Abstract
Objective
This study aimed to investigate the occurrence of medication-related osteonecrosis of the jaw (MRONJ) after tooth extraction due to periodontitis in ovariectomized rats.
Methods
Twenty-four osteoporosis-induced rats were administered with zoledronic acid (ZA; ZA group) or saline (CONT group). In both groups, tooth extraction was performed after inducing periodontitis, and all animals were sacrificed 8-week after tooth extraction.
Results
Micro-CT of the tibia showed that the bone volume fraction, bone surface density, trabecular number, and bone mineral density were significantly higher in the ZA group than in the CONT group. Histologically, the proliferative zone on the growth plate was thicker in the ZA group than in the CONT group. Micro-CT of the extraction sites revealed that the bone volume fraction was significantly higher in the ZA group than in the CONT group. Radiologically, the ZA group showed partial healing and delayed healing. Histological analysis revealed normal bone healing status with completely healed epithelium in the extraction sites of the CONT group, whereas abnormal empty osteocytes in the necrotic bone and inflammatory infiltration were observed in the ZA group.
Conclusion
The incidence of MRONJ increased in the rats administered with ZA.
Similar content being viewed by others
Introduction
Bisphosphonates (BP) are representative drugs affecting bone metabolism and are widely used in osteoporosis treatment. They prevent bone resorption by inhibiting the activation of osteoclasts [1,2,3]. BP are also used to treat bone diseases in multiple myeloma and bone metastases associated with solid tumors by inhibiting the bone resorption and angiogenesis [4,5,6]. The most serious side effect of BP is osteonecrosis of the jaw (ONJ). ONJ was first reported after dental treatment in BP-treated patients by Marx in 2003 [7]. There have been many reports of side effects associated with BP since Marx’s report, and BP-associated jaw necrosis was defined as bisphosphonate-related osteonecrosis of the jaw (BRONJ) [8]. Recently, it has been defined as medication-related osteonecrosis of the jaw (MRONJ) in association with anti-resorptive or anti-angiogenic medications, such as denosumab [9, 10].
The incidence of MRONJ is reportedly related to the duration, type, and dosage of BP administration [11, 12]. Particularly, higher incidence of MRONJ has been reported with high-dose intravenous zoledronic acid (ZA) than with oral BP [8, 13]. Dental causes considered as risk factors for MRONJ include tooth extractions following periodontal or periapical diseases and dental surgeries, such as periodontal flap surgery or micro-endodontic surgery [14, 15]. The major manifestation of MRONJ is exposure of the alveolar bone, which is accompanied by pain, edema, paresthesia, suppuration, and soft tissue ulceration [15]. The most serious problem with MRONJ is that effective treatment is evasive, despite the best oral healthcare practices including antibiotic therapy, parathyroid hormone therapy, and surgical debridement/resection [9, 16, 17]. Because the treatment of MRONJ is usually difficult and recurrence is frequent, efficient prevention of MRONJ in susceptible patients is vital.
The pathophysiology of MRONJ has not been elucidated completely, and several hypotheses have been suggested to explain its mechanism [18,19,20,21]. Many previous studies have used animal models that differ from the actual patients in clinic [22,23,24]. Most patients with MRONJ are female, old, and menopausal [8]. They have local inflammatory conditions such as periodontal or periapical diseases and general immunosuppressive conditions [25,26,27]. It has been reported that removal of inflammation prior to tooth extraction reduces the incidence of osteonecrosis [28]. Kim et al. emphasized the importance of dental pulp and periodontal disease as local factors in the development of MRONJ [28]. However, in the case of animal experiments, healthy teeth are extracted, which is a model that has difficulty in understanding the mechanism of MRONJ. Therefore, it is important to develop an animal model similar to the situations of such patients, with the local and systemic risk factors for MRONJ, in order to perform animal experiments that can be applied in clinics.
In this study, the effect of periodontitis on the pathogenesis of MRONJ was investigated using a periodontitis-induced animal model before tooth extraction.
