Abstract
Background
Pathogenic fungi are the source of the fungal illness known as pulmonary mycosis. The prevalence of pulmonary mycoses among patients with pulmonary tuberculosis is continuously rising, despite improvements in the disease’s diagnosis, treatment, and management. Three hundred clinically confirmed patients with pulmonary tuberculosis were recruited for this study. Sputum samples were collected and analyzed to detect M. tuberculosis using the GeneXpert machine. Fungal elements were determined using microscopy, culture, and fungal biochemical analysis. Fungal isolates were confirmed using nested PCR with the internal transcribed sequence region of the ribosomal cistron of the fungal species.
Results
Of the 300 sputum samples analyzed, 50 (16.7%) patients had pulmonary tuberculosis. Fungi pathogens were found in 142 patients (47.3%), with 99/142 (71.2%) primary infections, and 40/139 (29.5%) secondary infections. Among the secondary infections, 33 (11%) were fungi coinfections with rifampicin-sensitive MTB coinfections, while 7 (2.3%) were fungi co-infected with rifampicin-resistant MTB. Candida albican was the most common fungus isolate, accounting for 44 (31.7%), while non-Candidal albicans accounted for only 2 (1.4%). Of the 99 species responsible for primary infection, 33 (23.7%) were Blastomyces precursors, 30 (21.6%) were Candida species, and 21 (15.1%) were Aspergillus fumigatus. The fungal pathogen with the highest frequency of secondary infection was Candida species 14 (10.1%), followed by Aspergillus fumigatus 11 (7.9%), then Blastomyces precursors, and then 09 (6.5%).
Conclusion
In conclusion, this study determined the prevalence rate of fungal pathogens among pulmonary tuberculosis patients. The most dominant species observed were Blastomyces species, which are seldom reported in Africa and Nigeria. The two others were Aspergillus and Candida species. The study showed that a high percentage of cases of this species, responsible for pulmonary mycosis, were misdiagnosed and treated as pulmonary tuberculosis. Thus, there is a need for improved surveillance and accurate diagnosis of pulmonary infections for proper treatment.
Similar content being viewed by others
Background
Pulmonary mycosis is a fungal infection caused by pathogenic fungi. The infection is caused by inhaling fungal spores, which attack the bronchial and lung tissues, leading to pulmonary fungal infection [9]. Pulmonary fungal infection is common among patients with a suppressed immune system due to the interruption in the fungal microflora [13]. An estimated 13 million cases of fungal infection and 1.5 million deaths have been reported across the globe, of which 60% were associated with pulmonary mycoses [3]. Conversely, pulmonary tuberculosis is a bacterial infection caused by Mycobacterium tuberculosis. The bacteria attack the lungs and destroy other organs in the body. In 2020, there will be an estimated 10 million new cases worldwide. 5.6 million men, 3.3 million women, 1.1 million children, and 1.5–2 million deaths worldwide in 2022 [8]. The mortality rate in pulmonary tuberculosis can be as high as 7% in patients with a weakened immune system [5, 10]. Similarly, pulmonary tuberculosis and mycosis are transmitted via airborne inhalation of bacterial droplets and fungal spores from infected individuals and overgrown fungal cultures in the environment. Intriguingly, pulmonary mycoses have similar manifestations, imaging features, signs, and symptoms to pulmonary tuberculosis [10, 20]. This contributed to the difficulty in diagnosing and treating pulmonary mycoses. The difficulty in treatment and diagnosis remains a significant public health threat in areas with high cases of pulmonary tuberculosis [8, 9].
The burden of pulmonary fungal infection is difficult to ascertain due to limited data in most developing countries. Despite this, opportunistic fungi, including Aspergillus species, Cryptococcus species, Pneumocystis species, and Histoplasma species, are the primary sources of fungal infections in the lungs of humans. Other endemic fungi, including Aspergillus fumigatus, Candida albicans, and Trichophyton rubrum, were associated with systemic fungal infections [2, 20]. In Nigeria, the prevalence of pathogenic fungal diseases was estimated at around 11.8%, whereas the incidence remains unclear because no central units are coordinating the surveillance of pathogenic fungal infections at the national level [9, 18]. Previous studies on treating pulmonary tuberculosis instead of mycoses were reported to affect the patient’s immunity. Thus, this exposed the susceptible patient to a pulmonary fungal infection [3, 4, 10]. Misdiagnosed and untreated acute pulmonary mycosis has an 80% chance of spreading and disseminating into chronic pulmonary mycoses with fatal consequences [9, 18, 20].
