Abstract
Background
Epilepsy is a brain disorder affecting nearly 65 million people worldwide. It is characterized by sudden, transient, and uncontrolled episodes of brain dysfunction secondary to hypersynchronous abnormal discharge of cortical neuronal cells resulting in motor, sensory, and behavioral manifestations. Cognitive deterioration can occur in approximately 70–80% of epileptic patients with a variety of epilepsy-related characteristics being implicated. This study aimed to assess cognitive functions in a sample of patients with generalized tonic–clonic epilepsy and determine its relation to different epilepsy-related characteristics. It was designed as a case–control cross-sectional study in which 106 participants were enrolled and divided into two groups: a case group of fifty-three patients diagnosed with generalized tonic–clonic epilepsy and a control group including fifty-three healthy subjects. Sociodemographic and epilepsy-related characteristics and a variety of cognitive functions were assessed for both groups.
Results
Epileptic patients were significantly suffering from impairment in attention, memory, visuospatial (P = 0.001), and language functions (P = 0.018) compared to the healthy control group.
Conclusions
Epileptic patients are significantly suffering from cognitive impairment with a variety of contributing epilepsy-related characteristics.
Similar content being viewed by others
Background
Epilepsy is defined as a brain disorder generating epileptic seizures; it is associated with neurobiological, cognitive, psychological, and social outcomes [1]. Epilepsy is a common neurological disorder affecting 65 million patients worldwide with its lifetime prevalence rate among the Egyptian population being 12.67/1000 [2]. Frequent and recurrent epileptic seizures lead to irreversible damage to the brain which may cause cognitive changes [3]. Cognitive impairment is noticed in 70–80% of epileptic patients; it includes memory loss, cognitive slowing, and attention deficits negatively affecting multiple daily functions [4]. It is reported that cognitive impairment in epilepsy is related to multiple factors including organic brain lesions, uncontrolled seizures, drug treatment, and previous individual mental abilities [5]. Cognitive dysfunction may be present even before a first epileptic seizure indicating a bidirectional nature of cognitive impairment in epilepsy [6]. This study aimed to assess cognitive functions in a sample of patients with generalized tonic–clonic epilepsy in relation to different epilepsy-related characteristics.
Methods
Participants and procedures
A case–control cross-sectional study which started from December 2020 to June 2021 was done in which 106 participants were enrolled and divided into two groups:
-
Case group including fifty-three patients diagnosed with generalized tonic–clonic epilepsy who were attending the psychiatry and neurology outpatient clinic of Suez Canal University teaching hospital for follow-up.
Patients older than 18 years, from both genders, and who can read and write were included while those with a history of comorbid physical and other neurological or psychiatric disorders were excluded.
-
Control group including fifty-three healthy employees matching the case group regarding sociodemographic characteristics were recruited from different hospital departments.
The sample size was calculated according to the proportion of cognitive impairment among epileptic patients being 60%, absolute error of precision usually equals 10%, and the confidence interval as 1.96. The calculated sample size was 96 participants, but after adding the expected (drop-out) rate (10%), the final sample size was 106 participants [7].
Tools
The following data were gathered from both study groups in the psychiatry and neurology outpatient clinic on the course of two appointments 1 week apart:
-
Sociodemographic data including age, sex, marital status, socioeconomic status, educational level, and occupation
-
Epilepsy-related characteristics including duration of epilepsy, seizure frequency per year, duration of treatment, and number of antiepileptic medications patients are receiving
-
Psychiatric interviewing was done using M.I.N.I.—a brief structured diagnostic interview—for exclusion of current major psychiatric disorders
-
Assessment of a variety of cognitive functions was done as follows:
-
Attention
The WAIS digit span subtest was used. The test has two parts: in the first part (digits forward), participants were told a series of numbers and asked to say them back to the examiner. In the second part (digits reversed), they were told a series of numbers but this time they were asked to say them back to the examiner in reverse order. The maximum score is 17.
