Abstract
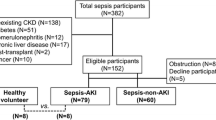
Sepsis due to microbial invasion often causes multiple organ failure (MOF), including acute kidney injury (AKI), with high mortality rates in serious cases. Hence, there is an urgent need for diagnostic biomarkers that can be used to rapidly, accurately, and easily detect sepsis to identify the condition early and guide the selection of appropriate treatment. Liver-type fatty acid-binding protein (L-FABP), which localizes in renal proximal tubules, is excreted into the urine in response to oxidative stress-induced tubular injury. Because of this mechanism, L-FABP has been reported to be a useful urinary biomarker not only for renal disease but also for the severity of sepsis. Based on this concept, we developed a new L-FABP point-of-care (POC) assay kit that can be used to rapidly measure human L-FABP in the urine to further improve the usefulness of this biomarker in clinical settings. In this review, we describe the molecular mechanisms of L-FABP, its clinical usefulness, and the performance of the POC assay kit.
Similar content being viewed by others
Background
Sepsis is a severe inflammatory response to microbial invasion of the bloodstream and causes multiple organ failure (MOF), including acute kidney injury (AKI). Serious cases of sepsis have a high mortality rate. The initial definition of sepsis was proposed in 1991 [1] and then revised in 2001 [2] and 2016 [3] by the sepsis definition task-force. The most recent definition emphasized the severity of organ failure, although previous definitions mainly focused on inflammation. Sepsis was defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” in the most recent revision [3]. Moreover, Systemic Inflammatory Response Syndrome (SIRS) criteria were excluded, and a new clinical score for multiple organ failure was proposed, named the quick sepsis-related organ failure assessment (qSOFA) criteria, which comprise the following: a high respiratory rate (≥22/min), altered mentation, and low systolic blood pressure (≤100 mmHg). With the qSOFA criteria, a blood test is not necessary, and the scoring is very simple and intuitive compared with the SIRS criteria. Thus, all medical staff can identify patients with infections who are likely to have a poor outcome by using the qSOFA at the bedside, and the patients can receive appropriate treatment at an early stage.
Therefore, diagnostic biomarkers that can be used to rapidly detect sepsis and MOF and predict its progression are needed. These biomarkers could guide early decisions regarding the appropriate treatment for sepsis. To date, more than 170 biomarkers for sepsis have been evaluated [4]. Among these biomarkers, C-reactive protein (CRP) and procalcitonin (PCT) are reported that these have been most widely used, but these biomarkers require broader validation before they can be incorporated into the clinical criteria describing sepsis [3]. Hence, there is an urgent need for diagnostic biomarkers that can be used to rapidly, accurately, and easily detect the severity of sepsis to identify the condition early and guide the selection of appropriate treatment.
Liver-type fatty acid-binding protein (L-FABP), which localizes in renal proximal tubules, is excreted into the urine during the response to tubular injury in renal disease [5]. L-FABP has been shown to be a useful urinary biomarker for the diagnosis of renal disease in the following clinical conditions: diabetic nephropathy [6,7,8,9], anemia [10], acute kidney injury (AKI) [11,12,13,14,15,16], pediatric AKI [17], contrast medium-induced nephropathy [18, 19], IgA nephropathy [20], human immunodeficiency virus (HIV)-associated nephropathy [21, 22], and reduced graft function in renal transplantation [23, 24]. Numerous AKI cohort studies have reported increased urinary levels of L-FABP in patients with septic shock-induced AKI [25,26,27,28]. In this review, we describe the molecular mechanisms of L-FABP in response to ischemic and oxidative stress, the clinical usefulness of urinary L-FABP for sepsis, and a new method for detecting L-FABP using a POC assay kit.
Molecular characteristics of L-FABP
Fatty acid-binding proteins (FABPs) are members of the intracellular lipid-binding protein family and are expressed as 14–15 kDa proteins; they reversibly bind to hydrophobic ligands such as fatty acids and function as intracellular transporters [29]. To date, nine human FABPs have been identified: L-FABP (or FABP1), intestinal FABP (I-FABP or FABP2), heart FABP (H-FABP or FABP3), adipocyte FABP (A-FABP or FABP4), epidermal FABP (E-FABP or FABP5), ileal FABP (Il-FABP or FABP6), brain FABP (B-FABP or FABP7), myelin FABP (M-FABP or FABP8), and testis FABP (T-FABP, FABP9). The structure of L-FABP includes ten stranded β-barrel structures that form interior hydrophobic ligand binding pockets and two α-helixes as cap domains [30] (Fig. 1). The l-fabp gene has binding domains for the following transcriptional factors: hypoxia inducible factor (HIF-1α and HIF-2α), caudal-related homeobox (CDX), CCAAT/enhancer-binding protein (C/EBP), forkhead box A (FOXA), GATA, hepatocyte nuclear factor (HNF-1 and HNF-4), and peroxisome proliferator-activated receptor (PPAR), which are related to cell proliferation, cell differentiation, and lipid metabolism [31,32,33]. Hence, it was concluded that L-FABP transports free fatty acids to organelles such as the mitochondria and lysosomes for β-oxidation for use in these cellular processes [34].
