complex component 1
- LLGL2:
-
LLGL scribble cell polarity complex component 2
- LMNTD1:
-
Lamin tail domain containing 1
- LOXL2:
-
Lysyl oxidase like 2
- LPAR1:
-
Lysophosphatidic acid receptor 1
- LRRC37A:
-
Leucine rich repeat containing 37 A
- LRRC3B:
-
Leucine rich repeat containing 3B
- LSP1:
-
Lymphocyte specific protein 1
- MACIR:
-
macrophage immunometabolism regulator
- MAL:
-
Mal
- MALAT1:
-
Metastasis associated lung adenocarcinoma transcript 1
- MAN2C1:
-
Mannosidase alpha class 2 C member 1
- MAP2K7:
-
Mitogen-activated protein kinase kinase 7
- MAP3K1:
-
Mitogen-activated protein kinase kinase kinase 1
- MAP3K8:
-
Mitogen-activated protein kinase kinase kinase 8
- MAP4K4:
-
Mitogen-activated protein kinase kinase kinase kinase 4
- MAPK1:
-
Mitogen-activated protein kinase 1
- MAPK14:
-
Mitogen-activated protein kinase 14
- MAPK3:
-
Mitogen-activated protein kinase 3
- MARCKS:
-
Myristoylated alanine rich protein kinase C substrate
- MCL1:
-
MCL1 apoptosis regulator
- MDM2:
-
MDM2 proto-oncogene
- MDM4:
-
MDM4 regulator of p53
- MECOM:
-
MDS1 and EVI1 complex locus
- MED12:
-
Mediator complex subunit 12
- MED28:
-
Mediator complex subunit 28
- MEIS1:
-
Meis homeobox 1
- MET:
-
MET proto-oncogen
- METTL6:
-
Methyltransferase 6
- MFGE8:
-
Milk fat globule EGF and factor V/VIII domain containing
- MIF:
-
Macrophage migration inhibitory factor
- MIR10A:
-
MicroRNA 10a
- MIR1246:
-
MicroRNA 1246
- MIR126:
-
MicroRNA 126
- MIR127:
-
MicroRNA 127
- MIR136:
-
MicroRNA 136
- MIR141:
-
MicroRNA 141
- MIR145:
-
MicroRNA 145
- MIR146A:
-
MicroRNA 146a
- MIR152:
-
MicroRNA 152
- MIR154:
-
MicroRNA 154
- MIR155:
-
MicroRNA 155
- MIR193A:
-
MicroRNA 193a
- MIR200B:
-
MicroRNA 200b
- MIR200C:
-
MicroRNA 200c
- MIR205:
-
MicroRNA 205
- MIR206:
-
MicroRNA 206
- MIR21:
-
MicroRNA 21
- MIR22:
-
MicroRNA 22
- MIR221:
-
MicroRNA 221
- MIR222:
-
MicroRNA 222
- MIR224:
-
MicroRNA 224
- MIR242:
-
MicroRNA 242
- MIR24-2:
-
MicroRNA 24 − 2
- MIR29A:
-
MicroRNA 29a
- MIR30:
-
MicroRNA 30
- MIR301A:
-
MicroRNA 301a
- MIR302D:
-
MicroRNA 302d
- MIR30A:
-
MicroRNA 30a
- MIR31:
-
MicroRNA 31
- MIR31HG:
-
MIR31 host gene
- MIR34B:
-
MicroRNA 34b
- MIR34C:
-
MicroRNA 34c
- MIR369:
-
MicroRNA 369
- MIR370:
-
MicroRNA 370
- MIR410:
-
MicroRNA 410
- MIR429:
-
MicroRNA 429
- MIR4435-2HG:
-
MIR4435-2 host gene
- MIR487B:
-
MicroRNA 487b
- MIR494:
-
MicroRNA 494
- MIR506:
-
MicroRNA 506
- MIR98:
-
MicroRNA 98
- MIRLET7BHG:
-
MIRLET7B host gene
- MKI67:
-
Marker of proliferation Ki-67
- MME:
-
Membrane metalloendopeptidase
- MMP1:
-
Matrix metallopeptidase 1
- MMP1:
-
Matrix metallopeptidase 1
- MMP10:
-
Matrix metallopeptidase 10
- MMP14:
-
Matrix metallopeptidase 14
- MMP1A:
-
Matrix metallopeptidase 1a
- MMP2:
-
Matrix metallopeptidase 2
- MMP3:
-
Matrix metallopeptidase 3
- MMP9:
-
Matrix metallopeptidase 9
- MOE:
-
South Korea Ministry of Environment
- MOL:
-
South Korea Ministry of Labour
- MPO:
-
Myeloperoxidase
- MPP1:
-
MAGUK p55 scaffold protein 1
- MRPL13:
-
Mitochondrial ribosomal protein L13
- MRPL19:
-
Mitochondrial ribosomal protein L19
- MRPL9:
-
Mitochondrial ribosomal protein L9
- MRPS22:
-
Mitochondrial ribosomal protein S22
- MRPS23:
-
Mitochondrial ribosomal protein S23
- MRPS28:
-
Mitochondrial ribosomal protein S28
- MRPS7:
-
Mitochondrial ribosomal protein S7
- MST1:
-
Macrophage stimulating 1
- MT3:
-
Metallothionein 3
- MTDH:
-
Metadherin
- MTHFR:
-
Methylenetetrahydrofolate reductase
- MTOR:
-
Mechanistic target of rapamycin kinase
- MTR:
-
5-methyltetrahydrofolate-homocysteine methyltransferase
- MUC12:
-
Mucin 12
- MUC16:
-
Mucin 16
- MYC:
-
MYC proto-oncogene
- MYH9:
-
Myosin heavy chain 9
- MYO18B:
-
Myosin XVIIIB
- NAT2:
-
N-acetyltransferase 2
- NCOA1:
-
Nuclear receptor coactivator 1
- NCOA2:
-
Nuclear receptor coactivator 2
- NCOA3:
-
Nuclear receptor coactivator 3
- NCOR1:
-
Nuclear receptor corepressor 1
- NDRG1:
-
N-myc downstream regulated 1
- NDUFS3:
-
NADH: ubiquinone oxidoreductase core subunit S3
- NECTIN2:
-
Nectin cell adhesion molecule 2
- NFE2L2:
-
NFE2 like bZIP transcription factor 2
- NFKBIA:
-
NFKB inhibitorα
- NFYA:
-
Nuclear transcription factor Y subunitα
- NISCH:
-
Nischarin
- NMBR:
-
Neuromedin B receptor
- NOP9:
-
NOP9 nucleolar protein
- NOS2:
-
Nitric oxide synthase 2
- NOS3:
-
Nitric oxide synthase 3
- NOTCH1:
-
Notch receptor 1
- NOTCH2:
-
Notch receptor 2
- NOTCH3:
-
Notch receptor 3
- NOTCH4:
-
Notch receptor 4
- NPPA:
-
Natriuretic peptide A
- NQO1:
-
NAD(P)H quinone dehydrogenase 1
- NQO1:
-
NAD(P)H quinone dehydrogenase 1
- NQO2:
-
NAD(P)H quinone dehydrogenase 2
- NR2F1:
-
Nuclear receptor subfamily 2 group F member 1
- NR2F6:
-
Nuclear receptor subfamily 2 group F member 6
- NR2F6:
-
Nuclear receptor subfamily 2 group F member 6
- NRCAM:
-
Neuronal cell adhesion molecule
- NRG1:
-
Neuregulin 1
- NRIP1:
-
Nuclear receptor interacting protein 1
- NSD2:
-
Nuclear receptor binding SET domain protein 2
- NSUN6:
-
NOP2/Sun RNA methyltransferase 6
- NUDT17:
-
Nudix hydrolase 17
- NUDT2:
-
Nudix hydrolase 2
- O&G:
-
Oil and gas
- OCLN:
-
Occluding
- OEHHA:
-
Office of Environment Health Hazard Assessment
- OGG1:
-
8-oxoguanine DNA glycosylase
- PABPC1:
-
Poly(A) binding protein cytoplasmic 1
- PAEP:
-
Progestagen associated endometrial protein
- PAK1:
-
P21 (RAC1) activated kinase 1
- PALB2:
-
Partner and localizer of BRCA2
- PARP1:
-
Poly(ADP-ribose) polymerase 1
- PCBP1:
-
Poly(rC) binding protein 1
- PCDHGB6:
-
Protocadherin gamma subfamily B,6
- PCNA:
-
Proliferating cell nuclear antigen
- PDCD1:
-
Programmed cell death 1
- PDCD4:
-
Programmed cell death 4
- PDE2A:
-
Phosphodiesterase 2 A
- PDGFA:
-
Platelet derived growth factor subunit A
- PDLIM4:
-
PDZ and LIM domain 4
- PDPK1:
-
3-phosphoinositide dependent protein kinase 1
- PDZK1:
-
PDZ domain containing 1
- PER3:
-
Period circadian regulator 3
- PGGT1B:
-
Protein geranylgeranyltransferase type I subunit beta
- PGR:
-
Progesterone receptor
- PHB1:
-
Prohibitin 1
- PHGDH:
-
Phosphoglycerate dehydrogenase
- PIK3CA:
-
Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunitα
- PIM1:
-
Pim-1 proto-oncogene, serine/threonine kinase
- PIN1:
-
Peptidylprolyl cis/trans isomerase, NIMA-interacting 1
- PLA2G4A:
-
Phospholipase A2 group IVA
- PLEKHD1:
-
Pleckstrin homology and coiled-coil domain containing D1
- PON1:
-
Paraoxonase 1
- PPARGC1B:
-
PPARG coactivator 1β
- PPBP:
-
Pro-platelet basic protein
- PPM1D:
-
Protein phosphatase, Mg2+/Mn2 + dependent 1D
- PPP1R12B:
-
Protein phosphatase 1 regulatory subunit 12B
- PPP2R1B:
-
Protein phosphatase 2 scaffold subunit 1β
- PPRTV:
-
USEPA Provisional Peer-Reviewed Toxicity Values
- PRC1:
-
Protein regulator of cytokinesis 1
- PRDX1:
-
Peroxiredoxin 1
- PRDX6:
-
Peroxiredoxin 6
- PRKN:
-
Parkin RBR E3 ubiquitin protein ligase
- PRSS46:
-
Protease, serine 46
- PSMA4:
-
Proteasome 20 S subunit α 4
- PTEN:
-
Phosphatase and tensin homolog
- PTGIS:
-
Prostaglandin I2 synthase
- PTGS1:
-
Prostaglandin-endoperoxide synthase 1
- PTGS2:
-
Prostaglandin-endoperoxide synthase 2
- PTHLH:
-
Parathyroid hormone like hormone
- PTMA:
-
Prothymosinα
- PTPRD:
-
Protein tyrosine phosphatase receptor type D
- PYCARD:
-
PYD and CARD domain containing
- RAD51:
-
RAD51 recombinase
- RAD51B:
-
RAD51 paralog B
- RAD51C:
-
RAD51 paralog C
- RAD52:
-
RAD52 homolog, DNA repair protein
- RAD54L:
-
RAD54 like
- RAF1:
-
Raf-1 proto-oncogene, serine/threonine kinase
- RALYL:
-
RALY RNA binding protein like
- RAMP2:
-
Receptor activity modifying protein 2
- RARA:
-
Retinoic acid receptorα
- RARB:
-
Retinoic acid receptorβ
- RASSF1:
-
Ras association domain family member 1
- RB1:
-
RB transcriptional corepressor 1
- RB1CC1:
-
RB1 inducible coiled-coil 1
- RBM3:
-
RNA binding motif protein 3
- RBP4:
-
Retinol binding protein 4
- RCCD1:
-
RCC1 domain containing 1
- RCHY1:
-
Ring finger and CHY zinc finger domain containing 1
- RECQL:
-
RecQ like helicase
- RELA:
-
RELA proto-oncogene, NF-kB subunit
- REPS2:
-
RALBP1 associated Eps domain containing 2
- RGS2:
-
Regulator of G protein signaling 2
- RIBC2:
-
RIB43A domain with coiled-coils 2
- RIC8A:
-
RIC8 guanine nucleotide exchange factor A
- RIOX2:
-
Ribosomal oxygenase 2
- RMND1:
-
Required for meiotic nuclear division 1 homolog
- RNASET2:
-
Ribonuclease T2
- RNF115:
-
Ring finger protein 115
- RNF182:
-
Ring finger protein 182
- ROBO1:
-
Roundabout guidance receptor 1
- ROR1:
-
Receptor tyrosine kinase like orphan receptor 1
- RPL23A:
-
Ribosomal protein L23a
- RPL31:
-
Ribosomal protein L31
- RPLP2:
-
Ribosomal protein lateral stalk subunit P2
- RPS4X:
-
Ribosomal protein S4 X-linked
- RPS6:
-
Ribosomal protein S6
- RPS6KB2:
-
Ribosomal protein S6 kinase B2
- RPS7:
-
Ribosomal protein S7
- RPS8:
-
Ribosomal protein S8
- RRAD:
-
Ras related glycolysis inhibitor and calcium channel regulator
- RSPO3:
-
R-spondin 3
- RTEL1:
-
Regulator of telomere elongation helicase 1
- RUNX2:
-
RUNX family transcription factor 2
- RUNX3:
-
RUNX family transcription factor 3
- RXRB:
-
Retinoid X receptorβ
- SECISBP2L:
-
SECIS binding protein 2 like
- SELENBP1:
-
Selenium binding protein 1
- SELENOP:
-
Selenoprotein P
- SERPINA1:
-
Serpin family A member 1
- SERPINB2:
-
Serpin family B member 2
- SERPINB5:
-
Serpin family B member 5
- SERPING1:
-
Serpin family G member 1
- SETBP1:
-
SET binding protein 1
- SETD2:
-
SET domain containing 2,histone lysine methyltransferase
- SFRP1:
-
Secreted frizzled related protein 1
- SFRP2:
-
Secreted frizzled related protein 2
- SFRP5:
-
Secreted frizzled related protein 5
- SFTPB:
-
Surfactant protein B
- SFTPD:
-
Surfactant protein D
- SHMT1:
-
Serine hydroxymethyltransferase 1
- SIDT2:
-
SID1 transmembrane family member 2
- SIM1:
-
SIM bHLH transcription factor 1
- SIRT1:
-
Sirtuin 1
- SLC10A6:
-
Solute carrier family 10 member 6
- SLC16A3:
-
Solute carrier family 16 member 3
- SLC22A18:
-
Solute carrier family 22 member 18
- SLC28A1:
-
Solute carrier family 28 member 1
- SLC2A1:
-
Solute carrier family 2 member 1