Methods
Animals
In this study, 24 skeletally mature, 12-week-old, female Sprague-Dawley rats (Orientbio Co., Ltd.; Seongnam-si, Gyenggi-do, Korea) were used. The mean weight of the animals was 281 g at 12 weeks of age and 421 g immediately before sacrifice. The animals were housed under standard laboratory conditions (temperature, 20 °C ± 5 °C; humidity, 50% ± 10%; lighting cycle, 12 h light/12 h dark), with 2–3 rats per cage and marked individually. All animals had ad libitum access to standard laboratory pellet diet and water. This investigation was carried out in accordance with the revised animals Act 1986 in the UK used for scientific procedure, and confirm the study complied with the ARRIVE guidelines. Animal selection, management, surgical protocol, and preparation followed a routine protocol approved by the Institutional Animal Care and Use Committee of Yonsei University Health System (IACUC No. 2016 − 0171).
Experimental design
These 24 animals were randomly divided into two groups administered with saline (CONT group, N = 13) and zoledronic acid (ZA) (ZA group, N = 11), respectively (Fig. 1). Based on the results of the pilot study, the sample size was calculated, and G-power 3.1 was used. This was set at an effect size of 0.5, significance of 0.05, and power of 90%. Considering the dropout rate of 20%, 13 animals per group were finally calculated. At 12 weeks of age, bilateral ovariectomy (OVX) was performed in all animals under general anesthesia by intraperitoneal combination injection of tiletamine and zolazepam (50 mg/mL, 0.6 mL/kg; Zoletil®, Virbac Lab. Carros, France) and xylazine (23.32 mg/mL, 0.4 mL/kg; Rompun®, Bayer, Leverkusen, Germany). The OVX procedure is as follows: After shaving the spine, such as the lower abdomen, disinfect it. Afterwards, a 15 mm incision is made in the skin and a 5 mm incision is made in the peritoneum where the left/right ovary is located. The OVX is performed by exposing the ovary, and the remaining organs are placed back into the peritoneum. The peritoneum is not sutured, only the dorsal skin is sutured.
Postoperatively, meloxicam (1 mg/kg, once a day for 5 days; Metacam®, Boehringer Ingelheim, Rhein, Germany) and enfloxacin (10 mg/kg/day, once a day for 5 days; Baytril®, Bayer, Germany) were administered subcutaneously (SC).
Eight weeks later, 4 − 0 black silk ligation was performed on the cervical portion of the right mandibular first molar (M1) and second molar (M2) under general anesthesia in all rats (Fig. 1). Four weeks later, ZA (Zometa ready®, Novartis, Basel, Switzerland; 40 µg/kg, once a week for 4 weeks) was administered in the ZA group and saline (same volume as ZA) in the CONT group intravenously (IV) [29, 30].
Eight weeks later, silk remove with tooth extraction was performed under general anesthesia in all animals. Clinical observations such as gingival tenderness and tooth mobility around the ligated teeth were made before tooth extraction and silk removal. Local anesthesia was induced using 2% lidocaine (1: 80,000 epinephrine). The ligated right mandibular M1 and M2 were extracted using a sharp dental explorer after ensuring sufficient mobility. Bleeding was controlled by gauze pressure, and suturing was not required. After tooth extraction, meloxicam and enfloxacin were administered SC to prevent postoperative infection and achieve pain control.
All animals were sacrificed 8 weeks after tooth extraction by perfusion under general anesthesia. After removing the skin, the organs were extracted and fixed in 10% formalin.
Micro-computed tomography (micro-CT)
Ten specimens (CONT group, N = 5; ZA group, N = 5) were subjected to micro-CT (Skyscan1173, Skyscan, Konitch, Belgium) at 100 kV, 100 µA, and 13.86 μm pixel size in the tibia and 18.12 μm pixel size in the jaw. CTAn (Skyscan, Aartselaar, Belgium) was used to reconstruct and analyze the images.