-
Working memory
The WAIS digit span and arithmetic subtests were both used to asses working memory. The arithmetic test consists of a series of mental arithmetic questions such as the following: If someone has 13 apples, he decided to eat 5 and give away another 2 so how many apples are left? The test has a maximum score of 14 and was designed to measure a number of mental tasks including the ability to hold information in memory while it is being used.
-
Language
The WAIS vocabulary subtest was used where participants were presented with words and asked to define them. The test has a maximum score of 42 and was developed to measure word knowledge and verbal concept formation.
The WAIS similarities subtest was also used in which participants were presented with two words and asked how they are alike; for example, they were asked how a banana and an apple are alike. The test has a maximum score of 24 and is designed to assess verbal reasoning and concept development.
The verbal fluency test was used as a screening instrument of general verbal functioning. It is a short test where participants are given 1 min to produce as many different words as possible within a semantic category (category fluency) or starting with a given letter (letter fluency). The participant’s score in each task is the number of different correct words.
-
Visuospatial orientation
The WAIS block design subtest was used where participants were required to copy a pattern using colored blocks. The test has a maximum score of 42 and was designed to assess an individual’s ability to understand complex visual information.
The WAIS digit symbol subtest was also used where participants were given a series of double boxes with a number given in the upper part. The task is to draw a symbol relevant to this number into the lower part of the boxes. Nine fixed pairs of numbers and symbols were given at the top of the test sheet. The test result is the number of boxes correctly filled within 90 s and 67 is the maximum score.
-
Statistical analysis
The data were coded and imported into the Statistical Package for the Social Sciences (SPSS version 25) software. Data normality of distribution was tested before data analysis. All studied variables were expressed as means, standard deviations, and percentages. The chi-square test, independent samples t-test, and logistic regression explained the study results. The results were considered significant if the P value was ≤ 0.05.
Results
Nearly two-thirds of the epileptic group were males (56.6%), the mean age was 27.6 ± 6.6, and 64.2% were of middle socioeconomic status. Most of them were diagnosed with epilepsy and were receiving treatment for more than 10 years: 54.7% and 75.5% respectively. No statistically significant difference between both case and control groups was found regarding sociodemographic characteristics (Table 1).
The epileptic group was significantly suffering from cognitive impairment compared to the control group regarding a variety of cognitive functions: attention (P > 0.001), working memory (P > 0.001), language (P = 0.018), and visuospatial orientation (P = 0.021) (Table 2).
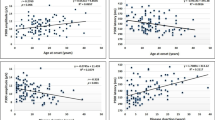
Impairment of attention and working memory among epileptic patients was significantly related to a variety of epilepsy-related characteristics including duration of epilepsy (P = 0.013), seizure frequency per year (P = 0.001), and duration of treatment (P = 0.044). However, impairment of language functions and visuospatial orientation was significantly related only to seizure frequency per year (P = 0.008) (Table 3).
Seizure frequency per year was the most epilepsy-related characteristic predictive of cognitive impairment in epileptic patients as shown by regression analysis of all statistically significant related-epileptic characteristics (Table 4).
Discussion
This study aimed to assess cognitive functions in a sample of patients diagnosed with generalized tonic–clonic epilepsy and determine its relation with different epilepsy-related characteristics. Our findings showed that patients with epilepsy were significantly suffering from cognitive impairment compared to healthy subjects. More than 80% of examined patients were having impairment in attention, memory, language, and visuospatial functions. Different epilepsy-related characteristics were significantly related to cognitive impairment in examined patients including duration of epilepsy, duration of treatment, and more importantly frequency of seizures per year which was found to be the most predictive epilepsy-related characteristic significantly related to impairment in all examined cognitive domains.
Epilepsy is a group of neurological disorders characterized by frequent seizures; its prevalence is 1% of the general population and is mostly present in the developing world. Cognition is the mental process of acquiring knowledge and experience utilizing the senses of attention, memory, judgment, problem solving, decision-making, comprehension, and language functions [8].