- SLC2A10:
-
Solute carrier family 2 member 10
- SLC2A2:
-
Solute carrier family 2 member 2
- SLC2A5:
-
Solute carrier family 2 member 5
- SLC39A6:
-
Solute carrier family 39 member 6
- SLC3A2:
-
Solute carrier family 3 member 2
- SLC5A5:
-
Solute carrier family 5 member 5
- SLC7A5:
-
Solute carrier family 7 member 5
- SLCO1B1:
-
Solute carrier organic anion transporter family member 1B1
- SLCO1B3:
-
Solute carrier organic anion transporter family member 1B3
- SMARCC1:
-
SWI/SNF related, matrix associated, actin dependent regulator of chromatin subfamily c member 1
- SMC2:
-
Structural maintenance of chromosomes 2
- SNAI1:
-
Snail family transcriptional repressor 1
- SNAI2:
-
Snail family transcriptional repressor 2
- SNCG:
-
Synuclein gamma
- SND1:
-
Staphylococcal nuclease and tudor domain containing 1
- SNX32:
-
Sorting nexin 32
- SOD2:
-
Superoxide dismutase 2
- SOX2:
-
SRY-box transcription factor 2
- SOX30:
-
SRY-box transcription factor 30
- SOX9:
-
SRY-box transcription factor 9
- SPATA18:
-
Spermatogenesis associated 18
- SPP1:
-
Secreted phosphoprotein 1
- SPRY2:
-
Sprouty RTK signaling antagonist 2
- SRC:
-
SRC proto-oncogene, non-receptor tyrosine kinase
- SREBF2:
-
Sterol regulatory element binding transcription factor 2
- STARD8:
-
StAR related lipid transfer domain containing 8
- STAT3:
-
Signal transducer and activator of transcription 3
- STAT5A:
-
Signal transducer and activator of transcription 5 A
- STC2:
-
Stanniocalcin 2
- STIM1:
-
Stromal interaction molecule 1
- STK11:
-
Serine/threonine kinase 11
- STMN1:
-
Stathmin 1
- STN1:
-
STN1 subunit of CST complex
- STXBP4:
-
Syntaxin binding protein 4
- SULT1A1:
-
Sulfotransferase family 1 A member 1
- SYNE1:
-
Spectrin repeat containing nuclear envelope protein 1
- SYNJ2:
-
Synaptojanin 2
- TAFA4:
-
TAFA chemokine like family member 4
- TANK:
-
TRAF family member associated NFKB activator
- TBX3:
-
T-box transcription factor
- TCL1B:
-
TCL1 family AKT coactivator B
- TEP1:
-
Telomerase associated protein 1
- TERT:
-
Telomerase reverse transcriptase
- TFAP2A:
-
Transcription factor AP-2α
- TFPI2:
-
Tissue factor pathway inhibitor 2
- TFRC:
-
Transferrin receptor
- TGFB1:
-
Transforming growth factor β 1
- TGFBR2:
-
Transforming growth factor beta receptor 2
- TGM2:
-
Transglutaminase 2
- THBS1:
-
Thrombospondin 1
- THEMIS2:
-
Thymocyte selection associated family member 2
- TLE3:
-
TLE family member 3
- TLR4:
-
Toll like receptor 4
- TMEM25:
-
Transmembrane protein 25
- TMEM45A:
-
Transmembrane protein 45 A
- TNF:
-
Tumor necrosis factor
- TNFSF10:
-
TNF superfamily member 10
- TNIP1:
-
TNFAIP3 interacting protein 1
- TOP2A:
-
DNA topoisomerase IIα
- TOX3:
-
TOX high mobility group box family member 3
- TP53:
-
Tumor protein p53
- TP53BP1:
-
Tumor protein p53 binding protein 1
- TP53BP2:
-
Tumor protein p53 binding protein 2
- TP63:
-
Tumor protein p63
- TP73:
-
Tumor protein p73
- TRERF1:
-
Transcriptional regulating factor 1
- TRIM12A:
-
Tripartite motif-containing 12 A
- TRIM47:
-
Tripartite motif containing 47
- TRIO:
-
Trio Rho guanine nucleotide exchange factor
- TRMT11:
-
TRNA methyltransferase 11 homolog
- TRP53:
-
Transformation related protein 53
- TRP63:
-
Transformation related protein 63
- TSC2:
-
TSC complex subunit 2
- TSHR:
-
Thyroid stimulating hormone receptor
- TTR:
-
Transthyretin
- TUBB3:
-
Tubulin beta 3 class III
- TXN:
-
Thioredoxin
- TYMS:
-
Thymidylate synthetase
- TYRP1:
-
Tyrosinase related protein 1
- UBD:
-
Ubiquitin D
- UBE2C:
-
Ubiquitin conjugating enzyme E2 C
- UBLCP1:
-
Ubiquitin like domain containing CTD phosphatase 1
- UGT2B17:
-
UDP glucuronosyltransferase family 2 member B17
- UMPS:
-
Uridine monophosphate synthetase
- UN GHS:
-
United Nations Globally Harmonized System of Classification and Labelling of Chemicals
- UPK1B:
-
Uroplakin 1B
- USP18:
-
Ubiquitin specific peptidase 18
- VDR:
-
Vitamin D receptor
- VEGFB:
-
Vascular endothelial growth factor B
- VEGFC:
-
Vascular endothelial growth factor C
- VHL:
-
Von Hippel-Lindau tumor suppressor
- VIM:
-
Vimentin
- VPS39:
-
VPS39 subunit of HOPS complex
- WNT10B:
-
Wnt family member 10B
- WNT5A:
-
Wnt family member 5 A
- WT1:
-
WT1 transcription factor
- WWOX:
-
WW domain containing oxidoreductase
- XPC:
-
XPC complex subunit
- XRCC2:
-
X-ray repair cross complementing 2
- XRCC3:
-
X-ray repair cross complementing 3
- YAP1:
-
Yes1 associated transcriptional regulator
- YBX1:
-
Y-box binding protein 1
- ZC3H11A:
-
Zinc finger CCCH-type containing 11 A
- ZEB1:
-
Zinc finger E-box binding homeobox 1
- ZEB2:
-
Zinc finger E-box binding homeobox 2
- ZFP366:
-
Zinc finger protein 366
- ZNF365:
-
Zinc finger protein 365
- ZNF366:
-
Zinc finger protein 366
- ZNF404:
-
Zinc finger protein 404
- ZNF432:
-
Zinc finger protein 432
- ZNF595:
-
Zinc finger protein 595
- ZSCAN22:
-
Zinc finger and SCAN domain containing 22
- ZSWIM5:
-
Zinc finger SWIM-type containing 5
References
WHO. Ambient (outdoor) air pollution (who.int). Access on 7 Aug 2023.