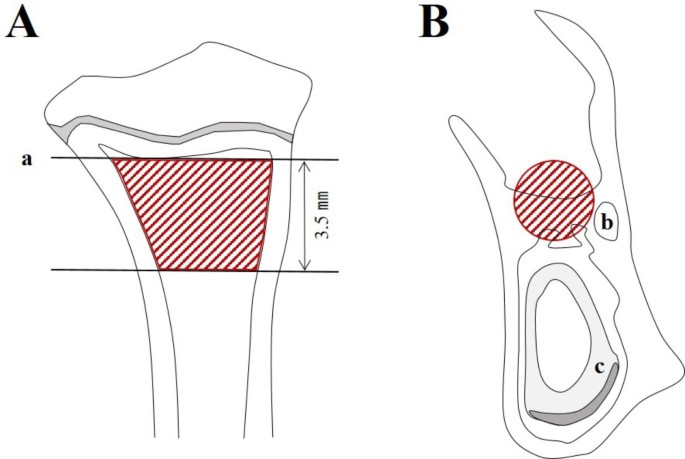
For the trabecular bone morphometry of the tibia, the region of interest (ROI) in the tibia was the growth plate and 3.5 mm of the upper trabecular bone (Fig. 2A and a) [31]. For the trabecular bone morphometry of the extraction site, the ROI was the interradicular bone of Ø0.6 mm-sized cylindrical shape in the coronal view (Fig. 2B, b and c). The posterior border was the mesial root surface of the third molar, and the anterior border was considered 4 mm from the posterior border.
The bone volume fraction (bone volume [BV]/total volume [TV], %), specific bone surface (bone surface [BS]/BV, mm2/mm3), bone surface density (BS/TV, mm2/mm3), trabecular number (Tb.N, 1/mm), trabecular thickness (Tb.Th, mm), trabecular separation (Tb.Sp, mm), and bone mineral density (BMD, g/cm2) of each specimen were assessed in trabecular bone morphometry [32].
Histology
All specimens were decalcified using 10% ethylenediaminetetraacetic acid, embedded in paraffin, and 4-µm serial coronal sections were obtained. Hematoxylin and eosin staining was performed according to the manufacturer’s recommendations. Images were scanned using a light microscope (Case Viewer, 3DHISTECH Ltd., Budapest, Hungary). Histologically, MRONJ was diagnosed when one or more of the following signs were observed: exposed bone, necrotic bone, inflammatory infiltration, or sequestrum [33].
Statistical analysis
Statistical analyses were performed using Statistical Product and Service Solutions (IBM SPSS 23.0, IBM Corp., Armonk, NY, USA). Mann-Whitney U-test and chi-squared test were used to compare parameters between the CONT and ZA groups; p-values < 0.05 were considered statistically significant.
Results
Only 24 of 26 rats were included in the results. Two animals in the ZA group died. Both animals died of respiratory arrest during the tooth extraction process. The sample size was determined considering a dropout rate of 20%. Therefore, additional recruitment was not performed because the analyzed value of 24 rats did not affect the results.
No unexpected side effects (weight loss, behavioral abnormalities, serious infection at the experimental site) were found.
Micro-computed tomography: proximal tibia
Figure 3a and b show the difference in the tibia between the two groups after sacrificing the rats. In the CONT group, a thin and low-density growth plate was observed, whereas thick and high-density growth plates and high-density trabecular patterns were observed in the ZA group. Furthermore, in the cortical bone of the tibia, the ZA group showed higher BMD than that of the CONT group. The BV/TV, BS/TV, Tb.N, and BMD values were significantly higher in the ZA group than in the CONT group (Fig. 3c).
Micro-computed tomography: extraction socket
The extraction sockets showed different healing patterns between the ZA and CONT groups. The CONT group showed almost complete healing of the extraction socket, whereas the ZA group showed partial healing and delayed healing (Fig. 4a, b). The BV/TV of the extraction sockets was significantly higher in the CONT group than in the ZA group (Fig. 4c).
Treatment effect of ZA on the extraction site. A Micro-CT image of the CONT group, B Micro-CT image of the ZA group, C Micro-CT analysis of the trabecular bone (EXT socket, white square box; M3 root, red arrow; Incisor pulp chamber, white asterisk; *, P < 0.05)
Abbreviations: ZA = zoledronic acid, Micro-CT = micro-computed tomography, EXT = extraction, M3 = 3rd molar
Histology: proximal tibia
As compared to the ZA group, the CONT group showed a thinner proliferative zone of the growth plate and less clear trabecular pattern (Fig. 5a). The ZA group showed a thicker proliferative zone of the growth plate than that of the CONT group, and many trabecular patterns were observed in the bone marrow of the former (Fig. 5b).