Ischemic and oxidative stress induces the excretion of L-FABP into the urine
Hypoxic regulation induces l-fabp gene expression by HIF-1α and HIF-2α [33]. To evaluate the response of L-FABP to hypoxic stress, the gene expression of l-fabp was measured in the LLC-PK1 porcine cell line, which was derived from proximal tubules, after the cells were cultured in hypoxic conditions using an anaerobic chamber. The results indicated that the expression level of l-fabp was increased by hypoxic stress (Fig. 2), demonstrating that L-FABP was a hypoxic-induced protein in proximal tubular cells [35].
Expression of the l-fabp gene following hypoxic stress. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as the housekeeping gene. The results of the RT-PCR analysis are shown in (a), and the quantified the expression levels are shown in (b) [35]
It was also reported that L-FABP was excreted into the urine following ischemic stress in vivo. Yamamoto T. and colleagues studied the association of peritubular capillary blood flow with the urinary excretion of L-FABP during reperfusion after living donor kidney transplantation [36]. They found that urinary L-FABP was inversely correlated with peritubular capillary blood flow (Fig. 3). This finding indicates that L-FABP is excreted into the proximal tubular lumen in response to ischemic and oxidative stress [36].
Correlation between ischemic stress and urinary L-FABP. a Correlation between peritubular capillary blood flow and urinary L-FABP. b Correlation between ischemic time and urinary L-FABP. R indicates correlation coefficient [36]
Antioxidative effect of L-FABP
The findings regarding the response of L-FABP to ischemic and oxidative stress led to the hypothesis that L-FABP itself has an antioxidative role. Hence, the association of reactive oxygen species (ROS) generation with l-fabp gene expression was evaluated, and it was found that L-FABP itself has an antioxidative property that is independent of the activities of superoxide dismutase (SOD), glutathione peroxidase (GPx), and catalase (CAT) [37, 38]. The antioxidative capacity was also demonstrated using an animal model in which the human l-fabp gene was expressed in the proximal tubules of transgenic mice (Tg-mice) [39]. Administration of aristolochic acid [40] and aldosterone [41], which induced ROS generation, promoted tubular injury and the urinary excretion of L-FABP. However, the oxidative markers Nε-hexanoyl lysine (HEL) and 2-thiobarbituric acid reactive substances (TBARS) were lower in the Tg-mice than in the wild type controls, indicating that the tubulointerstitial injury caused by ischemic and oxidative stress was attenuated by the antioxidative effect of L-FABP. The kidney contains a large amount of fatty acids, which can easily form lipid peroxides (LOOH), through peroxidation. Because L-FABP has high selectivity for fatty acids possessing long alkyl chains or carbon double bonds, or fatty acid peroxides [42,43,44] (Table 1), suggesting that L-FABP might protect the kidney by removing LOOH from the proximal tubules as shown in Fig. 4.
Schematic model for the urinary excretion of L-FABP. In the kidney, fatty acids are transferred into proximal tubules together with albumin. Free fatty acids bind to L-FABP and are relocated to the mitochondria, peroxisome, or nucleus. If lipid peroxidation products accumulate in the proximal tubules, L-FABP binds to those cytotoxic lipids and is excreted into the urine
Urinary L-FABP reflects the severity of sepsis
As mentioned above, L-FABP has an antioxidant capacity and is excreted into the urine in response to ischemic and oxidative stress. It has also been reported that endotoxin-induced oxidative stress in sepsis induces AKI in patients [45], suggesting that L-FABP would be excreted into the urine in these cases. Indeed, it was shown that the urinary L-FABP level was higher in patients with sepsis than in healthy controls [25, 26] (Table 2). It was noted that urinary L-FABP levels differed significantly among patients with septic shock, severe sepsis, or AKI and healthy subjects (as well as patients with an infectious disease or a non-infectious disease). An endotoxin removal cartridge (Toraymyxin) composed of a polymyxin B-immobilized fiber (PMX-F) was developed to apply to patients with endotoxemia or suspected gram-negative infection [46]. Our group also showed that PMX-F hemoperfusion decreased the plasma endotoxin level, urinary L-FABP level, and urinary 8-hydroxy-2′-deoxyguanosine (8-OHdG) level [25, 47]. Doi K et al. were also reported that in patients treated with PMX, the urinary L-FABP and blood endotoxin levels decreased in survivors but not in non-survivors [48].These reports suggested that the urinary L-FABP level might reflect the severity of the oxidative state in patients with sepsis and have value as an indicator of whether the treatment is successful.
