Abstract
Background
Aim is to analyze alterations in third and fourth corneal higher-order aberrations using a ray tracing aberrometer (iTrace) induced by SMILE (small incision lenticule extraction) refractive surgery on Algerian patients; and also to investigate how corneal aberrations vary with spherical equivalent (SE), corneal central thickness (CCT), and age. Design Prospective, non-randomized case series that were carried out at the Chiali Smile Center, Algiers, Algeria.
Participants
A total of 219 eyes from 110 myopic patients, with and without astigmatism, successfully concluded the ultimate follow-up. Participants exhibited an average age of 32.48 years, with preoperative mean corneal high-order aberrations (CHOA) measuring 0.005 ± 0.036 μm.
Methods
A tracking trend analysis of high-order aberrations (HOAs) was conducted on the three groups of patients, assessing total corneal high-order aberrations after SMILE over periods of two, six, and twelve months.
Results
A substantial increase in total corneal high-order aberrations following SMILE, with a P value < 0.05. Conversely, there was a noteworthy and significant decrease in vertical trefoil for all groups (P value = 0.000). Interestingly, the corneal higher-order aberrations were more pronounced after two months compared to the six and twelve-month intervals. Spherical aberration demonstrated a significant increase with the extent of preoperative myopia and preoperative spherical equivalent both before and after SMILE surgery (P < 0.05), particularly in cases of high myopia. Moreover, there were significant reductions in preoperative and postoperative vertical coma (P = 0.047, P = 0.004, respectively) corresponding to the degree of preoperative myopia, with a more substantial decrease in vertical coma observed in cases of low myopia.
Conclusion
In the post-SMILE period, a notable increase in vertical coma and spherical aberrations was observed, accompanied by a significant decrease in vertical trefoil across all eyes. These aberration changes were identified to be closely associated with the spherical equivalent.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.1 Background
The aberrations inherent to the human eye, commonly denoted as high-order aberrations (HOAs), hold a central significance in diminishing retinal image quality. HOAs include a range of complex distortions such as coma, trefoil, and spherical aberration that cannot be corrected with conventional lenses [1, 2]. Numerous studies have delved into the exploration of ocular aberrations, employing diverse methodologies such as Hartmann–Shack wavefront sensing, Tscherning aberroscopy, and ray tracing refractometry. These methods have their unique advantages and limitations, with the iTrace aberrometer, utilizing ray tracing, standing out by measuring both the objective accommodative response and wavefront aberrations at varying distances [3,4,5].
Following corneal refractive surgeries, there is a documented increase in HOAs, significantly impacting patients' visual quality. LASIK (Laser-Assisted In Situ Keratomileusis) and PRK (Photorefractive Keratometry), for instance, have been shown to increase HOAs, which can lead to symptoms such as glare and halos, especially under low-light conditions. The assessment of alterations in wavefront aberrations serves as a critical measure for assessing the impact of refractive surgery on the quality of vision [6].
SMILE (small incision lenticule extraction), a recently devised corneal refractive correction technique, stands out as a minimally invasive alternative to LASIK and FS-LASIK (Femtosecond Laser-Assisted In Situ Keratomileusis), necessitating solely a minimal incision. This technique involves creating a lenticule within the corneal stroma, which is then extracted through a small incision, thus preserving the anterior corneal integrity [7,8,9]. Recent studies affirm the excellence of the SMILE procedure in terms of safety, predictability, efficacy, and postoperative ocular surface health. These studies highlight the reduced incidence of dry eye syndrome and faster recovery of corneal sensitivity compared to LASIK [10,11,12].
While previous studies on corneal HOAs post-SMILE have predominantly focused on anterior or total corneal HOAs, there is a scarcity of research comparing anterior, posterior, and total corneal HOAs concerning procedures addressing refractive errors. This gap in the literature suggests a need for comprehensive studies to understand the complete impact of SMILE on corneal HOAs [11,12,13,14].