Histology: extraction socket
Normal bone healing with completely healed epithelium at the extraction sites was observed in the CONT group, as were many normal osteocytes (Fig. 6a-d). In contrast, abnormal empty osteocytes in the necrotic bone and inflammatory infiltration were observed in the extraction sockets of the ZA group (Fig. 6e-h). Also alveolar bone resorption and furcation involvement around the M1 and M2 areas were observed in all the rats.
Representative images of the tooth extraction sites (100 and 200 x magnification). A-D CONT group, E-H ZA group (Normal bone healing state, black arrowhead; Completely filled EXT socket with bone, black asterisk; Normal osteocyte, black arrow; Opened wound, yellow box; Inflammatory infiltration, yellow asterisk; Empty lacunae, yellow arrow; Osteoclast, yellow arrowhead)
Abbreviations: EXT = extraction
Incidence of MRONJ-like lesions
MRONJ-like lesion were diagnosed based on the histological criteria (Fig. 7). The incidence of CONT group and ZA group were 68.1% (15 sites/22 sites) and 7.7% (2 sites/26 sites), respectively. The incidence of MRONJ lesions was significantly higher in the ZA group than in the CONT group (P < 0.000).
Discussion
In this study, MRONJ incidence was investigated when ZA was administered and tooth extraction was performed after inducing periodontitis in OVX rats. Although ZA improved the osteoporosis induced in the long bones, it also induced MRONJ onset.
Periodontal disease and caries are among the most common causes of tooth extraction [34]. MRONJ occurs in patients after tooth extraction, and the teeth cannot be restored owing to periapical infection with advanced dental caries or periodontal disease [20, 35, 36]. Inducing periodontal lesions was attempted by placing tooth ligation on the cervical portion of the teeth for 8 weeks before extraction. Duarte et al. reported that bacterial species commonly observed in humans were found in the biofilm around the ligature 42 days after ligation in the rats [37]. Liu et al. reported that a 28-day ligature could cause significant loss in the trabecular pattern of the alveolar bone in rats [38]. Therefore, the tooth ligation was kept for 8 weeks in our study, and this duration was adequate to induce periodontal lesions. However, there was no visible gingival inflammation or tooth mobility observed 8 weeks after ligation, which was an unexpected outcome. Additionally, the amount of alveolar bone resorption was less than expected. This could be explained by the rapid metabolism in rats and their remarkable ability to regenerate. Many previous studies have attempted to overcome the limitations of tooth ligation used to induce periodontal disease in animal models in various ways [39, 40]. It is necessary to include experimental data using different methods of inducing periodontal disease [41,42,43].
In the micro-CT analysis, as seen in previous studies, osteoporosis was induced in the long bone by performing OVX, and improved bone quality was observed with ZA administration; however, the mandible showed different findings. When MRONJ occurs, the BV/TV decreases because bone loss increases due to bone resorption and sequestrum formation. Due to the inhibitory action of ZA on osteoclasts, bone resorption is suppressed, BS/BV is lowered, and BS/TV is increased. Thus, there was substantial inflammation in and around the tooth extraction sockets in the ZA group in our study. In the ZA group, the Tb.Th and Tb.N values were high, but the Tb.Sp was low. These values are used to evaluate the characteristics of trabecular bone in osteoporosis, which shows decreased BV/TV, Tb.Th, and Tb.N and increased Tb.Sp; therefore, they can be used to evaluate the effectiveness of osteoporosis drugs. However, it is considered that the bone in a state of increased inflammation due to MRONJ should not be interpreted as an evaluation criterion for non-inflammatory trabecular bone. Summarizing the results of the tibia and jaw, we found that the BV/TV, Tb.Th, and Tb.N were high and Tb.Sp was low in the non-inflammatory state (tibia), but the BV/TV showed contrasting findings in the inflamed state (jaw) (Figs. 3 and 4). This is because osteosclerosis of the trabecular bone occurs when osteomyelitis develops.
