Abstract
Background and objective
The association of clinical factors of osteoarthritis (OA) with bone mineral density (BMD) is not well understood. We aimed to synthesize evidence regarding the associated clinical factors for low BMD in people with knee and/or hip osteoarthritis.
Methods
A systematic literature search limited to human studies was conducted from inception to September 12, 2022. CINAHL, Cochrane, Medline, PsycINFO, PubMed, Web of Science, and African Journal online databases were searched for all clinical factors associated with low BMD (either as osteopenia or osteoporosis). Gray literature or abstracts or protocols, studies with a mixed population of OA without a subgroup analysis for hip and or KOA and non-English were excluded. Following the title and abstract, full-text, screenings, and data extraction, data from eligible studies were synthesized based on the main objective of the study. The Joanna Brigg’s Institute (JBI) Critical Assessment tool was used for quality appraisal. Narrative synthesis and best evidence synthesis were used in the study.
Result
Five studies (2 case–control, 3 cross-sectional) were included after screening 3355 titles and abstracts. Clinical factors reported in the five studies included: body mass index (BMI); pain, function, and stiffness; symptom duration; presence of varus/valgus deformity; quality of life; and knee function. Whilst there was limited evidence to support the association between BMD measured at any site of the body and BMI, as well as conflicting evidence for the association of BMD with age and gender, there was insufficient evidence to support the association of BMD with other identified clinical factors of hip and or/ knee OA (p < 0.05). In addition, there is conflicting evidence for the association between BMD measured at the lumbar spine and BMI.
Conclusion
There is insufficient evidence on the association between BMD and its associated clinical factors. With the attendant likelihood of bias in existing studies, there is a need for well-designed studies on bone health in OA.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) and osteoporosis (OP) are two common age-related musculoskeletal disorders with a prevalence of 7% and 18.3%, respectively [15, 35]. Although earlier believed to be mutually exclusive [5, 16], some studies have indicated that both OA and OP are not mutually exclusive, and are common musculoskeletal disorders that could coexist in the same individual [1, 4, 12, 14]. The relationship between these two diseases remains unclear and is a subject of ongoing research. Studies focusing on the relationship between OA and bone mineral density (BMD) (indicating osteoporosis) posit that both diseases can have a direct relationship where higher BMD is observed in individuals with OA [3, 7, 18, 22, 30]. On the other hand, Foss et al. [13] as far back as 40 years ago, suggested an apparent inverse relationship between the two diseases. Similarly, other reports suggest an inverse relationship between the presence of OA and OP [10, 41].
Studies on radiographic OA of the hip and BMD showed an increase in BMD measurements taken at remote proximal and distal sites of the radius and at the calcaneus in women with severe hip OA compared to individuals without OA [17, 29]. Lingard et al. [27] submitted that a significant proportion of patients with OA have OP but that the diagnosis may be missed unless BMD measurements are performed at sites distant from the joints affected by OA. This is because OA characteristic features such as osteophyte formation and subchondral sclerosis that are presented at the joint can alter/increase the BMD measurements done by central dual-energy x-ray absorptiometry (DEXA) of the spine and hip [29]. Thus, whether there is a direct or inverse correlation between OA and OP, and whether low BMD may be a comorbidity of OA are separate questions. El Miedany et al. [12] submitted that an increase in BMD did not appear to be related to patient characteristics of body weight, age, physical activity, or medication use. Some of the clinical correlates of OA that have been documented in the literature include BMI, symptom duration, pain, function and stiffness, quality of life, etc. [33, 34]. Considering the possible interrelationship between OA and OP, clinical measures directed at ameliorating OA symptoms may improve BMD, and this might be an important therapeutic pathway. This systematic review seeks to synthesize the current evidence and offer direction on the knee OA-OP nexus to provide clinical care guidelines.
Methods
The Preferred Reporting Items of Systematic Reviews and Meta-analyses (PRISMA) [31] and the protocol defined by the Joanna Briggs Institute (JBI) Methodology for Systematic Reviews were followed in this review. The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42022334000).