Xue Y, Wang L, Zhang Y, Zhao Y, Liu Y. Air pollution: a culprit of lung cancer. J Hazard Mater. 2022;434:128937. https://doi.org/10.1016/j.jhazmat.2022.128937.
Amadou A, Praud D, Coudon T, Deygas F, Grassot L, Faure E, et al. Risk of breast cancer associated with long-term exposure to benzo[a]pyrene (BaP) air pollution: evidence from the French E3N cohort study. Environ Int. 2021;149:106399. https://doi.org/10.1016/j.envint.2021.106399.
Pedersen- JE, Hansen J. Employment and risk of female breast cancer in Denmark. Am J Ind Med. 2022;65(5):343–56. https://doi.org/10.1002/ajim.23342.
Zeinomar N, Oskar S, Kehm RD, Sahebzeda S, Terry MB. Environmental exposures and breast cancer risk in the context of underlying susceptibility: a systematic review of the epidemiological literature. Environ Res. 2020;187:109346. https://doi.org/10.1016/j.envres.2020.109346.
Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: an updated review of epidemiological literature informed by biological mechanisms. Environ Res. 2018;160:152–82. https://doi.org/10.1016/j.envres.2017.08.045.
Moayedi-Nia S, Pasquet R, Siemiatycki J, Koushik A, Ho V. Occupational exposures and Lung Cancer Risk-An analysis of the CARTaGENE Study. J Occup Environ Med. 2022;64(4):295–304. https://doi.org/10.1097/JOM.0000000000002481.
Olsson A, Guha N, Bouaoun L, Kromhout H, Peters S, Siemiatycki J, et al. Occupational exposure to polycyclic aromatic hydrocarbons and lung cancer risk: results from a pooled analysis of case-control studies (SYNERGY). Cancer Epidemiol Biomarkers Prev. 2022;31(7):1433–41. https://doi.org/10.1158/1055-9965.EPI-21-1428.
IARC Working Groups. 2012. Chemical Agents and Related Occupations: BENZO[a] PYRENE [Internet]. International Agency for Research on Cancer; https://www.ncbi.nlm.nih.gov/books/NBK304415/.
Cogliano VC, Baan R, Straif K, Grosse Y, Lauby-Secretan B, El Ghissassi F, et al. Preventable exposures associated with human cancers. J Natl Cancer Inst. 2011;103:1827–39.
Kim SM, Hwang KA, Choi DW, Choi KC. The cigarette smoke components induced the cell proliferation and epithelial to mesenchymal transition via production of reactive oxygen species in endometrial adenocarcinoma cells. Food Chem Toxicol. 2018;121:657–65. https://doi.org/10.1016/j.fct.2018.09.023.
Wong JYY, Bassig BA, Seow WJ, Hu W, Ji BT, Blair A, et al. Lung cancer risk in welders and foundry workers with a history of heavy smoking in the USA: the National Lung Screening Trial. Occup Environ Med. 2017;74(6):440–8. https://doi.org/10.1136/oemed-2016-104168.
Ismail M, Inayat Hussain SH, Yoneda M, Latif MT. Hazard Assessment for Hazardous Air Pollutants from Petroleum Refinery Operations Using Multi-Country Regulatory Databases. InSPE Asia Pacific Health, Safety, Security, Environment and Social Responsibility Symposium? 2019 Apr 19 (p. D022S010R001). SPE.
Riveles K, Nagai A. Analysis of refinery chemical emissions and health effects. Office of Environmental Health Hazard Assessment, California Environmental Protection Agency, Mar 209 [Internet]. Available from Analysis of Refinery Chemical Emissions and Health Effects.
Davis AP, Grondin CJ, Johnson RJ, Sciaky D, Wiegers J, Wiegers TC, Mattingly CJ. Comparative toxicogenomics database (CTD): update 2021. Nucleic Acids Res. 2021;49(D1):D1138–43.
Cline MS, Smoot M, Cerami E, Kuchinsky A, Landys N, Workman C, Christmas R, Avila-Campilo I, Creech M, Gross B, Hanspers K. Integration of biological networks and gene expression data using Cytoscape. Nat Protoc. 2007;2(10):2366–82.
Warde-Farley D, Donaldson SL, Comes O, Zuberi K, Badrawi R, Chao P, Franz M, Grouios C, Kazi F, Lopes CT, Maitland A. The GeneMANIA prediction server: biological network integration for gene prioritization and predicting gene function. Nucleic Acids Res. 2010;38(suppl 2):W214–20.
Franz M, Rodriguez H, Lopes C, Zuberi K, Montojo J, Bader GD, Morris Q. GeneMANIA update 2018. Nucleic Acids Res. 2018;46(W1):W60–4. https://doi.org/10.1093/nar/gky311.
Barrett T, Wilhite SE, Ledoux P, Evangelista C, Kim IF, Tomashevsky M, Marshall KA, Phillippy KH, Sherman PM, Holko M, Yefanov A. NCBI GEO: archive for functional genomics data sets—update. Nucleic Acids Res. 2012;41(D1):D991–5.
Oughtred R, Stark C, Breitkreutz BJ, Rust J, Boucher L, Chang C, Kolas N, O’Donnell L, Leung G, McAdam R, Zhang F. The BioGRID interaction database: 2019 update. Nucleic Acids Res. 2019;47(D1):D529–41.