MRONJ was diagnosed according to the histological criteria (exposed bone, necrotic bone, inflammatory cell infiltration, or sequestrum) at the extraction site. This was because there were MRONJ lesions in some rat specimens that could not be clinically detected and were only observed in the microscopic analysis. Although the definition of MRONJ is based on the macroscopic appearance in the clinic, MRONJ was diagnosed based on the following histological criteria under experimental conditions: (1) presence of ulcerative lesions with exposed and necrotic bone and/or osteolysis [44]; (2) presence of pseudo-epitheliomatous-like hyperplasia of the epithelium accompanied by inflammatory infiltration [31]; and (3) presence of sequestrum and bacterial colonies [8, 45]. The incidence of MRONJ in the ZA group was significantly higher than that in the CONT group. Notably, the incidence of 7.7% in the CONT group was unexpected. These results could be attributed to the general condition and root morphology of the rats. The rats used in this experiment could be considered immunosuppressed because they represented postmenopausal women with osteoporosis. Therefore, the extraction sites of the CONT group may have also shown inflammatory findings. The other reason is the morphological characteristics of the rat molars. Rat molars have more divergent roots than those of humans, resulting in more chances of remnant root pieces, which may affect the healing of the extraction sites. Fractured root was confirmed in 2 animals in the CONT group and 1 animal in the ZA group. Fractured root was 1 per tooth in all animals.
Many studies have been conducted to elucidate the pathogenesis of MRONJ, and there are several reports on those related to periodontal and pulp diseases in rats [46,47,48,49,50]. Particularly, when a surgical procedure such as tooth extraction is performed in a state of chronic inflammation such as periodontitis, the incidence of MRONJ is high [46,47,48,49]. Although various hypotheses have been proposed regarding the pathogenesis of MRONJ, the mechanism related to macrophage activation is considered the most influential [46]. It has been reported that MRONJ develops when ZA is administered in a periodontitis-induced rodent model [28]. Moreover, if tooth extraction is performed in the presence of periodontitis, the incidence of MRONJ increases, and the incidence of MRONJ is reduced when tooth extraction is performed in a healthy state in which inflammation is removed by treating periodontitis [51]. Interleukin-17 cytokine was found to increase the M1/M2 macrophage ratio in the mucosa surrounding the MRONJ affected area, suggesting that the activation of M1 macrophages acts as a major risk factor for MRONJ [52].
A limitation of this study is that a comparison of the incidence of MRONJ between ligated and non-ligated teeth was not performed. To investigate whether periodontal disease-induced extraction is a risk factor for MRONJ, ligated and non-ligated teeth should be extracted simultaneously from one specimen and analyzed to compare the differences of the extraction sites. The ligation period and ZA dose should be further adjusted in future studies. Moreover, an experimental design reflecting the withdrawal period before and after the extraction to simulate the patient’s situation is warranted.
Conclusion
In conclusion, our findings suggest that the pathological inflammatory state of the periodontal tissue after ZA administration is likely to induce MRONJ after tooth extraction.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMD:
-
Bone mineral density
- BP:
-
Bisphosphonate
- BRONJ:
-
Bisphosphonate-related osteonecrosis of the jaw
- BS/BV:
-
Specific bone surface
- BS/TV:
-
Bone surface density
- BS:
-
Bone surface
- BV:
-
Bone volume
- IV:
-
Intravenously
- M1:
-
First molar
- M2:
-
Second molar
- MRONJ:
-
Medication-related osteonecrosis of the jaw
- ONJ:
-
Osteonecrosis of the jaw
- OVX:
-
Ovariectomy
- ROI:
-
Region of interest
- SC:
-
Subcutaneously
- Tb.N:
-
Trabecular number
- Tb.Sp:
-
Trabecular separation
- Tb.Th:
-
Trabecular thickness
- TV:
-
Total volume
- ZA:
-
Zoledronic acid
References
Hughes DE, MacDonald BR, Russell RG, Gowen M. Inhibition of osteoclast-like cell formation by bisphosphonates in long-term cultures of human bone marrow. J Clin Invest. 1989;83(6):1930–5.