Predicting poor outcomes
Several studies have reported the clinical significance of urinary L-FABP as a predictor of and risk factor for poor outcomes. Urinary L-FABP can predict the onset of AKI after cardiac surgery [13, 49, 50], pediatric cardiopulmonary bypass [17], stem cell transplantation [12], and endovascular and open-abdominal aortic aneurysm repair [16] as well as in intensive care unit populations [15]. Additionally, L-FABP can also predict the progression to end-stage renal disease (ESRD), the onset of cardiovascular disease (CVD), or death for patients with AKI [14, 51], type 2 diabetes [8, 52], or chronic kidney disease (CKD) [53] or those who have undergone cardiac catheterization [54, 55] or renal transplantation [56, 57]. Clinical prospective observation studies to predict mortality in sepsis using urinary L-FABP have been conducted with both adult patients and pediatric patients (Table 3) [27, 28]. A significant difference in the urinary L-FABP level in the first urine sample was observed between survivors and non-survivors in each study. In the ROC curve analysis, the area under the curve (AUC) values were 0.993 (95% CI, 0.956–0.999) for adult patients and 0.647 (95% CI, 0.500–0.795) for pediatric patients. Further improvement would be required before using L-FABP as a predictor of mortality in pediatric patients with sepsis, but it might be useful for adult patients because the AUC-ROC of urinary L-FABP was significantly higher than the acute physiology and chronic health evaluation (APACHE) II score (0.927) and sepsis-related organ failure assessment (SOFA) score (0.813) (Fig. 5) [27].
Mortality prediction using urinary L-FABP, APACHE II, and SOFA. Receiver operation characteristic curve analysis for the prediction of mortality was performed using patients with septic shock with AKI (n = 145, mortality rate = 47%) [27]
Animal models of sepsis
Animal models that mimic human sepsis have been developed, and their usefulness was reviewed by Doi K. et al. [58]. The diagnostic value of urinary L-FABP for sepsis has been evaluated in animal models of sepsis [27]. In this study, sepsis was induced by cecal ligation puncture (CLP) or intratracheal lipopolysaccharide (LPS) injection, causing mild tubular damage with vacuolization, an increase in bronchoalveolar lavage fluid protein, and leukocyte infiltration in the interstitial space of the lung. Urinary L-FABP was higher in the severe group than in the less severe group and sham-operated animals, suggesting it can indicate the severity of sepsis.
These reports indicate that urinary L-FABP might not only detect the severity of sepsis but also predict poor outcomes. Although, to date, there have been several reports on diagnosing sepsis using urinary L-FABP, additional studies are required to elucidate the usefulness of urinary L-FABP within the context of the new definition of sepsis.
POC assay kit for urinary L-FABP
In many studies, L-FABP was measured using the enzyme-linked immunosorbent assay (ELISA) method. However, this assay requires several hours, specialized equipment, and highly trained personnel to obtain reliable results. If L-FABP is to be used to diagnose sepsis, the method must be rapid, accurate, and easy to perform at the bedside. Therefore, we developed the L-FABP POC assay kit, which can rapidly measure human L-FABP in the urine.
Clinical significance of the POC assay for urinary L-FABP
The principles of the POC assay kit are shown as Fig. 6. The POC assay kit utilizes an immuno-chromatography method, and the result is obtained within 15 min. The POC assay and ELISA (CMIC HOLDINGS Co., Ltd., Tokyo, Japan) were performed on urine samples from two groups of patients: 35 patients who were admitted to the intensive care unit (ICU) at Shinmatsudo Central General Hospital (Chiba, Japan) as critically ill patients with sepsis (186 points) and 80 patients who were outpatients with CKD at St. Marianna University School of Medicine Hospital (Kanagawa, Japan) (106 points). When the ELISA and POC assay results were compared, the result of POC assay was assessed using three-score method, score 1; <12.5 ng/ml, score 2; ≥12.5 ng/ml and <100 ng/ml, or score 3; ≥ 100 ng/ml (Fig. 7). It is important to measure the higher range near 100 ng/ml for ICU patients because it was suggested that upper levels of urinary L-FABP than 100 μg/g Cr may be specific to septic shock [25]. Additionally, it is also important to measure the range near 12.5 ng/ml for CKD patients because it was reported that levels of urinary L-FABP above the upper limit of the reference value (8.4 μg/g Cr [6]) are a risk factor for the progression to ESRD, the onset of cardiovascular disease CVD, and death [53]. When we reanalyzed reference value to L-FABP concentration, the reference value which converted to L-FABP concentration was 10.1 ng/ml. Therefore, the assessment of the upper level of 12.5 ng/ml in POC assay indicated that urinary L-FABP/creatinine level was at least the upper level of 8.4 μg/g Cr.