Brown KR, Jurisica I. Online predicted human interaction database. Bioinformatics. 2005;21(9):2076–82.
Keshava Prasad TS, Goel R, Kandasamy K, Keerthikumar S, Kumar S, Mathivanan S, et al. Human protein reference database—2009 update. Nucleic Acids Res. 2009;37(suppl1):D767–72.
Romero P, Wagg J, Green ML, Kaiser D, Krummenacker M, Karp PD. Computational prediction of human metabolic pathways from the complete human genome. Genome Biol. 2005;6(1):1–7.
Aranda B, Achuthan P, Alam-Faruque Y, Armean I, Bridge A, Derow C, et al. The IntAct molecular interaction database in 2010. Nucleic Acids Res. 2010;38(suppl1):D525–31.
Ceol A, Chatr Aryamontri A, Licata L, Peluso D, Briganti L, Perfetto L, et al. MINT, the molecular interaction database: 2009 update. Nucleic Acids Res. 2010;38(suppl1):D532–9.
Mostafavi S, Ray D, Warde-Farley D, Grouios C, Morris Q. GeneMANIA: a real-time multiple association network integration algorithm for predicting gene function. Genome Biol. 2008;9:1–5.
Jassal B, Matthews L, Viteri G, Gong C, Lorente P, Fabregat A, Sidiropoulos K, Cook J, Gillespie M, Haw R, Loney F. The reactome pathway knowledgebase. Nucleic Acids Res. 2020;48(D1):D498–503.
Kanehisa M, Goto S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28(1):27–30.
Kutmon M, Lotia S, Evelo CT, Pico AR. WikiPathways App for Cytoscape: making biological pathways amenable to network analysis and visualization. F1000Research. 2014;3.
Bindea G, Mlecnik B, Hackl H, Charoentong P, Tosolini M, Kirilovsky A, et al. ClueGO: a Cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics. 2009;25(8):1091–3. https://doi.org/10.1093/bioinformatics/btp101.
Jiang Y, Chen J, Tong J, Chen T. Trichloroethylene-induced gene expression and DNA methylation changes in B6C3F1 mouse liver. PLoS ONE. 2014;9(12):e116179.
Cao W, Zhang Y, Li A, Yu P, Song L, Liang J, et al. Curcumin reverses hepatic epithelial mesenchymal transition induced by trichloroethylene by inhibiting IL-6R/STAT3. Toxicol Mech Methods. 2021;31(8):589–99.
Sano Y, Nakashima H, Yoshioka N, Etho N, Nomiyama T, Nishiwaki Y, et al. Trichloroethylene liver toxicity in mouse and rat: microarray analysis reveals species differences in gene expression. Arch Toxicol. 2009;83(9):835–49.
Huang Y, Xia Y, Tao Y, Jin H, Ji C, Aniagu S, et al. Protective effects of resveratrol against the cardiac developmental toxicity of trichloroethylene in zebrafish embryos. Toxicology. 2021;452:152697. https://doi.org/10.1016/j.tox.2021.152697.
Rawls KD, Dougherty BV, Vinnakota KC, Pannala VR, Wallqvist A, Kolling GL, et al. Predicting changes in renal metabolism after compound exposure with a genome-scale metabolic model. Toxicol Appl Pharmacol. 2021;412:115390.
Sarma SN, Kim YJ, Ryu JC. Gene expression profiles of human promyelocytic leukemia cell lines exposed to volatile organic compounds. Toxicology. 2010;271(3):122–30.
Tao L, Yang S, Xie M, Kramer PM, Pereira MA. Effect of trichloroethylene and its metabolites, dichloroacetic acid and trichloroacetic acid, on the methylation and expression of c-Jun and c-Myc protooncogenes in mouse liver: prevention by methionine. Toxicol Sci. 2000;54(2):399–407.
Banerjee N, Wang H, Wang G, Khan MF. Enhancing the Nrf2 antioxidant signaling provides Protection Against Trichloroethene-mediated inflammation and autoimmune response. Toxicol Sci. 2020;175(1):64–74. https://doi.org/10.1093/toxsci/kfaa022.
Chen SJ, Wang JL, Chen JH, Huang RN. Possible involvement of glutathione and p53 in trichloroethylene- and perchloroethylene-induced lipid peroxidation and apoptosis in human lung cancer cells. Free Radic Biol Med. 2002;33(4):464–72.
Hendriksen PJ, Freidig AP, Jonker D, Thissen U, Bogaards JJ, Mumtaz MM, et al. Transcriptomics analysis of interactive effects of benzene, trichloroethylene and methyl mercury within binary and ternary mixtures on the liver and kidney following subchronic exposure in the rat. Toxicol Appl Pharmacol. 2007;225(2):171–88. https://doi.org/10.1016/j.taap.2007.08.017.
Jiang CL, He SW, Zhang YD, Duan HX, Huang T, Huang YC, et al. Air pollution and DNA methylation alterations in lung cancer: a systematic and comparative study. Oncotarget. 2017;8(1):1369–91.
Xueqin Y, Wenxue L, Peimao L, Wen Z, Xianqing H, Zhixiong Z. Cytokine expression and cytokine-based T-cell profiling in occupational medicamentosa-like dermatitis due to trichloroethylene. Toxicol Lett. 2018;288:129–35. https://doi.org/10.1016/j.toxlet.2018.02.012.
Jiang Y, Chen J, Yue C, Zhang H, Chen T, Trichloroethylene-Induced DNA. Methylation changes in male F344 rat liver. Chem Res Toxicol. 2016;29(10):1773–7. https://doi.org/10.1021/acs.chemrestox.6b00257.
Gilbert KM, Nelson AR, Cooney CA, Reisfeld B, Blossom SJ. Epigenetic alterations may regulate temporary reversal of CD4(+) T cell activation caused by trichloroethylene exposure. Toxicol Sci. 2012;127(1):169–78. https://doi.org/10.1093/toxsci/kfs093.
Wang G, Wang H, Banerjee N, Khan MF. Interplay and roles of oxidative stress, toll-like receptor 4 and Nrf2 in trichloroethene-mediated autoimmunity. Toxicol Appl Pharmacol. 2020;408:115258. https://doi.org/10.1016/j.taap.2020.115258.
Martínez-Sifuentes MA, Bassol-Mayagoitia S, Nava-Hernández MP, Ruiz-Flores P, Ramos-Treviño J, Haro-Santa Cruz J, et al. Survivin in breast Cancer: a review. Genet Test Mol Biomarkers. 2022;26(9):411–21. https://doi.org/10.1089/gtmb.2021.0286.
Boivin-Angèle S, Lefrançois L, Froment O, Spiethoff A, Bogdanffy MS, Wegener K, et al. Ras gene mutations in vinyl chloride-induced liver tumours are carcinogen-specific but vary with cell type and species. Int J Cancer. 2000;85(2):223–7.