In this prospective investigation, a comprehensive analysis of total corneal HOAs was undertaken both pre- and post-SMILE refractive surgery in eyes affected by myopia and myopic astigmatism. This study is significant because it aims to provide new insights into the impact of SMILE surgery on corneal HOAs, which are critical for understanding visual quality outcomes. Factors such as the degree of myopia, age, and corneal central thickness (CCT) measured with a topographer Oculus Pentacam, were considered. This exploration into the changes induced by SMILE in corneal HOAs in myopic eyes is an original contribution within the Algerian population. It is a distinctive endeavor conducted solely by a specialized SMILE surgeon in Algeria.
2 Methods
2.1 Participants
A prospective observational study encompassed 110 patients (219 eyes) who underwent SMILE at the Chiali Smile Center in Algiers, Algeria, between March 2018 and August 2021. One eye was excluded because it had high myopia greater than -10.00 diopters, which exceeds the correction limit of SMILE surgery.
The study spanned an average follow-up period of 6.26 ± 4.28 months. The time frame in this study is related to the postoperative follow-up of the cases. Patients were followed at different intervals after the SMILE surgery to assess both short-term and long-term outcomes. The follow-up periods were set at 2 months, 6 months, and 1 year, allowing for a comprehensive evaluation of changes and visual outcomes post-surgery. This rigorous follow-up schedule is essential to understanding the evolution of corneal HOAs and the overall visual quality in patients after the procedure.
Inclusion criteria comprised individuals aged 22 years or older dissatisfied with glasses or contact lenses, possessing a refraction spherical equivalent spanning from − 1.38 to − 11.50 D, a sphere of − 0.50 to − 10.00 D, and a cylinder of 0 to − 4.50 D. Furthermore, participants were required to have maintained stable refraction (where the patient's refractive error did not change) for a minimum of two years, and abstain from using contact lenses in the preceding two weeks. Criteria for exclusion encompassed conditions like severe dry eyes, suspected keratoconus, retinal detachment, cataract, ocular disorders, and connective tissue diseases. Comprehensive demographic and clinical profiles of patients in low, moderate, and high myopia groups are outlined in Table 1.
2.2 Surgical procedure
Preceding the surgery, patients received surface anesthesia, and explicit instructions were given to focus on a target light for the initiation of suction. The VisuMax femtosecond laser (Carl Zeiss Meditec AG) with a frequency of 500 kHz was employed for the procedure. Four precise cleavage planes were generated, covering the anterior and posterior surfaces of the refractive lenticule, the vertical edge of the refractive lenticule, and a singular sidecut incision. Following the femtosecond laser cutting, lenticule extraction was carried out through a small incision. The optical zone diameter (lenticule diameter) for all myopic corrections ranged from 6.0 to 6.5 mm; while, the cap thickness was consistently maintained at 110 µm. importantly, the procedure was consistently conducted by the same proficient surgeon.
Postoperative medications encompassed anti-inflammatory (Fluconcoll or Optifjam), wetting and lubricating gel (such as Liposic or Siccafluid gel), and an antibiotic (Tymercoll or Optiflox). Figure 1 illustrates the essential steps of the SMILE procedure, using an example from one of our patients.
2.3 Measurement of corneal HOAs
The quantification of preoperative and postoperative high-order aberrations in our patients was carried out using the iTrace aberrometer which operates on the fundamental principle of ray tracing (Tracey Technologies Corp. 16,720 Hedgecroft Drive, Suite 208 Houston, Texas 77,060 USA, version 6.1). This advanced device yielded comprehensive outcomes, encompassing all ocular aberrations. It differentiated between low order aberrations (LOAs) and HOAs, offering specific values for both corneal and internal aberrations. All measurements were carried out in a subdued lighting environment without inducing pupillary dilation.