Study selection criteria
Population, exposure, study types, settings, and outcomes
The population of interest of this review was male and female adults (≥ 40 years) diagnosed with hip and/or knee OA using the American College of Rheumatology Criteria (ACR), KL system of classification, doctor diagnosis, and Ahlback grading scale. Studies with general rheumatic and osteoarthritis conditions were considered only if subgroup results for hip and knee OA were presented. Studies that assessed BMD (either reported as BMD, osteopenia, or osteoporosis) at sites including the spine, femur, total hip, and /or a combination of these sites in individuals with hip and/or knee OA were included. We included all types of observational studies, i.e., cohort, case–control, and cross-sectional studies from all settings. All clinical outcomes reported in eligible studies were identified and included.
Eligibility criteria
Inclusion and exclusion criteria
Peer-reviewed studies that included a knee and/or hip OA population or sub-sample of knee and/or hip OA diagnosed using radiographic evidence and/or clinical diagnosis (as defined by the American College of Rheumatology criteria) [2] or according to Kellgren Lawrence (KL) grading [23] and that assessed the BMD as a measure of Osteoporosis.
According to the World Health Organization [39], OP was defined as a BMD T-score at the hip and/ or the spine of < 2.5 standard deviations (SD) for postmenopausal women, and T-scores of between − 1 and − 2.5 SD for men and women over the age of 50 years [21, 28]. Gray literature, abstracts, protocols, or non-human studies with a mixed population of OA without a subgroup analysis for hip and or knee OA and non-English were excluded.
Search strategy
Online electronic databases of CINAHL, Cochrane, Medline, PsycINFO, Pubmed, Web of Science, and African Journal (from inception to September 12, 2022). The initial keywords used in the review were “bone mineral density” OR “bone density” OR “Osteoporosis” OR “Osteopenia” OR “fracture”; “risk factors” OR “outcomes” OR “correlates” OR “Prevalence”; and “Knee osteoarthritis” OR “hip osteoarthritis”. The complete search strategy implemented is presented in Supplementary material (see Appendix). Also, the reference list of included studies and two related systematic reviews were screened to extract related articles. Eligible study design included prospective longitudinal cohort, cross-sectional, and case studies.
Screening and selection of studies
Duplicate citations were eliminated by one of the authors (BAA). In the first phase, three independent assessors (IO, HF, and OO) screened the titles and abstracts of the articles returned by the search. BAA arbitrated the searches of the two assessors where there were contentions on the inclusion/exclusion of articles. In the second phase, full-text manuscripts of possibly eligible studies were retrieved and reviewed by each of the independent assessors using a standardized Microsoft Excel screening spreadsheet to identify relevant studies. Data were extracted on study setting, study population, sample size, study design, measures of BMD and OA used, statistical analysis, and main findings. To ensure quality control of data extraction, both virtual and physical meetings were held among the assessors (IO, HF, and OO) and the third reviewer (BAA) to discuss cases.
Quality assessment of selected studies
Assessment of reporting quality and the risk of bias for each paper was done using the Joanna Brigg’s Institute (JBI) Critical Assessment tool which is a widely used and recommended assessment tool by Cochrane for evaluating qualities of observational and cross-sectional and case–control studies. The tool for observational and cross-sectional studies comprises 8 items (all applicable to cross-sectional studies) while that for case–control studies comprise 10 items. The quality assessment for each included study was carried out by two independent assessors (OI and HO) using the scoring system of yes (Y), No (N), Unclear (U), or not applicable (NA). An arbitrator (BAA) acted as a tie-breaker whenever a consensus could not be reached.
Data synthesis
Meta-analysis was not performed due to the high heterogeneity levels with regard to study designs and methodology. However, findings were presented using a narrative synthesis to report the association between clinical factors of hip and/or knee OA and BMD. Further, we performed the best evidence synthesis of clinical factors that were investigated in two or more studies and ranked evidence grading based on previous studies [38, 40] to grade the level of evidence supporting the association (see Appendix). We classified studies according to study design, with the preferred being cohort study followed by case–control design, and lastly cross-sectional design. Studies were ranked according to their methodological quality score. Identified clinical factors were classified in the direction and strength of association by using correlation or standardized coefficient as weak (< 0.3), moderate (> 0.3 < 0.7), and strong (≥ 0.7) [19] or with odds ratio [9] where these were reported. We adjudged results as consistent if BMD was significantly associated with the identified clinical factor of OA in the same direction of the association.