John Luo JC, Cheng TJ, Du CL, Wang JD. Molecular epidemiology of plasma oncoproteins in vinyl chloride monomer workers in Taiwan. Cancer Detect Prev. 2003;27(2):94–101.
Schindler J, Li Y, Marion MJ, Paroly A, Brandt-Rauf PW. The effect of genetic polymorphisms in the vinyl chloride metabolic pathway on mutagenic risk. J Hum Genet. 2007;52(5):448–55.
Weihrauch M, Bader M, Lehnert G, Koch B, Wittekind C, Wrbitzky R, Tannapfel A. Mutation analysis of K-ras-2 in liver angiosarcoma and adjacent nonneoplastic liver tissue from patients occupationally exposed to vinyl chloride. Environ Mol Mutagen. 2002;40(1):36–40.
Huang L, Guo Z, Wang F, Fu L. KRAS mutation: from undruggable to druggable in cancer. Signal Transduct Target Ther. 2021;6(1):386. https://doi.org/10.1038/s41392-021-00780-4.
Olivier M, Hollstein M, Hainaut P. TP53 mutations in human cancers: origins, consequences, and clinical use. Cold Spring Harb Perspect Biol. 2010;2(1):a001008. https://doi.org/10.1101/cshperspect.a001008.
Nesnow S, Ross JA, Mass MJ, Stoner GD. Mechanistic relationships between DNA adducts, oncogene mutations, and lung tumorigenesis in strain A mice. Exp Lung Res. 1998;24(4):395–405.
Mass MJ, Abu-Shakra A, Roop BC, Nelson G, Galati AJ, Stoner GD, et al. Benzo[b]fluoranthene: tumorigenicity in strain A/J mouse lungs, DNA adducts and mutations in the Ki-ras oncogene. Carcinogenesis. 1996;17(8):1701–4.
Chaudhry IS, El-Meanawy A, Khiyami A, Tomashefski JF JR, Machekano RN, Kass L. Short-term exposure to tobacco toxins alters expression of multiple proliferation gene markers in primary human bronchial epithelial cell cultures. J Oncol. 2011;2011:208563. https://doi.org/10.1155/2011/208563.
Christmann M, Boisseau C, Kitzinger R, Berac C, Allmann S, Sommer T, et al. Adaptive upregulation of DNA repair genes following benzo(a)pyrene diol epoxide protects against cell death at the expense of mutations. Nucleic Acids Res. 2016;44(22):10727–43.
Al-Anati L, Högberg J, Stenius U. Non-dioxin-like PCBs interact with benzo[a]pyrene-induced p53-responses and inhibit apoptosis. Toxicol Appl Pharmacol. 2010;249(2):166–77.
Huovinen M, Loikkanen J, Myllynen P, Vähäkangas KH. Characterization of human breast cancer cell lines for the studies on p53 in chemical carcinogenesis. Toxicol Vitro. 2011;25(5):1007–17.
Sills RC, Hong HL, Boorman GA, Devereux TR, Melnick RL. Point mutations of K-ras and H-ras genes in forestomach neoplasms from control B6C3F1 mice and following exposure to 1,3-butadiene, isoprene or chloroprene for up to 2-years. Chem Biol Interact. 2001;135–136:373–86.
Ramakrishna G, Perella C, Birely L, Diwan BA, Fornwald LA, Anderson LM. Decrease in K-ras p21 and increase in Raf1 and activated Erk 1 and 2 in murine lung tumors initiated by N-nitrosodimethylamine and promoted by 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Appl Pharmacol. 2002;179(1):21–34. https://doi.org/10.1006/taap.2001.9344.
Meng F, Knapp GW, Green T, Ross JA, Parsons BL. K-Ras mutant fraction in A/J mouse lung increases as a function of benzo[a]pyrene dose. Environ Mol Mutagen. 2010;51(2):146–55.
Aure MR, Fleischer T, Bjørklund S, Ankill J, Castro-Mondragon JA. Crosstalk between microRNA expression and DNA methylation drives the hormone-dependent phenotype of breast cancer. Genome Med. 2021;72(13). https://doi.org/10.1186/s13073-021-00880-4.
Hung PF, Hong TM, Chang CC, Hung CL, Hsu YL, Chang YL, et al. Hypoxia-induced slug SUMOylation enhances lung cancer metastasis. J Exp Clin Cancer Res. 2019;38(1):5. https://doi.org/10.1186/s13046-018-0996-8.
Laouali N, Pilorget C, Cyr D, Neri M, Kaerlev L, Sabroe S, et al. Occupational exposure to organic solvents and risk of male breast cancer: a European multicenter case-control study. Scand J Work Environ Health. 2018;44(3):310–22. https://doi.org/10.5271/sjweh.3717.
Chuang YS, Lee CY, Lin PC, Pan CH, Hsieh HM, Wu CF, Wu MT. Breast cancer incidence in a national cohort of female workers exposed to special health hazards in Taiwan: a retrospective case-cohort study of ~ 300,000 occupational records spanning 20 years. Int Arch Occup Environ Health. 2022;95(10):1979–93. https://doi.org/10.1007/s00420-022-01897-x.
Wohak LE, Krais AM, Kucab JE, Stertmann J, Ovrebø S, Seidel A et al. Carcinogenic polycyclic aromatic hydrocarbons induce CYP1A1 in human cells via a p53-dependent mechanism. Arch Toxicol. 2014;90(2)y:291–304.
Sweeney C, Lazennec G, Vogel CFA. Environmental exposure and the role of AhR in the tumor microenvironment of breast cancer. Front Pharmacol. 2022;13:1095289. https://doi.org/10.3389/fphar.2022.1095289.
Tsay JJ, Tchou-Wong KM, Greenberg AK, Pass H, Rom AN. Aryl hydrocarbon receptor and lung cancer. Anticancer Res. 2013;33(4):1247–56.
Stejskalova L, Dvorak Z, Pavek P. Endogenous and exogenous ligands of aryl hydrocarbon receptor: current state of art. Curr Drug Metab. 2011;12(2):198–212. https://doi.org/10.2174/138920011795016818.
Murray IA, Patterson AD, Perdew GH. Aryl hydrocarbon receptor ligands in cancer: friend and foe. Nat Rev Cancer. 2014;14(12):801–14. https://doi.org/10.1038/nrc3846.
Nebert DW, Roe AL, Dieter MZ, Solis WA, Yang Y, Dalton TP. Role of the aromatic hydrocarbon receptor and [Ah] gene battery in the oxidative stress response, cell cycle control, and apoptosis. Biochem Pharmacol. 2000;59:65–85. https://doi.org/10.1016/s0006-2952(99)00310-x.