L-FABP POC assay kit. a Schematic representation of the immuno-chromatographic assay. When the urine samples are applied to the sample pad, L-FABP proteins in the sample react with a gold colloid anti-human L-FABP mouse monoclonal antibody. The antigen-antibody complexes move in the assay bed by capillary action to a second anti-human L-FABP mouse monoclonal antibody situated on the test line, and the conjugate is visualized with a red line. b Color chart of the POC assay kit for quantitative measurements. The test line (T) and control line (C) were visualized within 15 min after applying the urine samples
Correlation between the ratio of urinary L-FABP to urinary creatinine and POC assay results. Urine samples from 35 patients who were admitted to the ICU (186 points) and from 80 patients who were outpatients with CKD (106 points) were measured with the ELISA test and POC assay. The test lines obtained with the POC assay were assessed using three-score method. The L-FABP/creatinine levels from the ELISA were log transformed, and the median and quartile values are presented with the score obtained with the POC assay. Statistical analysis was performed with the Mann-Whitney U test
The correlation between the ratio of urinary L-FABP to urinary creatinine and POC assay results and the accuracy of the L-FABP POC assay for diagnosis of the patients with sepsis or CKD was evaluated for clinical use. The ratio of urinary L-FABP to urinary creatinine for the ICU patients and the outpatients were determined and compared with the POC assay results. The results showed multi-group comparisons revealed significant differences in the L-FABP/creatinine levels between the results of the POC assay (Fig. 7). Additionally, it was found that the specificity (true negative ratio) and sensitivity (true positive ratio) to assess the reference value (8.4 μg/g Cr) were 99% (87/88) and 61% (125/204), respectively. Recently, Asada T. and colleagues reported that concentration of urinary L-FABP above the upper limit of the reference value (100 ng/ml) were defined as a risk factor of AKI in ICU patients [59]. This report supports the validity of the higher cutoff value of L-FABP (100 ng/ml) for diagnosis of AKI. Further evaluation is necessary to confirm the cutoff values of L-FABP. Moreover, Sato R. and colleagues reported that urinary L-FABP levels in ICU patients including those with sepsis were also measured using the POC assay [26]. They found a positive correlation between serum creatinine levels and POC assay score, suggesting that the L-FABP POC assay might be alternative method for assessing creatinine levels, which are widely used. These results indicate the potential of the POC assay for use in diagnosing sepsis-induced AKI and CKD in patients rapidly.
Clinical evaluation of POC assay for urinary L-FABP in PMX intervention
Clinical evaluation of the L-FABP POC assay kit was performed in PMX intervention.
The POC assay and ELISA (CMIC HOLDINGS Co., Ltd., Tokyo, Japan) were performed on urine samples from three patients who were admitted to the ICU at Shinmatsudo Central General Hospital (Chiba, Japan) as critically ill patient with sepsis. The lactate level which was described as the new criteria of sepsis in third international consensus definition for sepsis and septic shock (sepsis-3) was also evaluated at pre- and post-PMX intervention by the blood gas analyzer. In the result, the patient who is 84-year-old man had septic shock with transverse colon cancer after surgery suture failure. The lactate (mg/dl) and urinary L-FABP/creatinine (μg/g Cr) were decreased after PMX intervention. Moreover, the patient who is 93-year-old woman had septic shock with iliopsoas abscess. Similarly, the lactate and urinary L-FABP/creatinine were decreased after PMX intervention. The results of POC assay were assessed as score 3; ≥100 ng/ml at pre-1st PMX intervention and as score 1; <12.5 ng/ml at post-2nd PMX intervention in the patients (Fig. 8a, b). Urinary creatinine excretion was 78.6 and 112.7 mg/dl in pre-PMX and 117.3 and 220.1 mg/dl in post-PMX in two patients. These patients discharged from the hospital. In contrast, the patient who is a 75-year-old woman has septic shock with acute obstructive suppurative cholangitis. In the patient after PMX intervention, the lactate was decreased slightly, whereas the urinary L-FABP was increased. Also, the result of POC assay was assessed as score 2; ≥ 12.5 and <100 ng/ml at pre-PMX intervention, and as score 3; ≥100 ng/ml at post-PMX intervention (Fig. 8c). Urinary creatinine excretion was 78.6 mg/dl in pre-PMX and 19.1 mg/dl in post-PMX. The patient died after 3 days of PMX intervention. In this case, serum lactate and urinary L-FABP levels were sustained abnormal level in each point. In this sense, neither lactate value nor urine L-FABP value decreased by PMX intervention. Furthermore, another group developed a new algorithm by combining urinary NGAL and L-FABP with stratification by the APACHE II score, presence of sepsis and blood lactate levels to improve their AKI predictive performance [59]. From this report, it is also considered that there are cases in which it is difficult to make a prognostic prediction only by changes in urine L-FABP in a high concentration range. As a whole, when the score of POC assay for urinary L-FABP and lactate level were decreased in the patients after PMX intervention, the patient tended to improve the condition. On the other hand, when the score of POC assay and lactate were sustained high level in the patient even after PMX intervention, the patient tended to deteriorate the condition. Therefore, these results suggested that POC assay for urinary L-FABP may be useful to evaluate therapeutic efficacy of PMX intervention in sepsis patient.