Cognitive impairment can occur in nearly 70–80% of patients with epilepsy [5]. It includes memory impairment and deficits in attention, executive, and language functions [9]. Previous studies found that multiple factors affect cognitive functions in epileptic patients including epilepsy itself, treatment of epilepsy, psychosocial consequences of epilepsy such as stigma and marginalization, structural brain deficits, and individual reserve abilities. Animal models of epilepsy showed that epileptic seizures have a negative effect on brain structure and behavior [10].
The nature of brain damage is related to the number, duration, and severity of epileptic seizures. Ictal and postictal cognitive impairment is reversible; however, a higher frequency of seizures causes a progressive mental decline in patients with chronic uncontrolled epilepsy [11].
Seizures lead to cellular and metabolic changes together with neuronal loss in the hippocampus, neoneurogenesis, and synaptic reorganization causing behavioral and cognitive impairment that gets worse with the cumulative number of seizures over time [12].
Cognitive dysfunction may be evident even before the onset of seizures. In a study assessing cognition in a sample of patients with newly diagnosed, untreated epilepsy, there was nearly 75% having deficits in attention, executive functions, and memory [13]. This indicates that comorbidity does not always indicate causality and that a bidirectional concept of cognitive impairment in patients with epilepsy should rather be adopted [14].
Similar to our findings, Seidenberg et al. indicated that the duration of epilepsy is related to cognitive impairment after 3 to 4 years of onset in children and adults diagnosed with epilepsy [15].
Also, a case–control study including epileptic patients and age/sex-matched healthy controls from July to September 2017 in Bilomo, sub-Saharan Africa, found the prevalence of cognitive impairment was much higher in epileptic patients—especially executive functions and verbal fluency—compared to healthy controls. Longer disease duration and higher seizure frequency were significantly associated with poor cognitive performance [16].
Different studies have found conflicting results regarding seizure control and cognitive impairment. A study in which a wide range of tests exploring memory were applied to seventy-one patients with unilateral mesial temporal epilepsy after being divided into two groups—according to seizure frequency—while other epilepsy-related characteristics such as lateralization, type of lesion, age of onset, duration of seizures, etiologic factors, and number of currently administered antiepileptic medications were controlled found that the low seizure frequency group was significantly better than the high seizure frequency group on anterograde memory tests. This suggests that high seizure frequency, on its own, potentiates the effects of mesial temporal lobe damage on memory impairment [17].
Meanwhile, in another study to assess the impact of seizure frequency on cognitive performance of adult epileptic patients in a rural community in South Eastern Nigeria, the control group performed better in almost all neurocognitive tests when compared with low seizure frequency and high seizure frequency groups.
However, the high seizure frequency group patients showed a significantly greater risk of memory impairment but not as in other neurocognitive domains compared with the low seizure frequency group indicating that while adults with epilepsy performed poorly in a wide range of neurocognitive functions, there was no significant adverse effect of higher seizure frequency observed on neurocognitive functions other than memory [18].
This study highlights the importance of epilepsy-related characteristics in the management of patients with epilepsy where proper seizure control had been found as an important predictor of the cognitive status of epileptic patients. Also, it showed the importance of early screening for cognitive impairment in patients with epilepsy that should go hand to hand with their treatment follow-up, and this should improve the overall quality of life in patients with epilepsy.
Conclusions
Patients with epilepsy are significantly suffering from cognitive impairment with a variety of epilepsy-related characteristics being implicated. Frequent seizures are the most predictive characteristic of significant cognitive impairment.
Availability of data and materials
All data generated or analyzed during this study are available on request.