Results
Literature search and study selection
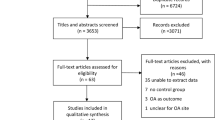
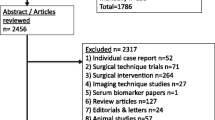
Three thousand, three hundred and fifty-five (3355) articles were identified through database searches, and 3 articles were identified through a review of the reference lists of relevant papers and a hand search. Of these articles, we removed 1751 duplicates. The titles and abstracts of the 1604 remaining articles were screened, and of these, 25 full papers were accessed for further review of eligibility. Twenty-one articles were excluded and the remaining 5 articles ((3 cross-sectional studies [11, 27, 37] and 2 case–control studies [8, 32])) The PRISMA flow diagram on the search strategy results of this review is shown in Fig. 1.
PRISMA flow diagram (source— [31])
Study characteristics and association between BMD and OA clinical factors
Extracted data included data for 1295 participants. All five studies were completed in different countries, viz; Germany [11], Korea [8], UK [27], China [37], and Poland [32]. Two of the studies [11, 27]) had more female than male participants, while 3 recruited only female participants [8, 32, 37]. Furthermore, one of the studies specifically recruited only post-menopausal women [32].
Three of the studies [8, 11, 37] diagnosed BMD using Kellgren-Lawrence (KL) scores. One study [27] only required a doctor’s diagnosis while the final study [32] made use of the American College of Rheumatology (ACR) clinical classification criteria for Knee OA.
Clinical factors assessed by the studies were: BMI [11, 27, 32, 37],pain, function, and stiffness [8, 27],symptom duration [37],presence of varus/valgus deformity [37],quality of life [8],and knee function [8]. Tables 1 and 2 show the summary of all the studies included in the review.
Results across four studies showed BMI to be an important clinical factor associated with BMD among people with osteoarthritis [11, 27, 32, 37]. Pain, function, and stiffness [8], female gender [27], varus deformity [37], QoL-physical component [8], and knee function [8] were all also significantly associated with BMD.
However, mental component summary QoL [8], symptom duration [37], valgus deformity [37], and incidence of bilateral KOA [37], did not demonstrate significant associations with BMD among the population.
Quality assessment
Three (3 cross-sectional studies [11, 27, 37], and two case–control studies [8, 32] were rated as having good quality and included in the review. The summary of the quality assessment is presented in Tables 3 and 4.
Best evidence synthesis
Following the best evidence synthesis, there was limited evidence to support the association between BMD measured at any site of the body and BMI. In addition, there was a conflicting evidence for the association of BMD with age and gender. When BMD was measured at the lumbar spine, the evidence for the association between BMD and BMI became conflicting. For other identified clinical factors, there was insufficient evidence to support an association with BMD. Strengths of association and levels of best evidence are summarized in Tables 5 and 6, respectively.
Discussion
This systematic review aimed to summarize current epidemiological evidence on the association between BMD and clinical factors of hip and/or knee OA. Due to high heterogeneity levels in study designs and limited number of studies, the review employed a narrative and best evidence synthesis, which enabled grading of factors into different levels of evidence. There were five studies that evaluated the association of BMI with BMD, with majority having longitudinal design. The best evidence synthesis found limited evidence for the positive association between low BMI and poor BMD measured at any site of the body. Conflicting evidence was found for the association between BMD and each of age and gender. When BMD was measured at the lumbar spine, the evidence for the association between BMD and BMI became conflicting. All other factors identified had insufficient evidence. From the table above, all the studies reviewed were from Europe and Asia. No study was found from Africa or America. Furthermore, most of the reviewed studies recruited knee OA alone and only one recruited patients with hip and knee OA [27].
The association between bone mineral density and OA has long been a subject of debate in the literature [18, 36]. Although the exact pathophysiology remains unclear, this association between OA and OP has been known from early cross-sectional studies [6, 20, 26, 33]. Bone is considered an integral structure in the pathogenesis of OA and the role of local and systemic bone mineral density (BMD) is gaining increasing interest [33]. A relatively recent review demonstrated the similarities in etiology, risk factors, and shared mechanisms between BMD and OA, which suggests a possible association with clinical factors of OA like BMI [14]. It is important to note that high BMI may be protective of BMD especially in among males and black populations populations [25]. However, excessive BMI may be harmful to BMD as Li [25] reported an inverted U-shaped association between BMD and BMI. More studies are needed to understand these associations among the blacks and especially in the African population. Longitudinal BMD loss has been reported to be associated with progressive cartilage loss in knees with OA Patients thus suggesting that severity of knee OA may be directly related to the BMD of the individual [24]. With the advent of therapies that modify bone turnover, a better understanding of the relationship between BMD and structural/ clinical changes in knee OA may have important implications for important clinical outcomes of the disease like,onset and/or progression [24].