Hughes DE, Wright KR, Uy HL, Sasaki A, Yoneda T, Roodman GD, et al. Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res. 1995;10(10):1478–87.
Vitte C, Fleisch H, Guenther HL. Bisphosphonates induce osteoblasts to secrete an inhibitor of osteoclast-mediated resorption. Endocrinology. 1996;137(6):2324–33.
Pozzi S, Raje N. The role of bisphosphonates in multiple myeloma: mechanisms, side effects, and the future. Oncologist. 2011;16(5):651–62.
Green JR. Antitumor effects of bisphosphonates. Cancer. 2003;97(3 Suppl):840–7.
Santini D, Vincenzi B, Dicuonzo G, Avvisati G, Massacesi C, Battistoni F, et al. Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res. 2003;9(8):2893–7.
Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61(9):1115–7.
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of oral and maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw–2014 update. J Oral Maxillofac Surg. 2014;72(10):1938–56.
Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O’Ryan F, et al. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res. 2015;30(1):3–23.
Svejda B, Muschitz C, Gruber R, Brandtner C, Svejda C, Gasser RW, et al. [Position paper on medication-related osteonecrosis of the jaw (MRONJ)]. Wien Med Wochenschr. 2016;166(1–2):68–74.
Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D. American Association of oral and maxillofacial Surgeons’ position paper on medication-related osteonecrosis of the Jaws-2022 Update. J Oral Maxillofac Surg. 2022;80(5):920–43.
Yarom N, Shapiro CL, Peterson DE, Van Poznak CH, Bohlke K, Ruggiero SL, et al. Medication-related osteonecrosis of the Jaw: MASCC/ISOO/ASCO Clinical Practice Guideline. J Clin Oncol. 2019;37(25):2270–90.
Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol. 2011;29(9):1125–32.
Hoff AO, Toth BB, Altundag K, Johnson MM, Warneke CL, Hu M, et al. Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. J Bone Miner Res. 2008;23(6):826–36.
Walter C, Al-Nawas B, Grotz KA, Thomas C, Thuroff JW, Zinser V, et al. Prevalence and risk factors of bisphosphonate-associated osteonecrosis of the jaw in prostate cancer patients with advanced disease treated with zoledronate. Eur Urol. 2008;54(5):1066–72.
Owosho AA, Estilo CL, Huryn JM, Yom SK. Pentoxifylline and tocopherol in the management of cancer patients with medication-related osteonecrosis of the jaw: an observational retrospective study of initial case series. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(4):455–9.
Rubin MR, Bilezikian JP. The anabolic effects of parathyroid hormone therapy. Clin Geriatr Med. 2003;19(2):415–32.
Mashiba T, Hirano T, Turner CH, Forwood MR, Johnston CC, Burr DB. Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res. 2000;15(4):613–20.
Rogers MJ, Watts DJ, Russell RG. Overview of bisphosphonates. Cancer. 1997;80(8 Suppl):1652–60.
Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63(11):1567–75.
Reszka AA, Halasy-Nagy J, Rodan GA. Nitrogen-bisphosphonates block retinoblastoma phosphorylation and cell growth by inhibiting the cholesterol biosynthetic pathway in a keratinocyte model for esophageal irritation. Mol Pharmacol. 2001;59(2):193–202.
Dayisoylu EH, Senel FC, Ungor C, Tosun E, Cankaya M, Ersoz S, et al. The effects of adjunctive parathyroid hormone injection on bisphosphonate-related osteonecrosis of the jaws: an animal study. Int J Oral Maxillofac Surg. 2013;42(11):1475–80.
Maahs MP, Azambuja AA, Campos MM, Salum FG, Cherubini K. Association between bisphosphonates and jaw osteonecrosis: a study in Wistar rats. Head Neck. 2011;33(2):199–207.