Abbreviations
- WAIS:
-
Wechsler Adult Intelligence Scale
- M.I.N.I:
-
Mini-International Neuropsychiatric Interview
References
Çelik AÖ, Pınar KURT, Yener G, Alkin T, Öztura İ, Baklan B (2015) Comparison of cognitive impairment between patients having epilepsy and psychogenic nonepileptic seizures. Nöro Psikiyatri Arşivi 52(2):163
Khedr EM, Shawky OA, Ahmed MA, Elfetoh NA, Al Attar G, Ali AM, Farweez H (2013) A community based epidemiological study of epilepsy in Assiut Governorate/Egypt. Epilepsy research. 103(2–3):294–302
Hermann BP, Dabbs K, Becker T, Jones JE, JE Myers y Gutierrez A, Wendt G, Seidenberg M (2010) Brain development in children with new onset epilepsy: a prospective controlled cohort investigation. Epilepsia 51(10):2038–2046
Lodhi S, Agrawal N (2012) Neurocognitive problems in epilepsy. Adv Psychiatr Treat 18(3):232–240
Elger CE, Helmstaedter C, Kurthen M (2004) Chronic epilepsy and cognition. Lancet Neurology 3(11):663–672
Witt JA, Helmstaedter C (2012) Should cognition be screened in new-onset epilepsies? A study in 247 untreated patients. J Neurol 259(8):1727–1731
Charan J, Biswas T (2013) How to calculate sample size for different study designs in medical research? Indian J Psychol Med 35(2):121–126
Helmstaedter C (2013) The impact of epilepsy on cognitive function. J Neurol Neurosurg Psychiatry 84(9):e1–e1
Cerminara C, D’Agati E, Casarelli L, Kaunzinger I, Lange KW, Pitzianti M, Curatolo P (2013) Attention impairment in childhood absence epilepsy: an impulsivity problem? Epilepsy Behav. 27(2):337–341
Sutula TP, Hagen J, Pitkänen A (2003) Do epileptic seizures damage the brain? Curr Opin Neurol 16(2):189–195
Lado FA, Laureta EC, Moshé SL (2002) Seizure-induced hippocampal damage in the mature and immature brain. Epileptic Disord 4(2):83–97
Lukoyanov NV, Sá MJ, Madeira MD, Paula-Barbosa MM (2004) Selective loss of hilar neurons and impairment of initial learning in rats after repeated administration of electroconvulsive shock seizures. Exp Brain Res 154(2):192–200
Witt JA, Helmstaedter C (2012) Should cognition be screened in new-onset epilepsies? A study in 247 untreated patients. J Neurol 259(8):1727–1731
Abdellatif MG, Morad OAR, Arafa AG, Amin AE (2019) Cognitive implications in epilepsy. Sohag Medical Journal 24(1):57–63
Seidenberg M, Pulsipher DT, Hermann B (2007) Cognitive progression in epilepsy. Neuropsychol Rev 17(4):445–454
Njamnshi AK, Chokote ES, Ngarka L, Nfor LN, Tabah EN, Atchou JGB, Ruffieux N (2020) Epilepsy-associated neurocognitive disorders (EAND) in an onchocerciasis-endemic rural community in Cameroon: a population-based case–control study. Epilepsy Behav. 112:107437
Voltzenlogel V, Vignal JP, Hirsch E, Manning L (2014) The influence of seizure frequency on anterograde and remote memory in mesial temporal lobe epilepsy. Seizure 23(9):792–798
Arinzechi EO, Ogunrin OA, Nwosu CM, Nwani PO, Enwereji KO, Asomugha LA, Dimkpa U (2019) Seizure frequency and risk of cognitive impairment in people living with epilepsy in a sub-urban community in South Eastern Nigeria. J Clin Neurosci 59:98–105
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
NS and SA recruited the participants, analyzed and interpreted the data, and were the contributors in writing the manuscript. MA and AH revised the data interpretation and read and approved the final manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethical Committee Board of the Faculty of Medicine, Suez Canal University. The reference number is 4393/30–11-2020. Methods were performed following the principles of the Declaration of Helsinki (2000 revision). Written informed consent was obtained from all participants after explaining the purpose of the study.
Consent for publication
The participants consented to publishing their data results.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sayed, N.M., Aldin, M.T.K., Ali, S.E. et al. Cognitive functions and epilepsy-related characteristics in patients with generalized tonic–clonic epilepsy: a cross-sectional study. Middle East Curr Psychiatry 30, 15 (2023). https://doi.org/10.1186/s43045-023-00293-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43045-023-00293-6