Subsequent to the surgical procedure, a comprehensive assessment of visual acuity for all cases was conducted on the initial postoperative day. Furthermore, the identical cases underwent categorization into three distinct groups based on the duration of aberrometric follow-up. Specifically, 53 patients (106 eyes) were observed for 2 months, 34 patients (67 eyes) for 6 months, and 32 patients (63 eyes) for a period of 1 year or more. Notably, 9 patients underwent two follow-ups, either at 2 and 6 months, or at 2 months and 1 year or more. This variation in follow-up periods was designed to comprehensively evaluate the outcomes of SMILE surgery over different time frames. Short-term follow-ups at 2 and 6 months allowed for early assessment of postoperative changes, monitoring of healing progress, and timely detection of any immediate complications. In contrast, the longer-term follow-up at 1 year or more provided insights into the stability of visual outcomes, the persistence of refractive changes, and the durability of the surgical intervention's effectiveness.
A meticulous examination of ocular aberrations, comprising corneal HOAs, coma, spherical aberrations, secondary astigmatism, and trefoil, was performed subsequent to SMILE surgery, utilizing the iTrace aberrometer consistently for accurate quantification of the observed changes. Figure 2 demonstrates an example from the left eye of one of our patients, showing changes in HOAs before and after the SMILE procedure.
2.4 Sample size
The sample size for this study was determined through a power analysis conducted prior to the study to ensure adequate power to detect meaningful effects. Based on previous studies and expected effect sizes for changes in corneal HOAs, pre- and post-SMILE.
-
Significance level (alpha): 0.05
-
Power (1-beta): 0.80
-
Expected effect size (d): 0.5 (based on previous literature)
Using these parameters, we calculated that a sample size of approximately 32 eyes per group would be sufficient to detect significantly the changes of corneal HOAs postoperatively. To enhance the robustness of our study, we included 110 patients (219 eyes), which exceeds the initial estimate and provides a strong statistical basis for our findings.
2.5 Statistical analysis
The analysis of measured outcomes and comparisons between preoperative and postoperative data employed IBM SPSS Statistics version 21.0 software. The Spearman rank correlation test assessed relationships, including corneal HOAs pre- and post-SMILE surgery. Analysis explored links between induced aberrations and preoperative factors (spherical equivalent, sphere, cylinder, CCT, and age). Group comparisons utilized the ANOVA test, with significance set at P < 0.05.
2.6 Ethical considerations
This study adhered to the ethical principles outlined in the Declaration of Helsinki. Prior to participation, all patients provided written informed consent after being thoroughly informed about the nature of the study, the surgical procedure, potential risks, and benefits. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of our university for the doctoral thesis project in optometry to the scientific and ethical standards outlined in Ministerial Decree No.991 dated May 12, 2023. Confidentiality and anonymity of the participants were strictly maintained throughout the study, with data being coded and securely stored to protect patient privacy. Only authorized personnel had access to the data, ensuring compliance with ethical standards for human research
3 Results
3.1 Preoperative data
All surgical procedures were executed successfully, devoid of intraoperative or postoperative complications, as detailed in Table 1. This table presents demographic data including gender distribution, age, and refractive parameters (sphere, cylinder, spherical equivalent) across three groups, along with CCT. Importantly, the absence of observed cases of corneal ectasia further supports the procedural success observed in this study. Statistical analysis revealed no significant variations in patient age, preoperative SE, sphere, cylinder, and CCT among the three groups. This lack of differences ensures a fair comparison of corneal HOA). Comprehensive preoperative corneal HOA values are detailed in Table 2. Mean preoperative corneal HOA measurements, including SA, coma, trefoil, secondary astigmatism, and tetrafoil, did not exhibit significant differences between groups (F = 0.024, P = 0.878).
3.2 Preoperative correlations
Table 3 presents the correlations between SE, sphere, cylinder, age, CCT, and preoperative corneal HOAs. SE demonstrated significant correlations with spherical aberration and secondary astigmatism in the first and third groups (P = 0.014, P = 0.027, P = 0.039, P = 0.046, respectively), as well as with vertical coma in the third group (P = 0.050). Only the first group's cylindrical diopter exhibited significant correlations with spherical aberration, vertical coma, and secondary astigmatism (P = 0.003, P = 0.045, P = 0.007, respectively). Additionally, patient age showed significant correlations with spherical aberration, vertical coma, and vertical trefoil in the first group (P = 0.004, P = 0.009, P = 0.036, respectively), and with secondary astigmatism and vertical tetrafoil in the third group (P = 0.002, P = 0.017, respectively). CCT displayed a significant correlation only with vertical coma in the first group (P = 0.024). Notably, in the second group, there were no statistically significant correlations identified between the mentioned parameters and total corneal HOAs.