There was considerable variation in the assessment sites for BMD in the studies. The studies by some of the authors [8, 11] had BMD measurements made at the proximal femur and lumbar spines in their studies. In one study [37], BMD was assessed at the proximal femur, femoral neck and lumbar spines. In the fifth study [32], BMD assessment was done at the proximal femur and lumbar spine. Lingard et al. [27] who made measurements at the forearm in addition to the spine and proximal femur, reported significant proportion of patients with severe OA had low BMD and that the diagnosis may be missed unless BMD measurements are performed at sites distant from the joints affected by OA.
Implications for clinical practice
Clinicians should potentially target increased BMI, especially by strengthening skeletal muscles which may improve BMD of patients with osteoporosis and osteopenia in the long run. In addition, an increase in BMI may promote mechanical stress on the body density, subsequently improving BMD.
Implications for further research
Well-conducted longitudinal studies with adequate sample sizes and diverse OA populations are needed as this would provide more comprehensive understanding of the association between clinical factors and BMD in osteoarthritis. In addition, it is important to investigate clinical factors associated with BMD in other climes such as Africa and America as environmental factors may influence the perpetuation and presentation of OA. Further, future studies may consider other potentially relevant factors that may be associated with BMD, including: medication use, physical activity levels, sedentary behavior patterns, and dietary habits.
Strengths and limitations
This study is the first to investigate the association between BMD and clinical factors of hip and or knee OA. In addition, we used best evidence synthesis to adjudge the current level of evidence for the association. This study is however with limitations. These study findings were based on only five studies a higher proportion of which were cross-sectional designs, limiting the ability to draw robust conclusions. As noted by one of the studies the variability of assessment sites might influence BMD detection [27]. The use of convenience sampling techniques would also negatively impact the internal validity of these studies. In addition, our search might have missed some studies published in non-English journals, thus, other clinical factors might not have been identified.
Conclusion
This systematic review synthesizes current evidence on BMD and its associated clinical factors. High likelihood of bias and limited evidence at best suggests a need for well-designed studies on the relationship between OA and BMD.
Availability of data and materials
Data from this study were pooled from Online electronic databases of CINAHL, Cochrane, Medline, PsycINFO, PubMed, Web of Science, and African Journal (from inception to September 12, 2022).
References
Alkhatatba M, Abualadas J, Tabar MAA, Abueed M, Alghzawi AA, Abualadas R, Radaideh A, Essa SB, Obeidat N, Alma Aiteh AA, Al-Omari J. Is there a role for ordering a DEXA (Dual Energy X-Ray Absorptiometry) scan for patients with symptomatic advanced knee osteoarthritis? Acta Inform Med. 2023;31(2):111–4. https://doi.org/10.5455/aim.2023.31.111-114.
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum. 1986;29(8):1039–49.
Bergink AP, Rivadeneira F, Bierma-Zeinstra SM, Zillikens MC, Ikram MA, Uitterlinden AG, van Meurs JB. Are bone mineral density and fractures related to the incidence and progression of radiographic osteoarthritis of the knee, hip, and hand in elderly men and women? The Rotterdam study. Arthritis Rheumatol. 2019;71(3):361–9.
Blumer MHM. Bone mineral content versus bone density in a population with osteoarthritis: a new twist to the controversy? J Rheumatol. 2005;32(10):1868–9.
Bultink IE, Lems WF. Osteoarthritis and osteoporosis: what is the overlap? Curr Rheumatol Rep. 2013;15(5):328. https://doi.org/10.1007/s11926-013-0328-0.
Burger H, van Daele PL, Odding E, Valkenburg HA, Hofman A, Grobbee DE, et al. Association of radiographically evident osteoarthritis with higher bone mineral density and increased bone loss with age. The Rotterdam study. Arthritis Rheum. 1996;39:81e6.