Correlation between the ratio of urinary L-FABP to urinary creatinine, POC assay results and lactate levels in PMX-treated patients. Urine samples from three patients who were admitted to the ICU were measured with the ELISA test and POC assay. The test lines obtained with the POC assay kit were scored using three-score method. Lactate levels measured by the blood gas analyzer. Two patients had discharged from the hospital (a, b). Another patient died after 3 days of PMX intervention (c)
Conclusions
In conclusion, endotoxin induces oxidative stress and the excretion of L-FABP into the urine in patients with sepsis-induced AKI. If urinary L-FABP can be measured in these patients, it is possible to diagnose the severity of sepsis. However, to date, there is little evidence for the clinical usefulness of urinary L-FABP for sepsis. Further studies are required to elucidate the reliability of diagnostic methods using urinary L-FABP and to determine the cutoff values for predicting poor outcomes. The L-FABP POC assay kit is expected to be useful for its rapidness and simplicity. Our study was performed at a single center. Our findings should be confirmed in a large multicenter trial. Future studies need to be conducted.
Abbreviations
- A-FABP/FABP4:
-
Adipocyte-type fatty acid-binding protein
- AKI:
-
Acute kidney injury
- APACHE:
-
Acute physiology and chronic health evaluation
- AUC:
-
Area under the curve
- B-FABP/FABP7:
-
Brain-type fatty acid binding protein
- CAT:
-
Catalase
- CDX:
-
Caudal-related homeobox
- C/EBP:
-
CCAAT/enhancer-binding protein
- CKD:
-
Chronic kidney disease
- CLP:
-
Cecal ligation puncture
- Cr:
-
Creatinine
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- E-FABP/FABP5:
-
Epidermal-type fatty acid-binding protein
- ELISA:
-
Enzyme-linked immunosorbent assay
- ESRD:
-
End-stage renal disease
- FABPs:
-
Fatty acid-binding proteins
- FOXA:
-
Forkhead box A
- GPx:
-
Glutathione peroxidase
- HEL:
-
Nε-hexanoyl lysine
- HIF:
-
Hypoxia inducible factor
- HIV:
-
Human immunodeficiency virus
- H-FABP/FABP3:
-
Heart-type fatty acid-binding protein
- HNF:
-
Hepatocyte nuclear factor
- ICU:
-
Intensive care unit
- I-FABP/FABP2:
-
Intestinal-type fatty acid-binding protein
- Il-FABP/FABP6:
-
Ileal-type fatty acid binding protein
- L-FABP/FABP1:
-
Liver-type fatty acid-binding protein
- LOOH:
-
Lipid peroxides
- M-FABP/FABP8:
-
Myelin-type fatty acid-binding protein
- MOF:
-
Multiple organ failure
- 8-OHdG:
-
8-Hydroxy-2′-deoxyguanosine
- PCT:
-
Procalcitonin
- PPAR:
-
Peroxisome proliferator-activated receptor
- POC:
-
Point-of-care
- PMX-F:
-
Polymyxin B-immobilized fiber
- qSOFA:
-
Quick sepsis-related organ failure assessment
- ROC:
-
Receiver operatorating characteristic
- ROS:
-
Reactive oxygen species
- SIRS:
-
Systemic inflammatory response syndrome
- SOD:
-
Superoxide dismutase
- SOFA:
-
Sepsis-related organ failure assessment
- TBARS:
-
2-Thiobarbituric acid reactive substances
- T-FABP/FABP9:
-
Testis-type fatty acid-binding protein
- Tg-mice:
-
Transgenic mice
References
Bone R, Balk R, Cerra F, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine. Chest. 1992;101(6):1644–55.
Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med. 2003;29(4):530–8.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care. 2010;14(1):R15.
Kamijo A, Kimura K, Sugaya T, et al. Urinary fatty acid-binding protein as a new clinical marker of the progression of chronic renal disease. J Lab Clin Med. 2004;143(1):23–30.
Kamijo-Ikemori A, Sugaya T, Yasuda T, et al. Clinical significance of urinary liver-type fatty acid-binding protein in diabetic nephropathy of type 2 diabetic patients. Diabetes Care. 2011;34(3):691–6.
Nielsen SE, Sugaya T, Tarnow L, et al. Tubular and glomerular injury in diabetes and the impact of ACE inhibition. Diabetes Care. 2009;32(9):1684–8.
Fufaa GD, Weil EJ, Nelson RG, et al. Association of urinary KIM-1, L-FABP, NAG and NGAL with incident end-stage renal disease and mortality in American Indians with type 2 diabetes mellitus. Diabetologia. 2015;58(1):188–98.
Fu WJ, Wang DJ, Deng RT, et al. Urinary liver-type fatty acid-binding protein change in gestational diabetes mellitus. Diabetes Res Clin Pract. 2015;109(3):e36–8.
Imai N, Yasuda T, Kamijo-Ikemori A, et al. Distinct roles of urinary liver-type fatty acid-binding protein in non-diabetic patients with anemia. PLoS ONE. 2015;10(5):e0126990.
Matsui K, Kamijo-Ikemori A, Sugaya T, et al. Usefulness of urinary biomarkers in early detection of acute kidney injury after cardiac surgery in adults. Circ J. 2012;76(1):213–20.
Shingai N, Morito T, Najima Y, et al. Urinary liver-type fatty acid-binding protein linked with increased risk of acute kidney injury after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20(12):2010–4.
Portilla D, Dent C, Sugaya T, et al. Liver fatty acid-binding protein as a biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2008;73(4):465–72.
Parr SK, Clark AJ, Bian A, et al. Urinary L-FABP predicts poor outcomes in critically ill patients with early acute kidney injury. Kidney Int. 2014;87(3):640–8.
Doi K, Negishi K, Ishizu T, et al. Evaluation of new acute kidney injury biomarkers in a mixed intensive care unit. Crit Care Med. 2011;39(11):2464–9.
Obata Y, Kamijo-Ikemori A, Ichikawa D, et al. Clinical usefulness of urinary liver-type fatty-acid-binding protein as a perioperative marker of acute kidney injury in patients undergoing endovascular or open-abdominal aortic aneurysm repair. J Anesth. 2016;30(1):89–99.
Krawczeski CD, Goldstein SL, Woo JG, et al. Temporal relationship and predictive value of urinary acute kidney injury biomarkers after pediatric cardiopulmonary bypass. J Am Coll Cardiol. 2011;58(22):2301–9.
Manabe K, Kamihata H, Motohiro M, et al. Urinary liver-type fatty acid-binding protein level as a predictive biomarker of contrast-induced acute kidney injury. Eur J Clin Invest. 2012;42(5):557–63.
Nakamura T, Sugaya T, Node K, et al. Urinary excretion of liver-type fatty acid-binding protein in contrast medium-induced nephropathy. Am J Kidney Dis. 2006;47(3):439–44.
Nakamura T, Sugaya T, Ebihara I, et al. Urinary liver-type fatty acid-binding protein: discrimination between IgA nephropathy and thin basement membrane nephropathy. Am J Nephrol. 2005;25(5):447–50.
Jablonowska E, Wojcik K, Piekarska A. Urine liver-type fatty acid-binding protein and kidney injury molecule-1 in HIV-infected patients receiving combined antiretroviral treatment based on tenofovir. AIDS Res Hum Retroviruses. 2014;30(4):363–9.
Peralta C, Scherzer R, Grunfeld C, et al. Urinary biomarkers of kidney injury are associated with all-cause mortality in the Women’s Interagency HIV Study (WIHS). HIV Med. 2014;15(5):291–300.
Parikh CR, Hall IE, Bhangoo RS, et al. Associations of perfusate biomarkers and pump parameters with delayed graft function and deceased-donor kidney allograft function. Am J Transplant. 2016;16(5):1526–39.