3.3 Postoperative changes
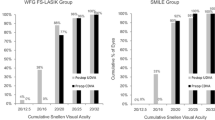
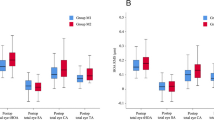
Postoperative changes are detailed in Table 4, highlighting significant increases in vertical and horizontal coma, horizontal trefoil, secondary astigmatism, spherical aberrations, and oblique tetrafoil of the total cornea across all groups (P1 < 0.016, P2 < 0.031, and P3 < 0.050, respectively; Fig. 3A–C). However, no statistically significant correlations were observed for vertical tetrafoil in the second group (P2 = 0.112); while, significant decreases were noted in the third group (P3 = 0.047). Vertical trefoil exhibited significant decreases in all groups (P1 = 0.000, P2 = 0.015, P3 = 0.027), with values in Group 1 surpassing those in the other two groups, as illustrated in Fig. 4
3.4 Postoperative correlations
Table 5 outlines the associations between SE, sphere, cylinder, age, CCT, and postoperative corneal HOAs. Preoperative SE displayed significant correlations with spherical aberration in the first group (P1 = 0.000) and vertical coma in the first and third groups (P1 = 0.002, P2 = 0.006, respectively). It also significantly correlated with vertical tetrafoil in the first and third groups (P1 = 0.008, P3 = 0.033, respectively). Cylindrical diopter exhibited significant correlations with secondary astigmatism across all groups (P1 = 0.000, P2 = 0.021, and P3 = 0.020, respectively), and with vertical tetrafoil in the first two groups (P1 = 0.008, P2 = 0.016, respectively). Patient age was significantly correlated only with secondary astigmatism in the second and third groups (P2 = 0.010, P3 = 0.005, respectively). CCT showed significant correlations with vertical trefoil in the first two groups (P1 = 0.014, P2 = 0.003, respectively), and with spherical aberration, horizontal coma, and vertical tetrafoil in the first group (P1 = 0.038, P1 = 0.001, P1 = 0.032, respectively).
3.5 Comparison of preoperative and postoperative parameters
Upon comparing Tables 3 and 5, several notable findings emerged.
3.5.1 Spherical aberration
In the first group, there was a substantial correlation between the degree of myopia and 4th-order spherical aberration (SA), with a notable increase in SA both preoperatively and postoperatively (P = 0.025, P = 0.000, respectively). High myopia was associated with significantly higher SA values (Refer to Fig. 5A).
Relationship between preoperative myopia and spherical aberration (SA) and vertical coma values before and after SMILE refractive surgery. These figures demonstrate how the degree of myopia influences specific aberrations, both preoperatively and postoperatively. A first group; B second group; C third group
3.5.2 Vertical coma
In the third group, a significant correlation was detected between preoperative myopia and 3rd-order vertical coma. There was a significant decrease in both preoperative and postoperative vertical coma associated with preoperative myopia (P = 0.047, P = 0.004, respectively). The reduction in vertical coma was more pronounced in cases of low myopia (Refer to Fig. 5C).
No significant relationship was established between preoperative myopia and other high-order aberrations (HOAs) (P > 0.05).
3.5.3 Preoperative spherical equivalent (SE)
Significant correlations were observed between preoperative SE and both preoperative and postoperative SA in group 1, as well as vertical coma in group 3:
-
Postoperative SA demonstrated a significant increase with preoperative SE (P = 0.000, Refer to Fig. 6A).
-
Postoperative vertical coma exhibited a lesser increase when preoperative SE was less than − 6.00 D compared to cases with preoperative SE higher than − 6.00 D (P = 0.006, Refer to Fig. 6B).