Cai G, Otahal P, Cicuttini F, Wu F, Munugoda IP, Jones G, Aitken D. The association of subchondral and systemic bone mineral density with osteoarthritis-related joint replacements in older adults. Osteoarthritis Cartilage. 2020;28(4):438–45.
Chang CB, Kim TK, Kang YG, Seong SC, Kang SB. Prevalence of osteoporosis in female patients with advanced knee osteoarthritis undergoing total knee arthroplasty. J Korean Med Sci. 2014;29(10):1425–31. https://doi.org/10.3346/jkms.2014.29.10.1425.
Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat Simul Comput. 2010;39:860–4.
Clayton ES, Hochberg MC. Osteoporosis and osteoarthritis, rheumatoid arthritis and spondylarthropathies. Curr Osteoporos Rep. 2013;11:257–62.
Delsmann MM, Schmidt C, Mühlenfeld M, Jandl NM, Boese CK, Beil FT, Rolvien T, Ries C. Prevalence of osteoporosis and osteopenia in elderly patients scheduled for total knee arthroplasty. Arch Orthop Trauma Surg. 2021;142:3957–64.
El Miedany YM, Mehanna AN, El Baddini MA. Altered bone mineral density in patients with osteoarthritis. Joint Bone Spine. 2000;67:521–7.
Foss MV, Byers PD. Bone density, osteoarthrosis of the hip, and fracture of the upper end of the femur. Ann Rheum Dis. 1972;31(4):259–64. https://doi.org/10.1136/ard.31.4.259.
Geusens PP, van den Bergh JP. Osteoporosis and osteoarthritis: Shared mechanisms and epidemiology. Curr Opin Rheumatol. 2016;28(2):97–103. https://doi.org/10.1097/BOR.0000000000000256.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) results. http://ghdx.healthdata.org/gbd-results-tool. Accessed 10 Apr 2024.
Glowacki J. Osteoarthritis and osteoporosis: coexistence of osteoporosis in patients with osteoarthritis. Minerva Ortop Traumatol. 2010;61(2):115–22.
Hannan MT, Anderson JJ, Zhang Y, et al. Bone mineral density and knee osteoarthritis in elderly men and women. The Framingham Study. Arthritis Rheum. 1993;36:1671–6.
Herrero-Beaumont G, Roman-Blas JA, Largo R, Berenbaum F, Castaneda S. Bone mineral density and joint cartilage: four clinical settings of a complex relationship in osteoarthritis. Ann Rheum Dis. 2011;70:1523e5.
Hinkle D, Wiersma W, Jurs S. Applied statistics for the behavioural sciences. 3rd ed. Boston: Houghton Mifflin Company; 2003.
Ishii Y, Noguchi H, Sato J, Ishii H, Todoroki K, Toyabe S, ichi. Association between bone mineral density distribution and various radiographic parameters in patients with advanced medial osteoarthritis of the knee. J Orthop Sci. 2019;24(4):686–92. https://doi.org/10.1016/j.jos.2018.12.019.
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42(3):467–75. https://doi.org/10.1016/j.bone.2007.11.001.
Kasher M, Williams FMK, Freidin MB, Cherny S, Livshits G. An in-depth study of the associations between osteoarthritis-and osteoporosis-related phenotypes at different skeletal locations. Osteoporos Int. 2020;31:2197–208.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. Available from: http://ard.bmj.com/cgi/doi/https://doi.org/10.1136/ard.16.4.494.
Lee JY, Harvey WF, Price LL, Paulus JK, Dawson-Hughes B, McAlindon TE. Relationship of bone mineral density to progression of knee osteoarthritis. Arthritis Rheum. 2013;65(6):1541–6. https://doi.org/10.1002/art.37926.
Li Y. Association between obesity and bone mineral density in middle-aged adults. J Orthop Surg Res. 2022;17:268. https://doi.org/10.1186/s13018-022-03161-x.
Liang F, Tong P, Hongting J. Defining disease progression in chinese mainland people association between bone mineral density with knee osteoarthritis. Osteoarthritis Cartilage. 2020;28:S367. https://doi.org/10.1016/j.joca.2020.02.574.
Lingard EA, Mitchell SY, Francis RM, Rawlings D, Peaston R, Birrell FN, McCaskie AW. The prevalence of osteoporosis in patients with severe hip and knee osteoarthritis awaiting joint arthroplasty. Age Ageing. 2010;39(2):234–9. https://doi.org/10.1093/ageing/afp222.