Shinde R, McGaha TL. The aryl hydrocarbon receptor: connecting immunity to the microenvironment. Trends Immunol. 2018;39(12):1005–20. https://doi.org/10.1016/j.it.2018.10.010.
Marlowe JL, Puga A. Aryl hydrocarbon receptor, cell cycle regulation, toxicity, and tumorigenesis. J Cell Biochem. 2005;96(6):1174–84.
Bock KW, Kohle C. Ah receptor- and TCDD-mediated liver tumor promotion: clonal selection and expansion of cells evading growth arrest and apoptosis. Biochem Pharmacol. 2005;69(10):1403–8.
Gouedard C, Barouki R, Morel Y. Induction of the paraoxonase-1 gene expression by resveratrol. Arterioscler Thromb Vasc Biol. 2004;24(12):2378–83.
Gouedard C, Barouki R, Morel Y. Dietary polyphenols increase paraoxonase 1 gene expression by an aryl hydrocarbon receptor dependent mechanism. Mol Cell Biol. 2004;24(12):5209–22.
Gasiewicz TA, Henry EC, Collins LL. Expression and activity of aryl hydrocarbon receptors in development and cancer. Crit Rev Eukaryot Gene Expr. 2008;18(4):279–321.
Ray S, Swanson HI. Activation of the aryl hydrocarbon receptor by TCDD inhibits senescence: a tumor promoting event? Biochem Pharmacol. 2009;77(4):681–8.
Wei C, Caccavale RJ, Kehoe JJ, Thomas PE, Iba MM. CYP1A2 is expressed along with CYP1A1 in the human lung. Cancer Lett. 2001;171(1):113–20. https://doi.org/10.1016/s0304-3835(01)00529-8.
Min JY, Lee GH, Khanal T, Jin SW, Lee SY, Kim HG, et al. Upregulation of CYP1B1 by hypoxia is mediated by ERα activation in breast cancer cells. Am J Cancer Res. 2022;12(6):2798–816.
Huang Z, Fasco MJ, Figge HL, Keyomarsi K, Kaminsky LS. Expression of cytochromes P450 in human breast tissue and tumors. Drug Metab Dispos. 1996;24(8):899–905.
Moorthy B, Chu C, Carlin DJ. Polycyclic aromatic hydrocarbons: from metabolism to lung cancer. Toxicol Sci. 2015;145(1):5–15. https://doi.org/10.1093/toxsci/kfv040.
McLemore TL, Adelberg S, Liu MC, McMahon NA, Yu SJ, Hubbard WC, et al. Expression of CYP1A1 gene in patients with lung cancer: evidence for cigarette smoke-induced gene expression in normal lung tissue and for altered gene regulation in primary pulmonary carcinomas. J Natl Cancer Inst. 1990;82(16):1333–9. https://doi.org/10.1093/jnci/82.16.1333.
Kim JH, Sherman ME, Curriero FC, Guengerich FP, Strickland PT, Sutter TR. Expression of cytochromes P450 1A1 and 1B1 in human lung from smokers, non-smokers, and ex-smokers. Toxicol Appl Pharmacol. 2004;199(3):210–9. https://doi.org/10.1016/j.taap.2003.11.015.
Anttila S, Hietanen E, Vainio H, Camus AM, Gelboin HV, Park SS, et al. Smoking and peripheral type of cancer are related to high levels of pulmonary cytochrome P450IA in lung cancer patients. Int J Cancer. 1991;47(5):681–5. https://doi.org/10.1002/ijc.2910470509.
Ryberg D, Hewer A, Phillips DH, Haugen A. Different susceptibility to smoking-induced DNA damage among male and female lung cancer patients. Cancer Res. 1994;54(22):5801–3.
Mollerup S, Ryberg D, Hewer A, Phillips DH, Haugen A. Sex differences in lung CYP1A1 expression and DNA adduct levels among lung cancer patients. Cancer Res. 1999;59(14):3317–20.
Mollerup S, Berge G, Baera R, Skaug V, Hewer A, Phillips DH, et al. Sex differences in risk of lung cancer: expression of genes in the PAH bioactivation pathway in relation to smoking and bulky DNA adducts. Int J Cancer. 2006;119(4):741–4. https://doi.org/10.1002/ijc.21891.
Uppstad H, Øvrebø S, Haugen A, Mollerup S. Importance of CYP1A1 and CYP1B1 in bioactivation of benzo[a]pyrene in human lung cell lines. Toxicol Lett. 2010;192(2):221–8. https://doi.org/10.1016/j.toxlet.2009.10.025.
Pfeifer GP, Denissenko MF, Olivier M, Tretyakova N, Hecht SS, Hainaut P. Tobacco smoke carcinogens, DNA damage and p53 mutations in smoking-associated cancers. Oncogene. 2002;21(48):7435–51. https://doi.org/10.1038/sj.onc.1205803.
Li D, Wang M, Firozi PF, Chang P, Zhang W, Baer-Dubowska W, et al. Characterization of a major aromatic DNA adduct detected in human breast tissues. Environ Mol Mutagen. 2002;39(2–3):193–200. https://doi.org/10.1002/em.10063.
Li D, Wang M, Dhingra K, Hittelman WN. Aromatic DNA adducts in adjacent tissues of breast cancer patients: clues to breast cancer etiology. Cancer Res. 1996;56(2):287–93.
Abu-Bakar A, Tan BH, Halim H, Ramli, Pan Y, Ong CE. Cytochrome P450: role on carcinogenesis and relevance to cancers. Curr Drug Metab. 2022;23(5):355–73. https://doi.org/10.2174/1389200223666220328143828.
Kolluri SK, Weiss C, Koff A, Gottlicher M. p27(Kip1) induction and inhibition of proliferation by the intracellular Ah receptor in developing thymus and hepatoma cells. Genes Dev. 1999;13:1742–53. https://doi.org/10.1101/gad.13.13.1742.
Pang PH, Lin YH, Lee YH, Hou HH, Hsu SP, Juan SH. Molecular mechanisms of p21 and p27 induction by 3-methylcholanthrene, an aryl-hydrocarbon receptor agonist, involved in antiproliferation of human umbilical vascular endothelial cells. J Cell Physiol. 2008;215:161–71. https://doi.org/10.1002/jcp.21299.
Barhoover MA, Hall JM, Greenlee WF, Thomas RS. Aryl hydrocarbon receptor regulates cell cycle progression in human breast cancer cells via a functional interaction with cyclin-dependent kinase 4. Mol Pharmacol. 2010;77(2):195–201. https://doi.org/10.1124/mol.109.059675.