-
Both preoperative SA and vertical coma demonstrated significant stability in relation to preoperative SE (P = 0.014 for SA, P = 0.050 for vertical coma)
Relationship between preoperative spherical equivalent (SE) and: A Spherical aberration values before and 2 months after SMILE refractive surgery. B Vertical coma values before and one year after SMILE refractive surgery. This figure examines how SE affects specific corneal aberrations at different postoperative intervals
3.5.4 Impact of patient age
Figure 7 illustrates a significant increase in 4th-order secondary astigmatism with patient age, particularly in the third group. Specifically, the values of second astigmatism before and after Smile refractive surgery (P = 0.002, P = 0.005, respectively) were notably higher in middle-aged individuals. No significant preoperative–postoperative correlation was observed in the other two groups.
4 Discussion
This study delves into the intricate correlations between preoperative refraction parameters (spherical and cylindrical diopters, and SE) and the consequent alterations induced by SMILE on corneal HOAs in myopic eyes. Notably, the investigation stands as an original contribution within the Algerian population, exclusively carried out by a seasoned surgeon.
Our findings illuminate a significant upswing in total corneal HOAs, specifically in coma and spherical aberration, following SMILE surgery, as depicted in Fig. 3 and Table 4. Moreover, our results uncover a noteworthy correlation between changes in total corneal coma and spherical aberration and preoperative spherical equivalent (SE), aligning with previous studies' outcomes [8, 11, 12].
In exploring the surge in HOAs, insights from Liu et al. suggest that disparities in lenticule center positioning during SMILE surgery could impact postoperative corneal HOA changes [15]. Prevailing research indicates that decentration significantly contributes to heightened coma and spherical aberrations following corneal refractive surgery [16,17,18]. In our analysis, we also contemplate additional factors influencing induced coma aberrations in SMILE procedure. Our hypothesis posits that coma aberration could be linked to the single incision in SMILE, potentially leading disproportionate corneal healing responses and alterations in optics. Additionally, the induction of coma with SMILE may be attributed to the absence of iris alignment or an eye tracker [7, 19].
Furthermore, our data reveals a noteworthy rise in postoperative HOAs in cases of high myopia when compared to moderate and low myopia. Aligning with the observations of Hou et al. we extend this interpretation by highlighting the positive correlation between SMILE refractive surgery and preoperative spherical diopter and astigmatism. This implies that the foreseen degree of correction before surgery has a substantial impact on the outcomes. Particularly, with an increase in the anticipated correction degree, there is a corresponding rise in the thickness of the lens to be removed, requiring a more extensive cut of corneal tissue. Consequently, these alterations in corneal surface morphology contribute to the observed escalation in postoperative HOAs [20, 21].
The introduction of spherical aberrations in refractive surgery results from the modification of the corneal shape, shifting from its inherent prolate aspheric optical architecture to an oblate surface, there by accentuating spherical aberrations [20, 21]. The investigation conducted by Hassan Hashemi et al. elucidated a positive correlation between the degree of correction, corneal aspheric change, ablation depth, and spherical aberration [7]. Hence, the resulting spherical aberration in cases of high myopia was notably higher than that observed in individuals with moderate and low myopia [7, 12, 22].
Contrary to prior studies [11, 12, 14, 23], Our results revealed a significant decrease in third-order vertical trefoil after SMILE refractive surgery in all eyes. This deviation from previous findings could be attributed to several specific geometric considerations and nuances of the SMILE technique. Firstly, the SMILE procedure involves creating a lenticule within the cornea, which is then removed through a small incision. The vertical cut of the lenticule, a critical step in the SMILE technique, may influence the corneal shape in a way that reduces vertical trefoil. The precision of this vertical cut is crucial, as it can alter the distribution of corneal stress and reshape the corneal surface more symmetrically. Vertical trefoil is a complex geometric aberration that primarily affects the peripheral regions of the cornea. The SMILE technique, by centralizing the treatment, significantly modifies the central corneal curvature while minimizing disruptions in the peripheral zones. This centralization means that peripheral aberrations, such as vertical trefoil, are indirectly corrected by the changes in the central corneal shape. Additionally, the SMILE procedure uses micro-incisions that preserve the structural integrity of the cornea better than techniques with larger cuts, such as LASIK. This preservation minimizes incision-induced side effects, which can also contribute to the reduction of third-order aberrations, including vertical trefoil. These considerations underscore the importance of accounting for the specific geometry of aberrations and the characteristics of the SMILE surgical procedure for accurate result interpretation.