Despite advances in the diagnosis, treatment, and control of pulmonary tuberculosis and mycosis, there is a continuous increase in the number of pulmonary mycoses among patients with pulmonary tuberculosis [5, 7, 8, 18]. This study examined the level of pulmonary mycoses in patients with confirmed pulmonary tuberculosis in Kebbi State, Nigeria.
Methods
Study area
Kebbi State is located in Northern Nigeria. The state’s climate is tropical continental, influenced by tropical maritime and continental air masses. Dominant seasons are the wet and dry seasons. The temperature is generally high, with a mean annual temperature of about 26ºC in all locations. Except during the wet season, when relative humidity reaches an average of 8%, night temperatures are generally lower.
Study design
This is a hospital-based cross-sectional study conducted in the microbiology departments of five general hospitals using a gene Xpert machine to diagnose M. tuberculosis. The hospitals involved in this study are General Hospital Argungu, General Hospital Kamba, General Hospital Zuru, General Hospital Yauri, and Federal Medical Center Birnin-kebbi. Samples were collected from male and female patients positive for M. tuberculosis on the GeneXpert machine until the desired sample size was obtained. The study was carried out from July 2020 to March 2021.
Study subjects
Three hundred patients with confirmed M. tuberculosis were recruited for the study. They include (1) pulmonary tuberculosis patients with either rifampicin resistance or rifampicin-sensitive tuberculosis. (2) Patients with pulmonary tuberculosis who are not infected with pulmonary mycoses. (3) Patients with suspected cases of pulmonary mycoses infection and not on antifungal treatments. Patients with suspected pulmonary tuberculosis who did not provide sputum samples were excluded from this study. Approval to carry out this research was obtained from the Research Committee of the Kebbi State Ministry of Health. The adult participant signed informed consent, while written informed assent for minors was obtained from the guardian before sputum sample collection.
Specimen collection and processing
Sputum samples were collected in a sterile container. The samples were diagnosed using GeneXpert and fungus cultures and assays. The samples were processed in the pathology laboratory of the Federal Medical Center, Birnin Kebbi, on the same day they were collected. Samples awaiting processing were stored in a refrigerator at 4–8 °C. The socio-demographic and clinical status of the study patients whose samples were collected were recorded.
GeneXpert assay for detection of M. tuberculosis
Detection of M. tuberculosis from sputum specimens was determined using the GeneXpert assay machine (Cepheid, Sunnyvale, CA, USA). Briefly, an early morning sputum sample collected from patients was mixed with sample reagent in a ratio of 2:1 and allowed to settle at room temperature in the laboratory. Subsequently, 2 ml of the mixture was transferred into the GeneXpert cartridge and loaded into the GeneXpert machine for 2 h. The result was interpreted as “MTB detected” or “MTB not detected.”
Fungal culture, isolation, and identification
Potassium hydroxide (KOH) wet mounts
The potassium hydroxide (KOH) wet mounts were used to observe the presence or absence of fungal elements. Briefly, a drop of 10% KOH was placed on a clean glass slide using a Pasteur pipette. A small portion of sputum was mixed with a drop of KOH. The slide was covered with a coverslip and preserved in a moist chamber at room temperature for 30 min. The slide was viewed under the microscope using 10 and 40 objectives.
Gram staining for yeast cells
Briefly, a smear was made from the sputum samples on a clean glass slide. The cells and cell fragments are dried on a slide and stained with a standard Gram stain. The absence or presence of pseudohyphae in the sputum was recorded for gram-positive yeast-like cells. For differential staining, the slide was treated for 5 min with 1% phosphomolybdic acid, washed, and stained for 0.5 min with 1% aqueous methyl green. Whole or intact yeast cells appeared dark purple or black, while broken yeast cells with exposed cytoplasm were stained light purple.
Fungal culture
Sputum samples were streaked onto Sabouraud dextrose agar (SDA) to isolate pure colonies. The plates were inverted and incubated at 25–30 °C. The fungal growth on SDA plates was examined after seven days and held for four weeks before being reported as unfavorable. The morphology, texture, growth rate, colony surface, and pigmentation on the surface of SDA tubes were recorded. The fungal isolates on culture were identified using standard mycological procedures.