Miller PD, Njeh CF, Jankowski LG, Lenchik L. What are the standards by which bone mass measurement at peripheral skeletal sites should be used in the diagnosis of osteoporosis? J Clin Densitom. 2002;5(SUPPL.). https://doi.org/10.1385/JCD:5:3S:S39.
Nevitt MC, Lane NE, Scott JC, Hochberg MC, Pressman AR, Genant HK, et al. Radiographic osteoarthritis of the hip and bone mineral density. The study of osteoporotic fractures research group. Arthritis Rheum. 1995;38:907e16.
Nevitt MC, Felson DT. High bone density and radiographic osteoarthritis: questions answered and unanswered. Osteoarthritis Cartilage. 2020;28(9):1151–3.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Povoroznyuk VV, Zaverukha NV, Musiienko AS. Bone mineral density and trabecular bone score in postmenopausal women with knee osteoarthritis and obesity. Wiad Lek. 2020;73(3):529–33. https://doi.org/10.36740/wlek202003124.
Rizou S, Chronopoulos E, Ballas M, Lyritis GP. Clinical manifestations of osteoarthritis in osteoporotic and osteopenic postmenopausal women. J Musculoskelet Neuronal Interact. 2018;18(2):208–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016499/.
Russell Esposito E, Wilken JM. Biomechanical risk factors for knee osteoarthritis when using passive and powered ankle-foot prostheses. Clin Biomech. 2014;29(10):1186–92. https://doi.org/10.1016/j.clinbiomech.2014.09.005.
Salari N, Ghasemi H, Mohammadi L, Behzadi MH, Rabieenia E, Shohaimi S, Mohammadi M. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16:1–20.
Stewart A, Black AJ. Bone mineral density in osteoarthritis. Curr Opin Rheumatol. 2000;12:464e7.
Tao Y, Tang S, Huang X, Wang H, Zhou A, Zhang J. Prevalence and risk factors of osteoporosis in Chinese postmenopausal women awaiting total knee arthroplasty. Clin Interv Aging. 2021;16:379–87. https://doi.org/10.2147/CIA.S297947.
Van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. In Spine; 2003. https://doi.org/10.1097/00007632-200306150-00014.
World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129.
Yusuf E, Nelissen RG, Ioan-Facsinay A, Stojanovic-Susulic V, DeGroot J, Van Osch G, Middeldorp S, Huizinga TWJ, Kloppenburg M. Association between weight or body mass index and hand osteoarthritis: a systematic review. Ann Rheum Dis. 2010. https://doi.org/10.1136/ard.2008.106930.
Im GI, Kim MK. The relationship between osteoarthritis and osteoporosis. J Bone Miner Metab. 2014;32:101-9.
Acknowledgements
Not applicable.
Funding
There was no outside funding for this study.
Author information
Authors and Affiliations
Contributions
BA: Conceptualization, study design, write-up. CE: Conceptualization data collection and write-up. OA: Data collection, analysis, and write-up. AA: Data collection, analysis, and write-up. OA: Data collection and write-up. HO: Data collection and write-up. J: Data collection and write-up. T: Data collection and write-up. AO: Conceptualization and study design
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by The University of Ibadan/University College Hospital Ibadan ethics review committee in Oyo state, Nigeria.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Search strategy
-
# S1 TI bone mineral density OR TI BMD OR TI bone density OR TI BD OR TI osteoporosis OR TI osteopenia
-
#S2 AB bone mineral density OR AB BMD OR AB bone density OR AB BD OR AB osteoporosis OR AB
Osteopenia
-
#S3 TI clinical factors OR TI outcomes OR TI correlates OR TI determinants OR TI prevalence OR TI
predictors OR TI predictor
-
#S4 AB clinical factors OR AB outcomes OR AB correlates OR AB determinants OR AB prevalence OR AB predictors OR AB predictor
-