In our examination of the correlation between age and corneal HOAs in this investigation, we observed no significant correlation of age with corneal HOAs, except for a positive correlation with fourth-order secondary astigmatism one year after Smile refractive surgery and a positive correlation with preoperative vertical coma. Interestingly, these outcomes diverge from the research by Amano et al. exploring age-related changes in ocular and corneal higher-order aberrations, where a positive correlation between age and both corneal and ocular coma RMS was observed [24]. Additionally, these findings are also somewhat similar of another study indicating that corneal coma tends to escalate with age [25]. Our interpretation of why our results differ slightly suggests that the unique demographic composition of our dataset, where more than three-quarters of the patients were under 40 years old (with only 16.67% falling into the middle age category), may contribute to these distinctive findings. This aspect calls for careful consideration and underscores the need for a nuanced understanding of the interplay between age and corneal aberrations in the context of SMILE refractive surgery.
Concerning the correlation between CCT and HOAs, we identified a postoperative (2 months) direct and significant correlation between CCT and spherical aberration, vertical trefoil, horizontal coma, and vertical tetrafoil (P < 0.038). Postoperative corneal HOAs values were found to be greater in normal CCT compared to thin CCT. However, our results diverge from those reported by Jia Qu et al. who indicated a very weak association between corneal central thickness and wavefront aberrations in myopic eyes [26]. Another investigation by Engy M. Mohamed et al. revealed no relationship between central and peripheral corneal thickness (PCT) and ocular and corneal aberrations [27]. Our working hypothesis posits that the observed increase in corneal thickness may be linked to an elevated rate of wavefront phase shift, providing a plausible rationale for the observed alterations in corneal high-order aberrations.
Nevertheless, this study has certain limitations. While we enrolled 110 subjects (219 eyes), the available data covered only 2 months for 106 eyes, 6 months for 67 eyes, and one year for 61 eyes. Consequently, these three groups were not of equal size, warranting caution in interpreting the results. To validate our initial observations, it is imperative that future studies incorporate longer-term follow-up visits and larger sample sizes. Furthermore, a more comprehensive characterization of ocular aberrations could be achieved by extending beyond the 4th order in Zernike terms. Additionally, for patients treated bilaterally, the correlation between the two eyes of each patient was not explored, necessitating further investigations to understand the impact on visual outcomes, particularly concerning corneal HOAs. This research also omitted corneal biomechanical parameters, which could provide insights into the correlation among corneal biomechanics and surgically induced corneal HOAs in advanced SMILE surgery in Algerian patients. Recognizing the potential significance of corneal biomechanics for preoperative screening and optimizing postoperative visual qualities [28]. In future investigations, there is a scope to explore potential relationships between corneal biomechanics and surgically induced corneal high HOAs in the SMILE procedure specifically in Algerian patients.
5 Conclusion
This comprehensive exploration into the alterations in HOAs after SMILE surgery within the Algerian population highlights several key findings. The primary outcome of assessing changes in total corneal HOAs revealed a significant elevation in spherical aberrations and vertical coma aberrations across the total cornea; while, there was a notable decrease in vertical trefoil. Secondary outcomes showed that these postoperative aberrations are intricately connected to the preoperative SE.
Our findings suggest that SMILE is particularly advantageous in cases of low and moderate myopia. To enhance postoperative visual quality, minimizing decentration is crucial. Surgeons should strive to position the center of the visual axis with utmost accuracy to mitigate the induced spherical aberration when employing SMILE surgery.
Availability of data and materials
Not applicable.