Zandi M, Dehghan A, Ghadermazi K, Malekzadeh H, Akbarzadeh M. Perioperative discontinuation of intravenous bisphosphonate therapy reduces the incidence and severity of bisphosphonate-related osteonecrosis of the jaw: a randomized, controlled, prospective experimental study in rats. J Craniomaxillofac Surg. 2015;43(9):1823–8.
Vahtsevanos K, Kyrgidis A, Verrou E, Katodritou E, Triaridis S, Andreadis CG, et al. Longitudinal cohort study of risk factors in cancer patients of bisphosphonate-related osteonecrosis of the jaw. J Clin Oncol. 2009;27(32):5356–62.
Fehm T, Beck V, Banys M, Lipp HP, Hairass M, Reinert S, et al. Bisphosphonate-induced osteonecrosis of the jaw (ONJ): incidence and risk factors in patients with breast cancer and gynecological malignancies. Gynecol Oncol. 2009;112(3):605–9.
Saad F, Brown JE, Van Poznak C, Ibrahim T, Stemmer SM, Stopeck AT, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012;23(5):1341–7.
Kim T, Kim S, Song M, Lee C, Yagita H, Williams DW, et al. Removal of pre-existing Periodontal Inflammatory Condition before tooth extraction ameliorates medication-related osteonecrosis of the Jaw-Like Lesion in mice. Am J Pathol. 2018;188(10):2318–27.
Biasotto M, Chiandussi S, Zacchigna S, Moimas S, Dore F, Pozzato G, et al. A novel animal model to study non-spontaneous bisphosphonates osteonecrosis of jaw. J Oral Pathol Med. 2010;39(5):390–6.
Sarkarat F, Modarresi A, Chiniforush N, Yazdanparast L, Rakhshan V. Efficacy of photodynamic therapy in minimizing bisphosphonate-related osteonecrosis of the Jaws after Dental extraction: a preliminary animal study. J Oral Maxillofac Surg. 2019;77(2):307–14.
Kim JY, Jang HW, Kim JI, Cha IH. Effects of pre-extraction intermittent PTH administration on extraction socket healing in bisphosphonate administered ovariectomized rats. Sci Rep. 2021;11(1):54.
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Muller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res. 2010;25(7):1468–86.
Pacheco VN, Langie R, Etges A, Ponzoni D, Puricelli E. Nitrogen-containing bisphosphonate therapy: assessment of the alveolar bone structure in rats - a blind randomized controlled trial. Int J Exp Pathol. 2015;96(4):255–60.
Phipps KR, Stevens VJ. Relative contribution of caries and periodontal disease in adult tooth loss for an HMO dental population. J Public Health Dent. 1995;55(4):250–2.
Ficarra G, Beninati F, Rubino I, Vannucchi A, Longo G, Tonelli P, et al. Osteonecrosis of the jaws in periodontal patients with a history of bisphosphonates treatment. J Clin Periodontol. 2005;32(11):1123–8.
Boonyapakorn T, Schirmer I, Reichart PA, Sturm I, Massenkeil G. Bisphosphonate-induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol. 2008;44(9):857–69.
Duarte PM, Tezolin KR, Figueiredo LC, Feres M, Bastos MF. Microbial profile of ligature-induced periodontitis in rats. Arch Oral Biol. 2010;55(2):142–7.
Liu YF, Wu LA, Wang J, Wen LY, Wang XJ. Micro-computerized tomography analysis of alveolar bone loss in ligature- and nicotine-induced experimental periodontitis in rats. J Periodontal Res. 2010;45(6):714–9.
Bjornsson MJ, Velschow S, Stoltze K, Havemose-Poulsen A, Schou S, Holmstrup P. The influence of diet consistence, drinking water and bedding on periodontal disease in Sprague-Dawley rats. J Periodontal Res. 2003;38(6):543–50.
Meulman T, Peruzzo DC, Stipp RN, Goncalves PF, Sallum EA, Casati MZ, et al. Impact of Porphyromonas gingivalis inoculation on ligature-induced alveolar bone loss. A pilot study in rats. J Periodontal Res. 2011;46(5):629–36.