#S5 TI osteoarthritis OR TI knee osteoarthritis OR TI KOA OR TI hip osteoarthritis OR TI HOA
-
#S6 AB osteoarthritis OR AB knee osteoarthritis OR AB KOA OR AB hip osteoarthritis OR AB HOA
-
#S7 S1 OR S2
-
#S8 S3 OR S4
-
#S9 S5 OR S6
-
#S10 S7 AND S8 AND S9
Search strategy for Medline
-
#S1 TI bone mineral density OR TI BMD OR TI bone density OR TI BD OR TI osteoporosis OR TI osteopenia
-
#S2 AB bone mineral density OR AB BMD OR AB bone density OR AB BD OR AB osteoporosis OR AB
Osteopenia
-
#S3 TI clinical factors OR TI outcomes OR TI correlates OR TI determinants OR TI prevalence OR TI
predictors OR TI predictor
-
#S4 AB clinical factors OR AB outcomes OR AB correlates OR AB determinants OR AB prevalence OR AB predictors OR AB predictor
-
#S5 TI osteoarthritis OR TI knee osteoarthritis OR TI KOA OR TI hip osteoarthritis OR TI HOA
-
#S6 AB osteoarthritis OR AB knee osteoarthritis OR AB KOA OR AB hip osteoarthritis OR AB HOA
-
#S7 S1 OR S2
-
#S8 S3 OR S4
-
#S9 S5 OR S6
-
#S10 S7 AND S8 AND S9
Search strategy for PsyCINFO
-
#S1 TI bone mineral density OR TI BMD OR TI BD OR TI Bone density OR TI osteoporosis OR TI osteopenia
-
#S2 AB bone mineral density OR AB BMD OR AB BD OR AB Bone density OR AB osteoporosis OR AB
-
osteopenia
-
#S3 TI clinical factors OR TI outcomes OR TI correlates OR TI determinants OR TI predictors OR TI predictor
-
#S4 AB clinical factors OR AB outcomes OR AB correlates OR AB determinants OR AB predictors OR TI predictor
-
#S5 TI osteoarthritis OR TI knee osteoarthritis OR TI KOA OR TI hip osteoarthritis OR TI HOA
-
#S6 S1 OR S2
-
#S7 S3 OR S4
-
#S8 AB osteoarthritis OR AB knee osteoarthritis OR AB KOA OR AB hip osteoarthritis OR AB HOA
-
#S9 S5 OR S8
-
#S10 S6 AND S7 AND S9
Search strategy for web of science
-
1.
bone mineral density (Title) OR BMD (Title) OR bone density (Title) OR BD (Title) OR Osteoporosis (Title) OR osteopenia (Title)
-
2.
bone mineral density (Abstract) OR BMD (Abstract) OR bone density (Abstract) OR BD (Abstract) OR Osteoporosis (Abstract) OR osteopenia (Abstract)
-
3.
#1 OR #2
-
4.
clinical factors (Title) OR risk factors (Title) OR outcomes (Title) OR determinants (Title) OR predictor (Title) OR prevalence (Title)
-
5.
clinical factors (Title) OR risk factors (Abstract) OR outcomes (Abstract) OR determinants (Abstract) OR predictor (Abstract) OR prevalence (Abstract)
-
6.
6: #5 OR #4
-
7.
osteoarthritis (Title) OR knee osteoarthritis (Title) OR KOA (Title) OR hip osteoarthritis (Title) OR HOA (Title)
-
8.
osteoarthritis (Abstract) OR knee osteoarthritis (Abstract) OR KOA (Abstract) OR hip osteoarthritis (Abstract) OR HOA (Abstract)
-
9.
#8 OR #7
-
10.
#9 AND #6 AND #3
Modified best-evidence synthesis
Strong evidence | Generally, consistent findings in multiple high-quality cohort studies. |
Moderate evidence | When one high-quality cohort study and two or more high-quality case–control studies or at least three high-quality case–control studies generally show consistent findings. |
Limited evidence | Generally consistent findings in a single cohort study and/or in maximum two case–control studies, or in multiple cross-sectional studies. |
Conflicting evidence | Less than 75% of the studies reported consistent findings. |
Insufficient evidence | Less than two studies available. |
No evidence | When no study could be found. |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adekanla, B.A., Mbada, C.E., Idowu, O.A. et al. Clinical factors associated with bone mineral density among individuals with osteoarthritis of the hip and/or knee: a systematic review. Bull Fac Phys Ther 29, 46 (2024). https://doi.org/10.1186/s43161-024-00209-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43161-024-00209-3