Abbreviations
- SMILE:
-
Small incision lenticule extraction
- SE:
-
Spherical aberration
- CCT:
-
Corneal central thickness
- HOA:
-
High order aberration
- CHOA:
-
Corneal high-order aberration
- LOA:
-
Low order aberration
- SA:
-
Spherical aberration
References
Wang L, Dai E, Koch DD, Nathoo A (2003) Optical aberrations of the human anterior cornea. J Cataract Refract Surg 29(8):1514–1521
Cerviño A, Hosking SL, Montes-Mico R, Bates K (2007) Clinical ocular wavefront analyzers. J Refract Surg 23(6):603–16
Rozema JJ, Van Dyck DEM, Tassignon MJ (2005) Clinical comparison of 6 aberrometers. Part 1: Technical specifications. J Cataract Refract Surg 31(6):1114–27
Mrochen M, Kaemmerer M, Mierdel P, Krinke HE, Seiler T (2000) Principles of Tscherning aberrometry. J Refract Surg 16:S570–S571
Win-Hall DM, Glasser A (2009) Objective accommodation measurements in pseudophakic subjects using an autorefractor and an aberrometer. J Cataract Refract Surg 35(2):282–290
Li L, Cheng GPM, Ng ALK, Chan TCY, Jhanji V, Wang Y (2017) Influence of refractive status on the higher-order aberration pattern after small incision lenticule extraction surgery. Cornea 36(8):967–972
Miraftab M, Hashemi H, Aghamirsalim M, Fayyaz S, Asgari S (2021) Matched comparison of corneal higher order aberrations induced by SMILE to femtosecond assisted LASIK and to PRK in correcting moderate and high myopia: 3.00 mm versus 6.00 mm. BMC Ophthalmol. 21(1):216
Hou X, Du K, Wen D, Hu S, Hu T, Li C et al (2021) Early visual quality outcomes after small-incision lenticule extraction surgery for correcting high myopic astigmatism. BMC Ophthalmol 21(1):48
Kirmaci Kabakci A, Kepez Yildiz B, Yildirim Y, Agca A, Ondes Yilmaz F, Demir G et al (2021) Refractive and visual outcomes of small incision lenticule extraction (SMILE) in eyes with thin corneas. Eye 35(8):2302–2309
Sekundo W, Kunert KS, Blum M (2011) Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol 95(3):335–339
Jin HY, Wan T, Wu F, Yao K (2017) Comparison of visual results and higher-order aberrations after small incision lenticule extraction (SMILE): high myopia versus mild to moderate myopia. BMC Ophthalmol 17(1):118
Jin HY, Wan T, Yu XN, Wu F, Yao K (2018) Corneal higher-order aberrations of the anterior surface, posterior surface, and total cornea after small incision lenticule extraction (SMILE): high myopia versus mild to moderate myopia. BMC Ophthalmol 18(1):295
Tan DKL, Tay WT, Chan C, Tan DTH, Mehta JS (2015) Postoperative ocular higher-order aberrations and contrast sensitivity: Femtosecond lenticule extraction versus pseudo small-incision lenticule extraction. J Cataract Refract Surg 41(3):623–634
Wu W, Wang Y (2016) Corneal higher-order aberrations of the anterior surface, posterior surface, and total cornea After SMILE, FS-LASIK, and FLEx surgeries. Eye Contact Lens Sci Clin Pract 42(6):358–365
Liu M, Sun Y, Wang D et al (2015) Decentration of optical zone center and its impact on visual outcomes following SMILE. Cornea 34(4):392–397
Li M, Zhao J, Miao H et al (2014) Mild decentration measured by a Scheimpflug camera and its impact on visual quality following SMILE in the early learning curve. Investig Ophthalmol Vis Sci 55(6):3886–3892
Yu Y, Zhang W, Cheng X, Cai J, Chen H (2017) Impact of treatment decentration on higher-order aberrations after SMILE. J Ophthalmol 2017:1–7
Mrochen M, Kaemmerer M, Mierdel P, Seiler T (2001) Increased higher-order optical aberrations after laser refractive surgery: a problem of subclinical decentration. J Cataract Refract Surg 27(3):362–369
Liu M, Chen Y, Wang D, Zhou Y, Zhang X, He J et al (2016) Clinical outcomes after SMILE and femtosecond laser-assisted LASIK for myopia and myopic astigmatism: a prospective randomized comparative study. Cornea 35:210–216
Bottos KM, Leite MT, Aventura-Isidro M et al (2011) Corneal asphericity and spherical aberration after refractive surgery. J Cataract Refract Surg 37:1109–1115