Lactophenol cotton blue staining
A drop of a small fragment of the fungal colony was placed on a grease-free glass slide containing lactophenol blue. The slide was covered with a coverslip, and the excess lactophenol blue stain was removed with blotting paper. The slide was viewed under the microscope using 10 and 40 objectives. The features and characteristics of fungal elements seen under the microscope were compared with established characteristic fungal features using mycology atlases.
Germ tube test
Candida albicans were identified by the germ tube tests. Yeast colonies were suspended in human serum in a test tube and incubated at 37 °C for 3 h. After observing a faintly turbid suspension, the suspension was examined under the microscope using 10 and 40 objectives to determine the presence or absence of germ tubes. The result is positive for C. albicans if germ tubes arose from the yeast cell and showed matching walls without any narrowing at their point of origin.
DNA extraction and amplification using PCR
Total DNA was extracted from 200 l of the suspension of the fungi isolate using a QIAamp Mini extraction kit according to the manufacturer’s protocol. The extracted DNA was stored at 200 ºC until used. The PCR was carried out using a Qiagen Top-Taq master mix kit. A 25-l reaction mix was prepared to contain 12.5 l of Qiagen Top Taq master mix and 1 l of 10 m-reach forward (ITS1-TCCGTAGGTGAACCTGCGG) and reverse (ITS4-TCCTCCGCTTATTGATATGC) primers [12]. These primers amplify approximately 600 base pairs of the ITS1-5.8S-ITS2 region of the ribosomal cistron: 1.5 l of coral load, 1 l of nuclease-free water, and 8 l of DNA template. The tubes were mixed and transferred into an Applied Biosystems 9700 computer programmed with the following cycling conditions: The first step was denaturation at 94° for 2 min, followed by 40 cycles at 94° for 30 s. The annealing was at 52° for 1 min, an extension at 72° for 1 min, and a final extension at 72° for 10 min. The amplicons were resolved in 1% agarose pre-stained with Safe Red. The gel image was viewed using a UV transilluminator (Analytik Jena US).
Statistical analysis
The data for each patient was entered and coded into Microsoft Excel 2013, version 1. The coded data were analyzed using Statistical Package for the Social Sciences (SPSS®, version 21; SPSS Inc., Chicago, IL, USA). Descriptive analysis was adopted to identify associations among variables. The associations between variables were presented as frequencies and percentages.
Results
Three hundred patients participated in the study. Of which 188 (63%) were males and 112 (37% were females). The patients’ ages ranged from 21 to 70 years old in 57 cases (19%), 31–40 years in 76 cases (25.3%), 41–50 years in 45 cases (15%), 51–60 years in 37 cases (12.3%), 61–70 years in 35 cases (11.7%), and more than 71 years in 7 cases (2.3%) (Table 1).
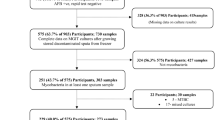
In all the sputum samples analyzed, 50/300 (16.7%) patients had pulmonary tuberculosis, of which 8 (2.7%) were rifampicin-sensitive MTB and 2 (0.7%) were rifampicin-resistant MTB. Fungal pathogens were detected in 139/300 (47.3%) patients; 99/139 (71.2%) were primary infections, while 40/139 (29.4%) were secondary infections. Among the secondary infections, 33 (11%) were fungi coinfections with rifampicin-sensitive MTB coinfections, while 7 (2.3%) were fungi co-infected with rifampicin-resistant MTB coinfections (Table 2).
Candida albican was the highest occurring fungal isolate with 44 (31.7%), followed by Blastomyces percursus with 43 (30.2%), and then Aspergillus fumigatus and Aspergillus niger with 32 (23%) and 14 (10.1%), respectively. The least common species were non-Candidal albicans, with 2 (1.4%) (Table 3). Of the 99 species responsible for primary infection, 33 (23.7%) were Blastomyces precursors, 30 (21.6%) were Candida species, and 21 (15.1%) were Aspergillus fumigatus (Table 4). The fungal pathogen with the highest frequency of secondary infection was Candida species 14 (10.1%), followed by Aspergillus fumigatus 11 (7.9%), then Blastomyces precursors 09 (6.5%) (Table 4).