Koo TY, Jeong JC, Lee Y, et al. Pre-transplant evaluation of donor urinary biomarkers can predict reduced graft function after deceased donor kidney transplantation. Medicine (Baltimore). 2016;95(11):e3076.
Nakamura T, Sugaya T, Koide H. Urinary liver-type fatty acid-binding protein in septic shock: effect of polymyxin B-immobilized fiber hemoperfusion. Shock. 2009;31(5):454–9.
Sato R, Suzuki Y, Takahashi G, et al. A newly developed kit for the measurement of urinary liver-type fatty acid-binding protein as a biomarker for acute kidney injury in patients with critical care. J Infect Chemother. 2014;21(3):165–9.
Doi K, Noiri E, Maeda-Mamiya R, et al. Urinary l-type fatty acid-binding protein as a new biomarker of sepsis complicated with acute kidney injury. Crit Care Med. 2010;38(10):2037–42.
Yoshimatsu S, Sugaya T, Hossain MI, et al. Urinary L-FABP as a mortality predictor among <5-year-old children with septic children in Bangladesh. Pediatr Int. 2016;58(3):185–91.
Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov. 2008;7(6):489–503.
Cai J, Lucke C, Chen Z, et al. Solution structure and backbone dynamics of human liver fatty acid binding protein: fatty acid binding revisited. Biophys J. 2012;102(11):2585–94.
Divine JK. McCaul SP. Simon T. C. HNF-1alpha and endodermal transcription factors cooperatively activate fabpl: MODY3 mutations abrogate cooperativity. Am J Physiol Gastrointest Liver Physiol. 2003;285(1):G62-72.
Schachtrup C, Scholzen TE, Grau V, et al. L-FABP is exclusively expressed in alveolar macrophages within the myeloid lineage: evidence for a PPARalpha-independent expression. Int J Biochem Cell Biol. 2004;36(10):2042–53.
Jadoon A, Cunningham P, McDermott LC. Regulation of fatty acid binding proteins by hypoxia inducible factors 1alpha and 2alpha in the placenta: relevance to pre-eclampsia. Prostaglandins Leukot Essent Fatty Acids. 2015;93:25–9.
Veerkamp JH, Zimmerman AW. Fatty acid-binding proteins of nervous tissue. J Mol Neurosci. 2001;16(2-3):133–42. discussion 151-7.
Okazaki M, Oikawa T, Sugaya T. The biomarker for CKD: urinary L-FABP-from molecular function to clinical significance. Nihon Yakurigaku Zasshi. 2015;146(1):27–32.
Yamamoto T, Noiri E, Ono Y, et al. Renal L-type fatty acid-binding protein in acute ischemic injury. J Am Soc Nephrol. 2007;18(11):2894–902.
Wang G, Gong Y, Anderson J, et al. Antioxidative function of L-FABP in L-FABP stably transfected chang liver cells. Hepatology. 2005;42(4):871–9.
Rajaraman G, Wang GQ, Yan J, et al. Role of cytosolic liver fatty acid binding protein in hepatocellular oxidative stress: effect of dexamethasone and clofibrate treatment. Mol Cell Biochem. 2007;295(1-2):27–34.
Kamijo A, Sugaya T, Hikawa A, et al. Urinary excretion of fatty acid-binding protein reflects stress overload on the proximal tubules. Am J Pathol. 2004;165(4):1243–55.
Matsui K, Kamijo-Ikemorif A, Sugaya T, et al. Renal liver-type fatty acid binding protein (L-FABP) attenuates acute kidney injury in aristolochic acid nephrotoxicity. Am J Pathol. 2011;178(3):1021–32.
Ichikawa D, Kamijo-Ikemori A, Sugaya T, et al. Human liver-type fatty acid-binding protein protects against tubulointerstitial injury in aldosterone-induced renal injury. Am J Physiol Renal Physiol. 2014;308(2):F114–121.
Zimmerman AW, van Moerkerk HT, Veerkamp JH. Ligand specificity and conformational stability of human fatty acid-binding proteins. Int J Biochem Cell Biol. 2001;33(9):865–76.
Norris AW, Spector AA. Very long chain n-3 and n-6 polyunsaturated fatty acids bind strongly to liver fatty acid-binding protein. J Lipid Res. 2002;43(4):646–53.
Raza H, Pongubala JR, Sorof S. Specific high affinity binding of lipoxygenase metabolites of arachidonic acid by liver fatty acid binding protein. Biochem Biophys Res Commun. 1989;161(2):448–55.
Kalakeche R, Hato T, Rhodes G, et al. Endotoxin uptake by S1 proximal tubular segment causes oxidative stress in the downstream S2 segment. J Am Soc Nephrol. 2011;22(8):1505–16.