Chen CC, Izadshenas A, Rana MA, Azar DT (2002) Corneal asphericity after hyperopic laser in situ keratomileusis. J Cataract Refract Surg 28:1539–1545
Zhang H, Wang Y, Li H (2017) Corneal spherical aberration and corneal asphericity after small incision lenticule extraction and femtosecond laser-assisted LASIK. J Ophthalmol 2017:1–7
Ağca A, Demirok A, Çankaya Kİ, Yaşa D, Demircan A, Yıldırım Y et al (2014) Comparison of visual acuity and higher-order aberrations after femtosecond lenticule extraction and small-incision lenticule extraction. Contact Lens Anterior Eye 37(4):292–296
Amano S, Amano Y, Yamagami S, Miyai T, Miyata K, Samejima T et al (2004) Age-related changes in corneal and ocular higher-order wavefront aberrations. Am J Ophthalmol 137(6):988–992
Salman A, Kailani O, Ghabra M, Omran R, Darwish TR, Shaaban R, Khalil H (2023) Corneal higher order aberrations by Sirius topography and their relation to different refractive errors. BMC Ophthalmol 23(1):104
Qu J, Lu F, Wu J, Wang Q, Xu C, Zhou X et al (2007) Wavefront aberration and its association with intraocular pressure and central corneal thickness in myopic eyes. J Cataract Refract Surg 33(8):1447–1454
Mohamed EM, Wojtowicz JC, Bowman W, Cavanagh HD, Mootha V, Verity S et al (2009) Corneal thickness association with ocular and corneal high-order aberrations. Eye Contact Lens Sci Clin Pract 35(6):297–301
Wu W, Wang Y (2015) The Correlation Analysis between Corneal Biomechanical Properties and the Surgically Induced Corneal High-Order Aberrations after Small Incision Lenticule Extraction and Femtosecond Laser In Situ Keratomileusis. J Ophthalmol 2015:1–10
Acknowledgements
The authors express sincere appreciation to Pr. C Abdelileh, founder of Chiali Smile Center, for generously+ providing the essential facilities for conducting this study. Special thanks are extended to Optometrist L. Mohamed for invaluable assistance, and gratitude goes to the patients who actively contributed in this research.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SH: Manuscript revision and assistance in using SPSS software and data analysis. DG: Contribution to study design and manuscript revision. FK: Academic guidance and project supervision, substantial contribution to in-depth data analysis, and assistance in establishing the bibliography. SC: Critical content review, and significant assistance in crafting the bibliography. SB: primary manuscript writing, study design, and comprehensive data collection.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study adhered to the ethical principles outlined in the Declaration of Helsinki. Prior to participation, all patients provided written informed consent after being thoroughly informed about the nature of the study, the surgical procedure, potential risks, and benefits. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Oran1 Ahmed Benbella University for the doctoral thesis project in optometry according to the scientific and ethical standards outlined in Ministerial Decree No. 991 dated May 12, 2023. The confidentiality and anonymity of the participants were strictly maintained throughout the study, with data being coded and securely stored to protect patient privacy. Only authorized personnel had access to the data, ensuring compliance with ethical standards for human research.
Consent for publication
Written informed consent for publication was obtained from the patients.
Competing interests
The authors (Sarra Belgacem, Saoussene Habani, Daoud Guernazi, Fatiha Kail, Selma Chiali) declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Belgacem, S., Habani, S., Guernazi, D. et al. Analysis of third and fourth corneal high-order aberrations before and after small incision lenticule extraction (SMILE) in myopic and myopic astigmatic eyes using ray tracing aberrometry. Beni-Suef Univ J Basic Appl Sci 13, 91 (2024). https://doi.org/10.1186/s43088-024-00544-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-024-00544-3