The gel electrophoresis analysis of randomly selected species confirmed the presence of approximately 600 base pairs in the internal transcribed sequence region of the ribosomal cistron of the fungal species isolated from patients with confirmed cases of pulmonary tuberculosis and pulmonary mycosis, as shown in Fig. 1. From the figure, M denotes marker, 1 denotes Aspergillus species, 2 denotes Candida species, three denotes non-Candida species 1, 4 denotes non-Candida species 2, 5 denotes Blastomyces precursors, and NC denotes negative control accordingly.
Discussion
In Nigeria and many regions around the globe, there is a gradual increase in pulmonary fungal infections caused by opportunistic fungal pathogens, especially among patients with pulmonary tuberculosis. This study examined the level of pulmonary mycoses in patients with confirmed pulmonary tuberculosis in Kebbi State, Nigeria. The current study revealed a 16.7% prevalence of pulmonary tuberculosis. The prevalence of pulmonary tuberculosis is slightly lower than 19.7% in the study area [7, 8]. The decrease in the prevailing rate of pulmonary tuberculosis might be due to the rate of successful treatment outcomes recorded in the area [8].
The prevalence of pulmonary fungal pathogens was 71.2%, and a 29.4% prevalence of pulmonary mycoses was observed in patients with confirmed pulmonary tuberculosis. The study revealed a high prevalence rate of the fungal pathogen, similar to reports of 74% among presumptive tuberculosis cases in Nigeria [21]. The finding on the prevalence rate of pulmonary mycoses in patients with confirmed pulmonary tuberculosis in Gombe was 6% (Sani et al., 2020), compared to 29.4% in this study. Nevertheless, it is higher among HIV patients in Maiduguri, Nigeria (68%) [16]. Other prevalent rates were reported in Ghana among chronic pulmonary Aspergillosis patients coinfected with presumed tuberculosis (50%) [17], 68% in patients with lung cancer cases [15] a coinfection rate of (15.4%) in Africa and Asia among pulmonary tuberculosis patients [11, 14]. The difference in prevalence rate might be primarily due to the study area and population, study designs, sampling, and diagnostic methods. In HIV patients, the variation might be due to immune suppression by the virus, while in pulmonary tuberculosis, it could be due to the prolonged use of antibiotics, which upset patients’ normal flora by making the patient susceptible to mycoses [3, 10, 18].
Blastomyces precursor was the predominant species isolated (23.7%), of which 6.5% were coinfections with patients confirmed to have pulmonary tuberculosis. The finding is similar to studies reported in Zaria among pulmonary TB patients [1] and around the world among patients managed for pulmonary tuberculosis [9]. In Africa and Nigeria, pulmonary blastomycosis is a rare pathologic condition [6]. Thus, blastomycosis pathogens are misdiagnosed as bacterial pneumonia in their acute stage and treated as pulmonary tuberculosis when chronic in tuberculosis burden areas [11]. This was evident in reported clinical cases of a 37-year-old Nigerian diagnosed with pulmonary blastomycosis after receiving extended treatment for pulmonary tuberculosis [11, 18].
C. albicans was the second-most common fungal pathogen isolated in this study, accounting for 21.6%, and the most common fungal pathogen isolated in patients with pulmonary tuberculosis, accounting for 10.1%. C. albicans is an opportunistic fungal pathogen that affects individuals with a prior history of pathogenic infectious disease with prolonged treatment therapy [4, 13]. The combined prevalence of C. albicans was reported to be between 12.7 and 36 among tuberculosis patients [5, 10]. The high occurrence of this species among pulmonary patients indicates fungal colonization due to the extended use of antibiotics. C. albicans was previously reported and has remained the most frequently isolated Candida species in the clinical setting [20]. However, this study shows that the incidence rate of other candida and non-Candida infections is increasing in some countries, including sub-Saharan Africa.
Pulmonary aspergillosis is a rare pulmonary disease complicating other respiratory disorders such as tuberculosis. However, in this study, A. fumigatus was the second most prevalent secondary fungal pathogen, at 7.9%. This result is lower than the reported pooled prevalence of Aspergillus coinfection among patients with pulmonary tuberculosis in Asia (14.7%) and Africa (17.7%) [17]. The rate at which Aspergillus species cause pulmonary mycoses is attributed to their ability to survive different environmental conditions similar to the study area [19]. They also possess unique spore-producing structures that release spores or conidia into the atmosphere, easily penetrate deep into the branches of air tubes in the lungs, and survive [2, 10, 19].