Shoji H. Extracorporeal endotoxin removal for the treatment of sepsis: endotoxin adsorption cartridge (Toraymyxin). Ther Apher Dial. 2003;7(1):108–14.
Nakamura T, Fujiwara N, Sato E, et al. Effect of polymyxin B-immobilized fiber hemoperfusion on serum high mobility group box-1 protein levels and oxidative stress in patients with acute respiratory distress syndrome. ASAIO J. 2009;55(4):395–9.
Doi K, Noiri E, Sugaya T. Urinary l-type fatty acid-binding protein as a new renal biomarker in critical care. Curr Opin Crit Care. 2010;16(6):545–9.
Ho J, Tangri N, Komenda P, et al. Urinary, plasma, and serum biomarkers’ utility for predicting acute kidney injury associated with cardiac surgery in adults: a meta-analysis. Am J Kidney Dis. 2015;66(6):993–1005.
Katagiri D, Doi K, Honda K, et al. Combination of two urinary biomarkers predicts acute kidney injury after adult cardiac surgery. Ann Thorac Surg. 2012;93(2):577–83.
Cooper DS, Claes D, Goldstein SL, et al. Follow-up renal assessment of injury long-term after acute kidney injury (FRAIL-AKI). Clin J Am Soc Nephrol. 2016;11(1):21–9.
Araki S, Haneda M, Koya D, et al. Predictive effects of urinary liver-type fatty acid-binding protein for deteriorating renal function and incidence of cardiovascular disease in type 2 diabetic patients without advanced nephropathy. Diabetes Care. 2013;36(5):1248–53.
Matsui K, Kamijo-Ikemori A, Imai N, et al. Clinical significance of urinary liver-type fatty acid-binding protein as a predictor of ESRD and CVD in patients with CKD. Clin Exp Nephrol. 2016;20(2):195–203.
Fujita D, Takahashi M, Doi K, et al. Response of urinary liver-type fatty acid-binding protein to contrast media administration has a potential to predict one-year renal outcome in patients with ischemic heart disease. Heart Vessels. 2015;30(3):296–303.
Kamijo-Ikemori A, Hashimoto N, Sugaya T, et al. Elevation of urinary liver-type fatty acid binding protein after cardiac catheterization related to cardiovascular events. Int J Nephrol Renovasc Dis. 2015;8:91–9.
Bansal N, Carpenter MA, Weiner DE, et al. Urine injury biomarkers and risk of adverse outcomes in recipients of prevalent kidney transplants: the folic acid for vascular outcome reduction in transplantation trial. J Am Soc Nephrol. 2016;27(7):2109–21.
Yang J, Choi HM, Seo MY, et al. Urine liver-type fatty acid-binding protein predicts graft outcome up to 2 years after kidney transplantation. Transplant Proc. 2014;46(2):376–80.
Doi K, Leelahavanichkul A, Yuen PS, et al. Animal models of sepsis and sepsis-induced kidney injury. J Clin Invest. 2009;119(10):2868–78.
Asada T, Isshiki R, Hayase N, et al. Impact of clinical context on acute kidney injury biomarker performances: differences between neutrophil gelatinase-associated lipocalin and L-type fatty acid-binding protein. Sci Rep. 2016;6:33077.
Acknowledgements
We also would like to thank Editage (http://www.editage.jp/) for English language editing.
Funding
There is no funding to be disclosed.
Availability of data and materials
Not applicable.
Authors’ contributions
ES, AK-I, TS, KK, TN, and YS contributed to the study design. AO, TO, AK-I, and ES performed the data collection. ES, TO, and TS participated in the data analysis. ES, AK-I, TO, TS, and TN interpreted the data. ES and TO carried out the literature search and generation of figures. ES and TO wrote the manuscript. All authors gave their final approval of the submitted version.
Competing interests
T. Sugaya is the Director and Senior scientist, and T. Oikawa and A. Okuda are the scientist of CMIC HOLDINGS Co., Ltd., the company that produced the ELISA and POC assay for L-FABP analysis.
None of the other authors have competing interest or financial disclosures of any relevance to the present study.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Our study received approval from the ethic examination of the ethics committee of St. Marianna University School of Medicine on November 11, 2014 (accept no. 2856). We obtained written informed consent from the subjects and registered them as study subjects.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sato, E., Kamijo-Ikemori, A., Oikawa, T. et al. Urinary excretion of liver-type fatty acid-binding protein reflects the severity of sepsis. Ren Replace Ther 3, 26 (2017). https://doi.org/10.1186/s41100-017-0107-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-017-0107-x