Aguirre JI, Castillo EJ, Kimmel DB. Preclinical models of medication-related osteonecrosis of the jaw (MRONJ). Bone. 2021;153:116184.
Tamaki S, Kuroshima S, Hayano H, Nakajima K, Kakehashi H, Ishisaki A, et al. Dynamic polarization shifting from M1 to M2 macrophages in reduced osteonecrosis of the jaw-like lesions by cessation of anti-RANKL antibody in mice. Bone. 2020;141:115560.
Soundia A, Hadaya D, Chau Y, Gkouveris I, Bezouglaia O, Dry S, et al. Local RANKL delivery improves socket healing in bisphosphonate treated rats. Bone. 2021;148:115945.
Adachi N, Ayukawa Y, Yasunami N, Furuhashi A, Imai M, Sanda K, et al. Preventive effect of fluvastatin on the development of medication-related osteonecrosis of the jaw. Sci Rep. 2020;10(1):5620.
Kim JW, Cha IH, Kim SJ, Kim MR. Biomarkers for bisphosphonate-related osteonecrosis of the Jaw. Clin Implant Dent Relat Res. 2016;18(2):281–91.
Aghaloo TL, Kang B, Sung EC, Shoff M, Ronconi M, Gotcher JE, et al. Periodontal disease and bisphosphonates induce osteonecrosis of the jaws in the rat. J Bone Miner Res. 2011;26(8):1871–82.
Cetinkaya BO, Keles GC, Ayas B, Gurgor P. Effects of risedronate on alveolar bone loss and angiogenesis: a stereologic study in rats. J Periodontol. 2008;79(10):1950–61.
Li CL, Lu WW, Seneviratne CJ, Leung WK, Zwahlen RA, Zheng LW. Role of periodontal disease in bisphosphonate-related osteonecrosis of the jaws in ovariectomized rats. Clin Oral Implants Res. 2016;27(1):1–6.
Tsurushima H, Kokuryo S, Sakaguchi O, Tanaka J, Tominaga K. Bacterial promotion of bisphosphonate-induced osteonecrosis in Wistar rats. Int J Oral Maxillofac Surg. 2013;42(11):1481–7.
Hadaya D, Gkouveris I, Soundia A, Bezouglaia O, Boyce RW, Stolina M, et al. Clinically relevant doses of sclerostin antibody do not induce osteonecrosis of the Jaw (ONJ) in rats with experimental periodontitis. J Bone Miner Res. 2019;34(1):171–81.
Zhang Q, Atsuta I, Liu S, Chen C, Shi S, Shi S, et al. IL-17-mediated M1/M2 macrophage alteration contributes to pathogenesis of bisphosphonate-related osteonecrosis of the jaws. Clin Cancer Res. 2013;19(12):3176–88.
Paschalidi P, Gkouveris I, Soundia A, Kalfarentzos E, Vardas E, Georgaki M, et al. The role of M1 and M2 macrophage polarization in progression of medication-related osteonecrosis of the jaw. Clin Oral Investig. 2021;25(5):2845–57.
Acknowledgements
Not applicable.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant no. 2017R1D1A1B03033657 and 2021R1A6A3A01087956).
Author information
Authors and Affiliations
Contributions
K.M.P. and J.C. wrote the drafted manuscript; W.P. and K.M.P. designed the study; K.M.P., J.C. and N.S.P. performed the animal experiments; J.C., N.S.P. and K.D.K. performed the data analysis; J.S.L., K.D.K. and W.P. performed critically revised the manuscript; W.P. supervised the manuscript preparation. All author reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This investigation was carried out in accordance with the revised animals Act 1986 in the UK used for scientific procedure, and confirm the study complied with the ARRIVE guidelines. Animal selection, management, surgical protocol, and preparation followed a routine protocol approved by the Institutional Animal Care and Use Committee of Yonsei University Health System (IACUC No. 2016 − 0171).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, KM., Cheong, J., Pang, NS. et al. Medication-related osteonecrosis of the jaw using periodontitis-induced rat before tooth extraction. BMC Oral Health 23, 561 (2023). https://doi.org/10.1186/s12903-023-03200-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03200-x