Findings from this study showed that elderly pulmonary tuberculosis patients had higher cases of pulmonary fungal infection than younger ones. Most studies found that older age groups had higher rates of fungal infections and a link between age and mycoses and tuberculosis coinfection [2, 10, 18]. Undeniably, old age is a known risk factor for pulmonary fungal infection due to a weakening immune system, as one grows older. Pulmonary tuberculosis is prevalent among immunocompromised patients and the same with pulmonary mycoses because it is an opportunistic infection. However, it is common for pulmonary fungal pathogens to co-exist with other microbes in the same infection niche. Therefore, either of the two can manifest in immunocompromised patients. The suppressed immune system of an immunocompromised patient disrupts the fungal flora and worsens the underlying process of lung infection [10, 18]. Pulmonary fungal pathogens and infections are more prevalent in males than females recruited in this study. This corroborates previous studies that reported two-thirds of pathogenic mycoses were isolated in males compared with females [5, 10, 18]. The male might be exposed to much more airborne fungal spores and conidia because they stay outdoors due to their role in the community as breadwinners, compared to females, who are mostly indoors in the study area. This study did not report the comorbidities and radiology of the cases under investigation because the study was based on medical laboratory sciences of diagnosis of pulmonary tuberculosis infection and pulmonary fungal infection but not clinical case studies. However, all clinical and radiological findings showing the status of the patients recruited in the study were confirmed before they were included.
In conclusion, this study determined the prevalence rate of fungal pathogens among pulmonary tuberculosis patients. The most dominant species observed were Blastomyces, rarely reported in Africa and Nigeria. The two others were Aspergillus and Candida species. The study showed that many cases of this species, responsible for pulmonary mycosis, were misdiagnosed and treated as pulmonary tuberculosis. Thus, there is a need for improved surveillance and accurate diagnosis of pulmonary infections for proper treatment. In addition, due to the high prevalence of pulmonary fungal pathogens in this study, the radiology of the cases needs to be looked into in subsequent studies.
Availability of data and materials
The datasets are available from the corresponding author upon request.
Abbreviations
- MTB:
-
Mycobacterium tuberculosis
- KOH:
-
Potassium hydroxide
- SDA:
-
Sabouraud dextrose agar
- DNA:
-
Deoxyribonucleic acid
- ITS:
-
Internal transcribed sequence
- HIV:
-
Human immunodeficiency virus
References
Anjorin FI, Kazmi R, Malu AO, Lawande RV, Fakunle YM (1984) A case of blastomycosis from Zaria, Nigeria. Trans R Soc Trop Med Hyg 78:577–580
Benedict K, Richardson M, Vallabhaneni S, Jackson BR, Chiller T (2017) Emerging issues, challenges, and changing epidemiology of fungal disease outbreaks. Lancet Infect Dis 17:e403–e411
Bongomin F, Gago S, Oladele RO, Denning DW (2017) Global and multi-national prevalence of fungal diseases-estimate precision. J Fungi (Basel, Switzerland) 3(4):57
Bongomin F, Ekeng BE, Kibone W, Nsenga L, Olum R, Itam-Eyo A et al (2022) Invasive fungal diseases in Africa: a ritical literature review. J Fungi 8(12):1236
Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, Kapata N, Mfinanga S, Hasnain SE, Katoto P, Bulabula ANH, Sam-Agudu NA, Nachega JB, Tiberi S, McHugh TD, Abubakar I, Zumla A (2021) Global Tuberculosis Report 2020 - reflections on the global TB burden, treatment and prevention efforts. Int J Infect Dis 113(Suppl 1):S7–S12
Cheikh Rouhou S, Racil H, Ismail O, Trabelsi S, Zarrouk M, Chaouch N, Hantous S, Khaled S, El Mezni F, Chabbou A (2008) Pulmonary blastomycosis: a case from Africa. ScientificWorldJournal 8:1098–1103