Shimba S, Komiyama K, Moro I, Tezuka M. Overexpression of the aryl hydrocarbon receptor (AhR) accelerates the cell proliferation of A549 cells. J Biochem. 2002;132(5):795–802. https://doi.org/10.1093/oxfordjournals.jbchem.a003289.
Vacher S, Castagnet P, Chemlali W, Lallemand F, Meseure D, Pocard M, et al. High AHR expression in breast tumors correlates with expression of genes from several signaling pathways namely inflammation and endogenous tryptophan metabolism. PLoS ONE. 2018;13(1):e0190619. https://doi.org/10.1371/journal.pone.0190619.
Minn AJ, Gupta GP, Siegel PM, Bos PD, Shu W, Giri DD, et al. Genes that mediate breast cancer metastasis to lung. Nature. 2005;436(7050):518–24. https://doi.org/10.1038/nature03799.
Han Z, Miwa Y, Obikane H, Mitsumata M, Takahashi-Yanaga F, Morimoto S, et al. Aryl hydrocarbon receptor mediates laminar fluid shear stress-induced CYP1A1 activation and cell cycle arrest in vascular endothelial cells. Cardiovasc Res. 2008;77:809–18. https://doi.org/10.1093/cvr/cvm095.
Conway DE, Sakurai Y, Weiss D, Vega JD, Taylor WR, Jo H, et al. Expression of CYP1A1 and CYP1B1 in human endothelial cells: regulation by fluid shear stress. Cardiovasc Res. 2009;81:669–77. https://doi.org/10.1093/cvr/cvn360.
Gearhart-Serna LM, Davis JB, Jolly MK, Jayasundara N, Sauer SJ, Di Giulio RT. A polycyclic aromatic hydrocarbon-enriched environmental chemical mixture enhances AhR, antiapoptotic signaling and a proliferative phenotype in breast cancer cells. Carcinogenesis. 2020;41(12):1648–59. https://doi.org/10.1093/carcin/bgaa047.
Liehr JG, Ulubelen AA, Strobel HW. Cytochrome P-450-mediated redox cycling of estrogens. J Biol Chem. 1986;261(36):16865–70.
Cavalieri E, Frenkel K, Liehr JG, Rogan E, Roy D. Estrogens as endogenous genotoxic agents: DNA adducts and mutations. J Natl Cancer Inst Monogr. 2000;27:75–93. https://doi.org/10.1093/oxfordjournals.jncimonographs.a024247.
Liehr JG. Role of DNA adducts in hormonal carcinogenesis. Regul Toxicol Pharmacol. 2000;32:276–82. https://doi.org/10.1006/rtph.2000.1432.
Vaclavikova R, Hubackova M, Stribrna-Sarmanova J, Kodet R, Mrhalova M, Novotny J, et al. RNA expression of cytochrome P450 in breast cancer patients. Anticancer Res. 2007;27(6 C):4443–50.
Leung T, Rajendran R, Singh S, Garva R, Krstic-Demonacos M, Demonacos C. Cytochrome P450 2E1 (CYP2E1) regulates the response to oxidative stress and migration of breast cancer cells. Breast Cancer Res. 2013;15(6):R107.
Jozkowicz A, Was H, Dulak J. Heme oxygenase-1 in tumors: is it a false friend? Antioxid Redox Signal. 2007;9(12):2099–117. https://doi.org/10.1089/ars.2007.1659.
Hirai K, Sasahira T, Ohmori H, Fujii K, Kuniyasu H. Inhibition of heme oxygenase-1 by zinc protoporphyrin IX reduces tumor growth of LL/2 lung cancer in C57BL mice. Int J Cancer. 2007;120:500–5. https://doi.org/10.1002/ijc.22287.
Hill M, Pereira V, Chauveau C, Zagani R, Remy S, Tesson L, et al. Heme oxygenase-1 inhibits rat and human breast cancer cell proliferation: mutual cross inhibition with indoleamine 2,3-dioxygenase. FASEB J. 2005;19:1957–68. https://doi.org/10.1096/fj.05-3875com.
Chen X, Kang K, Kroemer G, Tang D. Broadening horizons: the role of ferroptosis in cancer. Nat Rev Clin Oncol. 202;18(5):280–96. https://doi.org/10.1038/s41571-020-00462-0.
Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72. https://doi.org/10.1016/j.cell.2012.03.042.
Anandhan A, Dodson M, Schmidlin CJ, Liu P, Zhang DD. Breakdown of an ironclad defense system: the critical role of NRF2 in mediating ferroptosis. Cell Chem Biol. 2020;27(4):436–47. https://doi.org/10.1016/j.chembiol.2020.03.01.
Kwon MY, Park E, Lee SJ, Chung SW. Heme oxygenase-1 accelerates erastin-induced ferroptotic cell death. Oncotarget. 2015;6:24393–403. https://doi.org/10.18632/oncotarget.5162.
Chang LC, Chiang SK, Chen SE, Yu YL, Chou RH, Chang WC. Heme oxygenase-1 mediates BAY 11-7085 induced ferroptosis. Cancer Lett. 2018;416:124–37.
Hassannia B, Wiernicki B, Ingold I, Qu F, Van Herck S, Tyurina YY, et al. Nano-targeted induction of dual ferroptotic mechanisms eradicates high-risk neuroblastoma. J Clin Invest. 2018;128:3341–55.
Tew KD, Manevich Y, Grek C, Xiong Y, Uys J, Townsend DM. The role of glutathione S-transferase P in signaling pathways and S-glutathionylation in cancer. Free Radic Biol Med. 2011;51(2):299–313. https://doi.org/10.1016/j.freeradbiomed.2011.04.013.
Tan X, Huang X, Niu B, Guo X, Lei X, Qu B. Targeting GSTP1-dependent ferroptosis in lung cancer radiotherapy: existing evidence and future directions. Front Mol Biosci. 2022;9:1102158. https://doi.org/10.3389/fmolb.2022.1102158.
Peng Y, Ouyang L, Zhou Y, Lai W, Chen Y, Wang Z, et al. AhR promotes the development of non-small cell lung cancer by inducing SLC7A11-dependent antioxidant function. J Cancer. 2023;14(5):821–34. https://doi.org/10.7150/jca.82066.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SHIH, AAB, and MI contributed to the direction of the paper. MZIZ and NIAS updated hazard classification of the chemicals under the supervision of MI. NASZ conducted CTD data-mining and compilation networks images under the supervision of SH & AAB. All authors contribute to the writing of the manuscript and provided feedback in finalizing the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abu-Bakar, A., Ismail, M., Zulkifli, M.Z.I. et al. Mapping the influence of hydrocarbons mixture on molecular mechanisms, involved in breast and lung neoplasms: in silico toxicogenomic data-mining. Genes and Environ 46, 15 (2024). https://doi.org/10.1186/s41021-024-00310-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41021-024-00310-y