Danlami MB, Aliyu B, Samuel G (2021) Incidence of rifampicin-resistance presumptive M. tuberculosis cases among outpatients in Kebbi State. Nigeria Afr J Infect Dis 15:47–52
Danlami MB, Basiru A, Tajjudeen Y, Bazata AY, Gulumbe BH, Mohammed M (2022) Tuberculosis treatment outcomes among pulmonary TB patients attending public hospitals in Kebbi State, Northern Nigeria: a four-year retrospective study. Bull Natl Res Cent 46:281
Ekeng BE, Davies AA, Osaigbovo II, Warris A, Oladele RO, Denning DW (2022) Pulmonary and extrapulmonary manifestations of fungal infections misdiagnosed as tuberculosis: the need for prompt diagnosis and Management. J Fungi (Basel) 8(5):460
Harding E (2020) WHO global progress report on tuberculosis elimination. Lancet Respir Med 8:19
Kumar A, Kunoor A, Eapen M, Singh PK, Chowdhary A (2019) Blastomycosis misdiagnosed as tuberculosis, India. Emerg Infect Dis 25:1776–1777
Martin KJ, Rygiewicz PT (2005) Fungal-specific PCR primers developed for the analysis of the ITS region of environmental DNA extracts. BMC Microbiol 5:28
Matsuda JDS, Wanke B, Balieiro A, Santos C, Cavalcante R, Muniz MM, Torres DR, Pinheiro SB, Frickmann H, Souza JVB, Martinez-Espinosa FE (2021) Prevalence of pulmonary mycoses in smear-negative patients with suspected tuberculosis in the Brazilian Amazon. Rev Iberoam Micol 38:111–118
Mohamed A, Obanda BA, Njeri HK, Loroyokie SN, Mashedi OM, Ouko TT, Gatumwa EM, Korir RK, Yaguchi T, Bii CC (2022) Serological evidence of chronic pulmonary Aspergillosis in tuberculosis patients in Kenya. BMC Infect Dis 22:798
Mohammad Khairy El-Badrawy ARE, Ibrahim AAM, Eladl AE, Elmorsey RA (2023) Prevalence and pattern of isolated fungi from bronchoalveolar lavage among patients with lung cancer: a prospective cross-sectional study. Egypt J Bronchol 17:7
Talle M, Hamidu IM, Nasir IA, Abubakar M, Kalama BD, Mustapha J et al (2017) Prevalence and profile of pulmonary fungal pathogens among HIV-infected patients attending University of Maiduguri Teaching Hospital, Nigeria. Egypt J Intern Med 29:11–15
Ocansey BK, Otoo B, Adjei A, Gbadamosi H, Kotey FCN, Kosmidis C et al (2022) Chronic pulmonary aspergillosis is common among patients with presumed tuberculosis relapse in Ghana. Med Mycol 60(9):mmy/myac063
Oladele RO, Denning DW (2014) Burden of serious fungal infection in Nigeria. West Afr J Med 33:107–114
Jakribettu RP, George T, Abraham S, Farhan F, Shreevidya K, Manjeshwar SB (2019) Clinical and laboratory profile of chronic pulmonary aspergillosis: a retrospective study. Egypt J Bronchol 13:109–113
Salzer HJF, Burchard G, Cornely OA, Lange C, Rolling T, Schmiedel S, Libman M, Capone D, Le T, Dalcolmo MP, Heyckendorf J (2018) Diagnosis and Management of Systemic Endemic Mycoses Causing Pulmonary Disease. Respiration 96:283–301
Sani FM, Uba A, Tahir F, Abdullahi IN, Adekola HA, Mustapha J, Nwofe J, Usman Y, Daneji IM (2020) Spectrum of pulmonary fungal pathogens, associated risk factors, and anti-fungal susceptibility pattern among persons with presumptive tuberculosis at Gombe, Nigeria. Int J Mycobacterial 9:144–149
Acknowledgements
We acknowledged the four General Hospitals in Kebbi State and the Federal Medical Center Birnin Kebbi and State Ministry of Health for the support given towards the successful completion of this research.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
MBD, AMA, SSM, YOT, MBM, and ZMK Conceived and designed the experiments: MBD, AMA, and SSM, Analyzed the data: MBD and AM, MBM. Contributed materials and analysis tools: MBD, AMA, SSM, and YOT. Wrote the paper: MBD, AMA, ZMK and SSM. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Kebbi State Health Research Ethics Committee. Verbal informed consent was obtained from all patients who consented to participate in the study as approved by the research ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Danlami, M.B., Adefowepo, A.M., Manga, S.S. et al. Pulmonary mycoses among pulmonary tuberculosis in Kebbi State North Western Nigeria. Egypt J Bronchol 17, 39 (2023). https://doi.org/10.1186/s43168-023-00214-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00214-5